Abstract
Objective
This case report describes the effect of exercise-based chiropractic treatment on chronic and intractable low back pain complicated by lumbar disk extrusion.
Clinical Features
A 47-year–old male firefighter experienced chronic, unresponsive low back pain. Pre- and posttreatment outcome analysis was performed on numeric (0-10) pain scale, functional rating index, and the low back pain Oswestry data. Secondary outcome assessments included a 1-rep maximum leg press, balancing times, push-ups and sit-ups the patient performed in 60 seconds, and radiographic analysis.
Intervention and Outcome
The patient was treated with Pettibon manipulative and rehabilitative techniques. At 4 weeks, spinal decompression therapy was incorporated. After 12 weeks of treatment, the patient's self-reported numeric pain scale had reduced from 6 to 1. There was also overall improvement in muscular strength, balance times, self-rated functional status, low back Oswestry scores, and lumbar lordosis using pre- and posttreatment radiographic information.
Conclusion
Comprehensive, exercise-based chiropractic management may contribute to an improvement of physical fitness and to restoration of function, and may be a protective factor for low back injury. This case suggests promising interventions with otherwise intractable low back pain using a multimodal chiropractic approach that includes isometric strengthening, neuromuscular reeducation, and lumbar spinal decompression therapy.
Key indexing terms: Occupational health, Intervertebral disk displacement, Chiropractic, Rehabilitation, Lordosis
Introduction
Occupation-related low back injury has a tremendous impact on the economy of the United States. Work-related low back injuries and illnesses are responsible for the highest dollar amount of compensation in US industry and are the most common causes of lost-time injury.1 Supervised exercise therapy has been recommended as a first line of treatment of chronic low back pain (CLBP) as well as spinal manipulative therapy (SMT).2 Multidisciplinary treatment emphasizing function-centered rehabilitation has also recently been shown to reduce lost work days when compared with patient-centered treatment.3 Recent literature discusses the safety and efficacy of conservative and surgical treatment of sudden-onset low back pain.4-6 Most (80%-90%) of the patients experiencing acute low back pain typically recover function and become pain-free, as a result of treatment or the passage of time, within 6 to 8 weeks.7
For treatment of CLBP, however, the prognosis is not as promising.8 Educational programs such as back schools have shown effectiveness with patients with recurrent and CLBP in various occupational settings.9 Exercise therapy has also been indicated as an effective method of treatment, but it is unclear which therapeutic option offers the most cost-effective outcome.10,11 There is also no conclusive evidence to support a specific type of exercise recommendation in cases of CLBP.12 Chronic low back pain often presents with one or more underlying factors, and each must be discovered and considered in the treatment plan.
Lumbar stabilization exercise programs have recently gained interest in the biomedical literature. Structural changes in disks, altered neuromuscular recruitment patterns, and/or decreased muscular endurance has been implicated as potential risk factors in patients with CLBP. A superior manual method to test potential risk factors such as decreased strength, coordination, and a neutral spinal position remains unclear in the literature.13 In this case, initial testing involved the application of an external head and shoulder weight to provide a beginning reference point with respect to a neutral spinal position and initial spinal stability. This testing process has been previously outlined in the literature.14,15 The patient also presented with several complicating factors, including a postsurgical procedure and lumbar transitional segment. Although the use of spinal decompression therapy (SDT) is controversial,16-18 the benefits for certain subgroups of patients with low back pain remain undetermined.17 Subgroups with lumbosacral transitional segments, for example, have been reported in 2% to 11.5% of the presenting cases of CLBP.19-22 No conclusive evidence has been reported that associates transitional segments as a cause of low back pain; but such a comorbidity may present clinical complications regarding chiropractic techniques used and require change, for example, in line of drive and force applied.23 There also has been an increased risk of disk protrusion or disk extrusion above the transitional L5 vertebra in patients with low back pain.24
This case report discusses the treatment and results with a patient who had experienced a failed trial of SMT with CLBP, right extremity pain, and transitional segment in an occupation requiring elevated physical fitness standards.
Case report
A 47-year–old firefighter, 5′8″ tall and weighing 200 lb, presented for treatment with chief complaints of low back pain, right buttock pain, right extremity paresthesias, and difficulty walking including climbing stairs. He reported he was fearful of an early exit from the firefighting profession due to a low back disability. The patient had a very active lifestyle before his injury, reporting exercising at least 4 to 5 times per week. His exercise routine consisted of 2 to 3 days of strength training alternating with some form of aerobic conditioning, including bike riding, kayaking, and using a stair mill. He described the lower back pain as deep and dull in nature, the right buttock pain as sharp, and the sensation in the right leg as pins and needles. He reported eliciting temporary relief from the lower back and buttock pain by placing his fist in the central portion of his lower back around the L3 through L5 vertebral level forcing his lower back into slight extension. The patient also had difficulty sleeping, reporting that he awakened at least once nightly because of radicular pain. At the time of presentation, the patient was not taking any over-the-counter or prescribed medication. He was applying cold packs occasionally. Eleven years before presentation, the patient had an L4-5 herniated disk with a gradual progression of symptoms over time, which resulted in a lumbar diskectomy at the involved level. He could not recall any trauma or any specific date that the symptoms began. The patient experienced relief of radicular symptoms within days after the surgery; and for approximately 7 years after surgery, his radicular symptoms remained virtually nonexistent. However, within the past 4 years, he reported an increasing number of episodes, reporting 3 to 4 within the last year. The radicular symptoms were managed symptomatically with conventional chiropractic management consisting of high-velocity, low-amplitude (HVLA) SMT, typically resolving within 2 to 3 weeks of treatment. The patient had also experienced CLBP starting approximately 15 years ago with progressive worsening of symptoms over the past 4 years. The CLBP was virtually unresponsive to the surgical procedure or previous chiropractic management.
