Abstract
Introduction
The prevalence of obesity and elevated waist circumference in Germany is high. However, there are insufficient data on the situation in primary care and on regional distribution to support medical preventive measures.
Methods
The German Metabolic and Cardiovascular Risk Project (GEMCAS) is a national cross-sectional study including 1511 primary care practices and 35 869 patients. Height, weight, waist circumference, laboratory values, and type 2 diabetes were documented.
Results
The crude prevalence of obesity was 23.9% (95% CI 23.4 to 24.3) (standardized 22.8% [95% CI 22.3 to 23.2]), with a minimum in Bremen (19.8% [95% CI 15.1 to 24.5]) and a maximum in Saxony-Anhalt (28.3% [95% CI 25.4 to 31.1]). The crude prevalence of high waist circumference (> 102/88 cm) was 39.5% (95% CI 39.0 to 40.0) (standardized 36.5% [95% CI 36.0 to 36.9]), with a minimum in Hamburg (30.5% [95% CI 26.2 to 34.8]) and a maximum in Saxony-Anhalt (42.1% [95% CI 39.2 to 45.1]). The prevalence of obesity as assessed by BMI was higher in men than in women, but greater in women as assessed by waist circumference. Nationwide, 50 out of every 100 patients with obesity had type 2 diabetes, and 32 of 100 patients with a high waist circumference had type 2 diabetes.
Conclusions
The prevalence of obesity is higher in northeastern Germany than in the southwest. Overall, abdominal obesity is considerably more frequent than obesity based on BMI. Surprisingly, a high prevalence of obesity in some federal states does not automatically mean a higher number of people with type 2 diabetes.
Keywords: body mass index, overweight, prevalence, type 2 diabetes, regionalization, obesity
Overweight and obesity are common in Germany. An analysis of German data shows that the prevalence has increased continuously over the past 20 years (1). The recently published National Nutrition Survey II (Nationale Verzehrsstudie, NVS II) showed a prevalence of obesity in men of 20.5% and in women of 21.2% for 2006 (2). A notably increased waist circumference (>102 cm in men and >88 cm in women) was found in 27.4% of men and 31.8% of women. Between 1985 and 2002, a relative increase in the prevalence of obesity of 39% in men and 44% in women can be documented (3). According to data from the US National Health and Nutrition Examination Survey (NHANES), the prevalence of obesity is set to increase further (4).
The high prevalence of obesity requires new strategies, in order to stop this "epidemic" (5) at the individual level as well as the population level, and to reverse the trend. Preventing the growth of this epidemic is a classic public health task (3). In spite of many scientifically based treatment strategies, the medium term to long term success of conservative obesity therapies has been unsatisfactory. Only 15% of all persons with grade 1 and 2 obesity (body mass index [BMI] 30–40 kg/m2) are able to lose substantial amounts of weight and maintain their new weight for more than 5 years. Correcting grade 3 obesity (BMI ≥40 kg/m2) to a satisfactory degree by using conservative measures is possible only in rare exceptions. For this reason, the World Health Organization (WHO) has given greater priority to obesity prevention than has been the case so far (5).
The family doctor/general practitioner is the starting point for the population and may therefore assume a central role in the prevention and early detection of chronic diseases. Data on the prevalence of obesity and its accompanying problems as recorded in primary care settings is therefore urgently needed. This is also an essential condition for the future planning of resource distribution in the healthcare system. This is the focus of the current study, which reports current data on the prevalence of obesity as defined by BMI and waist circumference in Germany’s primary care system.
Additionally, data on the regional distribution and the association with type 2 diabetes are presented. Such a presentation makes sense as lifestyle habits and socioeconomic conditions within German differ widely and obesity prevalence rates may therefore also differ, as has been shown by NVS II (2).
Knowledge of regional distributions is also important because it provides a basis for the mostly regionally organized associations of statutory health insurance physicians to plan in accordance with healthcare needs. So far, only few regional preventive and therapeutic services have been available to tackle this condition in primary care; action is therefore urgently required. To provide current data on the prevalence of obesity, increased waist circumference, and type 2 diabetes and their regional distribution we evaluated the data set from the German Metabolic and Cardiovascular Risk Project (GEMCAS) (6, 7). This cross-sectional data collection was conducted in the fall of 2005 involving 1511 doctors’ surgeries with the participation of 35 869 patients.
Methods
Study design
GEMCAS data form the basis of this analysis (6, 7). This epidemiological, cross-sectional study aimed to collect data on the prevalence of the metabolic syndrome in primary care on a national level. The practices included were family doctors’ practices (general physicians, general practitioners, specialists in internal medicine—no practices specializing in diabetology or cardiology) from all over Germany, which were randomly selected. The objective was for the practices to recruit for the study in one morning all—as far as possible—patients older than 18 years, independently of the reason for their visit. The study was approved by the ethics committee at the University of Duisburg-Essen.
