Abstract
Objective
The purpose of this study was to perform a systematic review of the literature and other authoritative sources for recommendations regarding the appropriateness of physical and sporting activity for those with scoliosis.
Methods
The literature was systematically searched in PubMed, the Cumulative Index to Nursing and Allied Health Literature, the Index to Chiropractic Literature, and the National Guidelines Clearinghouse from the earliest date of each database through July 2008. All languages and research designs were included. Web sites of respected organizations were searched for position/white papers on scoliosis and physical activity. Included articles were rated using the Oxford Centre for Evidence-Based Medicine criteria, and recommendations for physical activity were made using the Oxford Centre's criteria for grades of recommendation.
Results
Of 42 articles retrieved, 11 met the inclusion criteria. The Internet review of 18 organizations yielded no previous guidelines or position papers for physical activity and scoliosis. Recommendations were made from 3 level 3b studies and 8 level 5 studies; they include the following: (1) brace-treated and surgically treated scoliosis patients have demonstrated that they can physically participate in physical activities at the same level as nonsurgical patients (grade C recommendation); (2) nonsurgically treated patients are encouraged to participate in sports and physical activity and (3) scoliosis is not a contraindication to participation in most sports (grade D recommendation); (4) brace-treated scoliosis patients are encouraged to exercise with their brace on; however, exercise may also be done outside of the brace (grade D recommendation); and (5) physical activity may be commenced after surgery for scoliosis; however, no high-quality evidence exists that guides the timing of return to physical activity (grade D recommendation). A potential association between elite-level competition in specific sports at an early age and an increased prevalence of scoliosis has been reported (grade C recommendation).
Conclusion
This article offers evidence-based guidance to health care providers and to patients with scoliosis when making decisions to participate in physical and sporting activities.
Key indexing terms: Scoliosis, Sports, Physical activity, Chiropractic
Introduction
Scoliosis is commonly defined as a lateral spinal curvature of at least 10° (Fig 1) when measured with Cobb's method1 and often results in a visible rib hump when the patient bends forward at the waist. Primary care providers and spine specialists often see patients with this condition. For those 16 years and younger, scoliosis has a prevalence of 2% to 3%,1 with a lower prevalence of 0.3% to 0.5% noted for curves larger than 20°.2 Scoliosis is present equally in males and females for curves of approximately 10°; but with larger curves, the prevalence for scoliosis is greater in females.1 In the United States, approximately 500 000 adults have scoliosis.3 Potential complications of scoliosis include back pain,1,4 curve progression,1 psychosocial effects,1,5 and, in severe cases, pulmonary symptoms.1,6,7 Although some cases of scoliosis are due to an underlying congenital anomaly or pathology, such as neurofibromatosis, connective tissue disorders, or spinal cord abnormalities,4 most (65%) of the curves are idiopathic.3
Fig 1.
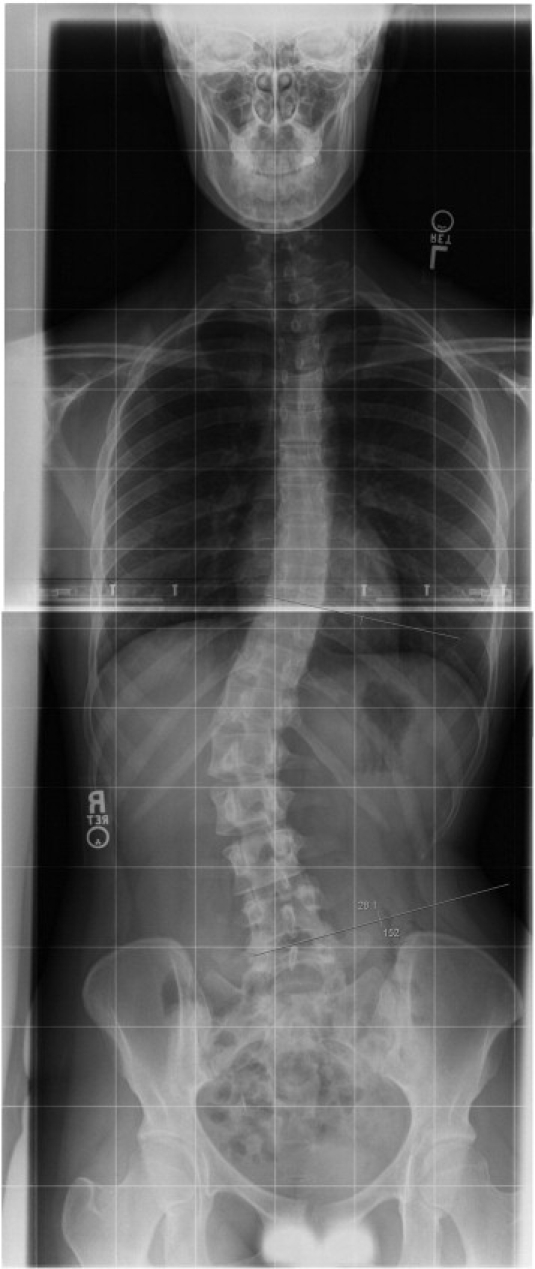
A young patient with scoliosis.
According to the literature, conventional management options for patients with scoliosis are 3-fold: observation, bracing, and surgery.8,9 During observation, for curves less than 25° in skeletally immature patients8,9 and less than 45° in skeletally mature patients,9 assessment is made over time via radiography to observe for progression of the scoliotic curve and any potentially related symptoms. When the curve progresses to 25°, patients are often treated with one of numerous braces available on the market in an effort to halt progression of the scoliosis.8 Spinal fusion is the final option for patients with progressing scoliotic curves8 greater than 40° to 50°.10 Therapeutic exercises,10,11 lateral electrical stimulation,12 manual therapy,13 a combination of manual therapy and rehabilitation exercises,14 traction,15 and acupuncture16 are additional scoliosis interventions noted in the literature; however, insufficient evidence currently suggests the efficacy of these procedures in halting curve progression or restoring a normal curve, although some may aid in reducing pain associated with scoliosis.
Despite the many studies regarding scoliosis treatment or the management of associated pain, previous authors4,10,17 have pointed out that little objective information is available to guide patients with scoliosis—or parents of young patients—about acceptable physical activities or if participation in sporting activities is prudent. Historically, in the United States, there are recommendations in the literature that people with scoliosis should not participate in exercise.11,18,19 One of the earliest studies on scoliosis and treatment was a 1941 study published by the American Orthopaedic Association.18 This group suggested that the use of exercise would worsen lateral curvatures for patients with idiopathic scoliosis. In 185 cases treated with exercise alone, approximately 60% of the patients experienced a worsening of the curve; and the curve remained unchanged in the remaining 40%. This article concluded that bracing and surgical fusion were the treatments of choice. The determinations made in this study eventually led to widespread recommendations for scoliosis patients to avoid sporting and exercise activities.11,19 This may explain the scarcity in the literature concerning the appropriateness of exercise and sporting activities for patients with scoliosis.
