INTRODUCTION
Thromboembolic disease is associated with significant mortality and morbidity, especially in hospitalized patients. Without thromboprophylaxis, the risk of deep-vein thrombosis (DVT) in hospitalized patients is 10% to 40% in medical and general surgical patients and 40% to 60% in patients undergoing orthopedic surgery.1 Adverse consequences of unrecognized, untreated, or inadequately treated venous thromboembolism (VTE) include an increased risk of symptomatic DVT or pulmonary embolism (PE), fatal PE, increased hospital expenditures, and an increased risk of chronic post-thrombotic syndrome.1 Prophylaxis and proper management with an appropriate anticoagulant can reduce these risks.
Current pharmacological options for the management and prevention of VTE are associated with several limitations and produce their anticoagulation effects at various points in the coagulation cascade. Unfractionated heparin (UFH) indirectly inhibits factors IIa, IXa, Xa, XIa, and XIIa by forming a complex with antithrombin and initiating its activity. Low-molecular-weight heparins (LMWHs) inhibit thrombin generation by a mechanism similar to that of UFH, but they have a stronger affinity for factor Xa than for factor IIa. Limitations of UFH and LMWHs include their ability to induce immune-mediated platelet activation, which can lead to heparin-induced thrombocytopenia (HIT), the need for frequent laboratory monitoring (with UFH only), adverse effects on bone metabolism, and a potential for increased serum transaminases.2
Although GlaxoSmithKline’s anticoagulant fondaparinux (Arixtra) selectively inhibits factor Xa, antithrombin is required as a cofactor to produce its effect. Direct thrombin inhibitors, such as argatroban (GlaxoSmithKline), lepirudin (Refludan, Bayer), and bivalirudin (Angiomax, The Medicines Company), bind directly to thrombin to produce their effect. These agents have a narrow therapeutic index and a short half-life. They must be given as a continuous infusion, thereby making this an unreasonable option for outpatients.2 These agents are also expensive and are available only as injectables that must be administered parenterally.
The only orally available agent for the long-term management of thromboembolic disease in the U.S. is warfarin (Coumadin, Bristol-Myers Squibb). Warfarin inhibits factors II, VII, IX, and X by blocking vitamin K–mediated carboxylation of their precursors.3 Although warfarin is effective in managing and preventing thromboembolic disease over time, its variable pharmacokinetics, its significant potential for drug interactions, its slow onset of effect, and a patient’s genetic factors contribute to its unpredictable response, thus requiring close monitoring for dose initiation and adjustments. Therefore, there is a need for a safe and effective anticoagulant with a predictable pharmacokinetic profile without the need for frequent laboratory monitoring.
Factor Xa is generated via the intrinsic and extrinsic pathways and is the rate-limiting step in the propagation of thrombin generation. Studies with fondaparinux have shown that factor Xa inhibition provides effective thromboprophylaxis. Rivaroxaban (Xarelto, Bayer) is an oral direct factor Xa inhibitor currently being evaluated in phase 3 clinical trials. This article reviews the pharmacology, pharmacokinetics, clinical efficacy, and safety data for this agent.
PHARMACOLOGY
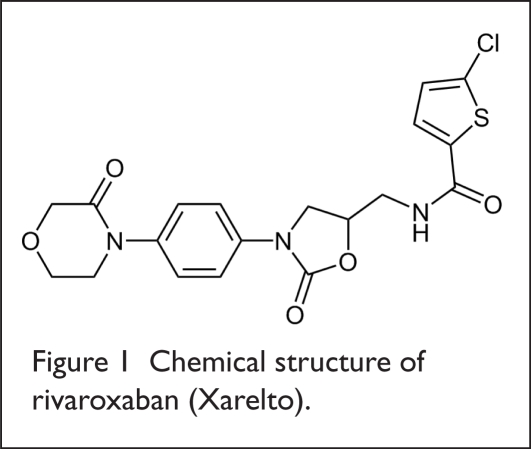
The chemical structure of rivaroxaban is depicted in Figure 1.
Figure 1.
Chemical structure of rivaroxaban (Xarelto).
