Abstract
Physical methods of gene (and/or drug) transfer need to combine two effects to deliver the therapeutic material into cells. The physical methods must induce reversible alterations in the plasma membrane to allow the direct passage of the molecules of interest into the cell cytosol. They must also bring the nucleic acids in contact with the permeabilized plasma membrane or facilitate access to the inside of the cell. These two effects can be achieved in one or more steps, depending upon the methods employed. In this review, we describe and compare several physical methods: biolistics, jet injection, hydrodynamic injection, ultrasound, magnetic field and electric pulse mediated gene transfer. We describe the physical mechanisms underlying these approaches and discuss the advantages and limitations of each approach as well as its potential application in research or in preclinical and clinical trials. We also provide conclusions, comparisons, and projections for future developments. While some of these methods are already in use in man, some are still under development or are used only within clinical trials for gene transfer. The possibilities offered by these methods are, however, not restricted to the transfer of genes and the complementary uses of these technologies are also discussed. As these methods of gene transfer may bypass some of the side effects linked to viral or biochemical approaches, they may find their place in specific clinical applications in the future.
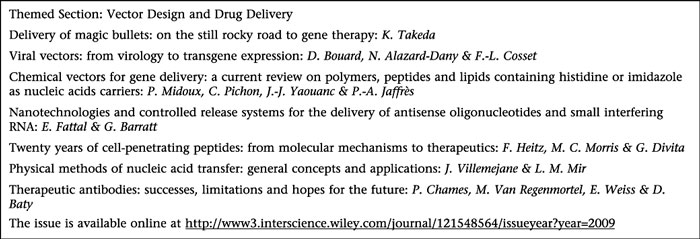
This article is part of a themed section on Vector Design and Drug Delivery. For a list of all articles in this section see the end of this paper, or visit: http://www3.interscience.wiley.com/journal/121548564/issueyear?year=2009
Keywords: gene gun, jet injection, hydrodynamic gene transfer, electro-gene therapy, electro-transfer, sonotransfection, magnetotransfection, naked DNA, cell permeabilization
Introduction
The existence of therapeutic targets located within cells has been known for decades. Most of the traditional anti-cancer drugs (still extensively used in chemotherapy) have intracellular targets, such as the cell DNA or the enzymes of the DNA synthesis pathways. These drugs easily enter cells, mainly due to their small size and physicochemical characteristics. Advances in understanding of many diverse intracellular mechanisms, such as signalling pathways, intracellular regulatory pathways through siRNAs, the identification of genes responsible for severe diseases etc., have identified new intracellular targets and novel therapeutic molecules are currently under development, including complete genes. Many of these molecules are nucleic acids, and they are not able to diffuse through the plasma membrane due to their size and/or their physicochemical properties, for instance hydrophilicity. The therapeutic expectations of gene therapy are considerable. The goal of curing genetic diseases by the transfer of genes coding for functional proteins absent in specific patients is highly desirable. Moreover, the use of gene-transfected cells to produce large quantities of secreted proteins for direct therapeutic application or for the production of vaccines is also of considerable benefit. Strategies for the transfer of nucleic acids, especially genes, have been developed. These strategies include the use of viral vectors, chemical vectors and physical vectors. The physical vectors allow the direct penetration into the cytosol of both small and large nucleic acid molecules, as well as of any other non-permeable molecule, which normally cannot reach the cell cytosol because it can not diffuse through the plasma membrane or because it is not actively transported across the plasma membrane.
Viral vectors are extremely effective in transferring genes and are the most advanced in development. The efficacy with which these agents affect DNA transfer, particularly in vivo, is due to their efficiency and specificity in entering cells and expressing the genes carried in the modified viral genome using the cell's own biosynthetic machinery. Unfortunately, there are well-known adverse effects, such as the immunogenicity of the adenoviral vectors, as well as potential and real risks associated with the use of such viruses, including cell transformation (by insertional mutagenesis with retroviruses), cancer development, etc.
On the other hand, physical and chemical methods of targeting also allow the transfer of long and short nucleic acids, DNA or RNA, across the cell membrane. Physical methods, that is non-viral and non-chemical, can bypass many of the side effects linked to viral or biochemical techniques, and they allow repeated administration of drugs or DNA. Another advantage is that, contrary to the situation with the viral vectors and some chemical vectors, there is no limitation in the length of the coding sequence that can be carried by the physical vectors.
The biggest challenge for these physical approaches is to attain the same efficiency of gene transfer as the viral methods. All the gene transfer methods (viral or non-viral) must overcome two major constraints
First, there is the need to bring the nucleic acids to the target cells. Viruses are ‘naturally’ equipped for such encounters. The more ‘intelligent’ chemical vectors, which are ‘stealthy’ with respect to the body defence mechanisms, such as the reticulo-endothelial system, are able to recognize specific antigens at the cell surface and are thus able to locate defined target cells. In the case of physical vectors, most use naked DNA, hence, not only does this DNA need to be brought to the target tissue (lung, muscle), but because of the absence of spontaneous diffusion of DNA within the tissues, there is a need for ‘active transport’ systems to move the DNA within the tissue to individual cells.
The second constraint is that of penetration of the nucleic acids into the cell through the plasma membrane. While viruses achieve this using natural mechanisms, chemical and physical vectors must perturb the plasma membrane (i.e. physical vectors) and/or internal vesicular membranes (e.g. the cationic lipids after their incorporation into the endosomes).
In order to obtain an efficient vector system, particularly a physical one, and to achieve a high rate of cell transfection, these two conditions must be integrated in the development of a genetic vector.
Here, we describe and compare several types of physical methods of gene or drug transfer in vivo: biolistics, jet injection, hydrodynamic injection, ultrasound, magnetic field and electric pulse mediated gene transfer. We discuss the physical mechanisms underlying these approaches and we compare their relative advantages and their potential therapeutic applications in research or in preclinical and clinical medicine. The possible uses of the techniques described in this article have not been restricted exclusively to the transfer of genes, and hence, complementary uses of these technologies are also discussed.
Preamble
In vivo, cells can take up naked DNA but the mechanism of this uptake is not completely defined. For example, a simple injection of a plasmid into skeletal muscle may result in the expression of the proteins coded by the DNA at low and extremely variable levels (Wolff et al., 1990; 1991). Similar results have been reported using other tissues such as heart (Acsadi et al., 1991; Li et al., 1997), skin (Hengge et al., 1996) and thyroid (Sikes et al., 1994). One hypothesis for this phenomenon proposed the existence of a DNA uptake pathway involving endocytosis mediated by DNA receptors (Budker et al., 2000).
It has been recently shown that a rapid injection into a tissue can also induce an increase of the gene expression compared with a ‘classical’ slow injection (Andréet al., 2006). In muscle, an injection of less than 2 s duration results in a 500-fold increase of gene expression compared with the expression obtained with the same amount of DNA injected over 25 s, even when using the same injection volume (20 µL). Most of this uptake can be inhibited by the addition of heparin, a linear polymer with anionic charges that mimics the phosphate charge distribution of DNA. This observation is suggestive of receptor-mediated uptake of DNA as heparin would be a competitive inhibitor of the DNA binding to the receptors. However, at the highest injection speed, a slight permeabilization of the muscle fibres was also observed (Andréet al., 2006). In the brain, another ‘simple injection’ technique has been applied to improve drug and gene transfer, known as the convection-enhanced delivery. It consists of a continuous injection of a fluid containing drugs or plasmids under positive pressure (Raghavan et al., 2006). The main benefit is that the volume distribution of the drug or the gene into the brain is enhanced because of their transport by convection, that is by the injected fluid itself (Voges et al., 2003; Raghavan et al., 2006).
The role of the injections is to introduce the naked DNA into the tissue. The injections are expected to have little or no influence on the uptake of the naked DNA into the cells, where the DNA will be expressed, which would explain their low efficacy. Therefore, in order to increase gene expression up to levels essential for a therapeutic effect and to achieve reproducible conditions to reach this level of expression, several types of physical methods of gene or drug transfer have been developed and are described below.
Biolistics (the ‘gene gun’)
In the biolistics technique, heavy metal particles are coated with naked DNA plasmid and propelled into the cells. The technique was first used in 1987 on plant cells (Klein et al., 1987) and later used on mammalian cells and then whole tissues (Yang et al., 1990; Williams et al., 1991).
Targeted tissues or cells are thus permeabilized by small beads of biocompatible heavy metal (gold or tungsten) with diameters from 1 to 5 µm and coated with the DNA plasmid of interest (Fynan et al., 1993). The necessary acceleration of the particles is made by a gas discharge in a gun (‘gene gun’). Water vaporization under high-voltage electric spark (Yang et al., 1990) or helium discharge (Wolff et al., 1991) can also give sufficient velocity to the particles to penetrate the cells. The area targeted in vivo using a classical gene gun (Helios, Bio-Rad Laboratories, Hercules, CA) is about 2 cm2. A single shot using this method requires 0.5–5 mg of gold beads coated by 1–10 µg of DNA. One advantage of this technique is that DNA is transported directly into the cytosol and is not damaged during its penetration into cells, for example, by transport via the endosomes (Condon et al., 1996; Porgador et al., 1998). The transfection efficiency of biolistics is due to the penetration of certain gold particles into the cell nucleus (Shestopalov et al., 2002). Under these conditions, high-level gene expression can appear after only 3 h in cattle (Loehr et al., 2000) and be present for up to 18 h in the cornea (Zagon et al., 2005). Another advantage is the long-lasting expression of the transfected DNA: transgene expression was present even after 28–50 days following the ‘shooting’ of particles into muscle (Ajiki et al., 2003). These effects were also seen in other tissues such as epithelial cells and neurons (Sudha et al., 2001).
Many organs can be reached without damaging the surrounding tissues: muscle (Zelenin et al., 1997; Lauritzen et al., 2002), liver (Kuryama et al., 2000; Watkins et al., 2005), heart (Matsuno et al., 2003) and brain (Zhang and Selzer, 2001; O'Brien and Lummis, 2004). However, the most important limitation of this method is the low efficiency of the metal particles in reaching the entire tissue due to the low penetration of the particles. Moreover, surgery is often necessary to use the technique in order to reach any non-superficial tissue. Although various kinds of injectors have been made (Dileo et al., 2003), the major application of this technique remains gene delivery to skin cells (Wang et al., 2004).
The approach has been used extensively for genetic vaccination (Larregina et al., 2001) and for ‘suicide’ gene therapy to treat certain cancers (Yang and Sun, 1995). Skin vaccination with DNA by gene gun induces two types of response (Tuting et al., 1998): generation of cytotoxic lymphocytes and generation of antibodies. Recent studies using skin reported the combination of this method together with different adjuvants to determine efficacy and to increase the transfection efficiency. One specific study combined an antigen-coding plasmid with the plasmid-encoding interleukin 3 (pIL-3) (Matthews et al., 2007).
The second type of application is the treatment of various types of cancer by DNA vaccination. Hung et al. (2007) developed various strategies to enhance the potency of the vaccines and to increase vaccine-elicited T-cell immune responses in cervical cancer. Clinical trials of these vaccines showed a disease regression in three of nine patients post vaccination (Hung et al., 2007). More recently,Luz Garcia-Hernandez et al. (2008) reported that the use of prostate stem cell antigen vaccination induced a long-term protective immune response against prostate cancer. Only one patient out of 12 displayed a complete regression, probably because of the advanced stage of the disease (the efficacy of anti-cancer vaccines is greater when administered in the early stages of disease).
Another potential application that was tested was the ex vivo gene transfer to liver allografts prior to transplantation (Nakamura et al., 2003): this DNA vaccination provides an effective strategy for inducing protective immunity to infection and malignancy.
