Abstract
Background:
When laparoscopic cholecystectomy (LC) is performed successfully, recovery is faster than after open cholecystectomy. However, LC results in higher incidences of biliary, bowel and vascular injury.
Methods:
We performed a retrospective review of LC-related claims reported to the National Health Service Litigation Authority (NHSLA) during 2000–2005. The data were analysed from a medicolegal perspective to assess the effects of type of injury and delay in recognition on litigation costs.
Results:
A total of 208 claims following laparoscopic procedures in general surgery were reported to NHSLA during 2000–2005, of which 133 (64%) were related to LC. Bile duct injury (BDI) accounted for the majority of claims (72%); bowel injury and ‘others’ accounted for 9% and 19%, respectively. Only 20% of BDIs were recognized during surgery; the majority were missed and diagnosed later. Claims related to LC resulted in payments totalling £6 m, of which £4.3 m was paid out for BDIs. The average cost was higher for patients who suffered a delay in diagnosis, as was the chance of a successful claim.
Conclusions:
Bile duct injury incurred during LC remains a serious hazard for patients. The resulting complications have led to litigation that has caused a huge financial drain on the health care system. Delayed recognition appears to correlate with more costly litigation.
Keywords: laparoscopic cholecystectomy, bile duct injuries, malpractice claims, litigations, delayed recognition of injury
Introduction
Laparoscopic cholecystectomy (LC) is regarded as the gold standard for the treatment of symptomatic gallstones. Since the introduction of laparoscopic surgery in the late 1980s,1,2 laparoscopic procedures, and LC in particular, have become well established in surgical residency training programmes. Major developments in technology have improved visualization and instrumentation. However, despite the improvements in equipment and training,3 the rate of bile duct injury (BDI) continues to be higher after LC than after open cholecystectomy (OC).4–7 Reports of the incidence of BDI after OC lie in the range of 0.1–0.3% (giving an average of one in 500 cases),8,9 whereas the incidence of BDI after LC is reported to be 0.15–0.7% (or an average of one in 200 cases).10–12 It appears that this risk remains higher for LC, even after a surgeon has gained experience and has passed the ‘learning curve’.13 It is thought that the lack of 3-dimensional vision and problems with perception inherent in laparoscopic surgery result in spatial disorientation and the misidentification of biliary anatomy, and these issues lead to more complications.
There are very few published data in the English language on litigation rates, factors affecting litigation or costs of litigation.14 Litigation after OC is uncommon; a report of OC-related litigation in the literature identified only 49 cases over a 20-year period.15 The few studies available from the USA appear to show a much higher incidence of litigation after LC compared with OC.16 The present study reports data from the National Health Service Litigation Authority (NHSLA) in the UK.
Materials and methods
We performed a retrospective review of claims relating to laparoscopic surgery reported to NHSLA for England from April 2000 to March 2005. The NHSLA is a special health authority (partof the NHS) set up in 1995 by the Department of Health and is responsible for handling negligence claims made against NHS bodies in England. The data were collected from a legal and health care management perspective, not from a clinical perspective. The subset of data that applied to LC were analysed on a case-by-case basis. The information available from NHSLA was limited as a result of issues relating to patient confidentiality. Data were anonymous with regard to surgeon, hospital, and age and sex of the patient. It was not possible to trace hospital records to obtain any information additional to that available in the NHSLA records. The clinical data in a number of cases were inadequate to allow comment on the cause of the injury and did not indicate whether an operative cholangiogram had been performed, the exact level or type of BDI, whether endoscopic retrograde cholangiopancreatography had been performed, or give details of how the injury had been managed.
The data were analysed with respect to type of injury (biliary, bowel, vascular, bleeding, miscellaneous), delay in recognition of the injury, mortality, and litigation costs. Vascular injuries to hepatic or portal vessels that occurred concomitantly with BDIs were classified as BDIs, whereas major vascular injuries resulting from Veress needle or trocar were grouped as vascular injuries. The miscellaneous causes of litigation included preoperative factors, diathermy burns, communication errors, and postoperative complications such as deep venous thrombosis, pulmonary embolism, pancreatitis and small bowel obstruction. The BDIs were subgrouped into those recognized at the time of the index operation and those recognized in the postoperative period. It was not possible to analyse the duration of delay in individual cases or to assess whether the delay resulted in clinical deterioration.