The examination included standardized measurement of BMI, waist circumference, and blood pressure, as well as blood glucose and serum lipid analysis. The study was conducted in accordance with the recommendations for good epidemiological practice (GEP). Nationwide onsite and telephone monitoring also secured the study quality (7).
Measuring and defining overweight, obesity, and increased waist circumference
On the study day, the doctors reported data on height, weight, and waist circumference. Overweight was defined as a BMI ≥25 kg/m2 and <30 kg/m2, and obesity as a BMI ≥30 kg/m2. Waist circumference was measured midway between the lower edge of the last rib and the highest part of the iliac crest. The measurements were classified as moderately (men >94 to 102 cm, women >80 to 88 cm) and notably increased waist circumference (men >102 cm, women >88 cm). Diabetes was recorded by doctors’ diagnoses.
Statistical analysis
The statistical analysis included the calculation of crude prevalence rates and their standardization by age and/or sex to the German population in 2004 (8). Regional allocation was done by using the doctors’ practices’ post codes. The software package SAS 9.1 was used to analyze the data.
Results
Of the 17 271 doctors who were invited to participate in the study, 2600 were willing to participate in principle. The final number of doctors recruited was 1511. The proportion of participating doctors relative to the total number of doctors in the respective federal state or the regional association of statutory health insurance physicians varied between 1.89% (Hamburg) and 4.57% (Saarland) (table 1). In the study period of 10 to 21 October 2005, doctors included 35 869 patients into the study (participation rate 85.6%). The patients’ mean age was 51.7±16.1 years; 38.9% of patients were men. Patients’ characteristics have been published elsewhere (6, 7, 11, 14, 20).
Table 1. Regional distribution of practices and patients.
| Federal state / regional Association of Statutory Health Insurance Physicians | Participating general practitioners | Total number of general practitioners*1 | % of all general practitioners | GEMCAS patients |
| Baden-Württemberg | 186 | 6927 | 2,68 | 4283 |
| Bavaria | 248 | 8923 | 2.78 | 5589 |
| Berlin | 91 | 2462 | 3.40 | 2126 |
| Brandenburg | 36 | 1520 | 2.37 | 968 |
| Bremen | 12 | 447 | 2.68 | 325 |
| Hamburg | 23 | 1216 | 1.89*2 | 435 |
| Hesse | 87 | 3914 | 2.22*2 | 2039 |
| Mecklenburg-Western Pomerania | 37 | 1128 | 3.28 | 915 |
| Lower Saxony | 141 | 4890 | 2.88 | 3153 |
| North Rhine-Westphalia | 313 | 10 778 | 2.90 | 7793 |
| Rhineland-Palatinate | 64 | 2633 | 2.43 | 1553 |
| Saarland | 30 | 657 | 4.57*2 | 727 |
| Saxony | 89 | 2693 | 3.30 | 2183 |
| Saxony-Anhalt | 42 | 1508 | 2.79 | 1108 |
| Schleswig-Holstein | 58 | 1935 | 3.00 | 1238 |
| Thuringia | 54 | 1514 | 3.57*2 | 1437 |
| Total | 1511 | 53 145 | 2.84 | 35 869 |
*1 According to the National Association of Statutory Health Insurance Physicians as at 31 December 2006 (www.kbv.de);
*2 Proportions that deviate from the mean by more than 20% in either direction
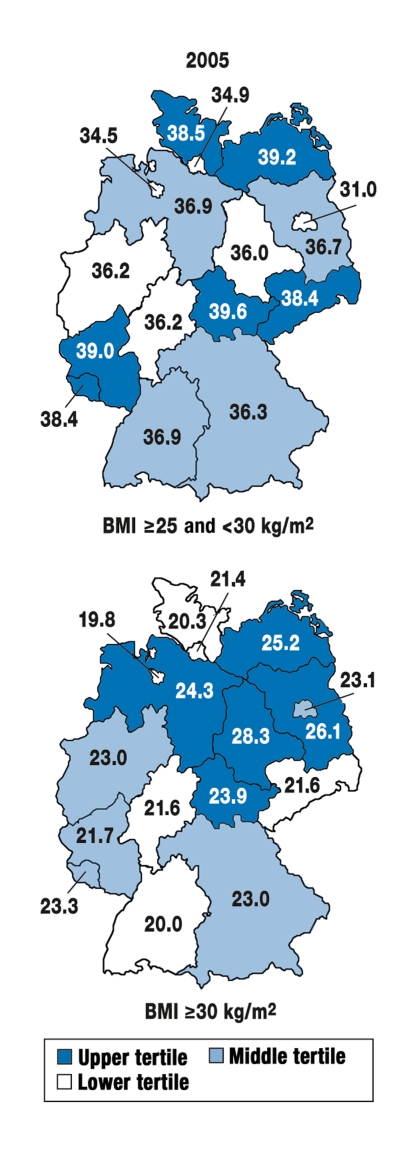
Overweight and obesity according to BMI
The prevalence of overweight was 36.4% (95% confidence interval [CI] 36.0 to 37.0), after standardization it was 36.6% (CI 36.1 to 37.2). The crude prevalence of obesity was 23.9% (CI 23.4 to 24.3), and the standardized prevalence was 22.8% (CI 22.3 to 23.2) (table 2). The prevalence of obesity increased notably with age. More men than women were obese. Table 3 shows the regional distribution of overweight and obesity, standardized by age and sex, by federal state (population of Germany in 2004). The highest prevalence rates were noted for the northeastern states (Mecklenburg-Western Pomerania, Brandenburg, Saxony-Anhalt, and Thuringia). The lowest rates for obesity were found in Schleswig-Holstein, Hesse, and Baden-Württemberg and in the city states Bremen and Hamburg. The maximum rate ratio of the states was 1.15 : 1 (Thuringia versus Bremen) and for obesity, 1.43 : 1 (Saxony-Anhalt versus Bremen). Figure 1 shows the regional distribution of overweight and obesity.