The main drawback of the gene gun approach is thought to be associated with the deposition of metal particles into the body and the potential long-term consequences. As an alternative to heavy metal particles,Lee et al. (2008a) used biodegradable polymeric nanoparticles in combination with a low-pressure gene gun. The chitosan and poly-gamma-glutamic acid beads showed the same efficiency of DNA transfection, as obtained with heavy metal particles (Lee et al., 2008a).
This technology has also been used in plant tissue to establish chloroplast transformation in cabbage (Liu et al., 2007) and to study protein targeting by genetic transformation in diatoms, unicellular eukaryotes playing an important role in ecology by fixing large amounts of CO2 in the oceans (Kroth, 2007).
Jet injection
Jet injection is also a ballistic method based on a principle close to that of the gene gun. Jet injection is the local injection of a liquid by means of a device that uses high pressure to force microdroplets of liquid to penetrate the skin or mucous membrane. The jet injection method is used to inject the molecules (drugs, nucleic acids) diluted in liquid without the use of a needle or particles. This high-pressure stream of liquid is used to pierce the skin or targeted tissues. Pressure can reach up to 3–4 bar, and the velocity of the droplets range from 100 m·s−1 to 200 m·s−1. The advantage of using jet injection is to minimize patient discomfort.
There are two types of jet injections: high volume (more than 100 µL) and low volume (20–30 µL). The low-volume method limits the volume of the injected solution, but it cannot target a large tissue area (anything greater than 1 cm2). Both methods use the same concentrations of DNA: from 0.1 to 1 µg·µL−1 of solution. Velocity of the fluid in jet injection contributes to the penetration into the skin, whereas the diameter of the jet and the injected volume limit the penetration depth of the solution (Arora et al., 2007).
The physical phenomenon linked to jet-induced penetration in the skin has only recently been investigated (Schramm-Baxter et al., 2004). A hole is created in the skin surface by the high pressure of the jet, most likely through the erosion or fracture of the skin. The depth of this hole is increased until the liquid that has accumulated in the hole created by the jet is sufficient to slow down the speed of the incoming jet, and the progression stops (Baxter and Mitragotri, 2005). The penetration of the injected molecules inside the cells is a consequence of the pressure caused by the liquid, locally delivered into the targeted tissue. The efficiency of this method and the depth of the penetration depend on several jet parameters including nozzle diameter (generally in the range of 150–300 µm), velocity of the liquid jet and the distance between the nozzle and the surface of the skin (Rajaratnam et al., 1994). For example, the highest concentration of DNA in keratinocytes was found using a distance of about 10 cm between the skin surface and the jet injector (Sawamura et al., 1999).
Since 1930, different types of jet injectors have been developed and used in clinical applications: immunization with vaccines (Canter et al., 1990; Ren et al., 2002), insulin delivery (Weller and Linder, 1966; Lindmayer et al., 1986), growth hormone delivery (Verhagen et al., 1995), local anaesthesia (Jimenez et al., 2006) and even tattooing (Kang et al., 2007). Jet injectors were and are still widely used in large vaccination campaigns, especially by the US War Department during the deployment of the American army in countries at risk (Warren et al., 1953; Foege and Eddins, 1973). The most important usage was probably in the WHO vaccination campaign against smallpox (Roberto et al., 1969). The feasibility of 600 or more subcutaneous injections per hour makes this the fastest immunization system (Grabenstein et al., 2006).
Jet injection can be also used in gene therapy for the transfer of genes to the skin or to tissues such as muscle, fat, skin and mammary cells of mice and sheep (Furth et al., 1995). In mice, injections of naked DNA coding for the cytosine deaminase suicide gene using the jet injection method promoted tumour regression caused by injection of 5-fluorocytosine (Walther et al., 2001; Walther et al., 2005). Intradermal genetic vaccination induces a jet-injected DNA immune response (Johansson et al., 2007). A preclinical evaluation of a CEA DNA prime/protein boost vaccination strategy against colorectal cancer has also been performed (Hallermalm et al., 2007). Another attractive application is jet-mediated gene delivery for the treatment of skin diseases caused by genetic defects, such as the production of abnormal proteins in keratinocytes (Sawamura et al., 1999). ShRNA encoding DNA, utilized to reverse the classical MDR1/P-glycoprotein-mediated multidrug resistance phenotype in vivo, was also delivered by a jet injection method in mice (Stein et al., 2008). Siegel et al. (2007) started a phase I trial of gene transfer into in-transit metastases from melanoma and skin metastases from breast cancer.
Other applications of jet injection have been considered. The combination of jet injection with conventional electroporation was tested in order to transfer DNA into murine muscles with the same or larger efficiency than with a needle injection before electro-transfer (Horiki et al., 2004).
Hydrodynamic injection
Hydrodynamic injection was first performed on mice by Budker et al. (1996). Gene transfer, mainly in the liver, was achieved through the rapid intravenous injection in the tail vein of a high volume of solution (almost equivalent to the blood volume of the treated animal) in just a few seconds. This method leads to an efficient gene transfer in mice with, for example, an injected volume of 8–12% of their mass and an injection duration of 5–10 s (Liu et al., 1999). The same result was shown in rats of 250 g with an injection volume of 25 mL containing 800 µg of DNA injected in 15 s in the tail vein (Maruyama et al., 2002). The transgene mRNA is mainly found in the liver (Herweijer and Wolff, 2003) and in lungs, kidney, spleen and heart, but in a lower extent. Both Liu et al. (1999) and Zhang et al. (1999) developed the tail vein approach to deliver genes by this method, but direct injection into liver vessels (Zhang et al., 1997) and muscle vessels (Budker et al., 1998) have also been used.
It is agreed that the volume of the injected liquid is too high to be handled by the heart in the normal way, so the liquid accumulates in the inferior vena cava (Zhang et al., 2004). Moreover, the low K+ content of the injection liquid also contributes to block the passage through the heart (Sawyer et al., 2007). Organs linked to the inferior vena cava (especially the liver, which can be easily distended) (Wolff and Budker, 2005), capture the injected DNA due to the high volume injected and the resulting pressure (Liu et al., 1999; Niidome and Huang, 2002).
There also appeared to be permeabilization of the membranes of hepatocytes, capillary endothelium and surrounding parenchymal cells, due to the increase of the hydrodynamic pressure (Zhang et al., 2004). The mechanism of hydrodynamic delivery in the liver is called hydroporation but the explanation of this hydrodynamic permeabilization is still hypothetical. The DNA uptake by the hepatocytes could also be mediated by DNA receptors (Budker et al., 2000) or by macropinocytosis (Sebestyen et al., 2006).
For many years, the hydrodynamic injection method was mostly limited to the hepatic transfer of genes in small animal research. The limitation of the procedure was essentially due to the high volume of DNA solution required for injection and the frequent lethality of rapid injection. Sawyer et al. (2007) reported temporary cardiac dysfunction in rats following hydrodynamic injection. Moreover,Liu and Huang (2001) showed that transfection could be improved by an interruption of hepatic blood flow for 3 min. Studies were performed on larger mammals, such as dogs and monkeys (Zhang et al., 2001; Wells, 2004), and more recently on pigs by isolating the inferior vena cava (Fabre et al., 2008). This last experiment was reproduced on a rat liver with a low-volume injection, but severe cardiovascular disturbances were induced (Sawyer et al., 2008). Until now, the delivery of DNA was tested with inserts less than 100 kb, but Hibbit et al. (2007) demonstrated the possibility of delivering a 135 kb human genomic DNA fragment containing the gene coding for the low-density lipoprotein receptor.
A computer-controlled injection device was recently developed to achieve an efficient, safe and automatically controlled hydrodynamic injection (Suda et al., 2008). This programmable device measures the pressure in the injected vessel, adjusting the speed of the injection to maintain a target pressure for a precise time, thus allowing efficient delivery of both viral and non-viral vectors to various organs with a minimal injection volume. This study should result in the advancement of a safe and programmable injection device for clinical use.
Ultrasound-mediated gene transfer
Sonoporation consists of the application of ultrasound to permeabilize cell membranes in order to improve internalization of large molecules. Although ultrasound has long been used for diagnostic purposes, its application as an experimental delivery system for molecules such as DNA is relatively new for studies in vitro (Kim et al., 1996; Bao et al., 1997; Tata et al., 1997). This technique has been used to produce growth factor (Schratzberger et al., 2002) or to transfect neuronal cells (Fischer et al., 2006). Ultrasonic waves were recently used in in vivo studies for the delivery of naked DNA into muscle (Taniyama et al., 2002a; Lu et al., 2003; Wang et al., 2005), carotid artery (Miller and Song, 2003), solid tumours (Huber et al., 2003), liver (Miao et al., 2005), kidney (Koike et al., 2005), heart (Taniyama et al., 2002b; Bekeredjian et al., 2003), and for transdermal delivery (Smith, 2007). Inhibition of prostate tumour growth was also demonstrated (Duvshani-Eschet et al., 2007) after the in situ transfer of genes encoding for hemopexin-like domain fragment by ultrasound (using ultrasound at 1 MHz and 2 W·cm−2 for 30 min with 10% of the volume of Optison). They have also been applied to gene transfer in plant cells (Liu et al., 2005).
Therapeutic ultrasound operates at frequencies from 1 to 3 MHz (or lower) and intensities of 0.5 to 3 W·cm−2. Other diagnostic techniques operate at higher frequencies (from 3.5 to 40 MHz) and lower intensities. Therapeutic trials consist of DNA plasmid injection followed by tissue irradiation by ultrasound for periods between 3 ms and 20–30 min. Ultrasound is easily approved for clinical use (delivery of chemotherapeutic, thrombolytic and gene-based drugs) because of the low energy delivered and because it is non-invasive (Ng and Liu, 2002). Ultrasound has other advantages: it has good penetration through soft tissue, does not damage cells or tissues (at appropriate intensities), and does not affect DNA integrity. One limitation of this technique is that it can cause the breakdown of the cytoskeleton, thus altering, among other mechanisms, the DNA trafficking inside the cells (Skorpikova et al., 2001).
Potential therapeutic application of ultrasound, as mentioned above, can be used in gene therapy. Ultrasound seems to facilitate the penetration of the DNA into several tissues (Newman et al., 2001) by increasing the porosity of membranes (Deng et al., 2004). Sonoporation mechanisms are not well characterized (Ferrara, 2008). Acoustic cavitation seems to be the most probable explanation of the phenomenon, coupled with acoustic pressure (Schlicher et al., 2006). The efficiency of this method can be improved by the use of an ultrasound contrast agent, which consists of compressible gas-filled microbubbles such as perfluorocarbon-filled microspheres of heat-denatured human albumin in the case of the commonly used Optison™ (Taniyama et al., 2002a; 2002b; Duvshani-Eschet and Machluf, 2007). The collapse of these microbubbles results in a gas jet that could explain the penetration of gene or drugs in cells (Prentice et al., 2005). Ultrasound also improved the transfer of DNA entrapped in nanoparticles, micelles (Husseini and Pitt, 2008) and liposomes (Huang, 2008).
High-intensity-focused ultrasound is also known to provoke the thermal ablation of tumours (Uchida et al., 2002; Wu et al., 2004). Another anti-tumour approach without thermal effects is the combination with bleomycin, which results in an effective tumour therapy (Larkin et al., 2008). Ultrasound can stimulate the anti-cancer effect of bleomycin in tumour-bearing tissues because of the ultrasound-induced permeabilization of the cell membrane. Ultrasound application is a mechanical way to permeabilize cells, to be compared with electroporation, an electrical way to cause cell permeabilization (see next paragraph). Yamashita et al. (2002) tried to combine sonoporation with the application of an electric field. This new method, called electro-sonoporation, consists of an intramuscular injection of naked DNA followed by a 5 min application of ultrasound combined with electric pulses. Greater efficiency was achieved when electrical pulses were applied in the middle of the ultrasound wave delivery.