Five weeks before presentation, the patient injured himself while shoveling snow and sought care from his previous chiropractor. Recent radiographs were not available; however, a records request from the previous chiropractor determined that his care consisted of HVLA side-lying manipulation along with diversified manipulative techniques for the cervical and thoracic spine, with no reduction of symptoms for 4 weeks at a frequency of 2 times per week. The radicular symptoms and associated sensorimotor deficits did not resolve and were not contraindicated in the 5-week period. At the time of presentation, the patient reported on the Oswestry outcome assessment form, “My pain is neither getting better nor worse,” with respect to changing pain levels. His low back Oswestry score was a 21/50 at the time of presentation to this office.
Magnetic resonance imaging was ordered by this office, which revealed a large right lateral disk extrusion at the L4-5 intervertebral level that completely effaced the lateral foramen. At this clinic, several forms and rating scales were used to evaluate and grade patient progress. Numeric pain scale (NPS) was recorded weekly, whereas functional rating index and a low back Oswestry were completed at 4-week intervals (Table 1). Initially, his self-rated NPS pain score was 6 on the 11-point, 0 to 10 scale; his functional rating index score was 17 (42% disability); and his low back Oswestry score was 21 (severe disability). Straight leg raise test result was positive on the right at 55° for right extremity radiculopathy consistent with L5 and partial S1 nerve root encroachment at the lateral one-third dorsum of the foot. Sensory testing revealed hypoesthesia to light and sharp touch over the anterolateral aspect of the right calf extending to the dorsum of the foot between the first and second metatarsal. Achilles reflexes were diminished bilaterally, +1. Although the patient reported weakness with certain movements, muscle strength testing revealed the lower extremities to be equal and full bilaterally. Heel and toe walk was performed with moderate difficulty due to acute low back pain and radicular pain in the L5/S1 nerve root distribution. Thoracolumbar range of motion was markedly limited in flexion, and mild limitations were noted in lateral flexion and rotation. A visual postural examination revealed a high right shoulder, high left iliac crest, mild antalgic forward and right upper body lean, and anterior head carriage. Postural analysis was also used here as a preliminary screening measure for radiographic studies. Palpatory examination revealed an active trigger point at the right piriformis muscle, right side paravertebral myospasm, and palpable tenderness at the L5 spinous process. The Sorenson test result was positive, with the patient performing prone lumbar extension for 38 seconds before failure, suggesting weak lumbar paraspinal musculature. Pain mildly altered the patient's gait, causing a limp on the right extremity with failure to fully extend the right leg. The patient's diagnosis included L4/L5 right lateral disk extrusion, sciatica at the L5 and partial S1 nerve root distribution, and lumbar sprain/strain.
Table 1.
Summary of self-rated pain, function, and disability findings
| Week | NPS Score | FRI | Low Back Oswestry |
|---|---|---|---|
| 1 | 6 | 21 | 43% |
| 2 | 6 | ||
| 3 | 5 | ||
| 4 | 8 | 19 | 40% |
| 5 | 7 | ||
| 6 | 6 | ||
| 7 | 6 | ||
| 8 | 3 | 11 | 30% |
| 9 | 3 | ||
| 10 | 3 | ||
| 11 | 2 | ||
| 12 | 1 | 5 | 15% |
FRI, Functional rating index.
