Abstract
Introduction
Surgeons from a number of different specialties are now more commonly performing nasal reconstruction procedures to repair deformities resulting from trauma or tumor resection. Whenever a nasal reconstruction is performed, it is very important that the currently well-established plastic surgical techniques in this area should be correctly applied.
Methods
Overview of the surgical techniques for nasal reconstruction applied to typical nasal defects, on the basis of a selective review of the literature.
Results
Any of the structurally important layers of the nose (skin, cartilaginous framework, inner lining) that are missing must be reconstructed. The current techniques follow the principle of esthetic reconstruction. Thorough patient counseling enables the patient to cope with temporally protracted treatment, to withstand the associated social and psychological stress, and to decide whether to undergo an autologous reconstruction or a prosthetic replacement.
Discussion
The operating surgeon must have a great deal of experience in nasal reconstruction. The surgeon must, therefore, be a specialist with a particular emphasis in this area.
Keywords: plastic surgery, facial surgery, cosmetic surgery, nasal defect, rhinoplasty
Nasal reconstruction occupies a special position in facial plastic surgery because of the complex three-dimensional surface of the nose, the varying thickness of the skin covering it, its varying types of scaffolding ranging from rigid bone to flexible cartilage, and its inner epithelial lining.
Burget and Menick have written a seminal text on functionally and esthetically superior nasal reconstruction (1).
Other authors have described particular reconstructive techniques that can be used advantageously to repair defects at certain special sites. There are, as yet, no controlled studies on the quality of nasal reconstruction. The defects are too varied, and the reconstructions, though always based on the same basic principles, allow a great deal of room for creativity on the plastic surgeon’s part. This is an important characteristic of plastic surgery in general that makes it difficult to consider the types of therapy under discussion from the point of view of "evidence-based medicine."
Inadequate results are not infrequently seen, particularly with more complex types of nasal reconstruction. Such experiences have motivated the authors to describe in this article, for the general medical public, the types of results that are attainable. In a later issue of the Deutsches Ärzteblatt International, another article will appear on the subject of reconstructive surgery of the face, head, and neck.
Methods
The reconstructive techniques will be described here in order of increasing difficulty. The authors have assessed and made use of the literature known to them in the light of their own experience. No meta-analyses have been published to date regarding this heterogeneous complex of subjects.
Post-traumatic nasal defects
Traumatic nasal defects are often caused by dog bites. The amputated nasal tissue should be handled as a composite graft. The distance of tissue requiring reperfusion, i.e., up to the center of the amputated tissue, should not exceed 5 mm. Cartilaginous components must be removed if they will be a barrier to revascularization. In borderline cases, this may make the difference between inadequate and adequate healing. The cartilaginous scaffolding can then be reconstructed after stable healing. If the amputated tissue is of a more complex type, it may not be able to find an adequate connection to the vascular system, with the result that the tissue will become necrotic after reimplantation (box 1, figures 1a and b). Nasal reconstruction after trauma follows the same principles as nasal reconstruction after tumor resection, e.g., with a frontal flap (figure 2).
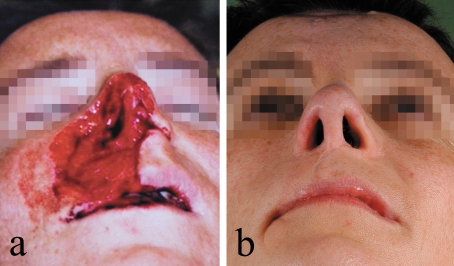
Box 1. Case illustration 1.
The patient sustained a dog-bite injury with partial amputation of the nose while away on vacation. An emergency reimplantation was performed in a nearby hospital, but the reimplanted tissue became necrotic and had to be removed. Treatment: lining of the interior of the right nostril with a pivot flap from the nasolabial area; support of the nostril, columella, and tip of the nose with ear cartilage; coverage with a forehead flap; rotated cheek flap for the nasolabial defect and the suboptimally transplanted right upper lip. The image on the right shows the result two and a half years later.