Table 2. Prevalence of overweight/obesity, moderately/notably increased waist circumference, and type 2 diabetes in primary care (October 2005).
| Overweight | Obesity | Moderately increased waist circumference | Notably increased waist circumference | Type 2 diabetes | |||||||||||
| n | % | 95% CI | n | % | 95% CI | n | % | 95% CI | n | % | 95% CI | n | % | 95% CI | |
| 18–34 years | |||||||||||||||
| Men | 589 | 31.2 | 29.1–33.3 | 248 | 13.1 | 11.6–14.7 | 263 | 14.0 | 12.5–15.6 | 241 | 12.8 | 11.3–14.4 | 9 | 0.5 | 0.2–1.0 |
| Women | 654 | 18.0 | 16.8–19.3 | 463 | 12.8 | 11.7–13.9 | 513 | 14.2 | 13.1–15.4 | 694 | 19.2 | 18.0–20.6 | 11 | 0.3 | 0.2–0.6 |
| 35–44 years | |||||||||||||||
| Men | 974 | 42.9 | 40.9–45.0 | 498 | 21.9 | 20.3–23.7 | 526 | 23.3 | 21.5–25.1 | 582 | 25.7 | 23.9–27.6 | 88 | 4.1 | 3.3–5.0 |
| Women | 1068 | 24.5 | 23.2–25.8 | 727 | 16.7 | 15.6–17.8 | 875 | 20.1 | 18.9–21.3 | 1215 | 27.9 | 26.6–29.3 | 82 | 2.0 | 1.6–2.4 |
| 45–54 years | |||||||||||||||
| Men | 1342 | 45.2 | 43.4–47.0 | 822 | 27.7 | 26.1–29.3 | 846 | 28.6 | 27.0–30.3 | 1081 | 36.6 | 34.8–38.3 | 351 | 12.5 | 11.3–13.8 |
| Women | 1493 | 30.6 | 29.3–31.9 | 1 196 | 24.5 | 23.3–25.7 | 1 063 | 21.8 | 20.7–23.0 | 1970 | 40.5 | 39.1–41.8 | 289 | 6.2 | 5.5–6.9 |
| 55–64 years | |||||||||||||||
| Men | 1488 | 50.3 | 48.5–52.1 | 846 | 28.6 | 27.0–30.3 | 836 | 28.4 | 26.7–30.0 | 1306 | 44.3 | 42.5–46.1 | 679 | 24.1 | 22.6–25.8 |
| Women | 1422 | 36.0 | 34.5–37.5 | 1199 | 30.3 | 28.9–31.8 | 906 | 23.0 | 21.6–24.3 | 2076 | 52.6 | 51.0–54.2 | 522 | 13.8 | 12.8–15.0 |
| 65–74 years | |||||||||||||||
| Men | 1363 | 51.6 | 49.6–53.5 | 762 | 30.0 | 28.2–31.8 | 798 | 30.2 | 28.4–32.0 | 1314 | 49.7 | 47.8–51.6 | 741 | 29.3 | 27.5–31.1 |
| Women | 1287 | 40.3 | 38.6–42.0 | 1062 | 33.2 | 31.6–34.9 | 690 | 21.7 | 20.2–23.1 | 2015 | 63.2 | 61.5–64.9 | 723 | 23.7 | 22.2–25.2 |
| 75–84 years | |||||||||||||||
| Men | 561 | 51.8 | 48.7–54.8 | 215 | 19.8 | 17.5–22.3 | 330 | 30.5 | 27.8–33.4 | 487 | 45.1 | 42.1–48.1 | 305 | 29.4 | 26.6–32.3 |
| Women | 688 | 41.7 | 39.3–44.1 | 425 | 25.8 | 23.7–27.9 | 384 | 23.4 | 21.4–25.5 | 982 | 59.8 | 57.4–62.2 | 434 | 27.4 | 25.2–29.6 |
| > 84 years | |||||||||||||||
| Men | 38 | 42.7 | 32.3–53.6 | 14 | 15.7 | 8.9–25.0 | 28 | 32.6 | 22.8–43.5 | 31 | 36.0 | 26.0–47.1 | 24 | 28.6 | 19.2–39.5 |