Cervical and lumbar radiographs were taken initially in both the anteroposterior and lateral views to quantify the configuration of the cervical and lumbar spine initially. This case, however, only reports on the lumbar radiographic evaluation. The radiographic procedures used here were consistent with those outlined by Jackson et al.25 Evaluation of the plain films revealed a transitional segment at L5 with a decrease in disk height at L4/L5, mild lumbar levoscoliosis, and a reduced lumbar lordosis. Initially, the lumbar lordosis measured 12° and the sacral base angle (Ferguson angle) measured 32° (Fig 1). Secondary outcome assessments included pre-and posttreatment lateral lumbar radiographic analysis and several specific muscle testing requirements. At baseline, the patient was asked to record his 1-rep maximum leg press performed on a seated leg press machine measured by a Fitlinxx26 software program (Fitlinxx, Norwalk, CT). Additional testing procedures were instructed by the licensed chiropractor with expertise in such assessment and were witnessed and recorded by a chiropractic assistant. These data included the number of push-ups and sit-ups the patient could perform in 60 seconds and balancing times on a Posturomed (Haider Bioswing, Bavaria, Germany).27 The results of the fitness testing are illustrated in Table 2 and Fig 3. At baseline, the patient was instructed to discontinue any muscle strength training regimen. The patient was tested by the author both pre- and posttreatment with exactly the same instructions while observing for faulty movements during the testing process. He also was asked to complete a questionnaire to assess various lifestyle variables—initially at baseline and then at 3-month intervals for approximately 1 year to determine the effectiveness of this treatment regimen. Treatment goals were designed to address quickly and effectively the multitude of contributory factors commonly witnessed in cases of CLBP. In this case, treatment focused on decreasing pain, improving spinal balance and proprioception, reducing asymmetrical spinal loading, enhancing muscular endurance strength, and educating the patient on proper body mechanics with his daily living and required occupational activities.
Fig 1.
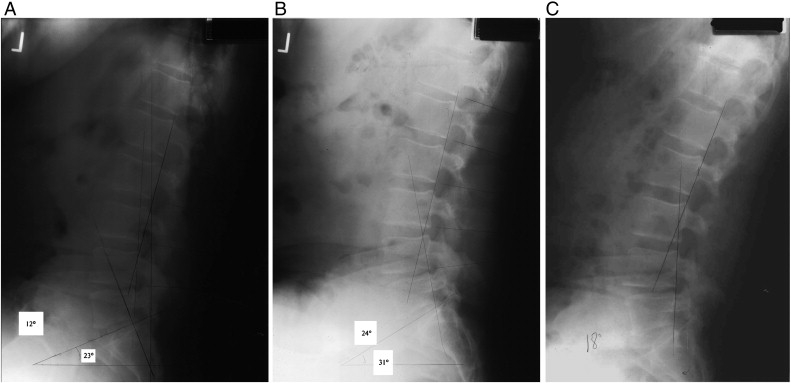
A to C, This figure shows the pre- and posttreatment lateral lumbar radiographs. This patient, after 36 visits in 12 weeks, obtained an apparent 12° increase in lumbar lordosis when measured from the posterior aspect of the L1 and L5 vertebral bodies.
Table 2.
Summary of pre- and posttreatment muscle strength/endurance testing
| Baseline | 90 d | ||
|---|---|---|---|
| Muscle Strength | Leg Press | 430 lb | 450 lb |
| Endurance (60 s) | Push-Ups | 50 Reps | 54 Reps |
| Sit-Ups | 31 Reps | 42 Reps |
Fig 3.
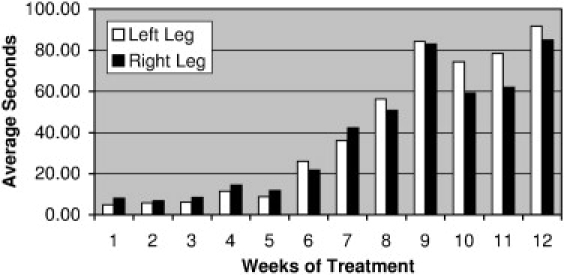
This figure illustrates the balancing times with the patient's eyes open on each leg while wearing a 4-lb head weight and 8-lb shoulder weight throughout the course of treatment. This procedure was performed after each manipulative and/or lumbar spine decompression treatment. Despite reinjury at the conclusion of week 4, the patient's balancing times improved overall.
The patient was treated 3 times weekly for the first 4 weeks of care. Office visits began with motion-based therapy (MBT) exercises on a Pettibon Wobble Chair (PWC) (Pettibon Institute, Gig Harbor, WA) for 4 minutes with an emphasis on left side lateral flexion of the lumbodorsal spine. Warm-up procedures were followed by SMT, neuromuscular reeducation, muscle stretching/strengthening on a Pettibon Linked Trainer (PLT) (Pettibon Institute), and positional traction. The PWC has been previously outlined in the literature.28-31 Spinal manipulative procedures were performed in accordance with the radiographic findings and consisted of anterior dorsal mobilization from the seventh through 11th thoracic vertebrae, cervical distractive adjustment at the level of the fifth and sixth cervical vertebrae in the y-axis, and mobilization of the level of the occiput and first cervical vertebra with a drop piece mechanism in the negative z-axis. A bilateral side posture lumbopelvic adjustment was also performed to mobilize the lumbosacral joints. The goal of the manipulative procedures has been previously reported in a comprehensive spine care setting.28,29,31,32 Spinal manipulative procedures were implemented at a frequency of 1 time per week beginning the first month and continued through the 12 weeks of treatment. Immediately after the first trial of manipulative procedures, the patient was fitted with a 4-lb anterior head weight and an 8-lb left external shoulder weight and instructed to walk while wearing the weights for 10 minutes. After walking with the anterior head weight and shoulder weight, a lateral lumbar stress radiograph was taken to predetermine the effectiveness of restoring a more normal lumbar lordosis (Fig 3).