Rivaroxaban produces its anticoagulant effects by directly, selectively, and reversibly inhibiting free and clot-bound factor Xa without binding to antithrombin.4 Inhibition of factor Xa prevents the conversion of factor II to factor IIa, resulting in decreased generation of thrombin. Rivaroxaban is 100,000-fold more selective for factor Xa than other biological proteases, such as thrombin, plasmin, factor VIIa, factor IXa, and activated protein C.5
Pharmacodynamics
In studies published in 2005, rivaroxaban at doses of 5 to 80 mg resulted in dose-dependent inhibition of factor Xa activity from 20% to 61%, with a maximum inhibition of factor Xa occurring one to four hours after administration; these effects lasted for five to 12 hours.4,6 Rivaroxaban also caused a prolonged prothrombin time (PT) and activated partial thromboplastin time (aPTT) in a dose-dependent manner.6 The maximum prolongation of PT was 1.3 to 2.6 times the baseline value;5 the maximum aPTT prolongation was approximately 1.5-fold from baseline;6 and the maximum prolongation of PT and aPTT was reached within one to four hours after administration of rivaroxaban.4
The pharmacodynamic properties of rivaroxaban are summarized in Table 1.
Table 1.
Pharmacodynamic Properties of Rivaroxaban
| Variable | Value |
|---|---|
| Factor Xa activity inhibitory effect* | 20%–61% |
| Time to maximum factor Xa inhibition | 1–4 hours |
| Duration of factor Xa inhibition | 5–12 hours |
| Maximum PT prolongation† | 1.3–2.6 times baseline |
| Maximum aPTT prolongation | 1.5 times baseline |
| Time to maximum PT and aPTT prolongation | 1–4 hours |
Based on single doses ranging from 5 mg to 80 mg.
Based on doses ranging from 5 mg to 30 mg twice daily.
PT = prothrombin time; aPTT = activated partial thromboplastin time.
Pharmacokinetics
Rivaroxaban is absorbed rapidly and almost completely after oral administration. Peak plasma concentrations are achieved within one to four hours, and bioavailability is 60% to 80%.4,6,7 Food appears to decrease the rate of absorption and to increase maximum rivaroxaban concentrations. The drug’s volume of distribution is approximately 1.36 L/kg. Approximately 90% of the agent is protein-bound.5,8
Rivaroxaban is metabolized hepatically by cytochrome P450 isoenzyme 3A4. The drug is excreted rapidly via a combination of renal elimination and the fecal and biliary route. Approximately 14% to 31% of rivaroxaban is excreted unchanged in the urine.5,7 The drug’s elimination half-life, at doses ranging from 5 mg daily to 30 mg twice daily, is five to nine hours.4,7
When administered to patients older than 75 years of age, patients with renal insufficiency (a creatinine clearance below 50 mL/minute), patients with low body weight (below 50 kg), and patients with moderate hepatic disease (Child-Pugh class B), rivaroxaban was associated with decreased renal clearance, a higher area-under-the-curve (AUC) concentration, and increased factor Xa inhibition, suggesting that dosage adjustments might be necessary for these patients.5,7–10
The pharmacokinetic parameters of rivaroxaban are summarized in Table 2.
Table 2.
Pharmacokinetic Properties of Rivaroxaban
| Variable | Value |
|---|---|
| Administration | Oral |
| Peak plasma concentration | 1–4 hours |
| Bioavailability | 60%–80% |
| Volume of distribution | 1.36 L/kg |
| Protein binding | Approx. 90% |
| Metabolism | Cytochrome P450 3A4 system |
| Clearance | Renal and fecal-biliary |
| Half-life | 5 to 9 hours |
| Monitoring | Signs and symptoms of bleeding |
| Liver enzymes |
CLINICAL TRIALS
Phase 2 Studies
Eriksson et al.11
Eriksson and colleagues conducted a randomized, open-label, active-comparator-controlled, multinational, dose-escalation phase 2a study with the goal of establishing a dose–response relationship for efficacy and safety of rivaroxaban in comparison to enoxaparin (Lovenox, Sanofi-Aventis). Patients scheduled for total hip replacement surgery, men 18 years of age or older, and postmenopausal women were eligible to enroll. Patients (n = 641) received oral rivaroxaban or subcutaneous (SQ) enoxaparin. Rivaroxaban was initiated six to eight hours after wound closure and was given either every 12 hours at doses of 2.5 mg, 5 mg, 10 mg, 20 mg, or 30 mg or every 24 hours at a dose of 30 mg. Enoxaparin was initiated the evening before surgery, followed by a second dose six to eight hours after wound closure and daily thereafter, at a dose of 40 mg. Therapy was continued for five to nine days after surgery.