| Women | 70 | 37.2 | 30.3–44.6 | 25 | 13.3 | 8.8–19.0 | 57 | 30.2 | 23.7–37.2 | 86 | 45.5 | 38.3–52.9 | 59 | 31.7 | 25.1–38.9 |
| Total | |||||||||||||||
| Men | 6355 | 45.7 | 44.9–46.5 | 3419 | 24.7 | 24.0–25.4 | 3627 | 26.2 | 25.4–26.9 | 5042 | 36.4 | 35.6–37.2 | 2 197 | 16.6 | 16.0–17.3 |
| Women | 6682 | 30.6 | 30.0–31.2 | 5097 | 23.3 | 22.8–23.9 | 4488 | 20.6 | 20.1–21.1 | 9038 | 41.5 | 40.8–42.1 | 2 120 | 10.1 | 9.7–10.5 |
Moderately increased waist circumference in men >94 cm and ≤102 cm, in women >80 cm and ≤88 cm; notably increased waist circumference in men >102 cm and in women, >88 cm. 95% CI, 95% confidence interval
Table 3. Prevalence of obesity and notably increased waist circumference (crude and adjusted for age and sex [8]) in primary care (October 2005), by federal state where the practice is based.
| BMI ≥ 30 kg/m2 | Waist circumference >102 cm in men and >88 cm in women | Type 2 diabetes | |||||||||||||
| Crude | Adjusted | Crude | Adjusted | Crude | Adjusted | ||||||||||
| n | % | 95% CI | % | 95% CI | n | % | 95% CI | % | 95% CI | n | % | 95% CI | % | 95% CI | |
| Baden-Württemberg | 911 | 21.3 | 20.1–22.6 | 20.0 | 18.8–21.3 | 1579 | 37.1 | 35.6–38.6 | 33.4 | 32.1–34.8 | 520 | 12.8 | 11.8–13.8 | 11.1 | 10.2–11.9 |
| Bavaria | 1322 | 23.7 | 22.6–24.9 | 23.0 | 21.8–24.1 | 2128 | 38.3 | 37.1–39.6 | 35.7 | 34.4–36.9 | 696 | 13.1 | 12.2–14.1 | 12.1 | 11.3–12.9 |
| Berlin | 666 | 23.7 | 21.9–25.5 | 23.1 | 21.2–24.9 | 746 | 35.2 | 33.2–37.3 | 33.2 | 31.2–35.2 | 261 | 12.7 | 11.3–14.2 | 12.1 | 10.8–13.4 |
| Brandenburg | 279 | 28.8 | 26.0–31.8 | 26.1 | 23.0–29.1 | 436 | 45.2 | 42.0–48.4 | 39.6 | 36.2–43.0 | 165 | 17.5 | 15.1–20.1 | 13.8 | 11.7–15.9 |
| Bremen | 63 | 19.4 | 15.2–24.1 | 19.8 | 15.1–24.5 | 118 | 36.3 | 31.1–41.8 | 34.2 | 29.0–39.5 | 32 | 10.3 | 7.1–14.2 | 9.5 | 6.3–12.8 |
| Hamburg | 97 | 22.4 | 18.6–26.6 | 21.4 | 17.5–25.3 | 139 | 32.0 | 27.7–36.6 | 30.5 | 26.2–34.8 | 33 | 8.3 | 5.8–11.4 | 7.5 | 5.1–9.9 |
| Hesse | 440 | 21.7 | 19.9–23.6 | 21.6 | 19.7–23.5 | 748 | 37.0 | 34.9–39.2 | 35.6 | 33.5–37.7 | 208 | 11.0 | 9.7–12.5 | 10.5 | 9.2–11.9 |
| Mecklenburg-Western Pomerania | 254 | 27.9 | 25.0–30.9 | 25.2 | 22.4–28.1 | 376 | 41.5 | 38.3–44.8 | 36.7 | 33.6–39.8 | 136 | 15.2 | 12.9–17.7 | 13.2 | 11.0–15.3 |