Results
A total of 208 claims were reported following laparoscopic procedures performed in general surgery over the 5-year period from April 2000 to March 2005 in England. The claims were grouped according to the index year of the original laparoscopic surgery. Of the claims, 133 (64%) concerned complications relating to LC (Fig. 1). Of these 133 LC-related claims, 116 were settled and 17 were still open at the time of data collection. Only 116 claims were analysed for this study. Bile duct injuries (83/116) accounted for the majority (72%) of the LC claims; other claims referred to bowel injury (9%), bleeding (4%), vascular damage (3%) and miscellaneous problems (12%). There were a total of seven deaths (6% mortality) following BDI and 12 deaths (9%) following all LC-related injuries amongst the claimants.
Figure 1.
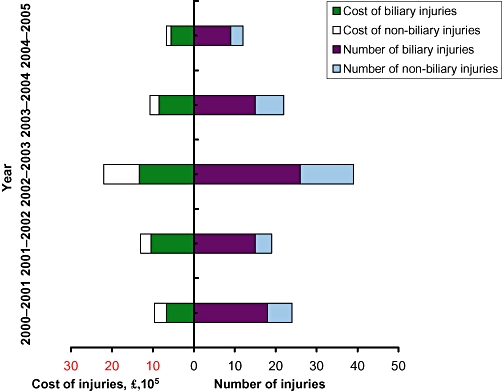
Total number of litigation actions brought for injuries related to laparoscopic cholecystectomy over the 5-year period 2000–2005, showing the relative contribution of biliary injuries, and costs incurred to settle the claims, showing the relative contribution of claims for biliary injuries
Financial compensation and type of injury
A total of £6.3 m (mean £53 863) was paid out to settle the 116 claims emanating from LC. Of this, £4.4 m (mean £53 901) related to claims for BDIs (Fig. 2). This figure includes both damages paid to patients and the legal costs borne by the NHS. A total of 80% (66/83) of the cases involving BDI in this study were settled in favour of the plaintiff. There was no significant difference between the cost of malpractice related to a BDI and that related to other complications from LC; however, the average payout was significantly higher (£89 930) for claims emanating from BDI that resulted in death.
Figure 2.
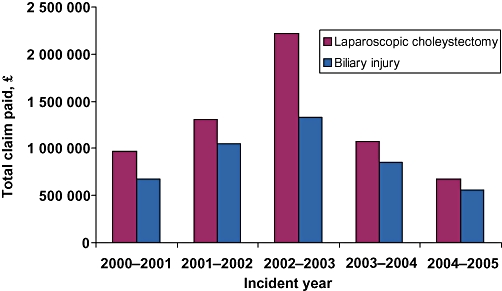
Total payments made to settle all claims for injuries occurring during laparoscopic cholecystectomy (LC) and the proportion attributed to bile duct injuries over the 5-year period 2000–2005
Success of litigation and timing of recognition of injury
Only 17 of 83 (20%) incidents of BDI were recognized at the time of surgery. The majority (64/83) were missed at surgery, resulting in late diagnosis (Fig. 3). The data were inadequate for two cases with regard to the timing of detection of injury. Only half the claims for injuries that had been recognized promptly were successful, whereas 90% of the claims for BDIs that were recognized later were successful.
Figure 3.
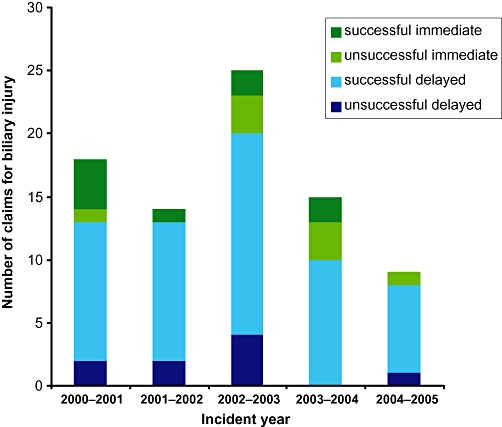
Numbers of bile duct injuries recognized at the time of the index operation compared with those recognized later, by year. About 90% of claims for injuries recognized later succeeded, whereas only 50% of claims for injuries recognized during index surgery were successful
Financial compensation and timing of recognition of injury
A total of £3.98 m was paid out to settle claims for injuries where diagnosis was delayed, resulting in an average of £62 248 per claim. £0.36 m was paid out for injuries that were recognized promptly, giving an average of £21 497 per claim. If the unsuccessful claims are excluded, the average compensation paid for injuries where diagnosis was delayed was £72 435, compared with £40 000 for those recognized early.