Specific exercises performed on the PLT were predetermined from radiographic analysis and have been used in the past in a comprehensive approach to spinal disorders.28,32 Neuromuscular reeducation was incorporated through PWC exercises with head and shoulder weight and balancing on a Posturomed27 with 1 leg while wearing a head and shoulder weight. The patient did this with eyes open and closed during this treatment and was timed weekly with his eyes open, and the data are reported in Fig 2. The timer started upon lifting the leg and stopped when the body noticeably leaned or if the elevated leg touched the platform. After 3 trials, the average time registered was 4.5 seconds on the left leg and 8 seconds on the right leg. The goal of this exercise was to improve the patient's postural stability, with the patient ideally being able to stand on each leg for a greater length of time as active adaptive learning occurred over the course of treatment. Spinal manipulative therapy and active rehabilitative procedures were followed by a cool-down session of left side-lying lumbar spinal molding on a high-density foam roll for a total of 8 minutes.
Fig 2.
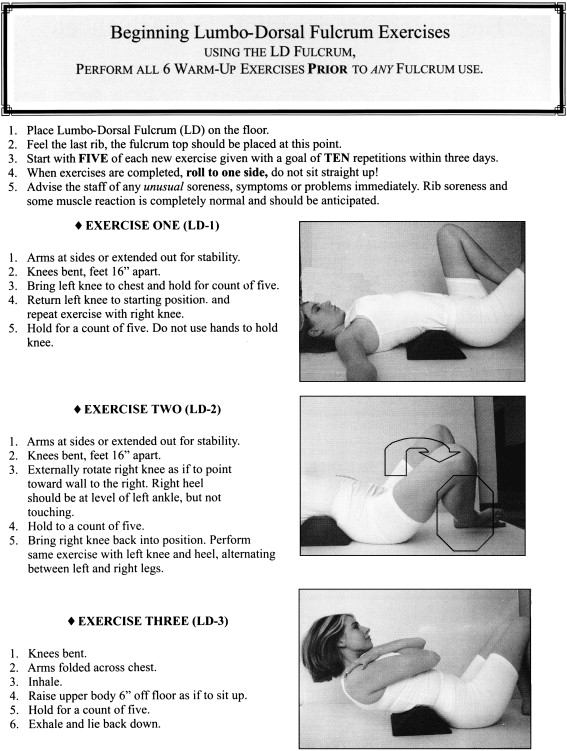
This figure is an illustration of the beginning lumbodorsal fulcrum exercises. The apex of the fulcrum is placed just below the last rib. These exercises were also performed in the at-home setting.
At home, rehabilitative therapy consisted of PWC exercises with the head and shoulder weight to be performed twice daily for 15 minutes per session. Just before the conclusion of the first month of care, the patient subjectively reported that his presenting complaints had improved 25%. However, at the end of the fourth week of care, the patient reinjured himself when he lifted a catalytic converter at work. The patient's symptomatology was worse than the initial visit, with his self-rated NPS score increasing to 8/10; however, orthopedic and neurologic examinations remained unchanged (Table 1).
At this time, the patient was emotionally fatigued, stating he felt “handicapped” as a result of his low back issues. A neurosurgical consult was ordered, and he was determined to be a surgical candidate. Given the relatively short trial of conservative treatment, however, the neurosurgeon supported another 4 to 6 weeks of trial unless neurologic deficits progressed or pain was refractory to treatment. After a second opinion, the patient elected to try another trial of chiropractic management described previously, as well as a trial of lumbar SDT with an attempt to reduce symptomatology and avoid a second diskectomy. Spinal decompression therapy was not used for the first 4 weeks because the patient was gradually improving and given the lack of literature supporting its effectiveness as compared with spinal manipulation, medication, exercise, etc.16,17
In this case, SDT was used with a Triton Decompression Therapy System (Chattanooga, Hexton, TN) with the patient in a supine position and the legs elevated to patient comfort (approximately 65° to the horizontal) under 2 rubber supports. The SDT treatment was derived from standardized traction settings and consisted of a 5-minute warm-up and 5-minute cool down with a 15-minute intermittent traction setting. Maximum traction poundage used was derived from a formula taking one half of the patient's body weight and then subtracting 10. The minimum poundage used was derived from calculating approximately 20% of the maximum traction weight. The SDT was implemented at a frequency of 3 times per week for the second 4 weeks.