Magnetic field mediated gene transfer
Magnetofection or magnetic gene transfer is based on the application of a magnetic field in order to set in motion super-paramagnetic iron oxide nanoparticles (SPION) (50 nm in diameter) that are coupled to DNA plasmids (Barnes et al., 2007).
This method is based on the use of cationic polymers that can combine the SPION and DNA, or RNA, via electrostatic interactions. They form stable complexes and DNA is protected from degradation (Hildebrandt et al., 2003). However, SPION can be used with viral vectors like paramyxoviruses (Kadota et al., 2005). In the presence of static magnets, the coupled magnetic polyplex nanoparticles display a transfection efficiency of reporter genes comparable with conventional non-viral transfection systems. The uptake of DNA/SPION complexes into the cells is by non-specific endocytosis (Huth et al., 2004). The magnetic field allows the concentration of the magnetic complexes within the target tissue. Moreover, it seems to cause the extravasation of the magnetic particles through the vascular wall into the target tissue (Goodwin et al., 2001). Although the influence of these magnetic particles on cellular functions is not well known, rapid kinetics of efficient transfection has been reported (Plank et al., 2003).
Other studies with pulsed magnetic fields reported an enhancement of the efficiency of in vitro non-viral gene delivery (Kamau et al., 2006). Magnetofection was used to transfect in vitro primary cells such as endothelial cells (Krotz et al., 2003), embryonic stem cells (Lee et al., 2008b) and neurons (Buerli et al., 2007). This technique is still in development for in vivo use, but early results have showed an enhancement of non-viral-mediated gene transfer into airway epithelium (Xenariou et al., 2006). Ex vivo trials, a compromise between in vitro and in vivo experiments, showed good results in gene transfer into osteoblast cells (Yang et al., 2008).
While static magnetic fields can be used for magnetofection, alternating magnetic fields can be used to heat tissue due to the movement of ferromagnetic nanoparticles, empty or filled with drugs or nucleic acids. The principle of this method is the direct injection of a magnetic fluid into a tumour, and then heating in an alternating magnetic field thereby causing a tumouricidal effect. Anti-tumour studies using this method have been reported for breast cancer (Kikumori et al., 2008), on prostate (Kawai et al., 2008), and on brain tumours (Jordan and Maier-Hauff, 2007). In addition, specific nano-entities have been developed for both the optical detection and the hyperthermic treatment (Jin et al., 2008). This technique cannot yet be considered as a method of gene transfer as it has only been used for drug transfer. Some experiments have been performed in tumour-bearing rabbits to transfer drugs into the tumour cells (Alexiou et al., 2000). The technique has also had limited use in clinical trials on patients with advanced sarcomas, using injected epirubicin and applying a 0.8 Tesla permanent magnetic field for a 30–120 min duration (Lubbe et al., 1996).
Electric pulse mediated gene transfer
Electroporation or electropermeabilization consists of the exposure of living cells to short and intense electric pulses. The first use of this method was published by Neumann et al. (1982) who demonstrated that DNA could be introduced into viable mouse lyoma cells by means of electric pulses. Two years later, the efficiency of this method was proved by transferring genes using standard laboratory equipment (generators for proteins and DNA electrophoresis) into mouse pre-B lymphocytes (Potter et al., 1984). These systems delivered exponentially decaying electric pulses. A square wave pulse generator was developed in 1985 by J. Teissié with outputs compatible for the treatment of cells (in suspension or attached) with rectangular pulses for which pulse duration and pulse amplitude are independently adjusted (Zerbib et al., 1985). Many trials started rapidly: not only on animal cells but also on plant cells, to transfer genes (Fromm et al., 1985) or to inhibit gene expression with antisense RNA (Ecker and Davis, 1986), and on bacterial transformation (Fiedler and Wirth, 1988; Taketo, 1988). Electroporation has been the most popular way to transfect bacterial cells since 1988.
The exposure of living cells to electric pulses induces a position-dependent modification of the transmembrane potential difference, which is numerically described by the equation of Schwan (1957). This induced transmembrane potential difference depends on physical parameters (pulse duration, field intensity and electrode geometry) and biological factors (cell size, shape and density). It is superimposed on the resting transmembrane potential difference. Electropermeabilization is generated when the net value of the transient transmembrane potential difference exceeds a threshold value between 0.2 and 0.4 V across the membrane (Teissié and Rols, 1993). Transient permeation structures are generated at the cell membrane level due to electrocompressive forces induced by the potential difference and the field effects on the water and membrane dipoles (Teissiéet al., 2005). This ‘de-structuring’ of the membrane takes place in a few tens of microseconds (the duration of the pulses usually applied to permeabilize cells or tissues is 100 µs), but the membrane remains permeable for several minutes. Electroporation mechanisms are still under investigation (Teissiéet al., 2005). Several models have been proposed (Neumann et al., 1982; Tsong, 1991), the more recent based on electric (Kotnik and Miklavcic, 2000) and molecular dynamics (Tieleman, 2006) simulation.
Under appropriate electrical parameters, the destabilization of membrane structure is completely reversible, ensuring the survival of the transiently permeabilized cells. Another property of this method comes from the fact that pulses are too short to provoke thermal effects, contributing to the reversibility of this phenomenon (Tsong and Su, 1999). When very high intensity fields are delivered to the cells, the changes in membrane structure can become permanent, resulting in the loss of the cell viability due to the generation of large, long-lived ‘holes’ in the membrane. This electroporation is termed irreversible and may be produced in the absence of thermal effects (Davalos et al., 2005). Recent molecular dynamics simulations have suggested that pores could indeed be generated, but these simulations are performed with numerical values of the transmembrane potential difference much larger than those necessary to obtain physiological reversible cell permeabilization (Tieleman et al., 2003).
One of the most frequent applications of cell electropermeabilization in vitro and in vivo is the electric pulse mediated transfer of nucleic acids, also termed DNA or gene electro-transfer or electro-gene therapy. It has been applied in a large number of tissues like the skeletal muscle (Aihara and Miyazaki, 1998; Mir et al., 1998 1999), human prostate cancer xenograft, skin (Mikata et al., 2002), tumours (Rols et al., 1998), cornea (Blair-Parks et al., 2004), brain (Kondoh et al., 2000) and liver (Suzuki et al, 1998). It has also been used to transfect fungal (Robinson and Sharon, 1999) and plant tissues (Dekeyser et al., 1990). The tissues, genes and type of experimental or therapeutic applications have been reviewed elsewhere (André and Mir, 2004; Mir et al., 2005). Long-term expression of the luciferase reporter gene can be detected for at least 9 months after DNA electro-transfer into muscle (Mir et al., 1998). Recent studies have shown the efficiency of this technique when transferring nucleic acids other than DNA plasmids, such as mRNA, to chronic lymphocytic leukemia cells (Van Bockstaele et al., 2008) or siRNA to tumours in vivo (Golzio et al., 2007).
While permeabilization is sufficient to ensure a good transfer of drugs, especially in vivo (see below), efficient and safe gene electro-transfer requires both target cell permeabilization and DNA electrophoretic transport towards the permeabilized membranes. It is thus necessary to deliver either trains of long (several milliseconds) identical pulses or combinations of permeabilizing high voltage (HV) short electric pulses and of electrophoretic low voltage (LV) long electric pulses (Satkauskas et al., 2002; Satkauskas et al., 2005). For example, in skeletal muscle, one HV pulse of 800 V·cm−1 and duration of 100 µs and 4 LV pulses of 80 V·cm−1 and duration of 100 ms result in very high level of expression (Andréet al., 2008).
The therapeutic use of the delivery of electric pulses in patients is, at present, confined to the transfer of anti-cancer drugs to tumour cells in vivo. Electrochemotherapy (ECT) combines the administration of an anti-tumour agent, like bleomycin or cisplatin, to the delivery of electric pulses to the tumours. Since the first clinical trial (Mir et al., 1991), clinical devices have been developed and clinical trials (Marty et al., 2006) allowed for the development of standard operating procedures of ECT for cutaneous and subcutaneous tumours (Mir et al., 2006). ECT is now routinely used for the treatment of cutaneous and subcutaneous tumours in humans (Sersa et al., 2008) and, more recently, in pet animals (Cemazar et al., 2008). But these results have paved the way for the clinical use of gene electro-transfer in humans. DNA electro-transfer is reaching the clinical stage as several clinical trials to transfer genes in tumours and in muscle are ongoing (Heller and Heller, 2006).
Discussion
We report six different physical methods of gene (and drug) transfer in cells or tissues. All methods have their advantages and limitations, and the choice of one over the others essentially depends on the proposed therapeutic application. All of them permit the delivery of therapeutic materials into cells by combining two effects: (i) the reversible alteration of the plasma membrane, which allows the passage of the molecules of interest directly into the cell cytosol; and (ii) the movement of the nucleic acids to the permeabilized plasma membrane or to the inside of the cell. These two effects can be achieved in one or two steps, depending upon the method and its physical basis.
The one step methods are the biolistic method, the jet injection and the hydrodynamic injection. In these methods, the DNA carriers (beads or liquids) not only carry the nucleic acids, but they are also responsible for the penetration of the DNA to inside the cell. Therefore, the DNA carriers bring the DNA close to the cell and are involved in the crossing of the plasma membrane. In all cases, energy is transferred to the DNA carriers. In the biolistics method (the ‘gene gun’), a kinetic energy is given to the small beads: they can cross the cell membrane and bring the DNA coated on their surface to the cell interior. In the jet injection method, the high-pressure fluid jet brings the DNA to and across the membrane. In the hydrodynamic injection, the high-injected volume causes an increase of the hydrodynamic pressure, especially in liver, thus inducing the permeabilization of the membrane and allowing the entrance of the DNA into the cells. All these methods do not need previous injection of DNA or other molecules close to the tissue to be treated, because the DNA is present in the solution or on the particles directly injected.
The multistep methods are the ultrasound, the magnetic field and the electric pulse mediated gene transfer approaches. The first step is the injection of the nucleic acids either intravenously or locally (almost mandatory for the electro-transfer, even though electro-transfer in liver at low levels of expression has been obtained by intravenous injections of DNA). The intravenous route of administration is suitable in the case of the magnetofection. The magnetic particles can be concentrated in particular areas of the body by magnets before a second event allows for their uptake by the cells. In all cases, the liquid in which the DNA is dissolved is not responsible for the permeabilization of the cell membranes or of the crossing of the membrane. In the case of the electro-transfer, these two functions are achieved by the electric pulses as described above; while in the case of the magnetofection or the sonoporation, they are achieved by these approaches alone or after combination with a second physical method. In this respect, these two methods can be combined with adjuvants: the sonoporation with echocontrast agents and the magnetofection with transfection reagents. It was shown that transgene expression can be increased 100-fold depending on the type of echocontrast agents that are coupled to optimize ultrasound physical parameters (e.g. delivered energy, frequency). (Zarnitsyn and Prausnitz, 2004). Under these favourable conditions, sonoporation permitted gene expression in 75% of the HL60 cells transfected in vitro (Gac et al., 2007) and transgene expression was evident in all treated animals in vivo (Li et al., 2003).