The primary endpoint of the study was the composite of any DVT, nonfatal PE, and all-cause mortality. Secondary endpoints included major VTE and the incidence of symptomatic VTE. The primary safety endpoint was major bleeding beginning at least four hours after the end of surgery or after the first intake of study drug.
Of the 641 patients enrolled, 76% were included in the per-protocol analysis. The primary efficacy endpoint was observed in 22.2%, 23.8%, 20%, 10.2%, 17.4%, and 15.1% of patients assigned to rivaroxaban 2.5 mg, 5 mg, 10 mg, 20 mg, 30 mg twice daily, and 30 mg daily, respectively.
The primary efficacy endpoint occurred in 16.8% of patients in the comparator group. The difference in occurrence of the primary endpoint was not statistically significant (P = 0.504). The incidence of major VTE ranged from 0% to 11.1% in the rivaroxaban patients compared with 4.7% in the enoxaparin group.
Three patients experienced PE, one patient experienced symptomatic DVT, and three patients died. All of these events occurred in patients receiving rivaroxaban. The incidence of major VTE decreased with increasing rivaroxaban doses in a dose-dependent manner (P = 0.0108). Major bleeding occurred in 0% to 10.8% of patients receiving rivaroxaban and in none of the patients receiving enoxaparin.
There was a statistically significant dose–response relationship between the rivaroxaban dosage and major bleeding (P = 0.0008). Elevations in alanine aminotransferase (ALT) and aspartate aminotransferase (AST) to more than three times the upper limit of normal (ULN) were documented in 4% and 2% of patients receiving rivaroxaban and in 4.6% and 2% of patients receiving enoxaparin.
The authors concluded that rivaroxaban was effective in reducing the incidence of VTE in patients undergoing total hip replacement.
The ODIXa–KNEE Trial12
Turpie and colleagues conducted a double-dummy, double-blind, randomized, parallel-group, dose-ranging study to compare the efficacy and safety of rivaroxaban with that of enoxaparin in preventing VTE following total knee replacement. A total of 621 patients received rivaroxaban 2.5 mg, 5 mg, 10 mg, 20 mg, or 30 mg twice daily starting six to eight hours after wound closure and every 12 hours thereafter, or enoxaparin 30 mg subcutaneously every 12 hours starting on the morning following the procedure. Treatment was continued for five to nine days.
The primary efficacy endpoint was the composite of the incidence of proximal and/or distal DVT, confirmed nonfatal PE, and all-cause mortality. The primary safety endpoint was major postoperative bleeding.
The incidence of the primary endpoint was 23.3% to 40.4% in the rivaroxaban patients and 44.3% in the enoxaparin patients. Major VTE events ranged from 0% to 6.7% of patients receiving rivaroxaban and in 4.3% of patients treated with enoxaparin.
The incidence of major postoperative bleeding was 0% to 7.5% for rivaroxaban and 1.9% for enoxaparin. The incidence of bleeding with rivaroxaban increased in a dose-dependent manner. The difference in the incidence of bleeding between any of the rivaroxaban dosage groups and enoxaparin was not statistically significant. The incidence of non-major bleeding was similar for the study drug and for enoxaparin.
The authors concluded that twice-daily rivaroxaban was as effective as enoxaparin in thromboprophylaxis following total knee replacement.
The ODIXa–Deep-Vein Thrombosis Trial13
Treatment of Proximal Deep-Vein Thrombosis with the Oral Direct factor Xa Inhibitor Rivaroxaban (ODIXa–DVT) was a randomized, parallel-group, partially blinded, phase 2, dose-finding trial that aimed to compare the efficacy of rivaroxaban with standard therapy for patients with acute proximal DVT. Patients (n = 613) with acute symptomatic DVT were assigned to one of five study groups: rivaroxaban 10 mg orally twice daily (n = 119), rivaroxaban 20 mg orally twice daily (n = 117), rivaroxaban 30 mg twice daily (n = 121), rivaroxaban 40 mg once daily (n = 126), and enoxaparin 1 mg/kg twice daily given by SQ injection, followed by a subsequent dose of a vitamin K antagonist (n = 126). Treatment continued for 12 weeks.