| Lower Saxony | 792 | 25.2 | 23.7–26.7 | 24.3 | 22.7–25.9 | 1346 | 42.9 | 41.1–44.6 | 40.4 | 38.7–42.1 | 304 | 10.1 | 9.0–11.2 | 9.4 | 8.4–10.4 |
| North Rhine-Westphalia | 1858 | 23.9 | 23.0–24.9 | 23.0 | 22.0–24.0 | 3123 | 40.4 | 39.3–41.5 | 37.5 | 36.4–38.6 | 889 | 12.0 | 11.3–12.8 | 10.8 | 10.2–11.5 |
| Rhineland-Palatinate | 347 | 22.4 | 20.4–24.6 | 21.7 | 19.6–23.9 | 633 | 40.9 | 38.5–43.4 | 37.8 | 35.3–40.2 | 183 | 12.3 | 10.7–14.1 | 11.2 | 9.7–12.7 |
| Saarland | 173 | 23.9 | 20.9–27.2 | 23.3 | 20.1–26.5 | 289 | 40.2 | 36.6–43.9 | 38.3 | 34.8–41.7 | 65 | 9.2 | 7.2–11.6 | 9.4 | 7.2–11.7 |
| Saxony | 517 | 23.7 | 21.9–25.6 | 21.6 | 19.8–23.4 | 828 | 38.1 | 36.0–40.1 | 33.4 | 31.4–35.3 | 383 | 18.2 | 16.6–19.9 | 15.8 | 14.4–17.3 |
| Saxony-Anhalt | 331 | 29.9 | 27.2–32.7 | 28.3 | 25.4–31.1 | 501 | 45.3 | 42.3–48.3 | 42.1 | 39.2–45.1 | 160 | 15.2 | 13.1–17.6 | 14.7 | 12.6–16.8 |
| Schleswig-Holstein | 264 | 21.3 | 19.1–23.7 | 20.3 | 17.9–22.6 | 470 | 38.3 | 35.5–41.1 | 36.0 | 33.3–38.7 | 95 | 8.1 | 6.6–9.8 | 8.0 | 6.5–9.5 |
| Thuringia | 382 | 26.7 | 24.4–29.1 | 23.9 | 21.7–26.2 | 620 | 43.5 | 40.9–46.2 | 38.4 | 35.9–40.9 | 187 | 13.5 | 11.8–15.4 | 11.4 | 9.9–12.9 |
| Total | 8696 | 23.9 | 23.4–24.3 | 22.8 | 22.3–23.2 | 14 080 | 39.5 | 39.0–40.0 | 36.5 | 36.0–36.9 | 4317 | 12.6 | 12.3–13.0 | 11.4 | 11.1–11.7 |
BMI, body mass index; 95% CI, 95% confidence interval
Figure 1.
Regional prevalence of overweight and obesity by federal state; standardized by age and sex according to (8)
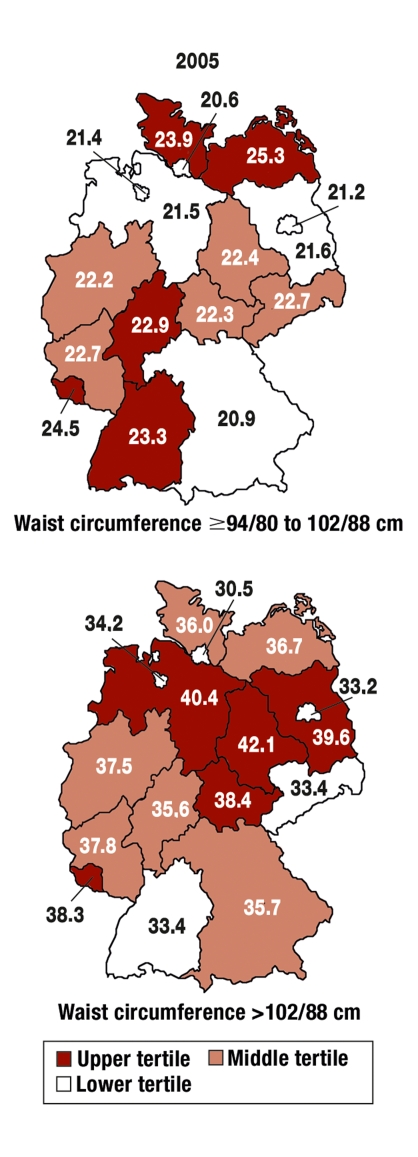
Abdominal obesity
The prevalence of moderately and notably increased waist circumference in the study population was 22.8% (CI 22.3 to 23.2) and 39.5% (CI 39.0 to 40.0). The standardized prevalence was 22.2% (CI 21.8 to 22.7) and 36.5% (CI 36.0 to 36.9). A clear increase was noted with increasing age. Women had an increased waist circumference notably more often than men (table 2). Table 3 shows the regional distribution of abdominal obesity. The northern and northeastern states (Lower Saxony, Mecklenburg-Western Pomerania, Brandenburg, Saxony-Anhalt, and Thuringia) had the highest prevalence rates. Patients were often overweight in Saarland and Rhineland-Palatinate. The lowest rates were seen in Berlin, Hamburg, and Bremen (only for abdominal obesity). Figure 2 shows the regional distribution of abdominal obesity.