More precisely, in the case of the multistep methods, we must distinguish permeabilization of the cell membrane (achieved by electroporating electric pulses or cavitational ultrasounds) and transfer of the DNA close or across the permeabilized membrane. This second step can be achieved by the magnetic forces dragging the iron oxide nanoparticles, by the electrophoretic component of the electric pulses, or by the mechanical energy carried by the ultrasonic forces combined with microbubbles from echocontrast agents which can collapse and produce the necessary pressure for molecules to penetrate into the cells.
Another step is required for efficient transfection: transport of the DNA from the plasma membrane to and across the nuclear membrane. Some of the physical methods presented here do little to address this step, but other strategies might be coupled with these physical approaches to address this transport, such as the inclusion of nuclear localization sequences in the sequence of the DNA molecules, or the formation of complexes with peptides presenting the nuclear import sequence, or the treatment of the cells by nuclear pore-enlarging molecules, such as trans-cyclohexane-1,2-diol. However, these strategies are beyond the scope of this review.
Concerning the transfection rates and the efficiency of the transfected gene expression, there is a general consensus that viral methods are, very often, more efficient than the non-viral methods listed here. However, the levels reached by hydrodynamic injections or by electro-transfer are important and in many cases are most likely sufficient to induce a therapeutic effect. The particular interest of the biophysical methods for gene transfer is that unmodified, naked DNA can be used. This provides a real simplification of the vector preparation, which can be considered as a chemical product for which the quality control and quality assurance procedures are well known. The production of DNA under GMP conditions is achievable, and safe products can be obtained. Conveniently applied, these methods are also safe by themselves. For example, electric pulses can be safely delivered as models of the electric field distribution in tissue have been produced and validated. Significant experience has been acquired in large animals and in humans by the application of electroporating pulses to treat solid tumours by ECT.
It is important to recall that the methods described have preferential targets and limitations, mainly due to the physical mechanisms on which these treatments are based. First of all, while the skin is a convenient target for the gene gun and jet injection, skin is not suitable for hydrodynamic injection. The low-depth penetration of particles in tissues by gene gun mediated delivery does not exceed 4 mm into the skin (Zelenin et al., 1997), though it is sufficient for skin DNA vaccination (Luz Garcia-Hernandez et al., 2008) or for the transfection of thin tissues, such as plant leaves (Remacle et al., 2006). If large volumes of tissue are considered, then the gene gun and the jet injection are not adequate as they only allow for the treatment of small areas or volumes. On the contrary, the methods that require the preliminary injection of the DNA in the tissue, such as electro-transfer, can be limited by the feasibility of this injection. It must be noted that intravenous DNA injection has been used for electro-transfer into liver cells (Andréet al., 2008). The ability to place the electrodes around the treated tissue may also limit the application of gene electro-transfer. This limitation may be overcome by using sonofection and magnetofection, as they do not require a direct physical contact between the devices and the tissues. Nevertheless, to apply these methods (particularly gene electro-transfer and magnetofection) on internal organs it is necessary to bring the devices delivering the physical energy close the target tissue. In this respect, the type of device used for the treatment can also modulate the effect on the gene expression. In the case of the gene gun approach, helium powered or gunpowder, hand-held or stand-alone systems do not give the same results. In electro-transfer, the choice between plate electrodes and needle electrodes with different geometries can be important depending on the shape, size and location of the treated tissue. Finally, the high volume injected in the hydrodynamic method limits the use to small animals or to organs that can be easily isolated from the rest of the body by means of clamps on the afferent arteries and efferent veins.
Some of these methods are also relatively new in their application to gene transfer and all the potential side effects are not yet known. For example, the long-term presence of gold beads in tissues after gene gun bombardment has not yet been studied, and their toxicity is not well known. The same is true for the magnetic nanoparticles used in magnetofection, although so far they have not proved to be toxic for the treated tissues (Plank et al., 2003). These methods must still be considered as investigational tools: even though a few clinical trials have already been performed (or are in progress for some of them), none has already become a routine technique.
In summary (see Table 1), all the physical methods we presented here have the common potential to deliver gene into cells and tissues by bringing the DNA across the plasma membrane into the cell cytosol. The high and rapid level of the foreign gene expression is likely to be due to the direct transfer of the DNA into the cytoplasm and into the nucleus, ensuring its integrity against enzymes. Although all these techniques have both positive and negative features in their efficiency, they can all find their use as physical methods to deliver specific genes into tissues.
Table 1.
Summary of the physical methods presented here
| Methods | Target tissue(s) | Mechanism(s) | Naked DNA alonea | |
|---|---|---|---|---|
| Single step methods | Biolistics (gene gun) | Skin (mainly used for DNA vaccination), muscle, liver, heart, brain, cornea | Heavy metal particles coated with naked DNA plasmid and propelled into the cells. Necessary acceleration is made by gas discharge in a gun. | Yes |
| Jet injection (needleless injection) | Skin, muscle, mammary cells; method also used for vaccination, insulin delivery, local anaesthesia | Local injection of a liquid by means of a device that uses high pressure to force the microdroplets of the liquid to penetrate the skin or mucous membrane. Uptake of DNA into cells is a consequence of the pressure due to the high volume locally delivered into the targeted tissue. | Yes | |
| Hydrodynamic injection | Liver, muscle, lungs, kidney, spleen, heart | In rodents, rapid intravenous injection in the tail vein of a high volume of solution in just a few seconds. Organs linked to the inferior vena cava capture the injected DNA due to the high volume injected and the resulting pressure. In large animals, target organs are clamped. | Yes | |
| Multistep methods | Ultrasound-mediated gene transfer | Muscle, carotid artery, liver, solid tumours, kidney, heart, skin | Application of ultrasound (frequencies from 1 to 3 MHz and intensities of 0.5 to 3 W·cm−2) increasing the permeability of the membrane due to the acoustic pressure. Efficiency is improved by the adjuvant use of ultrasound contrast agents containing microbubbles which can easily collapse and produce local high pressure. | Yes/No |
| Magnetic field-mediated gene transfer | Airway epithelium, synovium, tumours | Super-paramagnetic iron oxide nanoparticles (SPION) coupled to DNA in a cationic polymer to bring the DNA close to the targeted tissue by a magnetic field. Uptake of DNA/SPION complexes into the cells is by non-specific endocytosis. | No | |
| Electric pulse mediated gene transfer | Muscle, skin, tumours, cornea brain, liver, embryos, lung, tendons, spleen, cartilage, testis, ovaries, bladder, adipocytes … | Exposure of living cells or targeted tissues to short and intense electric pulses inducing a position-dependent modification of the transmembrane potential difference. Transient permeation structures are generated at the cell membrane level due to electrocompressive forces induced by the potential difference and the field effects on water and membrane dipoles. | Yes |
Not considering the carrier physiological fluid in which DNA is dissolved.
 |
Acknowledgments
This work was supported by grants from CNRS, Institut Gustave Roussy, Institut National du Cancer (INCa) and CLINIGENE (FP6 – LSH-2004-018933). The authors acknowledge An Vu for her detailed revision of the manuscript.
Glossary
Abbreviations
- ECT
electrochemotherapy
- EGT
electrogene therapy
- HV
high voltage pulses
- LV
low voltage pulses
- SPION
superparamagnetic iron oxide nanoparticles
Conflicts of interest
J.V. has no conflict of interest, while L.M.M. has been granted several patents covering some aspects of the electric pulses mediated drug and gene transfer.
References
- Acsadi G, Jiao SS, Jani A, Duke D, Williams P, Chong W, et al. Direct gene transfer and expression into rat heart in vivo. New Biol. 1991;3:71–81. [PubMed] [Google Scholar]
- Aihara H, Miyazaki J. Gene transfer into muscle by electroporation in vivo. Nat Biotechnol. 1998;16:867–870. doi: 10.1038/nbt0998-867. [DOI] [PubMed] [Google Scholar]
- Ajiki T, Murakami T, Kobayashi Y, Hakamata Y, Wang J, Inoue S, et al. Long-lasting gene expression by particle-mediated intramuscular transfection modified with bupivacaine: combinatorial gene therapy with IL-12 and IL-18 cDNA against rat sarcoma at a distant site. Cancer Gene Ther. 2003;10:318–329. doi: 10.1038/sj.cgt.7700575. [DOI] [PubMed] [Google Scholar]
- Alexiou C, Arnold W, Klein RJ, Parak FG, Hulin P, Bergemann C, et al. Locoregional cancer treatment with magnetic drug targeting. Cancer Res. 2000;60:6641–6648. [PubMed] [Google Scholar]
- André F, Mir LM. DNA electrotransfer: its principle and an updated review of its therapeutic applications. Gene Ther. 2004;11(Suppl.)(1):S33–43. doi: 10.1038/sj.gt.3302367. [DOI] [PubMed] [Google Scholar]