Patients were enrolled if they were at least 18 years of age, had no symptoms of PE, had not received a vitamin K antagonist, and had received, at most, 36 hours of treatment with UFH or LMWHs. The primary outcome was improvement in thrombotic burden, defined by a reduction of greater than 4 points in the thrombus score, as measured by Complete Compression Ultrasound (CCUS) at day 21, in the absence of extension or recurrence of DVT, symptomatic PE, or death related to thromboembolism.
The primary efficacy outcome was observed in 53%, 59.2%, 56.9%, and 43.8% of patients receiving rivaroxaban 10 mg, 20 mg, and 30 mg twice daily and 40 mg daily, respectively, and in 45.9% of the patients receiving standard therapy (P = 0.67). Bleeding was observed in 1.7%, 1.7%, 3.3%, and 1.7% of patients receiving twice-daily rivaroxaban 10 mg, 20 mg, 30 mg, and 40 mg daily, respectively, and 0% in the standard treatment group (P = 0.39). Elevations in ALT levels to more than three times the ULN occurred in 1.9% to 4.3% of the rivaroxaban patients and in 21.6% of the standardtherapy group.
Rivaroxaban was judged to be as effective and safe as standard therapy for acute proximal DVT, irrespective of the dose.
The ODIXa–HIP Trial14
Once-Daily, Oral, Direct Factor Xa Inhibitor, Rivaroxaban, for Thromboprophylaxis after Total Hip Replacement (ODIXa–HIP) was a randomized, double-blind, double-dummy, active-comparator-controlled, multinational, dose-ranging study conducted to evaluate the safety and efficacy of rivaroxaban once daily for preventing thrombosis following total hip replacement.
Men at least 18 years of age and post-menopausal women (n = 873) received rivaroxaban 5 mg, 10 mg, 20 mg, 30 mg, or 40 mg initiated six to eight hours after wound closure and administered daily thereafter. Enoxaparin SQ was given the evening before surgery, followed by 40 mg daily starting six to eight hours after wound closure. Treatment was continued for five to nine days.
The primary efficacy endpoint was the composite of the incidence of any DVT, PE, and all-cause mortality. Secondary endpoints were major VTE and symptomatic VTE. The primary safety outcome was the incidence of major bleeding. The primary efficacy analysis was performed on the per-protocol population (618 patients).
The difference in the primary efficacy endpoint between the rivaroxaban and enoxaparin groups was not statistically significant (P = 0.0852). The primary endpoint occurred in 14.9%, 10.6%, 8.5%, 13.5%, 6.4%, and 25.2% of patients receiving rivaroxaban 5 mg, 10 mg, 20 mg, 30 mg, 40 mg daily and enoxaparin, respectively. The observed incidence in the secondary endpoints was similar between rivaroxaban and enoxaparin.
Major postoperative bleeding occurred in 2.3%, 0.7%, 4.3%, 4.9%, and 5.1% of patients receiving rivaroxaban 5 mg, 10 mg, 20 mg, 30 mg, and 40 mg daily, respectively, compared with 1.9% of patients receiving enoxaparin. The difference in bleeding rates between rivaroxaban patients and enoxaparin patients was statistically significant (P = 0.0391). The difference in bleeding rates between any rivaroxaban dose and enoxaparin was not statistically significant; however, the study was not powered to evaluate this endpoint. Increases in ALT or AST to more than three times the ULN occurred in 3% to 6.2% of rivaroxaban patients and in 7.1% of enoxaparin patients.
The efficacy and safety profile of once-daily rivaroxaban was considered to be similar to that of enoxaparin.