At the conclusion of the sixth week of care, the PLT was reintroduced; and the patient was instructed in a beginning fulcrum exercise program (Pettibon Institute), as shown in Fig 3. The 3 levels of fulcrum exercises are beginning, intermediate, and advanced, with patient progression in levels after achieving the ability to complete 10 repetitions maintaining an isometric contraction for a 5-second count. The lumbar lordosis may also be enhanced as the patient progresses through the levels. The goal of the fulcrum exercises is to provide a sustained stretch and compressive force to rehabilitate the paravertebral supportive soft tissue of the spine.
The patient rapidly improved under this treatment plan, reporting at the end of the 8 weeks of treatment that he was 50% improved from his initial presentation. The NPS score (0-10) at week 8 was reported to be a 3 by the patient. At this time, the patient was very pleased with the results and elected for another 4-week trial of care. For the remaining 4 weeks, treatment stayed the same with the exception of the advancement in fulcrum exercise levels and reduction in frequency of SDT to 1 time per week. At 8 weeks, the patient progressed to intermediate lumbodorsal fulcrum exercises and, at 10 weeks, began the advanced level until completion at 12 weeks.
At the end of 90 days, the patient was essentially fully recovered. He reported mild episodic pain in the right buttock with no reported limitations on activities. The NPS score varied throughout treatment; however, it was rated at 6/10 on the first visit and at 1/10 at the conclusion of treatment. Functional rating index score improved from 17 to 6 (15% disability) and low back Oswestry from 21 to 5 (minimal disability) at the end of this treatment trial. Average balance times improved from an initial average of 4.5 seconds on the left leg and 8 seconds on the right leg to 91.5 left-leg seconds and 85 right-leg seconds, respectively. Radiographic analysis revealed an overall improvement of lumbar lordosis from 12° to 24°. Muscle testing revealed an improvement of muscular endurance, with the patient performing an additional 4 push-ups and 11 sit-ups in a 60-second timeframe, and a 20-lb increase in a 1-rep maximum leg press. At the end of the 90 days, reexamination revealed a negative straight leg raise test result with no reduction in thoracolumbar range of motion. Achilles reflexes were equal and active bilaterally, +2. Mild hypoesthesia was noted along the lateral aspect of the right ankle localized to the lateral malleolus. The Sorenson test result was also negative, which the patient was able to perform for more than 60 seconds. Upon completion of the treatment program, the patient was instructed to continue with the head and body weighting procedures at home and advanced fulcrum exercises at a frequency of 1 time per week for the next 9 months.
Discussion
This case reports on the successful treatment of a patient with CLBP and right leg pain in an occupation requiring an elevated level of physical fitness using a multimodal chiropractic management approach. In this case, risk factors were assessed at baseline to determine appropriate candidacy for this exercise program as well as an initial starting point. Chiropractic physicians need to consider emphasizing a multidisciplinary treatment or a comanagement approach given the evidence of the multifactorial nature of CLBP.
Short-term management focused on pain relief because duration of symptoms has also been implicated as a prognostic factor in outcomes of patients with CLBP.33 Symptom relief was emphasized through treatment of the large disk extrusion and associated symptomatology primarily through MBT, SDT, and SMT. Spinal decompression therapy has been shown to reduce pressure of the nucleus pulposus34 and possibly change the disk-nerve interface.35 Because NPS and low back Oswestry scores were reduced overall throughout the treatment, it seems that the cumulative effects of these modalities may have largely contributed to the reduction in pain. Deficits in neuromuscular control often found in cases of CLBP may explain why some individuals are more susceptible to disk degeneration due to altered mechanical loading.36 Because it is doubtful that any mechanical changes of the disk are maintained after the patient assumes an upright position, SDT was combined with active therapeutic intervention. One of these includes MBT of the lumbosacral spine to initiate and maintain effects of SDT through use of the PWC.
The multimodal management used in this case, including MBT, SDT, and SMT, was prescribed in a specific order to enable the subsequent rehabilitative procedures to have a more profound effect. The thought process behind this is that each modality prepares the appropriate spinal segment, region, etc, for the next procedure, which enhances effects of each subsequent procedure. Rationale for this management approach has been recently supported in the literature. Spinal manipulative therapy, although effective at activating superficial muscles, has not been shown to activate deeper trunk muscles such as the transverse abdominals.37 Thus, harnessing the immediate effects of SMT was accomplished through application of specific deep trunk muscle exercises to promote intervertebral stability. The results witnessed here concur with other findings indicating that trunk-strengthening exercises after a lumbar disk surgery are more effective at reducing pain and improving function when compared with no exercise at all.38
Spinal manipulative therapy procedures used in this case were correlated with radiographic line analysis, transitional segment, and the patient's presentation and were consistent with the manipulative procedures taught within the Pettibon curricula.39 Noteworthy to this patient's case was that he was misdiagnosed while under previous chiropractic care with a piriformis syndrome, and disk pathology was not suspected. Side posture HVLA is the most common treatment modality used by chiropractors,40,41 as was the initial care in this case. Therefore, it is questionable as to whether other techniques would have been used had a pathologic disk been suspected regardless of the primary diagnosis. Although previous chiropractic management had not been successful, it also seemed not to be contraindicated with side posture HVLA. The manipulative procedures performed on the cervical and dorsal spine may have also influenced the outcomes witnessed here; however, the patient was receiving SMT at these regions before presenting at this office. The narrative design of this report and the fact that the focus is on 1 patient do not allow these results to be definitively generalized to the general population or even to the population of firefighters with intractable back pain. This report does include diagnostic and evaluative measures, however, to help clinicians decide if such treatment given the patient in this research might also be relevant to similar patients under their care. Furthermore, this single case, as all single-group designs, lacks a matched individual or a randomly assigned group to which a waiting-list no-treatment “control” treatment might have been assigned to isolate the effects of treatment and the effects of the simple passage of time and the body's natural healing processes. Readers should also not discount the possible benefit due to the patient's belief that care would be successful.