- André FM, Cournil-Henrionnet C, Vernery D, Opolon P, Mir LM. Variability of naked DNA expression after direct local injection: the influence of the injection speed. Gene Ther. 2006;13:1619–1627. doi: 10.1038/sj.gt.3302827. [DOI] [PubMed] [Google Scholar]
- André FM, Gehl J, Sersa G, Préat V, Hojman P, Eriksen J, et al. Efficiency of high and low voltage pulse combinations for gene electrotransfer in muscle, liver, tumour and skin. Hum Gene Ther. 2008;19:1261–1271. doi: 10.1089/hum.2008.060. [DOI] [PubMed] [Google Scholar]
- Arora A, Hakim I, Baxter J, Rahtnasingham R, Srinivasan R, Fletcher DA, et al. Needle-free delivery of macromolecules across the skin by nanoliter-volume pulsed microjets. Proc Natl Acad Sci USA. 2007;104:4255–4260. doi: 10.1073/pnas.0700182104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao S, Thrall BD, Miller DL. Transfection of a reporter plasmid into cultured cells by sonoporation in vitro. Ultrasound Med Biol. 1997;23:953–959. doi: 10.1016/s0301-5629(97)00025-2. [DOI] [PubMed] [Google Scholar]
- Barnes AL, Wassel RA, Mondalek F, Chen K, Dormer KJ, Kopke RD. Magnetic characterization of superparamagnetic nanoparticles pulled through model membranes. Biomagn Res Technol. 2007;5:1. doi: 10.1186/1477-044X-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baxter J, Mitragotri S. Jet-induced skin puncture and its impact on needle-free jet injections: experimental studies and a predictive model. J Control Release. 2005;106:361–373. doi: 10.1016/j.jconrel.2005.05.023. [DOI] [PubMed] [Google Scholar]
- Bekeredjian R, Chen S, Frenkel PA, Grayburn PA, Shohet RV. Ultrasound-targeted microbubble destruction can repeatedly direct highly specific plasmid expression to the heart. Circulation. 2003;108:1022–1026. doi: 10.1161/01.CIR.0000084535.35435.AE. [DOI] [PubMed] [Google Scholar]
- Blair-Parks K, Weston BC, Dean DA. High-level gene transfer to the cornea using electroporation. J Gene Med. 2004;4:92–100. doi: 10.1002/jgm.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budker V, Zhang G, Knechtle S, Wolff JA. Naked DNA delivered intraportally expresses efficiently in hepatocytes. Gene Ther. 1996;3:593–598. [PubMed] [Google Scholar]
- Budker V, Zhang G, Danko I, Williams P, Wolff J. The efficient expression of intravascularly delivered DNA in rat muscle. Gene Ther. 1998;5:272–276. doi: 10.1038/sj.gt.3300572. [DOI] [PubMed] [Google Scholar]
- Budker VG, Budker T, Zhang G, Subbotin VM, Loomis A, Wolff JA. Hypothesis: naked plasmid DNA is taken up by cells in vivo by a receptor-mediated process. J Gene Med. 2000;2:874–888. doi: 10.1002/(SICI)1521-2254(200003/04)2:2<76::AID-JGM97>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- Buerli T, Pellegrino C, Baer K, Lardi-Studler B, Chudotvorova I, Fritschy JM, et al. Efficient transfection of DNA or shRNA vectors into neurons using magnetofection. Nat Protoc. 2007;2:3090–3101. doi: 10.1038/nprot.2007.445. [DOI] [PubMed] [Google Scholar]
- Canter J, Mackey K, Good LS, Roberto RR, Chin J, Bond WW, et al. An outbreak of hepatitis-B associated with jet injections in weight-reduction clinic. Arch Intern Med. 1990;150:1923–1927. [PubMed] [Google Scholar]
- Cemazar M, Tamzali Y, Sersa G, Tozon N, Mir LM, Miklavcic D, et al. Electrochemotherapy in vetenary oncology. J Vet Intern Med. 2008;22:826–831. doi: 10.1111/j.1939-1676.2008.0117.x. [DOI] [PubMed] [Google Scholar]
- Condon C, Watkins SC, Celluzzi CM, Thompson K, Falo LD. DNA-based immunization by in vivo transfection of dendritic cells. Nat Med. 1996;2:1122–1128. doi: 10.1038/nm1096-1122. [DOI] [PubMed] [Google Scholar]
- Davalos RV, Mir IL, Rubinsky B. Tissue ablation with irreversible elecroporation. Ann Biomed Eng. 2005;33:223–231. doi: 10.1007/s10439-005-8981-8. [DOI] [PubMed] [Google Scholar]
- Dekeyser RA, Claes B, De Rycke R, Habets ME, Van Montage MC, Caplan HB. Transient gene expression in the intact and organized rice tissues. Plant Cell. 1990;2:591–602. doi: 10.1105/tpc.2.7.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng CX, Sieling F, Pan H, Cui J. Ultrasound-induced cell membrane porosity. Ultrasound Med Biol. 2004;30:519–530. doi: 10.1016/j.ultrasmedbio.2004.01.005. [DOI] [PubMed] [Google Scholar]
- Dileo J, Miller TE, Jr, Chesnoy S, Huang L. Gene transfer to subdermal tissues via a new gene gun design. Hum Gene Ther. 2003;14:79–87. doi: 10.1089/10430340360464732. [DOI] [PubMed] [Google Scholar]
- Duvshani-Eschet M, Machluf M. Efficient transfection of tumours facilitated by long term therapeutic ultrasound in combination with contrast agent: from in vitro to in vivo setting. Cancer Gene Ther. 2007;14:306–315. doi: 10.1038/sj.cgt.7701015. [DOI] [PubMed] [Google Scholar]
- Duvshani-Eschet M, Benny O, Morgenstern A, Machluf M. Therapeutic ultrasound facilitates anti-angiogenic gene delivery and inhibits prostate tumour growth. Mol Cancer Ther. 2007;6:2371–2382. doi: 10.1158/1535-7163.MCT-07-0019. [DOI] [PubMed] [Google Scholar]
- Ecker JR, Davis RW. Inhibition of gene expression in plant cells by expression of antisense RNA. Proc Natl Acad Sci USA. 1986;83:5372–5376. doi: 10.1073/pnas.83.15.5372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabre JW, Grehan A, Whitehorne M, Sawyer GJ, Dong X, Salehi S, et al. Hydrodynamic gene delivery in the pig liver via an isolated segment of the inferior vena cava. Gene Ther. 2008;15:452–462. doi: 10.1038/sj.gt.3303079. [DOI] [PubMed] [Google Scholar]
- Ferrara W. Driving delivery vehicles with ultrasound. Adv Drug Deliv Rev. 2008;60:1097–1102. doi: 10.1016/j.addr.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiedler S, Wirth R. Transformation of bacteria with plasmid DNA by electroporation. Anal Biochem. 1988;170:38–44. doi: 10.1016/0003-2697(88)90086-3. [DOI] [PubMed] [Google Scholar]
- Fischer AJ, Stanke JJ, Omar G, Askwith CC, Burry RW. Ultrasound-mediated gene transfer into neuronal cells. J Biotechnol. 2006;20:393–411. doi: 10.1016/j.jbiotec.2005.10.006. [DOI] [PubMed] [Google Scholar]
- Foege WH, Eddins DL. Mass vaccination programs in developing countries. Prog Med Virol. 1973;15:205–243. [PubMed] [Google Scholar]
- Fromm M, Taylor LP, Walbot V. Expression of genes transferred into monocot and dicot plant cells by electroporation. Proc Natl Acad Sci USA. 1985;82:5824–5828. doi: 10.1073/pnas.82.17.5824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furth PA, Shamay A, Hennighausen L. Gene transfer into mammalian cells by jet injection. Hybridoma. 1995;14:149–152. doi: 10.1089/hyb.1995.14.149. [DOI] [PubMed] [Google Scholar]
- Fynan EF, Webster RG, Fuller DH, Haynes JR, Santoro JC, Robinson HL. DNA vaccines: protective immunizations by parenteral mucosal and gene-gun inoculations. Proc Natl Acad Sci USA. 1993;90:11478–11482. doi: 10.1073/pnas.90.24.11478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gac SL, Zwaan E, van den Berg A, Ohl CD. Sonoporation of suspension cells with a single cavitation bubble in a microfluidic confinement. Lab Chip. 2007;7:1666–1672. doi: 10.1039/b712897p. [DOI] [PubMed] [Google Scholar]
- Golzio M, Mazzolini L, Ledoux A, Paganin A, Izard M, Hellaudais L, et al. In vivo gene silencing in solid tumors by targeted electrically mediated siRNA delivery. Gene Ther. 2007;14:752–759. doi: 10.1038/sj.gt.3302920. [DOI] [PubMed] [Google Scholar]
- Goodwin SC, Bittner CA, Perterson CL, Wong G. Single-dose toxicity study of hepatic intra-arterial infusion of doxorubicin coupled to a novel magnetically targeted drug carrier. Toxicol Sci. 2001;60:177–183. doi: 10.1093/toxsci/60.1.177. [DOI] [PubMed] [Google Scholar]
- Grabenstein JD, Pittman PR, Greenwood JT, Engler RJM. Immunization to protect the US Armed Forces: heritage, current practice, and prospects. Epidemiol Rev. 2006;28:3–26. doi: 10.1093/epirev/mxj003. [DOI] [PubMed] [Google Scholar]
- Hallermalm K, Johansson S, Brave A, Ek M, Engstrom G, Boberg A, et al. Pre-clinical evaluation of a CEA DNA prime/protein boost vaccination strategy against colorectal cancer. Scand J Immunol. 2007;66:43–51. doi: 10.1111/j.1365-3083.2007.01945.x. [DOI] [PubMed] [Google Scholar]
- Heller LC, Heller R. In vivo electroporation for gene therapy. Hum Gene Ther. 2006;17:890–897. doi: 10.1089/hum.2006.17.890. [DOI] [PubMed] [Google Scholar]
- Hengge UR, Walker PS, Vogel JC. Expression of naked DNA in human, pig, and mouse skin. J Clin Invest. 1996;97:2911–2916. doi: 10.1172/JCI118750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herweijer H, Wolff JA. Progress and prospects: naked DNA gene transfer and therapy. Gene Ther. 2003;10:453–458. doi: 10.1038/sj.gt.3301983. [DOI] [PubMed] [Google Scholar]
- Hibbit OC, Harbottle RP, Waddington SN, Bursill CA, Coutelle C, Channon KM, et al. Delivery and long-term expression of a 135 kb LDLR genomic DNA locus in vivo by hydrodynamic tail vein injection. J Gene Med. 2007;9:488–497. doi: 10.1002/jgm.1041. [DOI] [PubMed] [Google Scholar]
- Hildebrandt IJ, Iyer M, Wagner E, Gambhir SS. Optical imaging of transferring targeted PEI/DNA complexes in living subjects. Gene Ther. 2003;10:758–764. doi: 10.1038/sj.gt.3301939. [DOI] [PubMed] [Google Scholar]
- Horiki M, Yamato E, Ikegami H, Ogihara T, Miyazaki J. Needleless in vivo gene transfer into muscles by jet injection in combination with electroporation. J Gene Med. 2004;6:1134–1138. doi: 10.1002/jgm.612. [DOI] [PubMed] [Google Scholar]
- Huang SL. Liposomes in ultrasonic drug and gene delivery. Adv Drug Deliv Rev. 2008;60:1167–1176. doi: 10.1016/j.addr.2008.03.003. [DOI] [PubMed] [Google Scholar]
- Huber PE, Mann MJ, Melo LG, Ehsan A, Kong D, Zhang L, et al. Focused ultrasound (HIFU) induces localized enhancement of reporter gene expression in rabbit carotid artery. Gene Ther. 2003;10:1600–1607. doi: 10.1038/sj.gt.3302045. [DOI] [PubMed] [Google Scholar]