The Einstein–Deep-Vein Thrombosis Dose-Ranging Study15
Einstein–DVT was a multicenter, randomized, dose-ranging study that compared the efficacy of once-daily rivaroxaban in patients with acute symptomatic DVT. A total of 543 patients were assigned to one of four treatment groups: rivaroxaban 20 mg, 30 mg, or 40 mg or conventional treatment. Standard therapy consisted of a vitamin K antagonist in combination with one of the following regimens: UFH at an initial bolus of 5,000 IU, followed by an infusion of 1,250 IU/hour; tinzaparin (Innohep, Pharmion) 175 IU/kg SQ daily; or enoxaparin 1.5 mg/kg SQ daily or 1 mg/kg SQ twice a day. This study was double-blinded for the rivaroxaban doses and open-label for the conventional-treatment arm. Patients were treated for 12 weeks.
The primary efficacy outcome was the composite of symptomatic recurrent DVT, symptomatic fatal or nonfatal PE, and asymptomatic deterioration in thrombotic burden. The individual components of the primary efficacy outcome were considered secondary efficacy outcomes.
The primary safety outcome was the composite of major and clinically relevant, but nonmajor, bleeding up to 48 hours after discontinuation of treatment. Any bleeding, all-cause mortality, and the individual components of the primary safety outcome were considered secondary safety outcomes.
The study results were based on the per-protocol population, which consisted of 449 patients. The primary outcome occurred in 6.1%, 5.4%, and 6.6% of the patients assigned to rivaroxaban 20 mg, 30 mg, and 40 mg, respectively, and in 9.9% of the patients assigned to conventional therapy. The incidence of symptomatic DVT ranged from 0% to 1.8% in the rivaroxaban patients and was 6.9% in the conventional-therapy group.
Asymptomatic deterioration in thrombotic burden was noted in 1.8% to 5% of rivaroxaban patients and in 3% of those managed with conventional therapy. The primary safety outcome occurred in 5.9%, 6%, and 2.2% in the patients receiving rivaroxaban 20 mg, 30 mg, and 40 mg, respectively, and in 8.8% of the conventional-therapy patients.
The authors concluded that the safety and efficacy profile of rivaroxaban was similar to that of conventional therapy.
Phase 3 Studies
RECORD 116
Regulation of Coagulation in Orthopedic Surgery to Prevent Deep Venous Thrombosis and Pulmonary Embolism 1 (RECORD 1) was a randomized, multinational, double-blind study to evaluate the efficacy and safety of rivaroxaban in thromboprophylaxis after total hip arthroplasty.
A total of 4,541 patients were assigned to receive either 10 mg of rivaroxaban orally daily (n = 2,266) or SQ enoxaparin 40 mg daily (n = 2,275). Rivaroxaban was initiated six to eight hours after wound closure. Enoxaparin was initiated 12 hours before surgery and was restarted six to nine hours after wound closure.
All patients older than 18 years of age who were scheduled for an elective total hip arthroplasty were eligible to participate in the trial. Patients were treated for 35 days following the procedure.
The primary efficacy outcome was a composite of DVT, nonfatal PE, or death from any cause up to 36 days. The secondary efficacy outcomes were major VTE, the incidence of symptomatic VTE, and death. The primary safety outcome was major bleeding.
The modified intent-to-treat analysis, which consisted of 3,153 patients (69.4%), reported the incidence of the primary outcome as 1.1% with rivaroxaban and as 3.7% with enoxaparin (P < 0.001). The incidence of major VTE was reported as 0.2% with rivaroxaban and as 2% with enoxaparin (P < 0.001). There was no statistically significant difference in bleeding rates between the two groups: 6% for rivaroxaban and 5.9% for enoxaparin (P = 0.94). Major bleeding occurred in 0.3% of rivaroxaban patients and in 0.1% of enoxaparin patients (P < 0.18).
The trial indicated that once-daily oral rivaroxaban was safe and effective in extended thromboprophylaxis following total hip arthoplasty.
RECORD 217
Regulation of Coagulation in Orthopedic Surgery to Prevent Deep-Vein Thrombosis and Pulmonary Embolism 2 (RECORD 2) was a randomized, multinational, double-blind, double-dummy study that aimed to compare the efficacy and safety of long-term treatment with rivaroxaban with short-term enoxaparin after total hip arthroplasty. As in RECORD 1, all patients 18 years of age or older who were scheduled for an elective total hip arthroplasty were eligible to enroll in the trial.
A total of 2,509 patients received either 10 mg of rivaroxaban orally once daily, continued for 31 to 39 days, or SQ enoxaparin 40 mg once daily, continued for 10 to 14 days. Time frames were the same as in RECORD 1 (rivaroxaban initiated six to eight hours after wound closure, enoxaparin initiated 12 hours before surgery and restarted six to nine hours after wound closure).