At present, no published recommendations are found regarding the suitability of physical activity for those with scoliosis. A new emphasis is being placed on exercise to combat the epidemic of obesity in the United States20; people with scoliosis often desire to remain active,4,19 and a rise in female participation in sports has been noted over the past couple of decades.21 Therefore, investigation into the appropriateness of physical activity for people with scoliosis is needed. The focus of this study is (1) to systematically and critically review the literature to evaluate if physical activity is considered a contraindication for individuals with scoliosis and (2) to synthesize this literature and offer recommendations for participation in physical activities for patients with scoliosis.
Methods
Search strategy
PubMed and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) were searched using EBSCOhost Web; the Index to Chiropractic Literature (ICL) was searched directly at its site (www.chiroindex.org). Searches for all databases were from their starting dates through July 2008, and they were conducted during the month of August 2008. The initial search strategy combined the term scoliosis with a variety of terms relevant to the topic of study (Table 1). When that search was completed, CINAHL was searched using the same strategy. Relevant hits were verified against the previously recorded relevant data from the PubMed search and were noted as “new hits” in Table 1. This same procedure was used for the ICL search, verifying results from the ICL against both PubMed and CINAHL results. We sought out additional articles referenced in the articles retrieved.
Table 1.
Search terms and results
| Search Terms | MEDLINE |
CINAHL |
ICL |
|||
|---|---|---|---|---|---|---|
| Total Hits | Potentially Relevant New Hits | Total Hits | Potentially Relevant New Hits | Total Hits | Potentially Relevant New Hits | |
| Scoliosis + sport | 137 | 37 | 3 | 0 | 83 | 0 |
| Scoliosis + sports | 157 | 8 | 17 | 0 | 0 | 0 |
| Scoliosis + athletic injuries | 30 | 1 | 9 | 1 | 3 | 0 |
| Scoliosis + athletic participation | 6 | 0 | 0 | 0 | 0 | 0 |
| Scoliosis + sport performance | 5 | 0 | 1 | 0 | 0 | 0 |
| Scoliosis + public health | 27 | 9 | 2 | 0 | 6 | 0 |
| Scoliosis + exercise | 319 | 6 | 90 | 3 | 3 | 0 |
| Total | 681 | 61 | 122 | 4 | 95 | 0 |
The National Guidelines Clearinghouse was searched for existing guidelines pertinent to physical activity participation for people with scoliosis. Scoliosis was the only search term, and all available guidelines were reviewed for relevance. We also investigated Web sites of organizations/agencies with a potential interest in scoliosis. These Web sites were selected by searching an Internet browser using the term scoliosis. All organizations returned by the search were searched for position/white papers about scoliosis and physical activity (Table 2).
Table 2.
Organization websites included in search for organization position statements regarding physical activity and scoliosis
| Organization | Web Site URL |
|---|---|
| American Academy of Family Physicians | www.aafp.org |
| American Academy of Orthopedic Surgeons | www.aaos.org |
| American Academy of Pediatrics | www.ap.org |
| American Chiropractic Association | www.amerchiro.org |
| American College of Sports Medicine | www.acsm.org |
| American Physical Therapy Association | www.apta.org |
| ARISE–The Scoliosis Research Trust | http://scoliosisresearchtrust.org.uk/ |
| International Chiropractic Association | www.chiropractic.org |
| International Chiropractic Pediatric Association | www.icpa4kids.org |
| International Society on Spinal Orthopaedic and Rehabilitation Treatment–SOSORT | www.sosort.org |
| National Athletic Trainers' Association | www.nata.org |
| National Institute of Arthritis and Musculoskeletal and Skin Diseases | www.niams.nih.gov |
| National Scoliosis Foundation | www.scoliosis.org |
| North American Spine Society | www.spine.org |
| Scoliosis Association | www.scoliosis-assoc.org |
| Scoliosis Care Foundation | www.scoliosiscare.org |
| Scoliosis Research Society | www.srs.org |
| Spine Society of Australia | www.scoliosis-australia.org |
Inclusion/exclusion criteria
Articles (all languages and all research designs) assessing or discussing the appropriateness of physical activity for people with all types of scoliosis were included. Articles published in languages other than English were translated to English using a software translator (Google Language Tools; Google Inc, Mountain View, CA). Only studies from peer-reviewed scholarly journals were included. Articles from trade magazines and nonscholarly sources were excluded, as were letters to the editor and articles not specific to the use or recommendations of physical activity participation for people with scoliosis. Reports of therapeutic exercises (eg, stretching, strengthening) used as a treatment to correct the curvature of scoliosis were excluded because of their intentional use as a therapeutic intervention, rather than as a means to merely exercise or maintain physical activity. Reports without abstracts but appearing potentially relevant were obtained when available, although the few articles that fit this category were usually more than 10 years old and in a foreign language. Abstracts of conference proceedings were not included because of the high rate of conference presentations that are never published.22,23 Web sites of private health care practitioners, private individuals, and group practices were excluded.
Methods of review
The primary author conducted the search; secondary authors were asked to contribute additional citations felt to be missing from the list. Abstracts of the citations that obviously met the review criteria, or possibly met the criteria, were saved. Full articles of each abstract were then retrieved. All authors independently reviewed each of the full articles to verify that they had met the inclusion criteria. Articles that did not meet the criteria were discarded, and a note was made as to why they were excluded. Once an article was included, the citation, study design, principal findings, and other pertinent notes were logged in a summary table. Differences in opinions of the authors regarding the particular inclusion or exclusion of any articles were settled by discussion and e-mail correspondence until consensus was achieved.
Quality scoring
The Oxford Centre for Evidence-Based Medicine levels of evidence rating scheme24 was used. In this system, evidence is rated for quality from levels 1 (best quality) to 5 (lowest quality), primarily on the research design. The levels of evidence for therapy, prevention, etiology, or harm studies are presented in Table 3. Included articles were rated using this scheme. This scheme is primarily based on the level of evidence inherently provided by the research design that a study team selects for their research. Thus, to rate an article, one must essentially identify the research design used by the research team. The authors did not have any disagreements pertaining to the identification of research designs or ranking. Information from the reviewed studies pertaining to physical activity and scoliosis was tracked in a spreadsheet and analyzed for similarity or contradictions. Recommendations for physical activity participation for those with scoliosis were made based upon areas of congruence between articles reviewed. The Oxford Centre for Evidence-Based Medicine grades of recommendation24 were used. This grading system is used in conjunction with the levels of evidence scheme described above. The strength of recommendations is made by considering the quality of the evidence obtained. The scale of strength of recommendations is presented in Table 4.
Table 3.