- Hung CF, Monie A, Alvarez RD, Wu TC. DNA vaccines for cervical cancer: from bench to bedside. Exp Mol Med. 2007;39:679–689. doi: 10.1038/emm.2007.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husseini GA, Pitt WG. Micelles and nanoparticles for ultrasonic drug and gene delivery. Adv Drug Deliv Rev. 2008;60:1137–1152. doi: 10.1016/j.addr.2008.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huth S, Lausier J, Gersting SW, Rudolph C, Plank C, Welshb U, et al. Insights into the mechanism of magnetofection using PEI-based magnetofectins for gene transfer. J Gene Med. 2004;6:923–936. doi: 10.1002/jgm.577. [DOI] [PubMed] [Google Scholar]
- Jimenez N, Bradford H, Seidel KD, Sousa M, Lynn AM. A comparison of a needle-free injection system for local anesthesia versus EMLA for intravenous catheter insertion in the paediatric patient. Anesth Analg. 2006;102:411–414. doi: 10.1213/01.ane.0000194293.10549.62. [DOI] [PubMed] [Google Scholar]
- Jin H, Hong B, Kakar SS, Kang KA. Tumour-specific nano-entities for optical detection and hyperthermic treatment of breast cancer. Adv Exp Med Biol. 2008;614:275–284. doi: 10.1007/978-0-387-74911-2_31. [DOI] [PubMed] [Google Scholar]
- Johansson S, Ek M, Wahren B, Stout R, Liu M, Hallermalm K. Intracellular targeting of CEA results in Th1-type antibody responses following intradermal genetic vaccination by a needle-free jet injection device. ScientificWorldJournal. 2007;7:987–999. doi: 10.1100/tsw.2007.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan A, Maier-Hauff K. Magnetic nanoparticles for intracranial thermotherapy. J Nanosci Nanotechnol. 2007;7:4604–4606. [PubMed] [Google Scholar]
- Kadota S, Kanayama T, Miyajima N, Takeuchi K, Nagata K. Enhancing of measles virus infection by magnetofection. J Virol Methods. 2005;128:61–66. doi: 10.1016/j.jviromet.2005.04.003. [DOI] [PubMed] [Google Scholar]
- Kamau SW, Hassa PO, Steitz B, Petri-Fink A, Hofmann H, Hofmann-Amtenbrink M, et al. Enhancement of the efficiency of non-viral gene delivery by application of pulsed magnetic field. Nucleic Acids Res. 2006;34:e40. doi: 10.1093/nar/gkl035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang MJ, Kim MY, Kim YJ, Park YM, Kim HO. Traumatic tattoo associated with jet injector (Dermojet) use. J Dermatol. 2007;34:732–733. doi: 10.1111/j.1346-8138.2007.00372.x. [DOI] [PubMed] [Google Scholar]
- Kawai N, Futakuchi M, Yoshida T, Ito A, Sato S, Naiki T, et al. Effect of heat therapy using magnetic nanoparticles conjugated with cationic liposomes on prostate tumour in bone. Prostate. 2008;68:784–792. doi: 10.1002/pros.20740. [DOI] [PubMed] [Google Scholar]
- Kikumori T, Kobayashi T, Sawaki M, Imai T. Anti-cancer effect of hyperthermia on breast cancer by magnetite nanoparticle-loaded anti-HER2 immunoliposomes. Breast Cancer Res Treat. 2008 doi: 10.1007/s10549-008-9948-x. Mar 2 [Epub ahead of print] PM10: 18311580. [DOI] [PubMed] [Google Scholar]
- Kim HJ, Greenleaf JF, Kinnick RR, Bronk JT, Bolander E. Ultrasound-mediated transfection of mammamian cells. Hum Gene Ther. 1996;7:1339–1346. doi: 10.1089/hum.1996.7.11-1339. [DOI] [PubMed] [Google Scholar]
- Klein TM, Wolf ED, Wu R, Sanford JC. High-velocity microprojectiles for delivering nucleic acids into living cells. Nature. 1987;327:70–73. [PubMed] [Google Scholar]
- Koike H, Tomita N, Azuma H, Taniyama Y, Yamasaki K, Kunugiza Y, et al. An efficient gene transfer method mediated by ultrasound and microbubbles into the kidney. J Gene Med. 2005;7:108–116. doi: 10.1002/jgm.632. [DOI] [PubMed] [Google Scholar]
- Kondoh T, Motooka Y, Bhattacharjee AK, Kokunai T, Saito N, Tamaki N. In vivo gene transfer into the periventricular region by electroporation. Neurol Med Chir (Tokyo) 2000;40:618–622. doi: 10.2176/nmc.40.618. [DOI] [PubMed] [Google Scholar]
- Kotnik T, Miklavcic D. Second-order model of membrane electric field induced by alternating external electric fields. IEEE Trans Biomed Eng. 2000;47:1074–1081. doi: 10.1109/10.855935. [DOI] [PubMed] [Google Scholar]
- Kroth PG. Genetic transformation: a tool to study protein targeting in diatoms. Methods Mol Biol. 2007;390:257–268. [PubMed] [Google Scholar]
- Krotz F, Sohn HY, Gloe T, Plank C, Pohl U. Magnetofection potentiates gene delivery to cultured endothelial cells. J Vasc Res. 2003;40:425–434. doi: 10.1159/000073901. [DOI] [PubMed] [Google Scholar]
- Kuryama S, Mitoro A, Tsujinoue H, Nakatani T, Yoshiji H, Tsujimoto T, et al. Particle-mediated gene transfer into murine livers using a newly developed gene gun. Gene Ther. 2000;7:1132–1136. doi: 10.1038/sj.gt.3301192. [DOI] [PubMed] [Google Scholar]
- Larkin JO, Casey GD, Tangney M, Cashman J, Collins CG, Soden DM, et al. Effective tumour treatment using optimized ultrasound-mediated delivery of bleomycin. Ultrasound Med Biol. 2008;34:406–413. doi: 10.1016/j.ultrasmedbio.2007.09.005. [DOI] [PubMed] [Google Scholar]
- Larregina AT, Watkins SC, Erdos G, Spencer LA, Storkus WJ, Beer SD, et al. Direct transfection and activation of human cutaneous dendritic cells. Gene Ther. 2001;8:608–617. doi: 10.1038/sj.gt.3301404. [DOI] [PubMed] [Google Scholar]
- Lauritzen HP, Reynet C, Schjerling P, Ralston E, Thomas S, Galbo H, et al. Gene gun bombardment-mediated expression and translocation of EGFP-tagged GLUT4 in skeletal muscle fibres in vivo. Pflugers Arch. 2002;444:710–721. doi: 10.1007/s00424-002-0862-5. [DOI] [PubMed] [Google Scholar]
- Lee PW, Peng SF, Su CJ, Mi FL, Chen HL, Wei MC, et al. The use of biodegradble polymeric nanoparticles in combination with a low-pressure gene gun for transfermal DNA delivery. Biomaterials. 2008a;29:742–751. doi: 10.1016/j.biomaterials.2007.10.034. [DOI] [PubMed] [Google Scholar]
- Lee CH, Kim EY, Jeon K, Tae JC, Lee KS, Kim YO, et al. Simple, efficient, and reproducible gene transfection of mouse embryonic stem cells by magnetofection. Stem Cells Dev. 2008b;17:133–142. doi: 10.1089/scd.2007.0064. [DOI] [PubMed] [Google Scholar]
- Li K, Welikson RE, Vikstrom KL, Leinwand LA. Direct gene transfer into mouse heart. J Mol Cell Cardiol. 1997;29:1499–1504. doi: 10.1006/jmcc.1997.0389. [DOI] [PubMed] [Google Scholar]
- Li T, Tachibana K, Kuroki M, Kuroki M. Gene transfer with echo-enhanced contrast agents: comparison between Albunex, Optison, and Levovist in mice – initial results. Radiology. 2003;229:423–428. doi: 10.1148/radiol.2292020500. [DOI] [PubMed] [Google Scholar]
- Lindmayer I, Menassa K, Lambert J, Moghrabi A, Legendre L, Legault C, et al. Development of new jet injector for insulin therapy. Diabetes Care. 1986;9:294–297. doi: 10.2337/diacare.9.3.294. [DOI] [PubMed] [Google Scholar]
- Liu CW, Lin CC, Chen JJ, Tseng MJ. Stable chloroplast transformation in cabbage (Brassica oleracea L. var. capitata L.) by particle bombardment. Plant Cell Rep. 2007;26:1733–1744. doi: 10.1007/s00299-007-0374-z. [DOI] [PubMed] [Google Scholar]
- Liu F, Huang L. Improving plasmid DNA-mediated liver gene transfer by prolonging its retention in the hepatic vasculature. J Gene Med. 2001;3:569–576. doi: 10.1002/jgm.222. [DOI] [PubMed] [Google Scholar]
- Liu F, Song Y, Liu D. Hydrodynamics-based transfection in animals by systemic administration of plasmid DNA. Gene Ther. 1999;6:1258–1266. doi: 10.1038/sj.gt.3300947. [DOI] [PubMed] [Google Scholar]
- Liu Y, Yang H, Sakanishi A. Ultrasound: mechanical gene transfer into plant cells by sonoporation. Biotechnol Adv. 2005;24:1–16. doi: 10.1016/j.biotechadv.2005.04.002. [DOI] [PubMed] [Google Scholar]
- Loehr BI, Willson P, Babiuk LA, van Drunen Little-van den Hurk S. Gene gun-mediated DNA immunization primes development of mucosal immunity against bovine herpes virus 1 in cattle. J Virol. 2000;74:6077–6086. doi: 10.1128/jvi.74.13.6077-6086.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu QL, Liang HD, Partridge T, Blomley MJ. Microbubble ultrasound improves the efficiency of gene transduction in skeletal muscle in vivo with reduced tissue damage. Gene Ther. 2003;10:396–405. doi: 10.1038/sj.gt.3301913. [DOI] [PubMed] [Google Scholar]
- Lubbe AS, Bergemann C, Riess H, Schriever F, Reichardt P, Possinger K, et al. Clinical experiences with magnetic drug targeting: a phase I study with 4′-epidoxorubicin in 14 patients with advanced solid tumours. Cancer Res. 1996;56:4686–4693. [PubMed] [Google Scholar]
- Luz Garcia-Hernandez M, Gray A, Hubby B, Klinger O, Kast WM. Prostate stem cell antigen vaccination induces a long-term protective immune response against prostate cancer in the absence of autoimmunity. Cancer Res. 2008;68:861–869. doi: 10.1158/0008-5472.CAN-07-0445. [DOI] [PubMed] [Google Scholar]
- Marty M, Sersa G, Garbay JR, Gehl J, Collins CG, Snoj M, et al. Electrochemotherapy – an easy, highly effective and safe treatment of cutaneous and subcutaneous metastases: results of ESOPE (European Standard Operating Procedures of Electrochemotherapy) study. Eur J Cancer. 2006;(4) Suppl:3–13. [Google Scholar]
- Maruyama H, Higuchi N, Nishikawa Y, Kameda S, Iino N, Kazama JJ, et al. High-level expression of naked DNA delivered to rat liver via tail vein injection. J Gene Med. 2002;4:333–341. doi: 10.1002/jgm.281. [DOI] [PubMed] [Google Scholar]
- Matsuno Y, Iwata H, Umeda Y, Takagi H, Mori Y, Miyazaki J, et al. Non-viral gene gun mediated transfer into the beating heart. ASAIO J. 2003;49:641–644. doi: 10.1097/01.mat.0000093746.63497.ae. [DOI] [PubMed] [Google Scholar]
- Matthews K, Rhind SM, Gossner AG, Dalziel RG, Hopkins J. The effects of gene gun delivered pIL-3 adjuvant on skin pathology and cytokine expression. Vet Immunol Immunopathol. 2007;119:233–242. doi: 10.1016/j.vetimm.2007.05.021. [DOI] [PubMed] [Google Scholar]
- Miao CH, Brayman AA, Loeb KR, Ye P, Zhou L, Mourad P, et al. Ultrasound enhances gene delivery of human factor IX plasmid. Hum Gene Ther. 2005;16:893–905. doi: 10.1089/hum.2005.16.893. [DOI] [PubMed] [Google Scholar]
- Mikata K, Uemura H, Ohuchi H, Ohta S, Nagashima Y, Kubota Y. Inhibition of growth of human prostate cancer xenograft by transfection of p53 gene: gene transfer by elecroporation. Mol Cancer Ther. 2002;1:247–252. [PubMed] [Google Scholar]
- Miller DL, Song J. Tumor growth reduction and DNA transfer by cavitation-enhanced high-intensity focused ultrasound in vivo. Ultrasound Med Biol. 2003;29:887–893. doi: 10.1016/s0301-5629(03)00031-0. [DOI] [PubMed] [Google Scholar]