The primary efficacy outcome was the composite of any DVT, nonfatal PE, and all-cause mortality up to days 30 to 42. Secondary outcomes included major VTE, the incidence of DVT, the incidence of symptomatic VTE, and death. Major bleeding was considered to be the main safety outcome.
Rivaroxaban was associated with a statistically significantly decreased incidence of the primary efficacy outcome: 2% with rivaroxaban and 9.3% with enoxaparin (P < 0.0001). The incidence of major VTE was also lower in the rivaroxaban patients than in the enoxaparin group (0.6% vs. 5.1%; P < 0.0001).
The incidence of on-treatment bleeding was higher with rivaroxaban (6.6%) than with enoxaparin (5.5%), however, this difference was not statistically significant (P = 0.25). The incidence of major bleeding was less than 0.1% in both treatment groups.
Only 1.6% of the patients receiving extended thromboprophylaxis with rivaroxaban experienced ALT elevations greater than three times the ULN. All elevations were resolved by the final follow-up visit. With a shorter duration of treatment, 4.7% of enoxaparin patients experienced the same elevation in ALT levels.
In summary, extended thromboprophylaxis with rivaroxaban was judged as more effective, with a similar safety profile, compared with short-term thromboprophylaxis with enoxaparin in patients who underwent total hip arthoplasty.
RECORD 318
Rivaroxaban versus Enoxaparin for Thromboprophylaxis after Total Knee Arthroplasty (RECORD 3) was a randomized, multinational, double-blind, double-dummy, active-control study designed to compare the non-inferiority and superiority of rivaroxaban with that of enoxaparin for thromboprophylaxis after total knee arthroplasty.
A total of 2,531 patients received either 10 mg of oral rivaroxaban once daily (n = 1,254) or 40 mg of SQ enoxaparin once daily (n = 1,277). Patients in both arms continued therapy for at least 11 days.
All patients age 18 years of age or older who were scheduled for an elective knee arthroplasty were eligible for enrollment. The primary efficacy outcome included a composite of DVT, nonfatal PE, or death from any cause 13 to 17 days after surgery. Secondary efficacy outcomes included major VTE, the incidence of DVT, symptomatic VTE, and death. The primary safety outcome was major bleeding.
The primary efficacy outcome was obser ved in 9.6% of the rivaroxaban patients and in 18.9% of the enoxaparin patients (P < 0.001). Major VTE occurred in 1% of the patients receiving rivaroxaban and in 2.6% of the patients receiving enoxaparin (P = 0.002). Major bleeding occurred in 0.6% of patients receiving rivaroxaban and in 0.5% of patients receiving enoxaparin (P = 0.77).
Oral, once-daily rivaroxaban was considered safe and effective in the thromboprophylaxis of patients undergoing total knee arthroplasty.
SAFETY AND TOLERABILITY
Adverse Drug Effects
The most commonly reported adverse effects of rivaroxaban were bleeding and elevated liver enzymes ALT and AST. At doses used in phase 3 clinical trials (10 mg daily), the frequency of major bleeding ranged from below 0.1% to 0.7% with rivaroxaban and from less than 0.1% to 1.9% with enoxaparin.14,16–18 Elevated ALT and AST levels were reported as 1.6% to 3.8% in patients taking rivaroxaban and at 1.6% to 7.1% in patients receiving enoxaparin.12,14,16–18 These differences in bleeding rates and increases in serum transaminases were not statistically significant.
Additional adverse effects that were documented in phase 1 clinical trials included headache, diarrhea, fatigue, flatulence, and dizziness.4 The frequency of these findings was similar to that for the comparator groups.