The Oxford Centre for Evidence-Based Medicine levels of evidence rating scheme
| Level | Study(ies) |
|---|---|
| 1a | Systematic review with homogeneity of randomized clinical trials |
| 1b | Individual randomized clinical trial with narrow confidence interval |
| 1c | All or none studies |
| 2a | Systematic review with homogeneity of cohort studies |
| 2b | Individual cohort study (including low-quality randomized clinical trial) |
| 2c | Outcomes research; ecological studies |
| 3a | Systematic review with homogeneity of case-control studies |
| 3b | Individual case-control study |
| 4 | Case series and poor-quality cohort and case-control studies |
| 5 | Expert opinion without explicit critical appraisal, or based on physiology, bench research, or “first principles” |
Table 4.
The Oxford Centre for Evidence-Based Medicine grades of recommendation
| Grade | Quality of Evidence |
|---|---|
| A | Consistent level 1 studies |
| B | Consistent level 2 or 3 studies or extrapolations from level 1 studies |
| C | Level 4 studies or extrapolations from level 2 or 3 studies |
| D | Level 5 evidence or troublingly inconsistent or inconclusive studies of any level |
Results
Quantity of studies
Eight hundred ninety-eight initial citations were found during the literature search. After applying the exclusion criteria, 65 potential studies were identified (Table 1); and 27 of these were discarded after a review of the abstracts made it apparent that the studies were not about scoliosis and physical activity. After each of the remaining 38 articles were read, 4 additional articles were retrieved after considering the articles cited in the references of the articles read. Consensus for inclusion of articles deemed 11 articles4,8,10,17,19,25-30 acceptable for review, thereby culling 31 articles. All 31 articles1,5-7,9,11,21,31-53 were excluded because they made no recommendations pertaining to physical activity and scoliosis. Four of the articles11,49,52,53 were also excluded because they focused on therapeutic exercises as a treatment of scoliosis curvature rather than reporting physical activity for people with scoliosis. All 3 potentially relevant guidelines found in the National Guidelines Clearinghouse3,54,55 were excluded from review because they did not address athletic participation for people with scoliosis. None of the 18 organization Web sites reviewed contained a position statement regarding the appropriateness of physical activity for people with scoliosis.
Summary of included studies
The summary table for the included studies is presented in Table 5. No systematic reviews (levels 1a, 2a, 3a), randomized clinical trials (levels 1b, 2b), all or none studies (level 1c), cohort studies (level 2b), ecological studies (level 2c), or case series (level 4) were identified that met the inclusion criteria and addressed the purpose of this study.
Table 5.
Summary table of studies included in this review
| Level of Evidence | Design | Author | Summary |
|---|---|---|---|
| 3b | Case control | Parsch (2002) | Scoliosis patients experienced more impairment to their sporting activities than did age-matched controls. Sport activity was not more restricted after extended spinal fusion than it was after nonoperative treatment. The primary reasons people with scoliosis reduced their activities were functional limitations and back pain; but they participated in sports equally as strenuous as age-matched controls, regardless of fusion or the number of fused segments. |
| 3b | Case control | Danielsson (2006) | Brace-treated and fusion-treated patients had less spinal mobility and muscle endurance at 20-y follow-up compared with healthy subjects. Physical function was not severely restricted for scoliosis subjects, however. |
| 3b | Case control | Meyer (2007) | In comparing exercise/sporting activity between teens with and without scoliosis, those with a double major scoliosis exercised more than single major curve patients and controls. The authors recommended regular and nonintensive physical/sport activity for scoliosis patients but to avoid spinal trauma, which the authors suggest may occur with judo, triple jump, long jump, butterfly swimming, weight lifting, and off-road cycling. |
| 5 | Narrative review | Von Strempel (1993) | With scoliosis less than 20°: recommended no restrictions to physical activity; 20°-30°: restricted from performance sport, but school sports and competitive sports allowed; 30°-50° or 20°-30° with progression of 5° in 6 mo: school sports allowable with brace, nonschool sports allowable (horseback riding, tennis, table tennis). Performance sport contraindicated, competitive sport at “club level” contraindicated but may be allowable at school with watchful eye of a teacher. Curves of 50° or more: recommended endurance sports (cycling, swimming, hiking, jogging). Postoperative patients: no sport for 1 y, including cycling and table tennis; no competition sports in second year; return to sports in third year if fusion mass is stable; no performance sport postoperatively even in year 3. Sports with axial and rotational load not recommended after surgery (ball games, tennis, alpine skiing, trampoline, technical athletics, rhythmic gymnastics, contact sports). Performance sport and competitive sport at mass sport not recommended. |
| 5 | Narrative review | Omey (2000) | Scoliosis is not a contraindication to participation in sports. Unless scoliosis is severe, it does not reduce physical function. If pain accompanies scoliosis, examination for underlying pathology (eg, syringomyelia, disk herniation, degenerative spinal disease) should be performed. Active strengthening and flexibility encouraged during brace wearing. Sports may be played while athlete is not wearing a brace. Swimming is not contraindicated, although some previous researchers felt that it increased scoliosis. Aquatic activity may help maintain flexibility, strength, and endurance. Professional volleyball should be avoided because of facet stressing, but recreational/amateur volleyball is acceptable. Postoperative patients: contact sports, gymnastics, and diving should not be performed. |
| 5 | Narrative review | Wood (2002) | Nonsurgically treated scoliosis is not a contraindication to participation in most sports. “There is no objective evidence in the literature to suggest that active participation in any sport is directly associated with worsening of scoliotic curvatures beyond that of the natural history of the disorder.” Active exercise was recommended for those who wear braces (eg, Milwaukee brace, Boston brace) for their scoliosis, and brace wearing during exercise was encouraged. According to this author, no study exists showing any negative effects of contact sports on the curve of a braced individual. Encouraged any and all athletic participation during hours out of a brace, not only for physical benefit, but for psychologic and social well-being. For postoperative scoliosis, the following recommendations were made: 2 mo = recreational swimming, cycling, hiking; 4 mo = light physical activity (tennis, catch, shooting basketballs); 6 mo = all activities, including contact (if fusion is solid, instrumentation is stable, and there is no pain). An exception was long fusions below L3, as the author cautioned against heavy twisting or contact sports. |
| 5 | Narrative review | Baker (2004) | Scoliosis alone is not a criterion for disqualification from sports. People with braces may require sports participation limitations while in the brace. No evidence that exercise can increase or decrease curvature. |
| 5 | Narrative review | Liljenqvist (2006) | Sporting activity should be encouraged for physical and psychologic well-being. Sports are allowable for those in a brace. Encouraged endurance sports without impact (cycling, swimming, walking, in-line skating, dance, step aerobics, yoga, horseback riding). Volleyball and high-impact sports not recommended. Postoperative patients: cycling allowable at 6 mo; swimming allowable; contact/collision not allowable. Sports with risk for falling should be avoided. |