Figure 1.
(a) Tissue defect after dog-bite injury; (b) result two and a half years after reconstruction of the nose and upper lip.
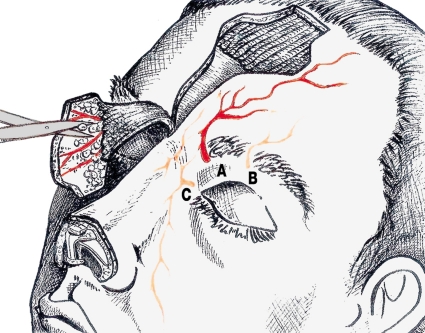
Figure 2.
Schematic illustration of the dissection of a forehead flap and the alternatives for vascular supply:
A, supratrochlear;
B, supraorbital;
C, branches of the angular artery system that can be used for a median frontal flap.
The strategy for nasal reconstruction after tumor resection
Most nasal tissue defects result from the resection of malignant tumors. Basal cell carcinoma is the most common type, followed by squamous cell carcinoma and melanoma. Other types of malignant tumor and benign destructive processes are rarer.
The difficult problems posed by basal cell carcinoma, a type of semi-malignant tumor, are often underestimated. If such a tumor is incompletely resected, with residual tumor either lateral or deep to the area of resection, the problem of reconstruction is much greater. This is particularly true of sclerodermiform basal cell carcinomas with poorly demarcated borders. R0 resection can best be assured by complete histopathological study of the tumor margins and base with 3D histology (2).
Squamous cell carcinoma can arise not only from the external skin of the nose, but also from its inner surface. Endonasal carcinomas are more dangerous, because they are discovered later. When these lesions are diagnosed early, organ-preserving surgical treatment can be performed, followed by partial reconstruction. The radicality of resection, however, must never be compromised. In borderline cases, it remains the best option to amputate a severely affected nose and reconstruct it later.
Single-procedure reconstructive techniques
Only small nasal defects are reparable by reconstructive techniques that can be performed completely in a single operative procedure. "Esthetic reconstruction" is the current name given cosmetically satisfactory results. Ideally, the skin flaps that are used will respect the borders between the various subunits of the nose—the dorsum, sidewall, and tip of the nose, the soft triangle, the nostrils, and the columella. Rotation flaps, transposition flaps, V-Y-plasties, subcutaneously pedicled sliding flaps (3–5) and bilobed flaps (1, 6) are the known standard techniques. The applied flaps will be very conspicuous if they extend beyond the furrows bordering the nostrils, or if the scar at their periphery crosses over the tip of the nose.
Median defects involving the tip and distal dorsum of the nose can be repaired with an extension flap from the cranial part of the dorsum (Rintala flap, [7]).
Very small defects at the tip of the nose can be covered with thick full-thickness skin grafts from the forehead beneath the hairline; these heal more slowly than the thinner full-thickness grafts that can be used to repair the cranial half of the nose but cannot provide fully adequate coverage of the tip.
Nostril defects involving less than about one-third of the nostril can be repaired with a "composite graft" (1) consisting of skin and cartilage from the ear, with a good chance of success.
If the defect involves more than 25% of the tip of the nose or of a nostril, then, for esthetic reasons, it should be reconstructed as an entire subunit of the nose, singly or in combination (1). It may no longer be possible to do this in a single procedure.
A prime example of the above is the reconstruction of an entire nostril. Although this can be done in a single procedure with a nasolabial rotation flap, the procedure destroys the furrow between the base of the nose and the cheek, which defines the border of the nose, and therefore causes a cosmetic deformity. Better cosmetic results can be achieved if a transposition flap with a cranial subcutaneous pedicle is used, and/or the flap is thinned in a second operative step. The advantage of a single surgical procedure is thereby lost.