- Mir LM, Belehradek M, Domenge C, Orlowski S, Poddevin B, Belehradek J, Jr, et al. Electrochemotherapy, a new antitumor treatment: first clinical trial. C R Acad Sci III. 1991;313:613–618. [PubMed] [Google Scholar]
- Mir LM, Bureau MF, Rangara R, Schwartz B, Scherman D. Long term, high level in vivo gene expression after electric pulse-mediated gene transfer into skeletal muscle. C R Acad Sci III. 1998;321:893–899. doi: 10.1016/s0764-4469(99)80003-1. [DOI] [PubMed] [Google Scholar]
- Mir LM, Bureau MF, Gehl J, Rangara R, Rouy D, Caillaud JM, et al. High-efficiency gene transfer into skeletal muscle mediated by electric pulses. Proc Natl Acad Sci USA. 1999;96:4262–4267. doi: 10.1073/pnas.96.8.4262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mir LM, Moller PH, André F, Gehl J. Electric pulse-mediated gene delivery to various animal tissues. Adv Genet. 2005;54:83–114. doi: 10.1016/S0065-2660(05)54005-7. [DOI] [PubMed] [Google Scholar]
- Mir LM, Gehl J, Sersa G, Collins CG, Garbay JR, Billard V, et al. Standard operating procedures of the electrochemotherapy: instructions for the use of bleomycin or cisplatin administered either systemically or locally and electric pulses delivered by the CliniporatorTM by means of invasive or non-invasive électrodes. Eur J Cancer. 2006;4(Suppl):14–25. [Google Scholar]
- Nakamura M, Wang J, Murakami T, Ajiki T, Hakamata Y, Kaneko T, et al. DNA immunization of the grafted liver by particle-mediated gene gun. Transplantation. 2003;15:1369–1375. doi: 10.1097/01.TP.0000091118.22413.E1. [DOI] [PubMed] [Google Scholar]
- Neumann E, Schaefer-Ridder M, Wang Y, Hofscheider PH. Gene transfer into mouse lyoma cells by electroporation in high electric fields. EMBO J. 1982;1:841–845. doi: 10.1002/j.1460-2075.1982.tb01257.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman CM, Laurie A, Brisken AF, Cumberland DC. Ultrasound gene therapy: on the road from concept to reality. Echocardiography. 2001;18:339–347. doi: 10.1046/j.1540-8175.2001.00339.x. [DOI] [PubMed] [Google Scholar]
- Ng KY, Liu Y. Therapeutic ultrasound: its application in drug delivery. Med Res Rev. 2002;22:204–223. doi: 10.1002/med.10004. [DOI] [PubMed] [Google Scholar]
- Niidome T, Huang L. Gene therapy progress and prospects: non-viral vectors. Gene Ther. 2002;9:1647–1652. doi: 10.1038/sj.gt.3301923. [DOI] [PubMed] [Google Scholar]
- O'Brien J, Lummis SC. Biolistic and diolistic transfection: using the gene gun to deliver DNA and lipophilic dyes into mammalian cells. Methods. 2004;33:121–125. doi: 10.1016/j.ymeth.2003.11.010. [DOI] [PubMed] [Google Scholar]
- Plank C, Schillinger U, Scherer F, Bergemann C, Remy JS, Krotz F, et al. The magnetofection method: using magnetic force to enhance gene delivery. Biol Chem. 2003;384:737–747. doi: 10.1515/BC.2003.082. [DOI] [PubMed] [Google Scholar]
- Porgador A, Irvine KR, Iwasaki A, Barber BH, Restifo NP, Germain RN. Predominant role for directly transfected dendritic cells in antigen presentation to CD8+ cells after gene gun immunization. J Exp Med. 1998;188:1075–1082. doi: 10.1084/jem.188.6.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potter H, Weir L, Leder P. Enhancer-dependent expression of human kappa immunoglobulin genes introduced into mouse pre-B lymphocytes by electroporation. Proc Natl Acad Sci USA. 1984;81:7161–7165. doi: 10.1073/pnas.81.22.7161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prentice P, Cuschierp A, Dholakia K, Prausnitz M, Campbell P. Membrane disruption by optically controlled microbubble cavitation. Nat Phys. 2005;1:107–110. [Google Scholar]
- Raghavan R, Brady ML, Rodríguez-Ponce MI, Hartlep A, Pedain C, Sampson JH. Convection-enhanced delivery of therapeutics for brain disease, and its optimization. Neurosurg Focus. 2006;20:E12. doi: 10.3171/foc.2006.20.4.7. [DOI] [PubMed] [Google Scholar]
- Rajaratnam N, Steffler PM, Rizvi SAH, Smy PR. An experimental study of very high velocity circular water jets in air. J Hydraul Res. 1994;32:461–470. [Google Scholar]
- Remacle C, Cardol P, Coosemans N, Gaisne M, Bonnefoy N. High-efficiency biolistic transformation of Chlamydomonas mitochondria can be used to insert mutations in complex I genes. Proc Natl Acad Sci USA. 2006;103:4771–4776. doi: 10.1073/pnas.0509501103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren S, Li M, Smith JM, DeTolla LJ, Furth PA. Low-volume jet injection for intradermal immunization in rabbits. BMC Biotechnol. 2002;23:2–10. doi: 10.1186/1472-6750-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberto RR, Wulff H, Millar JD. Smallpox vaccination by intradermal jet injection. 2. Cutaneous and serological responses to primary vaccination in children. Bull World Health Organ. 1969;41:761–769. [PMC free article] [PubMed] [Google Scholar]
- Robinson M, Sharon A. Transformation of the bioherbicide Colletotrichum gloeosporioides f. sp Aeschynomene by electroporation of germinated conidia. Curr Genet. 1999;36:98–104. doi: 10.1007/s002940050478. [DOI] [PubMed] [Google Scholar]
- Rols MP, Delteil C, Golzio M, Dumond P, Cros S, Teissié J. In vivo electrically mediated protein and gene transfer in murine melanoma. Nat Biotechnol. 1998;16:168–171. doi: 10.1038/nbt0298-168. [DOI] [PubMed] [Google Scholar]
- Satkauskas S, Bureau MF, Puc M, Mahfoudi A, Scherman D, Miklavcic D, et al. Mechanisms of in vivo DNA electrotransfer: respective contributions of cell electropermeabilization and DNA electrophoresis. Mol Ther. 2002;5:133–140. doi: 10.1006/mthe.2002.0526. [DOI] [PubMed] [Google Scholar]
- Satkauskas S, André F, Bureau MF, Scherman D, Miklavcic D, Mir LM. Electrophoretic component of electric pulses determines the efficacy of in vivo DNA electrotransfer. Hum Gene Ther. 2005;16:1194–1201. doi: 10.1089/hum.2005.16.1194. [DOI] [PubMed] [Google Scholar]
- Sawamura D, Ina S, Itai K, Meng X, Kon A, Tamai K, et al. In vivo gene introduction into keratinocytes using jet injection. Gene Ther. 1999;6:1785–1787. doi: 10.1038/sj.gt.3301002. [DOI] [PubMed] [Google Scholar]
- Sawyer GJ, Dong X, Whitehorne M, Grehan A, Seddon M, Shah AM, et al. Cardiovascular function following acute volume overload for hydrodynamic gene delivery in the liver. Gene Ther. 2007;14:1208–1217. doi: 10.1038/sj.gt.3302976. [DOI] [PubMed] [Google Scholar]
- Sawyer GJ, Grehan A, Dong X, Whitehorne M, Seddon M, Shah AM, et al. Low-volume hydrodynamic gene delivery to the rat liver via an isolated segment of the inferior vena cava: efficiency, cardiovascular response and intrahepatic vascular dynamics. J Gene Med. 2008;10:540–550. doi: 10.1002/jgm.1176. [DOI] [PubMed] [Google Scholar]
- Schlicher RK, Radhakrishna H, Tolentino TP, Apkarian RP, Zarnitsyn V, Prausnitz MR. Mechanism of intracellular delivery by acoustic cavitation. Ultrasound Med Biol. 2006;32:915–924. doi: 10.1016/j.ultrasmedbio.2006.02.1416. [DOI] [PubMed] [Google Scholar]
- Schramm-Baxter JR, Katrenick J, Mitragotri S. Jet injection into polyacrylamide gels: investigation of jet injection mechanisms. J Biomech. 2004;37:1181–1188. doi: 10.1016/j.jbiomech.2003.12.006. [DOI] [PubMed] [Google Scholar]
- Schratzberger P, Krainin JG, Schratzberger G, Silver M, Ma H, Kearney M, et al. Transcutaneous ultrasound augments naked DNA transfection of skeletal muscle. Mol Ther. 2002;6:576–583. [PubMed] [Google Scholar]
- Schwan HP. Electrical properties of tissue and cell suspensions. Adv Biol Med Phys. 1957;5:147–209. doi: 10.1016/b978-1-4832-3111-2.50008-0. [DOI] [PubMed] [Google Scholar]
- Sebestyen MG, Budker VG, Budker T, Subbotin VM, Zhang G, Monahan SD, et al. Mechanism of plasmid delivery by hydrodynamic tail vein injection. I. Hepatocyte uptake of various molecules. J Gene Med. 2006;8:852–873. doi: 10.1002/jgm.921. [DOI] [PubMed] [Google Scholar]
- Sersa G, Miklavcic D, Cemazar M, Rudolf Z, Pucihar G, Snoj M. Electrochemotherapy in treatment of tumours. Eur J Surg Oncol. 2008;34:232–240. doi: 10.1016/j.ejso.2007.05.016. [DOI] [PubMed] [Google Scholar]
- Shestopalov VI, Missey H, Bassnett S. Delivery of genes and fluorescent dyes into cells of the intact lens by particle bombardment. Exp Eye Res. 2002;74:639–649. doi: 10.1006/exer.2002.1191. [DOI] [PubMed] [Google Scholar]
- Siegel R, Stein U, Kobelt D, Aumann J, Schlag PM, Walther W. Early results of a phase-I-clinical trial of non-viral gene transfer by jet-injection into cutaneous lesions of metastatic breast cancer and in-transit lesions of metastatic melanoma. Chir Forum. 2007;36:441–443. [Google Scholar]
- Sikes M, O'Malley BW, Jr, Finegold MJ, Ledley FD. In vivo gene transfer into rabbit thyroid follicular cells by direct DNA injection. Hum Gene Ther. 1994;5:837–844. doi: 10.1089/hum.1994.5.7-837. [DOI] [PubMed] [Google Scholar]
- Skorpikova J, Dolnikova M, Hrazdira I, Janisch R. Changes in microtubules and microfilaments due to a combined effect of ultrasound and cytostatics in HeLa cells. Folia Biol (Praha) 2001;47:143–147. [PubMed] [Google Scholar]
- Smith NB. Perspectives on transdermal ultrasound mediated drug delivery. J Nanomedicine. 2007;2:585–594. [PMC free article] [PubMed] [Google Scholar]
- Stein U, Walther W, Stege A, Kaszubiak A, Fichtner I, Lage H. Complete in vivo reversal of the multidrug resistance phenotype by jet-injection of anti-MDR1 short hairpin RNA-endoding plasmid DNA. Mol Ther. 2008;16:178–186. doi: 10.1038/sj.mt.6300304. [DOI] [PubMed] [Google Scholar]
- Suda T, Suda K, Liu D. Computer-assisted hydrodynamic gene delivery. Mol Ther. 2008;16:1098–1104. doi: 10.1038/mt.2008.66. [DOI] [PubMed] [Google Scholar]
- Sudha PM, Low S, Kwang J, Gong Z. Multiple tissue transformation in adult zebrafish by gene gun bombardment and muscular injection of naked DNA. Mar Biotechnol. 2001;3:119–125. doi: 10.1007/s101260000056. [DOI] [PubMed] [Google Scholar]
- Suzuki T, Shin BC, Fujikura K, Matsuzaki T, Takata K. Direct gene transfer into rat liver cells by in vivo electroporation. FEBS Lett. 1998;425:436–440. doi: 10.1016/s0014-5793(98)00284-1. [DOI] [PubMed] [Google Scholar]