| 5 | Narrative review | Schiller (2008) | Author pointed out that a scarcity in the literature exists that documents appropriate guidelines for athletic participation after nonoperative and operative treatment. Recommended flexibility training. Stated that patients with scoliosis treated nonoperatively can participate in all sporting activities. Sport participation while wearing a brace is allowed, not protective, and should be advocated. Sport participation out of a brace is also possible. Conditioning should focus on flexibility of the spine and core strengthening. Addition of plyometrics and power lifting after appropriate conditioning is allowed. Athletes with scoliosis should be encouraged to participate in sport. Postoperative participation in sport should be at the discretion of the surgeon. Author did not recommend against torque sports (gymnastics, ballet, swimming, wrestling, javelin). |
| 5 | Survey | Rubery (2002) | Postoperative patients: among physicians surveyed, most popular time to allow low-impact, noncontact sports = 6 mo. Contact sport allowed between 6 and 12 mo. 13% felt no contact should ever be allowed in postoperative patients. No collision sports recommended by 60% of respondents; but for those who didallow it, it was after 12 mo. Gym class resumed at 6-12 mo. No catastrophic neurologic complications were identified by respondents as being related to postoperative sports participation. |
| 5 | Case report | Fuchs (2001) | A patient with a previous posterior T2-L1 fusion for scoliosis sustained a cervical dislocation during a fall on her head/neck during cheer-leading. The authors therefore recommended against collision sport and sports requiring excessive spinal mobility, such as cheer-leading and gymnastics, in postoperative scoliosis patients. |
The strongest evidence (level 3b) found pertaining to the appropriateness of physical activity for those with scoliosis were 3 case-control studies.25-27 Parsch et al25 assessed the sports activities of 2 groups of patients with idiopathic scoliosis. In 1 group, the scoliosis was treated operatively; and in the other group, the scoliosis was treated nonoperatively. Each was compared with age-matched controls. The authors found that scoliosis patients experienced more impairment to their sporting activities in the long term than did age-matched controls. Sport activity was not more restricted after extended spinal fusion than it was after nonoperative treatment. The primary reasons people with scoliosis reduced their physical activities were functional limitations and back pain; but they participated in sports equally as strenuous as age-matched controls, regardless of fusion or the number of fused segments. The authors concluded that a patient with idiopathic scoliosis who is considering surgical stabilization may have a comparable level of long-term sporting activity with that of a nonoperatively managed patient with the same magnitude of spinal curve. Danielsson et al27 assessed several physical and quality-of-life parameters of surgically treated and brace-treated scoliosis patients 20 years after their therapy was concluded and compared these outcomes with 100 age- and sex-matched controls. They found that, compared with the controls, patients who had brace-treated and surgically treated scoliosis had less spinal mobility and muscle endurance at 20-year follow-up. However, physical function was not severely restricted for the scoliosis patients. Meyer et al26 assessed associations between exercise and sporting activities and idiopathic scoliosis in 74 girls with 2 lateral curvatures (double major curves) and 95 girls with a single major curve who were age-matched to 100 control girls. Girls with a double major scoliosis exercised more frequently than single major curve patients and controls. The authors recommended regular and nonintensive physical/sport activity for scoliosis patients; but the patients were told to avoid spinal trauma, which the authors suggested may occur with judo, triple jump, long jump, butterfly swimming, weight lifting, and off-road cycling. However, these suggestions were not based upon data and were only the authors' opinions.
The bulk of the literature pertaining to the appropriateness of physical activity for those with scoliosis is level 5 evidence, consisting of 6 nonsystematic reviews of the literature (narrative overviews),4,8,10,19,28,29 1 survey,17 and 1 case report.30 Von Strempel et al29 published the earliest article found on the topic of physical activity and scoliosis. Based upon their experience in operatively and nonoperatively treated scoliosis patients, they made several recommendations regarding the appropriateness of physical activity for their patients. For scoliosis with a Cobb angle less than 20°, they suggested no restrictions on activity. For curves of 20° to 30°, they recommended restriction from what they termed performance sport; but school sports and competitive sports were allowed. For curves of 30° to 50° or 20° to 30° with progression of 5° in 6 months, they allowed school sports with patients wearing a brace and also allowed some nonschool sports (eg, horseback riding, tennis, table tennis) but did not recommend performance sport or competitive sports at club level. They would allow competitive sports, however, if performed at school; it should be under the watchful eye of a teacher. For curves of 50° or more, von Strempel et al recommended endurance sports (eg, cycling, swimming, hiking, jogging). For postoperative patients, they allowed no sport for 1 year, including cycling and table tennis, and no competitive sports in the second postoperative year; but they would allow the return to sports in the third year if the fusion mass was fully consolidated. The authors did not report by what means they determined full fusion. They would not allow a return to performance sport for postoperative patients at all, and sports with axial and rotational loads (inclusive of ball games, tennis, alpine skiing, trampoline, technical athletics, rhythmic gymnastics, contact sports) were not recommended after surgery.
Omey et al8 suggested that scoliosis is not a contraindication to participation in sports and asserted that, unless a scoliosis was severe, it would not reduce physical function. According to Omey et al,8 “Scoliosis is not a contraindication to participation in sports by the young athlete”; and they recommended examination for underlying pathology (eg, syringomyelia, disk herniation, degenerative spinal disease) if pain accompanied scoliosis. They also encouraged active strengthening and flexibility exercises for the spine during brace wearing and maintained that sports may be played while the athlete was not wearing a brace. Omey et al specifically asserted that aquatic activity may be helpful to maintain flexibility, strength, and endurance. They stated that professional volleyball should be avoided because of facet stressing, but felt that recreational/amateur volleyball is acceptable. For postoperative patients, they deemed that contact sports, gymnastics, and diving should not be performed. Similar to Omey et al, Wood19 declared that nonsurgically treated scoliosis is not a contraindication to participation in most sports. Wood was very direct in his opinion, stating that “There is no objective evidence in the literature to suggest that active participation in any sport is directly associated with worsening of scoliotic curvatures beyond that of the natural history of the disorder.” He recommended active exercise for those who wear braces (eg, Milwaukee brace, Boston brace) for their scoliosis, and brace wearing during exercise was encouraged. Wood also claimed that no study exists showing negative effects of contact sports on the curve of a braced individual. He encouraged any and all athletic participation during hours out of a brace, not only for physical benefit, but for psychologic and social well-being. For postoperative scoliosis patients, at 2 months, recreational swimming, cycling, and hiking were allowed; at 4 months, light physical activity (tennis, catch, shooting basketballs) was allowed; at 6 months, all activities, including contact sport, were allowed if the fusion was solid, instrumentation was stable, and the patient had no pain. An exception was long fusion below L3, as the author cautioned against heavy twisting or contact sports.