Multiple-step reconstructive techniques
A paramedian forehead flap (1) is the method of choice for complete reconstruction of a nostril in accordance with the subunit concept (box 2, figures 3a and b). This is a distant flap that obtains its blood supply from the medial side of the eyebrow. The vertical vascular architecture of the forehead enables the flap to be constructed with a bridge of skin from the forehead containing a defined blood vessel (figure 2), so that a large piece of skin can be displaced from the forehead into the nasal skin defect without any compromise of its blood supply. A second procedure is needed to divide the bridge, integrate the flap, and reconstruct the anatomy of the eyebrow. During this procedure, the graft donor site on the forehead is converted into a linear vertical scar.
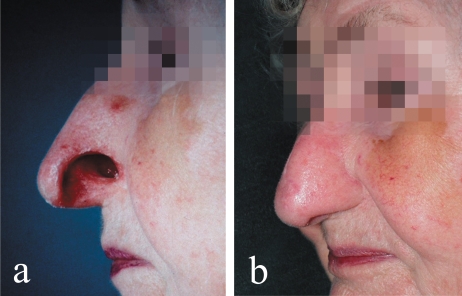
Box 2. Case illustration 2.
The patient was an 80-year-old woman with a small Merkel cell carcinoma of the left nostril. The entire nostril was resected as part of the R0 resection that was required. Because of the known frequency of local recurrence, treatment with a partial epithesis was chosen. The patient was not comfortable with the adhesive-affixed epithesis, however, and urgently requested a reconstructive procedure with autologous tissue. A thin cutaneous pedicle flap was swung over from the dorsum of the nose into the defect as an inverted flap to provide an inner lining, and the nostril was stabilized with ear cartilage. The combined skin defect of the nostril and the donor area was covered with a paramedian forehead flap. The skin of the neo-vestibulum healed in place without any peripheral necrosis. The reconstructed nostril held its form stably without shrinking over the ensuing year of follow-up.
Figure 3.
(a) Nostril defect due to Merkel cell carcinoma; (b) the result one year after three-layer nostril reconstruction.
The tip of the nose, too, is best reconstructed as an entire subunit with a forehead flap. When the columella is reconstructed, hairiness of the skin over the columella must sometimes be accepted as a temporary disadvantage, because the distance from the base of the pedicle on the eyebrow to the base of the columella where it meets the upper lip usually exceeds the height of the forehead below the hairline. Operative epilation by removal of the subcutaneous roots of the hair requires further intermittent surgical treatment. Nonsurgical alternatives such as laser epilation can be considered.
The patient’s age and personal wishes should also be considered when a reconstructive technique is chosen. In this context, the question must also be addressed whether the tissue defect must be extended to an entire esthetic subunit of the nose, which will then be totally reconstructed (8).
Two-layer nasal defects
When the tissue defect involves not just the skin of the nose, but its scaffolding as well, a stable reconstruction of the cartilaginous scaffolding requires repair of the skin with a vascular pedicle flap. If a free skin graft is performed, this will not be possible in a single procedure.
Septum cartilage is a very good substitute for the cartilaginous scaffolding of the tip of the nose and the columella. Alternatively, ear cartilage can be harvested from the concha. Because of its curvature, cartilage from this site is particularly useful as a supportive structure for the nostril. If no cartilage is inserted into the lateral portion of the nostril, it will shrink and lose its mechanical stability. This results in collapse of the nostril, particularly during inspiration, with impairment of breathing. From the esthetic point of view, a symmetrical result is impossible unless a cartilaginous splint of this kind is inserted, either primarily or secondarily.
Perforating defects involving all layers of the nose
These require a reconstruction of the inner lining of the nose (1) with vital tissue that will not shrink. An ipsi- or contralateral septal mucosal flap is suitable. The flap can be supported with a cartilaginous scaffolding at once and then covered with a skin flap. A forehead flap that is longer than about 2.5 cm cannot be adequately thinned primarily, because peripheral necrosis would develop. An intermediate step three weeks after the primary procedure is necessary for thinning of the flap. Consequently, the reconstruction must be performed in a total of three steps, which, from the first procedure to the last suture removal, take a total of two months.