- Taketo A. DNA transfection of Escherichia coli by electroporation. Biochim Biophys Acta. 1988;949:318–324. doi: 10.1016/0167-4781(88)90158-3. [DOI] [PubMed] [Google Scholar]
- Taniyama Y, Tachibana K, Hiraoka K, Aoki M, Yamamoto S, Matsumoto K, et al. Development of safe and efficient novel non-viral gene transfer using ultrasound: enhancement of transfection efficiency of naked plasmid DNA in skeletal muscle. Gene Ther. 2002a;9:372–380. doi: 10.1038/sj.gt.3301678. [DOI] [PubMed] [Google Scholar]
- Taniyama Y, Tachibana K, Hiraoka K, Namba T, Yamasaki K, Hashiya N, et al. Local delivery of plasmid DNA into rat carotid artery using ultrasound. Circulation. 2002b;105:1233–1239. doi: 10.1161/hc1002.105228. [DOI] [PubMed] [Google Scholar]
- Tata DB, Dunn F, Tindall DJ. Selective clinical ultrasound signals mediate differential gene transfer and expression in two human prostate cancer cell lines: LnCap and PC-3. Biochem Biophys Res Commun. 1997;234:64–67. doi: 10.1006/bbrc.1997.6578. [DOI] [PubMed] [Google Scholar]
- Teissié J, Rols MP. An experimental evaluation of the critical potential difference inducing cell membrane electropermeabilization. Biophys J. 1993;65:409–413. doi: 10.1016/S0006-3495(93)81052-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teissié J, Golzio M, Rols MP. Mechanisms of cell membrane electropermeabilization: a minireview of our present (lack of ?) knowledge. Biochim Biophys Acta. 2005;1724:270–280. doi: 10.1016/j.bbagen.2005.05.006. [DOI] [PubMed] [Google Scholar]
- Tieleman DP. Computer simulations of transport through membranes: passive diffusion, pores, channels and transporters. Clin Exp Pharmacol Physiol. 2006;33:893–903. doi: 10.1111/j.1440-1681.2006.04461.x. [DOI] [PubMed] [Google Scholar]
- Tieleman DP, Leontiadou H, Mark AE, Marrink SJ. Simulation of pore formation in lipid bilayers by mechanical stress and electric fields. J Am Chem Soc. 2003;125:6382–6383. doi: 10.1021/ja029504i. [DOI] [PubMed] [Google Scholar]
- Tsong TY. Electroporation of cell membranes. Biophys J. 1991;60:297–306. doi: 10.1016/S0006-3495(91)82054-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsong TY, Su ZD. Biological effects of electric shock and heat dénaturation and oxidation of molécules, membranes, and cellular functions. Ann N Y Acad Sci. 1999;888:211–232. doi: 10.1111/j.1749-6632.1999.tb07958.x. [DOI] [PubMed] [Google Scholar]
- Tuting T, Storkus WJ, Falo LD. DNA immunization targeting the skin: molecular control of adaptive immunity. J Invest Dermatol. 1998;111:183–188. doi: 10.1046/j.1523-1747.1998.00261.x. [DOI] [PubMed] [Google Scholar]
- Uchida T, Sanghyi NT, Gardner TA, Koch MO, Ishii D, Minei S, et al. Transrectal high-intensity focused ultrasound for treatment of patients with stage T1b-2n0m0 localized prostate cancer: a preliminary report. Urology. 2002;59:394–399. doi: 10.1016/s0090-4295(01)01624-7. [DOI] [PubMed] [Google Scholar]
- Van Bockstaele F, Pede V, Naessens E, Van Coppernolle S, Van Tendeloo V, Verhasselt B, et al. Efficient gene transfer in CLL by mRNA electroporation. Leukemia. 2008;22:323–329. doi: 10.1038/sj.leu.2405007. [DOI] [PubMed] [Google Scholar]
- Verhagen A, Ebels KT, Dogterom AA, Jonkman JH. Pharmacokinectics and pharmacodynamics of a single dose of recombinant human growth hormone after subcutaneous administration by jet-injection: comparison with conventional needle-injection. Eur J Clin Pharmacol. 1995;49:69–72. doi: 10.1007/BF00192361. [DOI] [PubMed] [Google Scholar]
- Voges J, Reszka R, Gossmann A, Dittmar C, Richter R, Garlip G, et al. Imaging-guided convection-enhanced delivery and gene therapy of glioblastoma. Ann Neurol. 2003;54:479–487. doi: 10.1002/ana.10688. [DOI] [PubMed] [Google Scholar]
- Walther W, Stein U, Fichtner I, Malcherek L, Lemm M, Schlag PM. Non-viral in vivo gene delivery into tumours using a novel low volume jet-injection technology. Gene Ther. 2001;8:173–180. doi: 10.1038/sj.gt.3301350. [DOI] [PubMed] [Google Scholar]
- Walther W, Stein U, Fichtner I, Kobelt D, Aumann J, Arlt F, et al. Non-viral jet-injection gene transfer for efficient in vivo cytosine deaminase suicide gene therapy of colon carcinoma. Mol Ther. 2005;12:1176–1184. doi: 10.1016/j.ymthe.2005.07.700. [DOI] [PubMed] [Google Scholar]
- Wang S, Joshi S, Lu S. Delivery of DNA to skin by particle bombardment. Methods Mol Biol. 2004;245:185–193. doi: 10.1385/1-59259-649-5:185. [DOI] [PubMed] [Google Scholar]
- Wang X, Liang HD, Dong B, Lu QL, Blomley MJ. Gene transfer with microbubble ultrasound and plasmid DNA into skeletal muscle of mice: comparison between commercially available microbubble contrast agents. Radiology. 2005;237:224–229. doi: 10.1148/radiol.2371040805. [DOI] [PubMed] [Google Scholar]
- Warren J, Ziherl FA, Kish AW, et al. Large-scale administration of vaccines by means of an automatic jet injection syringue. JAMA. 1953;157:633–637. doi: 10.1001/jama.1955.02950250007003. [DOI] [PubMed] [Google Scholar]
- Watkins C, Hopkins J, Harkiss G. Reporter gene expression in dendritic cells after gene gun administration of plasmid DNA. Vaccine. 2005;23:4247–4256. doi: 10.1016/j.vaccine.2005.03.023. [DOI] [PubMed] [Google Scholar]
- Weller C, Linder M. Jet injection of insulin vs the syringe-and-needle method. JAMA. 1966;195:844–847. doi: 10.1001/jama.1966.03100100096027. [DOI] [PubMed] [Google Scholar]
- Wells DJ. Gene therapy progress and prospects: electroporation and other physical methods. Gene Ther. 2004;11:1363–1369. doi: 10.1038/sj.gt.3302337. [DOI] [PubMed] [Google Scholar]
- Williams RS, Johnston SA, Riedy M, DeVit MJ, McElligott SG, Sanford JC. Introduction of foreign genes into tissues of living mice by DNA-coated microprojectiles. Proc Natl Acad Sci USA. 1991;88:2726–2730. doi: 10.1073/pnas.88.7.2726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff JA, Budker V. The mechanism of naked DNA uptake and expression. Adv Genet. 2005;54:3–20. doi: 10.1016/S0065-2660(05)54001-X. [DOI] [PubMed] [Google Scholar]
- Wolff JA, Malone RW, Williams P, Chong W, Acsadi G, Jani A, et al. Direct gene transfer into mouse muscle in vivo. Science. 1990;247:1465–1468. doi: 10.1126/science.1690918. [DOI] [PubMed] [Google Scholar]
- Wolff JA, Williams P, Acsadi G, Jiao S, Jani A, Chong W. Conditions affecting direct gene transfer into rodent muscle in vivo. Biotechniques. 1991;11:474–485. [PubMed] [Google Scholar]
- Wu F, Wang ZB, Chen WZ, Wang W, Gui Y, Zhang M, et al. Extracorporeal high intensity focused ultrasound ablation in the treatment of 1038 patients with solid carcinomas in China: an overview. Ultrason Sonochem. 2004;11:149–154. doi: 10.1016/j.ultsonch.2004.01.011. [DOI] [PubMed] [Google Scholar]
- Xenariou S, Griesenbach U, Ferrari S, Dean P, Scheule RK, Cheng SH, et al. Using magnetic forces to enhance non-viral gene transfer to airway epithelium in vivo. Gene Ther. 2006;13:1545–1552. doi: 10.1038/sj.gt.3302803. [DOI] [PubMed] [Google Scholar]
- Yamashita Y, Shimada M, Tachibana K, Harimoto N, Tsujita E, Shirabe K, et al. In vivo gene transfer into muscle via electro-sonoporation. Hum Gene Ther. 2002;13:2079–2084. doi: 10.1089/10430340260395929. [DOI] [PubMed] [Google Scholar]
- Yang NS, Sun WH. Gene gun and other non-viral approaches for cancer gene therapy. Nat Med. 1995;1:481–483. doi: 10.1038/nm0595-481. [DOI] [PubMed] [Google Scholar]
- Yang NS, Burkholder J, Roberts B, Martinell B, McCabe D. In vivo and in vitro gene transfer to mammalian somatic cells by particle bombardment. Proc Natl Acad Sci USA. 1990;87:9568–9572. doi: 10.1073/pnas.87.24.9568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang SY, Sun JS, Liu CH, Tsuang YH, Chen LT, Hong CY, et al. Ex vivo magnetofection with magnetic nanoparticles: a novel platform for non-viral tissue engineering. Artif Organs. 2008;32:195–204. doi: 10.1111/j.1525-1594.2007.00526.x. [DOI] [PubMed] [Google Scholar]
- Zagon IS, Sassani JW, Verderame MF, McLaughlin PJ. Particle-mediated gene transfer of opioid growth factor receptor cDNA regulates cell proliferation of the corneal epithelium. Cornea. 2005;24:614–619. doi: 10.1097/01.ico.0000153561.89902.57. [DOI] [PubMed] [Google Scholar]
- Zarnitsyn VG, Prausnitz MR. Physical parameters influencing optimization of ultrasound-mediated DNA transfection. Ultrasound Med Biol. 2004;30:527–538. doi: 10.1016/j.ultrasmedbio.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Zelenin AV, Kolesnikov VA, Tarasenko OA, Shafei RA, Zelenina IA, Mikhailov VV, et al. Bacterial beta-galactosidase and human dystrophin genes are expressed in mouse skeletal muscle fibers after ballistic transfection. FEBS Lett. 1997;414:319–322. doi: 10.1016/s0014-5793(97)01019-3. [DOI] [PubMed] [Google Scholar]
- Zerbib D, Amalric F, Teissié J. Electric field mediated transformation: isolation and characterization of a TK+ subclone. Biochem Biophys Res Commun. 1985;129:611–618. doi: 10.1016/0006-291x(85)91935-7. [DOI] [PubMed] [Google Scholar]
- Zhang G, Selzer ME. In vivo transfection of lamprey brain neurons by gene gun delivery of DNA. Exp Neurol. 2001;167:304–311. doi: 10.1006/exnr.2000.7584. [DOI] [PubMed] [Google Scholar]
- Zhang G, Vargo D, Budker V, Armstrong N, Knechtle S, Wolff JA. Expression of naked plasmid DNA injected into the afferent and efferent vessels of rodent and dog livers. Hum Gene Ther. 1997;8:1763–1772. doi: 10.1089/hum.1997.8.15-1763. [DOI] [PubMed] [Google Scholar]
- Zhang G, Budker V, Wolff JA. High levels of foreign gene expression in hepatocytes after tail vein injections of naked plasmid DNA. Hum Gene Ther. 1999;10:1735–1737. doi: 10.1089/10430349950017734. [DOI] [PubMed] [Google Scholar]
- Zhang G, Budker V, Williams P, Subbotin V, Wolff JA. Efficient expression of naked DNA delivered intra-arterially to limb muscles of nonhuman primates. Hum Gene Ther. 2001;12:427–438. doi: 10.1089/10430340150504046. [DOI] [PubMed] [Google Scholar]
- Zhang G, Gao X, Song YK, Vollmer R, Stolz DB, Gasiorowski JZ, et al. Hydroporation as the mechanism of hydrodynamic delivery. Gene Ther. 2004;11:675–682. doi: 10.1038/sj.gt.3302210. [DOI] [PMC free article] [PubMed] [Google Scholar]