As a result, the subjective and objective improvements the patient experienced cannot be directly attributable to the treatment procedures outlined. Although pain reduction and functional improvements were evident at the conclusion of treatment, it is unclear if time alone would have produced a similar outcome due to the natural history of disk herniations.42 Nevertheless, because the patient had previously experienced months of back pain and treatment without substantial benefit before the most recent and successful course of treatment was offered, and if “all other factors were otherwise unchanged,” some benefit of the current protocol might be inferred. This patient was also very compliant with the home care procedures, with a self-rated 90% compliance rate. At least 2 other conservative modalities may have been provided but were not available in this setting. These include Cox flexion-distraction43 and Harrison lumbar extension traction.44 However, with a reduced lumbar lordosis such as here, Cox flexion-distraction may have been a contraindication as reported by Harrison and Harrison45; and there was no retrolisthesis present.
This patient remains an active full-time firefighter and is being monitored at 3-month intervals for the next year through questionnaires to determine the long-term effectiveness of this treatment regimen.
Conclusion
The patient obtained both subjective and functional improvement using a comprehensive management approach including the incorporation of a fulcrum exercise protocol, which to the author's knowledge has not been outlined in any previous literature. Treatment included SMT, SDT, specific muscle strengthening/stretching exercises, motion-based therapy, neuromuscular reeducation, and education on maintaining proper posture.
Pre- and posttreatment outcome measures were used here to evaluate a comprehensive rehabilitative approach to improve patient function. Outcome measures included the NPS scale, low back Oswestry, functional rating index, radiograph analysis, muscular strength/endurance, lumbar lordosis, and balance. All of the predefined outcome measures improved; and, at least temporarily, surgery was avoided. These outcome measures allowed a viable means of evaluating patient progress as well as demonstrating the possible effects of a specific exercise program to enhance physical fitness levels.
This case supports the premise that a multimodal rehabilitative protocol with proper diagnosis and careful consideration of sagittal lordosis, faulty biomechanics, postural abnormalities, and predetermined occupational risk factors may have clinical and economical value to professions such as firefighters, bus drivers, police officers, emergency medical service workers, and other service-oriented professionals. The collaboration of other health professionals such as the neurosurgeon was quite helpful and should be recognized for others recommending multidisciplinary management plans. The improvement of physical fitness and reduction of patient symptomatology provided useful clinical information in this case and should be further investigated in chiropractic cases.
References
- 1.Bureau of Labor Statistics A. United States Department of Labor; Washington (DC): 2003. Workplace injury and illness summary: workplace injuries and illness in 2002. [Google Scholar]
- 2.Airaksinen O., Brox J.I., Cedraschi C. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006;15:S192–S300. doi: 10.1007/s00586-006-1072-1. [Chapter 4] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kool J., Bachmann S., Oesch P., Knuesel O., Ambergen T., Bic R. Function-centered rehabilitation increases work days in patients with nonacute nonspecific low back pain: 1-year results from a randomized controlled trial. Arch Phys Med Rehabil. 2008;88:1089–1094. doi: 10.1016/j.apmr.2007.05.022. [DOI] [PubMed] [Google Scholar]
- 4.Memmo A.P., Nadler S., Malnga G. Lumbar disc herniations: a review of surgical and non-surgical indications and outcomes. J Back Musculoskelet Rehabil. 2000;14:79–88. [Google Scholar]
- 5.Lisi J.A., Holmes J.E., Ammendolia C. High-velocity low-amplitude spinal manipulation for symptomatic lumbar disk disease. A systematic review of the literature. J Manipulative Physiol Ther. 2005;6:429–442. doi: 10.1016/j.jmpt.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 6.Santilli V., Beghi E., Finucci S. Chiropractic manipulation in the treatment of acute back pain and sciatica with disc protrusion: a randomized double-blind clinical trial of active and simulated spinal manipulations. Spine J. 2006;6:131–137. doi: 10.1016/j.spinee.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 7.Ljunggren A.E. Natural history and clinical role of the herniated disc. In: Wiesel S.W., Weinstein J.N., Herkowitz H.N., editors. The lumbar spine. 2nd ed. WB Saunders; Philadelphia (Pa): 1996. pp. 473–491. [Google Scholar]