In 2004, Baker and Patel28 reiterated the belief that scoliosis alone is not a criterion for disqualification from sports. They stated that people with braces may require sports participation limitations while the athlete is in the brace and echoed Wood's19 position that there is no evidence that exercise can increase or decrease a scoliosis curvature. Liljenqvist et al10 also encouraged sporting activity for physical and psychologic well-being, including for those patients wearing a brace. They encouraged endurance sports without impact, including cycling, swimming, walking, in-line skating, dance, step aerobics, yoga, and horseback riding, but did not recommend volleyball and other high-impact sports. For postoperative patients, they stated that cycling and swimming were allowable at 6 months, but that contact/collision sports were not allowable; and they felt that sports with a risk for falling should be avoided. A most recent review (2008) by Schiller and Eberson4 recommended flexibility training and indicated that patients with scoliosis treated nonoperatively can participate in all sporting activities. They held that sport participation while wearing a brace was allowed, albeit not as a protective device, and that sport participation out of a brace was also possible. The authors claimed that conditioning should focus on flexibility of the spine and core strengthening and felt that the addition of plyometrics and power lifting after appropriate conditioning was acceptable. Specifically, they felt that athletes with scoliosis should be encouraged to participate in sport. For postoperative patients, they maintained that sports participation should be at the discretion of the surgeon. They did not recommend against torque sports for postoperative patients (eg, gymnastics, ballet, swimming, wrestling, javelin), as had previous authors.
Rubery and Bradford17 surveyed the membership of the Scoliosis Research Society regarding their opinions of return to athletic activity after spinal surgery. Among the physicians surveyed (n = 316, 44% response rate), the most popular time to allow low-impact, noncontact sports was 6 months after surgery. Physicians allowed contact sports between 6 and 12 months after surgery. Thirteen percent felt that no contact sport should ever be allowed in postoperative patients. No collision sport was allowed by 60% of respondents; but for those that did allow it, participation was after 12 months. Gym class was commonly allowed to resume at 6 to 12 months. No catastrophic neurologic complications were identified by respondents as being related to postoperative sports participation.
Fuchs et al30 reported a case of a patient with a previous posterior T2-L1 fusion for scoliosis who sustained a cervical dislocation during a fall on her head/neck during a cheer-leading exercise. The authors therefore recommended against collision sport and sports requiring excessive spinal mobility, such as cheer-leading and gymnastics, in postoperative scoliosis patients.
Scoliosis may be more common in participants of various sports; the topic was broached in 7 articles8,10,19,28,32,35,36 among the 42 retrieved for this review, and 4 of these were included in the literature synthesis.8,10,19,28 Summarily, authors have reported scoliosis more commonly in the sports of dancing,8,19,28 ballet,19 swimming,8,19,28,36 javelin,8,19,36 table tennis,19 tennis,10,19 hurling,19 gymnastics,28,35 and rhythmic gymnastics.10,32 However, no clear causal relationship is established that demonstrates that a particular sport causes or contributes to scoliosis.
Quality scores
Because the 3 usual and customary categories for treating the curvature associated with scoliosis are observation, bracing, and surgery, the recommendations in this study follow this classification.
-
•
Brace-treated and surgically treated scoliosis patients have demonstrated that they can physically participate in sports activities at the same level as controls (grade C recommendation [2 level 3b studies25,27]).
-
•
Brace-treated or observation-only scoliosis patients are encouraged to participate in sports and physical activity (grade D recommendation [1 level 3b study26; 5 level 5 studies4,8,19,28,29]).
-
•
Nonsurgically treated scoliosis is not a contraindication to sports participation (grade D recommendation [3 level 5 studies8,19,28]).
-
•
Brace-treated scoliosis patients are encouraged to exercise with their braces on; however, exercise may also be done outside of the brace (grade D recommendation [4 level 5 studies4,8,19,29]).
-
•
Sports and exercise may be commenced in the months after surgery for scoliosis correction; however, there is no high-quality evidence guiding return to sport activity. Currently, return to activity is based upon the opinion of the attending surgeon (grade D recommendation [2 level 5 studies17,28]) and expert opinions without explicit critical appraisal (grade D recommendation [5 level 5 studies8,19,28-30]). No clear evidence or guideline is offered regarding contact and/or collision sports after surgery.
-
•
A potential association between elite-level competition in particular sports at an early age and an increased prevalence of scoliosis has been reported (grade C recommendation [1 level 3b study32; 1 level 4 study35; 5 level 5 studies8,10,19,28,36]).
Discussion
The primary finding from this review is that most studies support physical activity for patients with scoliosis. Exercise is encouraged in the available literature and not absolutely contraindicated, even for those who have had spinal surgery. This conclusion has application for those in clinical practice who can reassure their patients that they may continue to enjoy an active lifestyle. The information is also of use for clinicians to encourage individuals with scoliosis and to let them know that scoliosis is not a reason to avoid exercise. Furthermore, it demonstrates that little to no obvious harm is associated with physical activity and scoliosis. It would seem feasible that clinical trials could be conducted to determine which types of activity lead to better physical or quality of life outcomes for both operatively treated and nonoperatively treated patients.
We found 2 case-control studies25,27 of reasonable quality showing that brace-treated and surgically treated scoliosis patients can physically participate in sports activities at the same level as controls. However, the literature included in this review also contains several articles8,17,19,28-30 of lower quality wherein the authors advise against participating in the athletic activities of healthy subjects. There may be several explanations for this phenomenon. First, although physicians may tell patients not to engage in a particular activity, patients may not comply with the recommendation. Second, there may be a discord between what physicians think their patients can do and what the patients are actually capable of doing. Third, the potential of litigation for telling a postoperative patient to return to collision or contact sport might drive physician decision making. Fourth, it is possible that some physicians are not aware of published studies demonstrating that surgically treated patients are as active as nonsurgically treated ones. The gap between what physicians feel is appropriate for patients and what patients actually do is a fertile area for further study.
Another interesting finding is that the literature pertaining to physical activity for patients being treated with bracing is essentially anecdotal. We had hoped there would be more substantial data available to aid in clinical decision making when providers make physical activity recommendations to brace-treated patients. More research is needed in this area, particularly in focusing on physical activity risk factors associated with scoliosis progression and any risk of injury with sports participation.