Menick’s technique of nostril reconstruction involves surgery in three planned stages (9, 10). First, the inner lining of the nostril is replaced with a full-thickness skin graft, while the septal mucosa is spared. The graft is covered with a forehead flap at once and revascularized by it. The necessary cartilaginous splinting and thinning of the flap can only be performed in an intermediate step four weeks later, when the full-thickness skin graft has converted into a stable, autonomous lining of the nostril. Finally, three weeks after that, the reconstruction is completed in a third operation in which the pedicle of the forehead flap is divided.
More complex nasal defects and total loss of the nose
If the nasal septum, the central supportive structure of the nose, is lost, e.g., after the resection of an extensive, sclerodermiform basal cell carcinoma of the outer and inner nose (box 3, figures 4a and b), the anterior part of the septum must be reconstructed first. The septal scaffolding that remains dorsally must be reimplanted ventrally, and the mucosa must be moved forward in the form of bilateral rotated flaps (1). Reconstruction of the anterior septum is an indispensable prerequisite for total nasal reconstruction, because a scaffolding—even if it is no more than an L-shaped frame—cannot be constructed without an inner layer of tissue that is well perfused and has no gaps. It is true that the ventral rotation of residual septal tissue causes a large posterior septal defect, but this causes few problems for the patient, who must simply learn proper techniques of nasal hygiene. The inner lining of the respiratory passages can then be additionally reconstructed with inverted skin flaps from the medial cheeks. A delay procedure and a waiting period of one to three weeks improve the viability of these flaps.
Box 3. Case illustration 3.
This 55-year-old woman underwent resection of a basal cell carcinoma of the tip of the nose with full-thickness skin grafting alio loco 12 years before the procedure to be described. Five years later, an extensive recurrent tumor appeared, and there seemed to be no prospect for successful medical treatment in sight. Seven years of desperation and "alternative" treatments followed. Finally, the patient presented to us with an ulcus rodens involving the nose, upper lip, and neighboring areas of the cheeks. The treatment consisted of resection of the tumor well into the area of healthy tissue, including resection and reconstruction of the upper lip, full-thickness skin grafting to the areas of cutaneous resection on the cheeks, and epithetic treatment of the nose. Because of the history of tumor recurrence and the risk of a second recurrence, the patient was followed up for a further two years before nasal reconstruction was performed. The residual septum was transposed ventrally for anterior septal reconstruction after two delay procedures. Two months later, the initially severe edema had subsided so that the septum could be divided once again and a mucosal flap could be taken for partial lining of the nostril. The lateral portion of the nostril and the nasal walls were lined with turn over flaps from the transplanted areas of the medial cheeks, the cartilaginous scaffolding was built up, and the skin of the nose was closed with a large forehead flap. The skin defect on the cheeks in the area where the flaps had been taken was covered with extension flaps, while that on the upper forehead healed by second intention in cosmetically acceptable fashion over the course of a further 10 weeks. The patient can breathe freely and is very happy with the result.
Figure4.
(a) Recurrent basal cell carcinoma of the nose and upper lip; (b) the result one year after total nasal reconstruction.
If the surgeon must replace the entire scaffolding of the nose, rib cartilage will be needed. An L-shaped central scaffolding should be constructed out of rib cartilage in such a way that bending forces are neutralized. Once this graft heals in place, the patient can count on lifelong stability (11).
The skin of the nose is reconstructed in three steps with a forehead flap as already shown in the above discussion of partial reconstructions. The frontal defect at the donor site cannot, however, be closed primarily in view of the large surface area of tissue required to reconstruct the entire nose. It can only be made as narrow as possible and then allowed to heal by second intention. The ensuing scar borders on the hairy skin of the scalp and can often be adequately covered with hair.