Discussion
Statistically, surgeons are more at risk of litigation following LC than they are after any other general surgical procedure. Litigation after OC is rare and the only report of OC litigation in the literature identified only 49 cases over a 20-year period.15 It is not clear why this is so because complications are known to occur during OC. Currently, the majority of OCs are selected (often the most difficult cases), and biliary complications may be even higher than after LC.17 A variety of factors may play a role in the increased incidence of litigation following LC. These include: failure of the surgeon to fully inform the patient of the risks involved in the procedure; greater expectation on the part of the patient of a quick and smooth recovery after laparoscopic surgery, and greater likelihood that recognition of an injury that occurs in LC will be delayed. The majority of BDIs from LC were not recognized at the time of the index operation. It has been shown that the longterm outcomes of patients who undergo repair of BDIs are better when the injury is recognized early.5
The majority of comparative data available from the literature come from the USA.4,18,19 Although the datasets refer to two different decades, the figures regarding litigation after LC are surprisingly similar (Table 1). De Reuver et al.14 looked at BDIs reported to an insurance company in the Netherlands over a 13-year period and found that diagnosis of the injury had been delayed in 80% of cases. Similar figures have been reported by other authors: 86% by McLean,4 83% by the Physician Insurers Association of America19 and 80% by Carroll et al.20 It appears from our data that delayed recognition of a BDI strongly correlates with increased risk of litigation. This is probably because delayed recognition is often clinically relevant and can result in poorer outcomes. The present study shows a strong link between failure to recognize BDI at the time of surgery and the success of a resulting claim and higher malpractice costs. The data used in the present study were insufficient to allow for assessment of the role of operative cholangiography in preventing litigation over BDIs. The literature strongly suggests that performing intraoperative cholangiography (IOC) increases the likelihood that a BDI will be recognized at the time of surgery13,21 and therefore may minimize the extent and consequences of the injury.22 Thus IOC may have a role to play in reducing the cost of litigation when an injury occurs, although it does not per sereduce the risk for BDI.
Table 1.
Distribution of injuries occurring during laparoscopic cholecystectomy as reported in the literature
| No. of cases | Bile duct injury | Vascular injury | Bowel injury | Miscellaneous | |
|---|---|---|---|---|---|
| Kern (1997), USA | 44 | 61% | 9% | 9% | 14% |
| Physician Insurers Association of America (1994), USA | 324 | 70% | 9% | 11% | 10% |
| McLean (2006), USA | 104 | 78% | 7% | 2% | 13% |
| de Reuver et al. (2008), Netherlands | 210 | 62% | N/A | N/A | N/A |
| NHSLA, UK (present study) | 133 | 72% | 3% | 9% | 16% |
N/A, information not available; NHSLA, National Health Service Litigation Authority
From the present study, it is not possible to conclude whether lowering the threshold for conversion to open surgery would result in reduced litigation. The reasons for conversion and the timing of conversion with respect to the injury are not clear, and confidentiality precluded us from obtaining individual medical records. It is not clear whether patients who underwent conversion after a BDI made lower malpractice claims than those who did not undergo conversion. However, a surgeon is less likely to cause a BDI during open surgery, and the risk of injury could theoretically be reduced by early conversion.
We found mortality rates of 6% and 9% amongst claimants after BDI and after all LC-related injuries, respectively. This is comparable with reported mortality rates (for all injuries following LC) of 16%18 and 13%4 amongst claimants. The average cost per claim was approximately £53 000 according to the NHSLA database; this is in contrast with average payments per claim of $436 0004 and $500 00015 reported in two studies from the USA. The costs of medical malpractice, including a successful claim for BDI after LC, are significantly lower in England compared with in the USA. The Dutch study reported a mean financial compensation of €12 795,14 which is much less than that in either the UK or the USA. The percentage of claims that were settled in favour of the plaintiff (including by out-of-court settlement and plaintiff jury verdict) was as high as 80% in this study. This is by contrast with the 30% reported in the Dutch series.14 Equivalent figures from the USA vary between 50%18,19 and 86%.20,23
A total of 186 661 LCs took place in the NHS in England between 1 January 2000 and 31 December 2005, giving an average of 31 110 procedures per year. The expected incidence of BDI has been estimated to be 0.33%,24 although much larger numbers of patients suffer a bile leak. We might therefore expect an average of 103 BDIs to occur in England every year. However, an average of 17 BDIs after LC were referred to NHSLA per year over the period of this study. By extrapolation, only about 16% of BDIs in England result in malpractice claims, compared with 20–30% in the USA. These data imply that the litigation figures are a gross underestimate of the overall morbidity suffered by patients as a result of BDI in LC.