Despite surgery being a therapeutic option for scoliosis patients, the scarcity of the body of evidence to guide the physician in helping patients regain healthy and active lifestyles after surgery is remarkable. We found no guidelines or position statements that could serve as a standard of care in the area of safety of exercise for postsurgical patients. Rubery and Bradford17 confirmed our suspicion, “ … the nature and timing of postoperative return to sports has remained largely based on anecdote and traditional teaching”; they undertook a bold study to query the membership of the Scoliosis Research Society regarding their opinions of return to exercise after surgical correction of scoliosis. They found from this study that there was no consensus regarding return to activity. Twenty-four percent of physicians restricted postsurgical scoliosis patients from collision sports forever, 36% advised against, and 39% allowed this activity by 2 years after surgery. All responding physicians eventually allowed patients to return to low-impact, noncontact sports (eg, swimming and cross-country skiing); however, the waiting period ranged from immediately after surgery to 2 years. We acknowledge that every patient case must be given due consideration and that a guideline cannot possibly fit every unique situation; however, we do suggest that return to physical activity guidelines are needed for postsurgical scoliosis patients, such as programs designed for postoperative total hip arthroplasty patients.56
Although conjecture is found in the literature regarding concerns that physical activity may worsen a scoliotic curve or may increase the prevalence of scoliosis, little data support such hypotheses. Thus far, the number of epidemiology studies conducted is small; and we feel the quality could be improved. For example, the purpose of the study of Meyer et al26 was to determine the relationship between scoliosis curve type (outcome) and the type of physical activity (exposure) practiced by the subjects; however, no odds ratios were reported. A similar situation is found in the article of Tanchev et al32 wherein the term incidence is used in providing prevalence data; this is erroneous because incidence rate is used to describe the number of new cases in a population over a given period and prevalence simply means the number of cases present in the population.57 Most importantly, a causal association between participation in a specific sport and an increase in the prevalence of scoliosis in that sport should not be made without substantial investigation using prospective research designs, such as cohort studies. It is interesting to note that no cohort studies have been conducted to provide a closer causal association between various sports and scoliosis and to allow one to establish relative risks associated with such sporting activities. Cohort studies are generally used to examine rare exposures58; and although difficult to carry out, they would be a reasonable research design to make more definitive statements regarding the association of particular sports and their potential casual association with scoliosis. This is an area in the scoliosis literature in need of additional and more rigorous research.
Limitations
Although the present study is a stronger form of evidence than the many narrative overviews available on this topic, it does have some limitations. This study focused on idiopathic scoliosis; and the results may not be generalizable to those patients who have scoliosis resulting from another disorder, such as neurofibromatosis, spinal degeneration, or joint hypermobility syndrome. The degree to which our findings may be generalized to scoliosis patients with back pain is not known. Furthermore, our recommendations may be not be generalizable to those who have had multiple surgical procedures to correct spinal deformity or have other comorbidities that preclude exercise or sport. A potential drawback is that the literature pertaining to therapeutic exercise for the treatment of scoliosis curvature was not taken into consideration; it is possible that some evidence from the treatment literature may have provided further evidence of the safety of exercises for scoliosis patients and should be studied further. No level 1 or level 2 studies that applied to the study question were identified. The levels of evidence pertaining to physical activity safety and scoliosis are low; thus, the quality scores and recommendations are supported more by observational studies and expert opinion than by rigorous controlled studies.
Conclusion
Relatively low levels of evidence and recommendations (grades C and D) demonstrate that little objective evidence exists to inform patients, policy makers, or providers regarding the safety of physical activity for individuals with scoliosis. There is no evidence that sporting or physical activity is harmful to patients with scoliosis, with the possible exception of some cases immediately after surgery or instances of other underlying pathology. The principal findings of this review are as follows: (1) brace-treated and surgically treated scoliosis patients have demonstrated that they can physically participate in sports activities at the same level as controls; (2) nonsurgically treated patients are encouraged to participate in sports and physical activity, and scoliosis is not a contraindication to participation in most sports; (3) brace-treated scoliosis patients are encouraged to exercise with their brace on; however, exercise may also be done outside of the brace; (4) physical activity may commence after surgery for scoliosis; however, there is no high-quality evidence guiding return to sport activity; and (5) the potential association between elite-level competition in particular sports at an early age and an increased prevalence of scoliosis has been reported.
Acknowledgment
The members of the American Chiropractic Board of Sports Physicians Scoliosis and Physical Activity Guideline Committee are acknowledged for their volunteer efforts in providing critical review of early drafts of this manuscript and include the following: Pat Helma, DC, DACBSP; Robert Nelson, DC, DACBSP; Joe Horrigan, DC, DACBSP; Anne Sorrentino Hoover, DC, CCSP; Karen Chaney, DC, DACBSP; and Darren Hancock, DC, CCSP.
Footnotes
Disclaimer: The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government.
Refereeing Editor: Jerrilyn Cambron, DC, PhD (jcambron@nuhs.edu), was the Refereeing Editor for this manuscript. She was solely responsible for managing the peer review process, revision process, and the acceptance of this manuscript. The Editor and Associate Editor declare that they were not involved in the peer review process or acceptance decision for this paper.
The American Chiropractic Board of Sports Physicians provided funding for this study, which included a small stipend to the principal and second author of this paper. Each author signed a conflict of interest disclosure form provided and stored by the American Chiropractic Board of Sports Physicians. None of the authors had any conflicts of interest to declare.
Contributor Information
Bart N. Green, Email: bart.green@med.navy.mil, bgreen@nuhs.edu.
Claire Johnson, Email: cjohnson@nuhs.edu.
William Moreau, Email: dconline@mchsi.com.