- 8.Carey T.S., Garrett J.M., Jackson A.M. Beyond the good prognosis. Examination of an inception cohort of patients with chronic low back pain. Spine. 2000;25:115–120. doi: 10.1097/00007632-200001010-00019. [DOI] [PubMed] [Google Scholar]
- 9.Klaber-Moffett J., Chase S., Portek I., Ennis J. A controlled prospective study to evaluate the effectiveness of a back school in the relief of chronic low back pain. Spine. 1986;11:120–122. doi: 10.1097/00007632-198603000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Slade C.S., Keating L.J. Trunk-strengthening exercises for chronic back pain: a systematic review. J Manipulative Physiol Ther. 2006;29:163–173. doi: 10.1016/j.jmpt.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 11.Aure F.O., Nilsen H.J., Vasseljen O. Manual therapy and exercise therapy in patients with chronic low back pain. Spine. 2003;28:525–532. doi: 10.1097/01.BRS.0000049921.04200.A6. [DOI] [PubMed] [Google Scholar]
- 12.Petersen T., Larsen K., Jacobsen S. One-year follow-up comparison of the effectiveness of McKenzie treatment and strengthening training for patients with chronic low back pain. Spine. 2007;32:2948–2956. doi: 10.1097/BRS.0b013e31815cda4a. [DOI] [PubMed] [Google Scholar]
- 13.Barr K.P., Griggs M., Cadby T. Lumbar stabilization: a review of core concepts and current literature, part 2. Am J Phys Med Rehabil. 2007;86:72–80. doi: 10.1097/01.phm.0000250566.44629.a0. [DOI] [PubMed] [Google Scholar]
- 14.Saunders E.S., Woggon D., Cohen C. Improvement of cervical lordosis and reduction of forward head posture with anterior headweighting and proprioceptive balancing protocols. J Vertebral Subluxation Res. 2003;4:E1–E5. [Google Scholar]
- 15.Morningstar M.W., Strauchman M.N., Weeks D.A. Spinal manipulation and anterior headweighting for the correction of forward head posture and cervical hypolordosis: a pilot study. J Chiropr Med. 2003;2:51–54. doi: 10.1016/S0899-3467(07)60042-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Daniel M.D. Non-surgical spinal decompression therapy: does treatment support efficacy claims made in the advertising media. Chiropr Osteopat. 2007;15:7. doi: 10.1186/1746-1340-15-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gay R., Brault J. Evidence-informed management of chronic low back pain with traction therapy. Spine J. 2008;8:234–242. doi: 10.1016/j.spinee.2007.10.025. [DOI] [PubMed] [Google Scholar]
- 18.Clarke J., Tulder M., Blomberg S., Vet H., Heijden G., Bronfort G. Traction for low back pain with or without sciatica: an updated systematic review within the framework of the Cochrane collaboration. Spine. 2006;31:1591–1599. doi: 10.1097/01.brs.0000222043.09835.72. [DOI] [PubMed] [Google Scholar]
- 19.Elster A.D. Bertolotti's syndrome revisited: transitional vertebrae of the lumbar spine. Spine. 1989;14:1373–1377. [PubMed] [Google Scholar]
- 20.Tini P.G., Wieser C., Zinn W. The transitional vertebra of the lumbar spine: its radiological classification, incidence, prevalence and clinical significance. Rheumatol Rehabil. 1977;16:180–185. doi: 10.1093/rheumatology/16.3.180. [DOI] [PubMed] [Google Scholar]
- 21.Hsieh C.J., Vanderford J.D., Moreau S.R., Prong T. Lumbosacral transitional segments: classification, prevalence and effect on disc height. J Manipulative Physiol Ther. 2000;23:483–489. doi: 10.1067/mmt.2000.108817. [DOI] [PubMed] [Google Scholar]
- 22.Leboeuf C., Kimber D., White K. Prevalence of spondylolisthesis, transitional anomalies and low intercrestal line in a chiropractic patient population. J Manipulative Physiol Ther. 1989;12:200–204. [PubMed] [Google Scholar]
- 23.Beck W.R., Holt R.K., Fox A.M., Hurtgen-Grace L.K. Radiographic anomalies that may alter chiropractic intervention strategies found in a New Zealand population. J Manipulative Physiol Ther. 2004;27:554–559. doi: 10.1016/j.jmpt.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 24.Castellvi A., Goldstein L., Chan D. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine. 1984;9:493–495. doi: 10.1097/00007632-198407000-00014. [DOI] [PubMed] [Google Scholar]
- 25.Jackson B.L., Barker W.F., Pettibon B.R. Reliability of the Pettibon patient positioning system for radiographic production. J Vertebral Sublux Res. 2000;4:1. [Google Scholar]