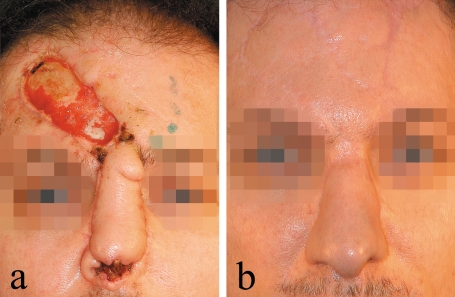
The greater the defects are, and when not only the septum, but also the nostril(s) and other parts of the wall of the nose are affected, the more precisely the operation must be planned in advance. Planning is more difficult if a reconstructive procedure has already been attempted without success (box 4, figures 5a and b).
Box 4. Case illustration 4.
A man in his mid-forties with nasal carcinoma underwent resection of the tumor followed by nasal reconstruction with a forehead flap based on a paramedian pedicle whose ascent in the lateral direction was atypically flat. The tip of the flap, which was meant to cover the columella, became necrotic. The flap could no longer be used to cover the defect but was successfully returned to its site of origin on the forehead. In the same procedure, the septum was rotated ventrally to support a new, central nasal reconstruction. After an interval of two months to allow stabilization of the septum and the right side of the forehead, a new, large forehead flap was taken from the left side and used to cover the entire nose, including the columella, with vital tissue. Four months later, there was a conspicuous frontal scar, but the patient’s nose had healed so well that his close friends could not immediately recognize it as a reconstruction.
Figure 5.
(a) Loss of the columella after nasal reconstruction with an oblique frontal flap, alio loco; (b) the result six months after revision and reoperative total nasal reconstruction.
The necessity of each individual operative step and the corresponding investment of time must be explained thoroughly to the patient. Sequential images of reconstructions that the surgeon has already performed are helpful for this. The best form of encouragement comes from other patients whose successful treatment is already complete.
Pedicle-based flaps from the vicinity of the nose and from the forehead can only replace a finite surface area of skin. The first priority is the need to reconstruct adequately wide nostrils and free respiratory passages. In case of very large defects with missing local material, the inner layer must first be reconstructed with free microvascular fasciocutaneous flaps in a preliminary operation (12). After four to five weeks, retrograde perfusion through the edges of the wound is assured. The subcutaneous tissue, which is too thick, must then be thinned and the external nose reconstructed with a cartilaginous scaffolding and a forehead flap in three further operations, as already described.
Waiting period and temporal planning of the reconstruction
The proper timing of a complex nasal reconstruction after the treatment of a malignant tumor is currently a matter of debate. Even after an R0 resection guided by 3D histology, the possibility of tumor recurrence can never be fully excluded. In view of the complex three-dimensional structure of the nose, the degree of certainty that the periphery of the tumor has been totally removed must be taken into account in further treatment planning, along with the type, grade, and stage of the tumor. If adjuvant therapy is needed, it should be provided immediately after tumor resection.
Nasal reconstruction makes it more difficult to inspect the local area for tumor recurrences. In doubtful cases, a secondary reconstruction should be recommended to the patient. The authors recommend a minimum interval of one year for carcinoma and two years for sclerodermiform basal cell carcinoma, which grows very slowly but is no less destructive. A nasal epithesis can be placed over the defect for temporary coverage of the missing tissue. This takes mental pressure off the patient so that he or she can more calmly consider the various possibilities for reconstruction, with the associated emotional stresses and limitations of each.
Conclusion
Various transplant techniques and plastic procedures involving flaps are available for the coverage of apparently small cutaneous defects of the nose. Not all of these techniques are of equal value, however. Nasal reconstructions must nowadays satisfy both high functional and high esthetic demands.