References
- 1.Weinstein S.L. Adolescent idiopathic scoliosis: prevalence and natural history. Instr Course Lect. 1989;38:115–128. [PubMed] [Google Scholar]
- 2.Dolan L.A., Weinstein S.L. Surgical rates after observation and bracing for adolescent idiopathic scoliosis: an evidence-based review. Spine. 2007;32(19 Suppl):S91–S100. doi: 10.1097/BRS.0b013e318134ead9. [DOI] [PubMed] [Google Scholar]
- 3.United States Preventive Services Task Force . Agency for Healthcare Research and Quality; Rockville: 2004. Screening for idiopathic scoliosis in adolescents: recommendation statement. [Google Scholar]
- 4.Schiller J.R., Eberson C.P. Spinal deformity and athletics. Sports Med Arthrosc. 2008;16(1):26–31. doi: 10.1097/JSA.0b013e3181629aa8. [DOI] [PubMed] [Google Scholar]
- 5.MacLean W.E., Green N.E., Pierre C.B., Ray D.C. Stress and coping with scoliosis: psychological effects on adolescents and their families. J Pediatr Orthop. 1989;9(3):257–261. [PubMed] [Google Scholar]
- 6.dos Santos Alves V.L., Stirbulov R., Avanzi O. Impact of a physical rehabilitation program on the respiratory function of adolescents with idiopathic scoliosis. Chest. 2006;130(2):500–505. doi: 10.1378/chest.130.2.500. [DOI] [PubMed] [Google Scholar]
- 7.Barrios C., Perez-Encinas C., Maruenda J.I., Laguia M. Significant ventilatory functional restriction in adolescents with mild or moderate scoliosis during maximal exercise tolerance test. Spine. 2005;30(14):1610–1615. doi: 10.1097/01.brs.0000169447.55556.01. [DOI] [PubMed] [Google Scholar]
- 8.Omey M.L., Micheli L.J., Gerbino P.G. Idiopathic scoliosis and spondylolysis in the female athlete. Tips for treatment. Clin Orthop Relat Res. 2000;(372):74–84. doi: 10.1097/00003086-200003000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Peelle M.W., Luhmann S.J. Management of adolescent idiopathic scoliosis. Neurosurg Clin N Am. 2007;18(4):575–583. doi: 10.1016/j.nec.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 10.Liljenqvist U., Witt K.A., Bullmann V., Steinbeck J., Volker K. Recommendations on sport activities for patients with idiopathic scoliosis. Sportverletz Sportschaden. 2006;20(1):36–42. doi: 10.1055/s-2005-859029. [DOI] [PubMed] [Google Scholar]
- 11.Weiss H.R., Negrini S., Hawes M.C., Rigo M., Kotwicki T., Grivas T.B. Physical exercises in the treatment of idiopathic scoliosis at risk of brace treatment—SOSORT consensus paper 2005. Scoliosis. 2006;1:6. doi: 10.1186/1748-7161-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rowe D.E., Feise R.J., Crowther E.R., Grod J.P., Menke J.M., Goldsmith C.H. Chiropractic manipulation in adolescent idiopathic scoliosis: a pilot study. Chiropr Osteopat. 2006;14:15. doi: 10.1186/1746-1340-14-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Romano M., Negrini S. Manual therapy as a conservative treatment for adolescent idiopathic scoliosis: a systematic review. Scoliosis. 2008;3:2. doi: 10.1186/1748-7161-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morningstar M.W., Woggon D., Lawrence G. Scoliosis treatment using a combination of manipulative and rehabilitative therapy: a retrospective case series. BMC Musculoskelet Disord. 2004;5:32. doi: 10.1186/1471-2474-5-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chromy C.A., Carey M.T., Balgaard K.G., Iaizzo P.A. The potential use of axial spinal unloading in the treatment of adolescent idiopathic scoliosis: a case series. Arch Phys Med Rehabil. 2006;87(11):1447–1453. doi: 10.1016/j.apmr.2006.08.325. [DOI] [PubMed] [Google Scholar]
- 16.Weiss H.R., Bohr S., Jahnke A., Pleines S. Acupuncture in the treatment of scoliosis—a single blind controlled pilot study. Scoliosis. 2008;3:4. doi: 10.1186/1748-7161-3-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rubery P.T., Bradford D.S. Athletic activity after spine surgery in children and adolescents: results of a survey. Spine. 2002;27(4):423–427. doi: 10.1097/00007632-200202150-00019. [DOI] [PubMed] [Google Scholar]
- 18.Shands A.R., Barr J.S., Colonna P.C., Noall L. End-result study of the treatment of idiopathic scoliosis: report of the Research Committee of the American Orthopedic Association. J Bone Joint Surg. 1941;23-A(4):963–977. [Google Scholar]
- 19.Wood K.B. Spinal deformity in the adolescent athlete. Clin Sports Med. 2002;21(1):77–92. doi: 10.1016/s0278-5919(03)00058-9. [DOI] [PubMed] [Google Scholar]
- 20.Nestle M., Jacobson M.F. Halting the obesity epidemic: a public health policy approach. Public Health Rep. 2000;115(1):12–24. doi: 10.1093/phr/115.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Loud K.J., Micheli L.J. Common athletic injuries in adolescent girls. Curr Opin Pediatr. 2001;13(4):317–322. doi: 10.1097/00008480-200108000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Scherer R.W., Langenberg P., von Elm E. Full publication of results initially presented in abstracts. Cochrane Database Syst Rev. 2007;(2):MR000005. doi: 10.1002/14651858.MR000005.pub3. [DOI] [PubMed] [Google Scholar]
- 23.Dumville J.C., Petherick E.S., Cullum N. When will I see you again? The fate of research findings from international wound care conferences⁎. Int Wound J. 2008;5(1):26–33. doi: 10.1111/j.1742-481X.2007.00343.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Phillips B., Ball C., Sackett D., Badenoch D., Straus S., Haynes B. Oxford Centre for Evidence-Based Medicine levels of evidence. Centre for Evidence-Based Medicine; Oxford: 2001. [Google Scholar]
- 25.Parsch D., Gartner V., Brocai D.R., Carstens C., Schmitt H. Sports activity of patients with idiopathic scoliosis at long-term follow-up. Clin J Sport Med. 2002;12(2):95–98. doi: 10.1097/00042752-200203000-00005. [DOI] [PubMed] [Google Scholar]
- 26.Meyer C., Haumont T., Gauchard G.C., Leheup B., Lascombes P., Perrin P.P. The practice of physical and sporting activity in teenagers with idiopathic scoliosis is related to the curve type. Scand J Med Sci Sports. 2008 doi: 10.1111/j.1600-0838.2007.00750.x. [DOI] [PubMed] [Google Scholar]
- 27.Danielsson A.J., Romberg K., Nachemson A.L. Spinal range of motion, muscle endurance, and back pain and function at least 20 years after fusion or brace treatment for adolescent idiopathic scoliosis: a case-control study. Spine. 2006;31(3):275–283. doi: 10.1097/01.brs.0000197652.52890.71. [DOI] [PubMed] [Google Scholar]
- 28.Baker R.J., Patel D. Lower back pain in the athlete: common conditions and treatment. Prim Care. 2005;32(1):201–229. doi: 10.1016/j.pop.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 29.von Strempel A., Scholz M., Daentzer M. Sports capacity of patients with scoliosis. Sportverletz Sportschaden. 1993;7(2):58–62. doi: 10.1055/s-2007-993483. [DOI] [PubMed] [Google Scholar]