Figure 2.
Regional prevalence of moderately or notably increased waist circumference by federal state; standardized according to (8)
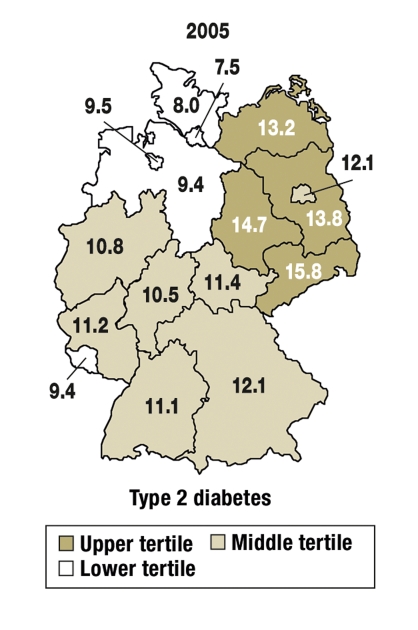
Type 2 diabetes relative to obesity
Regionalized prevalence rates of type 2 diabetes (as reported by doctors) are shown in figure 3. For the whole of Germany, we saw a mean of 50 patients with type 2 diabetes for every 100 patients with obesity; a mean number of 32 patients with type 2 diabetes were seen for every 100 patients with notably increased waist circumference. These numbers varied greatly between individual states.
Figure 3.
Regional prevalence of known type 2 diabetes (doctor’s diagnosis or medication) by federal state (prevalence); standardized according to (8)
Discussion
The results of the current study showed an average prevalence of obesity of 22.8% in primary care; wide variations existed between individual states (19.8% to 28.3%). In patients with normal weight or overweight, a substantial proportion had clearly increased waist circumference measurements according to the WHO definition. The overall prevalence of 36.5% for notably increased waist circumference was therefore higher than for obesity. A notable increase in prevalence was observed for both variables with increasing age. More men than women in all age groups were obese; women, however, in the mean had more often a notably increased waist circumference (threshold values >102 cm for men and >88 cm for women).
Representativeness was achieved by random selection of practices in all of Germany and the consecutive inclusion of patients on the study day. Further, targeted stratification was undertaken in order to be able to make valid statements about the group of younger patients that visit their doctors more rarely than older patients. Although important variables—such as the frequency of obesity, mean socioeconomic status, or the proportion of smokers—often corresponded with the result of population based studies (8), it was not the intention of this study to provide representative data for the total population but only to reflect the situation in primary health care.
Obesity data for Germany are available from various national health surveys (age range 25 to 69 years). Between 1985 and 2002, a notable increase in the age-adjusted prevalence of obesity was noted, of 39% in men (from 16.2% to 22.5%) and of 44% (from 16.2% to 23.3%) in women (1). The NVS II study is a more recent data source to estimate the population based prevalence of obesity (2006: men 20.5%, women 21.2%) (2). Further, results from two studies conducted in a primary care setting (HYDRA and DETECT) with respect to the prevalence of obesity were largely consistent with the results reported here (9, 10).
Data on the regional distribution of obesity can be found in NVS II (2). That study also found a higher obesity prevalence in Germany’s northeast (25.3% of men and 21.8% of women) than in the rest of the country. The data are comparable in detail to a limited degree only because they were aggregated for groups of federal states. In total, the prevalence of obesity was slightly higher in this study than in the NVS II study, which was being conducted simultaneously. This may be explained by the fact that obese people are likely to be overrepresented in a general practice’s population, owing to their comorbidities. More women than men use primary care. The average age is slightly higher than in the general population. However, we attempted to adjust for these differences in calculating standardized prevalence rates.
In recent years, waist circumference has increasingly become the predictor of an increased mortality and morbidity risk. It shows the pattern of fat distribution and identifies persons at increased cardiovascular risk better than the BMI (11, 12). The IDEA study has provided new data comparing primary care populations internationally (mean age 48.5 years, 18 to 80 years). The main prevalence of notably increased waist circumference in this study was 29% for men and 48% for women (cut-off >102/88 cm for men/women) (13). The results of the GEMCAS study (36% for men and 42% for women with a waist circumference >102/88 cm) add data from a mainly primary care cohort to these data. In contrast to the DETECT study, specialists such as cardiologists and diabetologists were excluded from participation because of the particular patient selection. To the authors’ knowledge, no published data have thus far been available on the regional distribution of increased waist circumference in Germany.