Because the available material for grafting is not very extensive, exact planning is always necessary, all the more so for larger nasal reconstructions. When the defect has been caused by a tumor, the possibility of recurrence must always be considered. If there is a risk of recurrence, a waiting period is advisable before the reconstruction. Timely collaboration of ENT surgeons and dermatologists with the plastic surgeon performing the reconstruction is highly desirable. The person who stands to benefit the most from a team effort is the patient.
Key messages.
Esthetic nasal reconstruction is one of the more difficult challenges in plastic surgery, particularly when the defect is in multiple tissue layers.
It may be necessary to enlarge a defect to an entire subunit of the nose (e.g., tip, nostril, or columella) before performing the reconstruction so that the repair will look normal.
The forehead flap is the most important and farthest-reaching type of cutaneous flap for nasal reconstruction.
The cartilaginous scaffolding must be adequately reconstructed; if not, the result will be a cosmetic deformity as well as impaired breathing because of functional instability (e.g., collapse of the nostril in inspiration).
If the vital inner cutaneous or mucosal lining of the nose is not reconstructed, scarring will result in a critical constriction of the airway, ranging all the way to possible occlusion.
Acknowledgments
We thank all of the patients for permission to use their photographs to illustrate the treatment concepts discussed in this article. We also thank Dr. med. Uwe Maisa for drawing the schematic illustration of the forehead flap (figure 2).
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement
The authors declare that they have no conflict of interest as defined by the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Burget GC, Menick FJ. Aesthetic reconstruction of the nose. St. Louis: Mosby; 1994. [Google Scholar]
- 2.Breuninger H, Konz B, Berg G. Mikroskopisch kontrollierte Chirurgie bei malignen Hauttumoren. Dtsch Arztebl. 2007;104:A427–A432. [Google Scholar]
- 3.Rieger RA. Local flap for repair of the nasal tip. Plast Reconstr Surg. 1967;40:147–149. doi: 10.1097/00006534-196708000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Marchac D, Toth B. The axial frontonasal flap revisited. Plast Reconstr Surg. 1985;76:686–694. doi: 10.1097/00006534-198511000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Tellioglu AT, Tekdemir I, Saray A, Eker E. Reconstruction of proximal nasal defects with island composite nasal flaps. Plast Reconstr Surg. 2005;115:416–422. doi: 10.1097/01.prs.0000149533.55827.b1. [DOI] [PubMed] [Google Scholar]
- 6.Jackson JT. Local flaps in head and neck reconstruction. St. Louis, Missouri: Quality Medical Publishing; pp. 169–170. [Google Scholar]
- 7.Rintala AE, Asko-Seljavaara S. Reconstruction of midline skin defects of the nose. Scand J Plast Reconstr Surg. 1969;3:105–108. doi: 10.3109/02844316909036701. [DOI] [PubMed] [Google Scholar]
- 8.Rohrich RJ, Griffin JR, Ansari M, Beran SJ, Potter JK. Nasal reconstruction - beyond aesthetic subunits: a 15-year review of 1334 Cases. Plast Reconstr Surg. 2004;114:1405–1416. doi: 10.1097/01.prs.0000138596.57393.05. [DOI] [PubMed] [Google Scholar]
- 9.Menick FJ. The use of skin grafts for nasal lining. Otolaryngol Clin. 2001;34:791–804. [PubMed] [Google Scholar]
- 10.Menick FJ. A 10-year experience in nasal reconstruction with three-staged forehead flap. Plast Reconstr Surg. 2002;109:1839–1855. doi: 10.1097/00006534-200205000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Horton CE, Metthews MS. Nasal reconstruction with autologous rib cartilage: a 43-year follow-up. Plast Reconstr Surg. 1992;89:131–135. [PubMed] [Google Scholar]
- 12.Walton RL, Burget GC, Beahm EK. Microsurgical reconstruction of the nasal lining. Plast Reconstr Surg. 2005;115:1813–1829. doi: 10.1097/01.prs.0000164683.34767.2f. [DOI] [PubMed] [Google Scholar]