- 30.Fuchs P.D., Bertrand S., Iwinski H., Pellet J. Traumatic C6-C7 dislocation in a 14 year old with posterior spinal fusion for idiopathic scoliosis. J Trauma. 2001;51(5):1004–1007. doi: 10.1097/00005373-200111000-00030. [DOI] [PubMed] [Google Scholar]
- 31.Mallau S., Bollini G., Jouve J.L., Assaiante C. Locomotor skills and balance strategies in adolescents idiopathic scoliosis. Spine. 2007;32(1):E14–E22. doi: 10.1097/01.brs.0000251069.58498.eb. [DOI] [PubMed] [Google Scholar]
- 32.Tanchev P.I., Dzherov A.D., Parushev A.D., Dikov D.M., Todorov M.B. Scoliosis in rhythmic gymnasts. Spine. 2000;25(11):1367–1372. doi: 10.1097/00007632-200006010-00008. [DOI] [PubMed] [Google Scholar]
- 33.Kesten S., Garfinkel S.K., Wright T., Rebuck A.S. Impaired exercise capacity in adults with moderate scoliosis. Chest. 1991;99(3):663–666. doi: 10.1378/chest.99.3.663. [DOI] [PubMed] [Google Scholar]
- 34.Bridwell K.H. Surgical treatment of adolescent idiopathic scoliosis: the basics and the controversies. Spine. 1994;19(9):1095–1100. doi: 10.1097/00007632-199405000-00020. [DOI] [PubMed] [Google Scholar]
- 35.Hellstrom M., Jacobsson B., Sward L., Peterson L. Radiologic abnormalities of the thoraco-lumbar spine in athletes. Acta Radiol. 1990;31(2):127–132. [PubMed] [Google Scholar]
- 36.Sward L. The thoracolumbar spine in young elite athletes. Current concepts on the effects of physical training. Sports Med. 1992;13(5):357–364. doi: 10.2165/00007256-199213050-00005. [DOI] [PubMed] [Google Scholar]
- 37.Negrini S., Antonini G., Carabalona R., Minozzi S. Physical exercises as a treatment for adolescent idiopathic scoliosis. a systematic review. Pediatr Rehabil. 2003;6(3-4):227–235. doi: 10.1080/13638490310001636781. [DOI] [PubMed] [Google Scholar]
- 38.Lundin O., Hellstrom M., Nilsson I., Sward L. Back pain and radiological changes in the thoraco-lumbar spine of athletes. A long-term follow-up. Scand J Med Sci Sports. 2001;11(2):103–109. doi: 10.1034/j.1600-0838.2001.011002103.x. [DOI] [PubMed] [Google Scholar]
- 39.Weinstein S.L., Dolan L.A., Spratt K.F., Peterson K.K., Spoonamore M.J., Ponseti I.V. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA. 2003;289(5):559–567. doi: 10.1001/jama.289.5.559. [DOI] [PubMed] [Google Scholar]
- 40.Ogon M., Riedl-Huter C., Sterzinger W., Krismer M., Spratt K.F., Wimmer C. Radiologic abnormalities and low back pain in elite skiers. Clin Orthop Relat Res. 2001;(390):151–162. doi: 10.1097/00003086-200109000-00018. [DOI] [PubMed] [Google Scholar]
- 41.Smyth R.J., Chapman K.R., Wright T.A., Crawford J.S., Rebuck A.S. Ventilatory patterns during hypoxia, hypercapnia, and exercise in adolescents with mild scoliosis. Pediatrics. 1986;77(5):692–697. [PubMed] [Google Scholar]
- 42.Danielsson A.J., Wiklund I., Pehrsson K., Nachemson A.L. Health-related quality of life in patients with adolescent idiopathic scoliosis: a matched follow-up at least 20 years after treatment with brace or surgery. Eur Spine J. 2001;10(4):278–288. doi: 10.1007/s005860100309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kocher M.S., Sarwark J.F. What's new in pediatric orthopaedics. J Bone Joint Surg Am. 2004;86-A(6):1337–1346. doi: 10.2106/00004623-200406000-00033. [DOI] [PubMed] [Google Scholar]
- 44.Romano M., Negrini S. Does bracing change the sport habits of patients? A controlled study. Scoliosis. 2007;2(Suppl 1):S25. [Google Scholar]
- 45.Weiss H.R. Is there a body of evidence for the treatment of patients with adolescent idiopathic scoliosis (AIS)? Scoliosis. 2007;2:19. doi: 10.1186/1748-7161-2-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Engsberg J.R., Bridwell K.H., Reitenbach A.K., Uhrich M.L., Baldus C., Blanke K. Preoperative gait comparisons between adults undergoing long spinal deformity fusion surgery (thoracic to L4, L5, or sacrum) and controls. Spine. 2001;26(18):2020–2028. doi: 10.1097/00007632-200109150-00016. [DOI] [PubMed] [Google Scholar]
- 47.Mahaudens P., Thonnard J.L., Detrembleur C. Influence of structural pelvic disorders during standing and walking in adolescents with idiopathic scoliosis. Spine J. 2005;5(4):427–433. doi: 10.1016/j.spinee.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 48.Bunge E.M., Juttmann R.E., van Biezen F.C., Creemers H., Hazebroek-Kampschreur A.A., Luttmer B.C. Estimating the effectiveness of screening for scoliosis: a case-control study. Pediatrics. 2008;121(1):9–14. doi: 10.1542/peds.2006-3673. [DOI] [PubMed] [Google Scholar]
- 49.Hawes M.C. The use of exercises in the treatment of scoliosis: an evidence-based critical review of the literature. Pediatr Rehabil. 2003;6(3-4):171–182. doi: 10.1080/0963828032000159202. [DOI] [PubMed] [Google Scholar]
- 50.Hutchinson M.R. Low back pain in elite rhythmic gymnasts. Med Sci Sports Exerc. 1999;31(11):1686–1688. doi: 10.1097/00005768-199911000-00027. [DOI] [PubMed] [Google Scholar]
- 51.Lerman J.A., Sullivan E., Haynes R.J. The Pediatric Outcomes Data Collection Instrument (PODCI) and functional assessment in patients with adolescent or juvenile idiopathic scoliosis and congenital scoliosis or kyphosis. Spine. 2002;27(18):2052–2057. doi: 10.1097/00007632-200209150-00016. [discussion 2057-8] [DOI] [PubMed] [Google Scholar]
- 52.Weiss H.R. Rehabilitation of adolescent patients with scoliosis—what do we know? A review of the literature. Pediatr Rehabil. 2003;6(3-4):183–194. doi: 10.1080/13638490310001636790. [DOI] [PubMed] [Google Scholar]
- 53.Romano M., Carabalona R., Petrilli S., Sibilla P., Negrini S. Forces exerted during exercises by patients with adolescent idiopathic scoliosis wearing fiberglass braces. Scoliosis. 2006;1:12. doi: 10.1186/1748-7161-1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Institute for Clinical Systems Improvement . Institute for Clinical Systems Improvement; Bloomington (Minn): 2007. Preventive services for children and adolescents. [Oct 2007 ed] [Google Scholar]
- 55.American Academy of Family Physicians . American Academy of Family Physicians; Leawood (Ky): 2007. Summary of recommendations for clinical preventive services. [Revision 6.4] [Google Scholar]
- 56.Klein G.R., Levine B.R., Hozack W.J., Strauss E.J., D'Antonio J.A., Macaulay W. Return to athletic activity after total hip arthroplasty. Consensus guidelines based on a survey of the Hip Society and American Association of Hip and Knee Surgeons. J Arthroplasty. 2007;22(2):171–175. doi: 10.1016/j.arth.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 57.McKenzie J.F., Pinger R.F., Kotecki J.E. 6th ed. Jones and Bartlett; Sudbury (Mass): 2008. An introduction to community health. [Google Scholar]
- 58.Friis R.H., Sellers T.A. 3rd ed. Jones and Bartlett; Sudbury (Mass): 2004. Epidemiology for public health practice. [Google Scholar]