Drug Interactions
Data on drug interactions with rivaroxaban are limited. Coadministration of digoxin (Lanoxin, GlaxoSmithKline), naproxen (e.g., Naprosyn, Roche) aspirin, clopidogrel (Plavix, Bristol-Myers Squibb/Sanofi-Aventis), or abciximab (ReoPro, Centocor/Lilly) has not been shown to significantly affect the pharmacokinetic or pharmacodynamic properties of rivaroxaban.8,19,20 Given the protein-binding properties of rivaroxaban, it may interact with other highly protein-bound agents, although studies to support this are lacking.8
DOSAGE AND ADMINISTRATION
The dose of rivaroxaban that was used in phase 3 trials for thromboprophylaxis following total hip and total knee arthoplasty was 10 mg orally once daily. Extrapolating from pharmacokinetic studies, dosage adjustments might be needed for elderly patients, patients with renal insufficiency or moderate-to-severe hepatic disease, and patients weighing less than 50 kg.5,7–10
COST
In Britain and Germany, the price of rivaroxaban is on a par with enoxaparin The cost is approximately 4.50 pounds ($7.96) per day in Britain.21 Rivaroxaban is still undergoing review in the U.S. The FDA is expected to make a decision on approval by May 28.22
CONCLUSION
Rivaroxaban is a direct, selective, reversible factor Xa inhibitor that is well tolerated when taken orally once daily for preventing thromboembolism following total hip or knee replacement. The drug has been well tolerated in clinical trials. The most commonly reported adverse effect has been bleeding; however, the frequency of bleeding associated with rivaroxaban was similar in the comparator group.
Rivaroxaban appears to have a low potential for drug interactions. The efficacy and long-tem safety of rivaroxaban are being evaluated in ongoing clinical trials to observe the drug’s effects in managing acute PE, preventing stroke in patients with atrial fibrillation, and managing acute coronary syndromes.
Footnotes
Disclosure: The authors have no financial conflicts of interest to report in regard to this article.
REFERENCES
- 1.Geerts WH, Bergqvist D, Pineo GF, et al. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines, 8th ed. Chest. 2008;133(6 Suppl):381S–453S. doi: 10.1378/chest.08-0656. [DOI] [PubMed] [Google Scholar]
- 2.Hirsh J, Bauer KA, Donati MB, et al. Parenteral anticoagulants: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines, 8th ed. Chest. 2008;133(6 Suppl):141S–159S. doi: 10.1378/chest.08-0689. [DOI] [PubMed] [Google Scholar]
- 3.Ansell J, Hirsh J, Hylek E, et al. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines, 8th ed. Chest. 2008;133(6 Suppl):160S–198S. doi: 10.1378/chest.08-0670. [DOI] [PubMed] [Google Scholar]
- 4.Kubitza D, Becka M, Wensing G, et al. Safety, pharmacodynamics, and pharmacokinetics of BAY 59-7939—an oral, direct factor Xa inhibitor—after multiple dosing in healthy male subjects. Eur J Clin Pharmacol. 2005;61(12):873–880. doi: 10.1007/s00228-005-0043-5. [DOI] [PubMed] [Google Scholar]
- 5.Gulseth MP, Michaud J, Nutescu EA. Rivaroxaban: An oral direct inhibitor of factor Xa. Am J Health Syst Pharm. 2008;65(16):1520–1529. doi: 10.2146/ajhp070624. [DOI] [PubMed] [Google Scholar]
- 6.Kubitza D, Becka M, Voith B, et al. Safety, pharmacodynamics, and pharmacokinetics of single doses of BAY 59-7939, an oral, direct factor Xa inhibitor. Clin Pharmacol Ther. 2005;78(4):412–421. doi: 10.1016/j.clpt.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 7.Mueck W, Borris LC, Dahl OE, et al. Population pharmacokinetics and pharmacodynamics of once- and twice-daily rivaroxaban for the prevention of venous thromboembolism in patients undergoing total hip replacement. Thromb Haemost. 2008;100(3):453–461. [PubMed] [Google Scholar]
- 8.Abrams PJ, Emerson CR. Rivaroxaban: A novel, oral, direct factor Xa inhibitor. Pharmacotherapy. 2009;29(2):167–181. doi: 10.1592/phco.29.2.167. [DOI] [PubMed] [Google Scholar]