The observation that more men than women have a raised BMI, whereas more women than men have an increased waist circumference is surprising at first glance only. The explanation lies in the defined different threshold values that take into account the different physical proportions of men and women. The threshold value for notably increased waist circumference in women (>88 cm) was defined on the basis of a Scottish population. It does not reflect the absolute risk levels according to PROCAM or SCORE that are currently used to estimate cardiovascular risk (14).
The association between (especially abdominal) obesity and development of type 2 diabetes is well documented and in accordance with the current definition of the metabolic syndrome of the International Diabetes Federation (15). A moderately increased waist circumference is a crucial criterion for the diagnosis of metabolic syndrome. 50 patients with type 2 diabetes are seen in Germany for every 100 obese patients, and 32 patients with type 2 diabetes for every 100 patients with notably increased waist circumference (metabolic syndrome 86 and 54). Considerable regional differences exist with different relations of obesity/increased waist circumference and a diagnosis of type 2 diabetes or metabolic syndrome (data not shown). The reasons for this are unclear.
A series of cohort studies have shown the association between BMI and the risk of diabetes (16–18). About half of all new diagnoses of diabetes were made in persons with a BMI >30 kg/m2, and almost 20% have a BMI >35 kg/m2 at the time the diagnosis is made (17, 18). Especially abdominal obesity, as measured by waist circumference, is associated with insulin resistance. No strong association exists, however, between BMI and the prevalence of type 2 diabetes. A recently published study (19) found 13 persons with diabetes for every 100 overweight or obese persons in the US, 99/100 in India, 25/100 in the Philippines, 37/100 in Taiwan, 34/100 in Hong Kong, 19/100 in China, 28/100 in Singapore, 25/100 in Korea, and 34/100 in Thailand. The authors assume that genetic differences are the most likely cause of this variation in insulin resistance (19). The current study found differences for Germany in the prevalence of diabetes relative to overweight. Whether these differences reflect genetic variation or have other causes not investigated in this study cannot be answered. Exploratory analyses of the regional distribution of the metabolic syndrome (20) have shown that common traits (Baden-Württemberg) and clear differences both exist compared with type 2 diabetes.
Conclusion
The prevalence data reported here for obesity as defined by BMI and increased waist circumference show that relevant regional differences exist in Germany. This documentation provides a good basis for developing targeted regional intervention strategies. It was surprising in this context, however, that high rates of obesity in individual German states were not automatically associated with a corresponding increase in the number of persons with type 2 diabetes. The reasons for these regional differences have not been explained thus far and require further studies.
Acknowledgments
This investigator-initiated study was funded by Sanofi Aventis Deutschland GmbH in Berlin.
Translated from the original German by Dr Birte Twisselmann.
Footnotes
Conflict of interest statement
Professor Hauner has received speaker honoraria from Sanofi-Aventis, Lilly, Novartis, and Novo Nordisk, as well as study support from Sanofi-Aventis, Lilly, and Pfizer.
PD Dr Bramlage has received support for research and speaking from Sanofi-Aventis, Takeda, Daiichi, Sankyo, Novartis, Berlin-Chemie, Schwarz Pharma, and Medac.
Christian Lösch has received financial support for speaking from Sanofi-Aventis.
Professor Schunkert has received honoraria for speaking and advisory work from Sanofi-Aventis.
Professor Wasem has received third party funding from Sanofi-Aventis.
Professor Jöckel is conducting a number of third party funded projects and expert assessments at his institute on behalf of AstraZeneca, Sanofi-Aventis, Takeda Pharma, and other pharmaceuticals manufacturers.
PD Dr Moebus has received speaker honoraria from Sanofi-Aventis.
References
- 1.Helmert U, Strube H. Die Entwicklung der Adipositas in Deutschland im Zeitraum von 1985 bis 2002. Gesundheitswesen. 2004;66:409–415. doi: 10.1055/s-2004-813324. [DOI] [PubMed] [Google Scholar]
- 2.Max Rubner Institut. Nationale Verzehrs-Studie II. www.was-esse-ich.de/uploads/media/NVS_II_Ergebnisbericht_Teil_1.pdf.