- 26.Annesi J.J. Effects of computer feedback on adherence to exercise. Percept Mot Skills. 1998;87:723–730. doi: 10.2466/pms.1998.87.2.723. [DOI] [PubMed] [Google Scholar]
- 27.Muller O., Gunther M., Krauss I., Horstmann T. Physical characteristics of the therapeutic device Posturomed as a measuring device-presentation of a procedure to characterize balancing ability. Biomed Tech (Berl) 2004;49:56–60. doi: 10.1515/BMT.2004.011. [DOI] [PubMed] [Google Scholar]
- 28.Morningstar M. Strength gains through lumbar lordosis restoration. J Chiropr Med. 2003;2:137–141. doi: 10.1016/S0899-3467(07)60077-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morningstar M.W., Woggon D., Lawrence G. Scoliosis treatment using a combination of manipulative and rehabilitative therapy: a retrospective case series. BMC Musculoskelet Disord. 2004;5:32. doi: 10.1186/1471-2474-5-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morningstar M., Pettibon B.R., Remz C. Neurospinal biomechanics. In: Savitz M.H., Chin J.C., Rauschning W., Yeung A.t., editors. The practice of minimally invasive spinal technique. AAMISS Press; New York: 2005. pp. 224–236. [Google Scholar]
- 31.Morningstar M. Improvement of lower extremity electrodiagnostic findings following a trial of spinal manipulation and motion-based therapy. Chiropr Osteopat. 2006;14:20. doi: 10.1186/1746-1340-14-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Morningstar M.W., Joy T. Scoliosis treatment using spinal manipulation and the Pettibon weighting system: a summary of 3 atypical presentations. Chiropr Osteopat. 2006;14:1. doi: 10.1186/1746-1340-14-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Radke M.B., Boissonnault W.G. Changes in disability following physical therapy intervention for patients with low back pain: dependence on symptom duration. Arch Phys Med Rehabil. 2006;87:749–756. doi: 10.1016/j.apmr.2006.02.033. [DOI] [PubMed] [Google Scholar]
- 34.Gudavalli M.R., Cox J.M., Baker J.A., Cramer G., Patwardian A.G. Intervertebral disc pressure changes during a chiropractic procedure. Adv Bioeng. 1997;36:215–216. [Google Scholar]
- 35.Knutsson E., Skoglund C.R., Natchev E. Changes in voluntary muscle strength, somatosensory transmission and skin temperature concomitant with pain relief during autotraction in patients with lumbar and sacral root lesions. Pain. 1988;33:173–179. doi: 10.1016/0304-3959(88)90088-7. [DOI] [PubMed] [Google Scholar]
- 36.Stokes I., Iatridis J. Mechanical conditions that accelerate intervertebral disc degeneration: overload versus immobilization. Spine. 2004;29:2724–2732. doi: 10.1097/01.brs.0000146049.52152.da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ferreira M., Ferreira P., Hodges P. Changes in postural activity of the trunk muscles following spinal manipulative therapy. Man Ther. 2007;12:240–248. doi: 10.1016/j.math.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 38.Twomey L., Taylor J. Spine update. Exercise and spinal manipulation in the treatment of low back pain. Spine. 1995;20:615–619. doi: 10.1097/00007632-199503010-00021. [DOI] [PubMed] [Google Scholar]
- 39.Pettibon B.R. Pettibon Institute; Gig Harbor (Wash): 2005. Chiropractic and rehabilitation procedures re-invented to correct the spine and posture. [Google Scholar]
- 40.Meeker W.C., Haldeman S. Chiropractic: a profession at the crossroads of mainstream and alternative medicine. Ann Intern Med. 2002;136:216–227. doi: 10.7326/0003-4819-136-3-200202050-00010. [DOI] [PubMed] [Google Scholar]
- 41.Christensen M.G., Kerkhoff D., Kollasch M.W. Job analysis of chiropractic 2000. National Board of Chiropractic Examiners; Greeley (Colo): 2000. p. 129. [Google Scholar]
- 42.Benoist M. The natural history of lumbar disc herniation and radiculopathy. Joint Bone Spine. 2002;69:155–160. doi: 10.1016/s1297-319x(02)00385-8. [DOI] [PubMed] [Google Scholar]
- 43.Cox J.M., Shreiner S. Chiropractic manipulation in low back pain and sciatica: statistical data on the diagnosis, treatment and response of 576 consecutive cases. J Manipulative Physiol Ther. 1984;7:1–11. [PubMed] [Google Scholar]
- 44.Harrison D.E., Calliet R., Harrison D.D., Janik T.J., Holland B. Changes in sagittal lumbar configuration with a new method of extension traction: non-randomized clinical control trial. Phys Med Rehabil. 2002;83:1585–1591. doi: 10.1053/apmr.2002.35485. [DOI] [PubMed] [Google Scholar]
- 45.Harrison D.E., Harrison D.D. Letter response to Dr. Cox part II. J Manipulative Physiol Ther. 1984;7:1–11. [PubMed] [Google Scholar]