- 9.Halabi A, Maatouk H, Klause N, et al. Effects of renal impairment on the pharmacology of rivaroxaban (BAY 59-7939), an oral, direct, factor Xa inhibitor. Annual Meeting of the American Society of Hematology (Abstracts) Blood 2006. 16; 10811913 [Google Scholar]
- 10.Kubitza D, Becka M, Mueck W, Zuehlsdorf M. The effect of extreme age, and gender, on the pharmacology and tolerability of rivaroxaban, an oral, direct factor Xa inhibitor. Annual Meeting of the American Society of Hematology (Abstracts) Blood. 2006;108(11):905. [Google Scholar]
- 11.Eriksson BI, Borris LC, Dahl OE, et al. Dose-escalation study of rivaroxaban (BAY 59-7939)—an oral, direct factor Xa inhibitor—for the prevention of venous thromboembolism in patients undergoing total hip replacement. Thromb Res. 2007;120(5):685–693. doi: 10.1016/j.thromres.2006.12.025. [DOI] [PubMed] [Google Scholar]
- 12.Turpie AG, Fisher WD, Bauer KA, et al. BAY 59-7939: An oral, direct factor Xa inhibitor for the prevention of venous thromboembolism in patients after total knee replacement: A phase II dose-ranging study. J Thromb Haemost. 2005;3(11):2479–2486. doi: 10.1111/j.1538-7836.2005.01602.x. [DOI] [PubMed] [Google Scholar]
- 13.Agnelli G, Gallus A, Goldhaber SZ, et al. Treatment of proximal deep-vein thrombosis with the oral direct factor Xa inhibitor rivaroxaban (BAY 59-7939): The ODIXa–DVT (oral direct factor Xa inhibitor BAY 59-7939 in patients with acute symptomatic deep-vein thrombosis) study. Circulation. 2007;116(2):180–187. doi: 10.1161/CIRCULATIONAHA.106.668020. [DOI] [PubMed] [Google Scholar]
- 14.Eriksson BI, Borris LC, Dahl OE, et al. A once-daily, oral, direct factor Xa inhibitor, rivaroxaban (BAY 59-7939), for thromboprophylaxis after total hip replacement. Circulation. 2006;114(22):2374–2381. doi: 10.1161/CIRCULATIONAHA.106.642074. [DOI] [PubMed] [Google Scholar]
- 15.Buller HR, Lensing AW, Prins MH, et al. A dose-ranging study evaluating once-daily oral administration of the factor Xa inhibitor rivaroxaban in the treatment of patients with acute symptomatic deep vein thrombosis: The Einstein–DVT Dose-Ranging Study. Blood. 2008;112(6):2242–2247. doi: 10.1182/blood-2008-05-160143. [DOI] [PubMed] [Google Scholar]
- 16.Eriksson BI, Borris LC, Friedman RJ, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after hip arthroplasty. N Engl J Med. 2008;358(26):2765–2775. doi: 10.1056/NEJMoa0800374. [DOI] [PubMed] [Google Scholar]
- 17.Kakkar AK, Brenner B, Dahl OE, et al. Extended duration rivaroxaban versus short-term enoxaparin for the prevention of venous thromboembolism after total hip arthroplasty: A double-blind, randomised controlled trial. Lancet. 2008;372(9632):31–39. doi: 10.1016/S0140-6736(08)60880-6. [DOI] [PubMed] [Google Scholar]
- 18.Lassen MR, Ageno W, Borris LC, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty. N Engl J Med. 2008;358(26):2776–2786. doi: 10.1056/NEJMoa076016. [DOI] [PubMed] [Google Scholar]
- 19.Kubitza D, Becka M, Mueck W, Zuehlsdorf M. Rivaroxaban (BAY 59-7939)—an oral, direct factor Xa inhibitor—has no clinically relevant interaction with naproxen. Br J Clin Pharmacol. 2007;63(4):469–476. doi: 10.1111/j.1365-2125.2006.02776.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kubitza D, Becka M, Mueck W, Zuehlsdorf M. Safety, tolerability, pharmacodynamics, and pharmacokinetics of rivaroxaban—an oral, direct factor Xa inhibitor—are not affected by aspirin. J Clin Pharmacol. 2006;46(9):981–990. doi: 10.1177/0091270006292127. [DOI] [PubMed] [Google Scholar]
- 21.Update 1. Bayer launches Xarelto in EU: Cost matches Lovenox. Reuters, October 2, 2008.
- 22.FDA panel votes on anticlotting drug Xarelto and other health news. U.S. News & World Report, April 16, 2009. [Google Scholar]