- 3.Prugger C, Keil U. Entwicklung der Adipositas in Deutschland - Größenordnung, Determinanten und Perspektiven. Dtsch Med Wochenschr. 2007;132:892–897. doi: 10.1055/s-2007-973636. [DOI] [PubMed] [Google Scholar]
- 4.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999-2000. JAMA. 2002;288:1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Obesity - preventing and managing the global epidemic. Geneva: WHO Technical Report; 2000. Series 894. [PubMed] [Google Scholar]
- 6.Moebus S, Hanisch JU, Aidelsburger P, Bramlage P, Wasem J, Jöckel K-H. Impact of four different definitions used for assessment of the prevalence of metabolic syndrome in a primary health care setting. The German Metabolic and Cardiovascular Risk Project (GEMCAS) Cardiovasc Diabetol. 2007;6 doi: 10.1186/1475-2840-6-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moebus S, Hanisch JU, Neuhäuser M, Aidelsburger P, Wasem J, Jöckel K-H. Assessing the metabolic syndrome according to NCEP ATP III in Germany: feasibility of a two step approach in 1 550 randomly selected primary health care practices. GMS. 2006;4 Doc7 (20061009) [PMC free article] [PubMed] [Google Scholar]
- 8.Statistisches Bundesamt. Statistisches Jahrbuch für die Bundesrepublik Deutschland. Wiesbaden: Statistisches Bundesamt; 2006. www-ec.destatis.de. [Google Scholar]
- 9.Bramlage P, Wittchen HU, Pittrow D, et al. Recognition and management of overweight and obesity in primary care in Germany. Int J Obes Relat Metab Disord. 2004;28:1299–1308. doi: 10.1038/sj.ijo.0802752. [DOI] [PubMed] [Google Scholar]
- 10.Wittchen HU, Glaesmer H, Marz W, et al. Cardiovascular risk factors in primary care: methods and baseline prevalence rates - the DETECT program. Curr Med Res Opin. 2005;21:619–630. doi: 10.1185/030079905X38187. [DOI] [PubMed] [Google Scholar]
- 11.Hauner H, Bramlage P, Lösch C, et al. Prevalence of Obesity in Primary Care using different Anthropometric Measures - Results of the German Metabolic and Cardiovascular Risk Project (GEMCAS) BMC Public Health. 2008;8 doi: 10.1186/1471-2458-8-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yusuf S, Hawken S, Ounpuu S, et al. Obesity and the risk of myocardial infarction in 27.000 participants from 52 countries: a case-control study. Lancet. 2005;366:1640–1652. doi: 10.1016/S0140-6736(05)67663-5. [DOI] [PubMed] [Google Scholar]
- 13.Balkau B, Deanfield JE, Despres JP, et al. International Day for the Evaluation of Abdominal Obesity (IDEA): a study of waist circumference, cardiovascular disease, and diabetes mellitus in 168,000 primary care patients in 63 countries. Circulation. 2007;116:1942–1951. doi: 10.1161/CIRCULATIONAHA.106.676379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schunkert H, Moebus S, Hanisch J, et al. The correlation between waist circumference and ESC cardiovascular risk score: data from the German metabolic and cardiovascular risk project (GEMCAS) Clin Res Cardiol. 2008;97:827–835. doi: 10.1007/s00392-008-0694-1. [DOI] [PubMed] [Google Scholar]
- 15.Alberti KG, Zimmet P, Shaw J. The metabolic syndrome - a new worldwide definition. Lancet. 2005;366:1059–1062. doi: 10.1016/S0140-6736(05)67402-8. [DOI] [PubMed] [Google Scholar]
- 16.Ford ES, Williamson DF, Liu S. Weight change and diabetes incidence: findings from a national cohort of US adults. Am J Epidemiol. 1997;146:214–222. doi: 10.1093/oxfordjournals.aje.a009256. [DOI] [PubMed] [Google Scholar]
- 17.Leibson CL, Williamson DF, Melton LJ, et al. Temporal trends in BMI among adults with diabetes. Diabetes Care. 2001;24:1584–1589. doi: 10.2337/diacare.24.9.1584. [DOI] [PubMed] [Google Scholar]
- 18.Burke JP, Williams K, Narayan KM, Leibson C, Haffner SM, Stern MP. A population perspective on diabetes prevention: whom should we target for preventing weight gain? Diabetes Care. 2003;26:1999–2004. doi: 10.2337/diacare.26.7.1999. [DOI] [PubMed] [Google Scholar]
- 19.Yoon KH, Lee JH, Kim JW, et al. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368:1681–1688. doi: 10.1016/S0140-6736(06)69703-1. [DOI] [PubMed] [Google Scholar]
- 20.Moebus S, Hanisch J, Bramlage P, et al. Regional Differences in the Prevalence of the Metabolic Syndrome in Primary Care Practices in Germany. Dtsch Arztebl Int. 2008;105(12):207–213. doi: 10.3238/artzebl.2008.0207. [DOI] [PMC free article] [PubMed] [Google Scholar]