The present study was limited by the quality of the available data. Patient confidentiality precluded us from identifying individual cases or accessing medical records. The information available from NHSLA often lacked clinical details and we were unable to draw any conclusions regarding the cause of injury, the seniority or experience of the operating surgeon, the use of operative cholangiography, the extent of delay in diagnosis, the perceived clinical significance of that delay, or how the injury had been managed. There can be considerable delay between the occurrence of a complication and the subsequent claim. We analysed data until March 2005 in the expectation that nearly all cases during that period that had led to litigation would have been referred to NHSLA by the time of our data analysis. However, it is possible that fresh cases come to light more than 2 years after their occurrence.
Some of the published studies were limited by the small samples and selection bias present in legal data banks.18,20 The strength of the present study is that it includes all cases reported over a 5-year period to NHSLA, a central body that oversees all malpractice claims against the NHS in England, and is thus not subject to the specific selection biases that affect other studies.
Conclusions
Laparoscopic cholecystectomy is the largest source of malpractice claims against general surgeons in England. Litigation remains much more common after LC than after OC. Injuries that are not recognized at the index operation are more likely to result in successful claims and are associated with higher settlements. The likelihood and cost of a BDI that results in a malpractice claim are lower in England than in the USA.
Conflicts of interest
None declared.
References
- 1.Reddick EJ, Olsen DO. Laparoscopic laser cholecystectomy. A comparison with mini-lap cholecystectomy. Surg Endosc. 1989;3:131–133. doi: 10.1007/BF00591357. [DOI] [PubMed] [Google Scholar]
- 2.Gadacz TR, Talamini MA, Lillemoe KD, Yeo CJ. Laparoscopic cholecystectomy. Surg Clin North Am. 1990;70:1249–1262. doi: 10.1016/s0039-6109(16)45282-5. [DOI] [PubMed] [Google Scholar]
- 3.Hugh TB. New strategies to prevent laparoscopic bile duct injury – surgeons can learn from pilots. Surgery. 2002;132:826–835. doi: 10.1067/msy.2002.127681. [DOI] [PubMed] [Google Scholar]
- 4.McLean TR. Risk management observations from litigation involving laparoscopic cholecystectomy. Arch Surg. 2006;141:643–648. doi: 10.1001/archsurg.141.7.643. discussion 648. [DOI] [PubMed] [Google Scholar]
- 5.Connor S, Garden OJ. Bile duct injury in the era of laparoscopic cholecystectomy. Br J Surg. 2006;93:158–168. doi: 10.1002/bjs.5266. [DOI] [PubMed] [Google Scholar]
- 6.Windsor JA, Pong J. Laparoscopic biliary injury: more than a learning curve problem. Aust N Z J Surg. 1998;68:186–189. doi: 10.1111/j.1445-2197.1998.tb04742.x. [DOI] [PubMed] [Google Scholar]
- 7.Cohen MM, Young W, Theriault ME, Hernandez R. Has laparoscopic cholecystectomy changed patterns of practice and patient outcome in Ontario? CMAJ. 1996;154:491–500. [PMC free article] [PubMed] [Google Scholar]
- 8.Melton GB, Lillemoe KD, Cameron JL, Sauter PA, Coleman J, Yeo CJ. Major bile duct injuries associated with laparoscopic cholecystectomy: effect of surgical repair on quality of life. Ann Surg. 2002;235:888–895. doi: 10.1097/00000658-200206000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Russell JC, Walsh SJ, Mattie AS, Lynch JT. Bile duct injuries, 1989–1993. A statewide experience. Connecticut Laparoscopic Cholecystectomy Registry. Arch Surg. 1996;131:382–388. doi: 10.1001/archsurg.1996.01430160040007. [DOI] [PubMed] [Google Scholar]
- 10.Walsh RM, Henderson JM, Vogt DP, Mayes JT, Grundfest-Broniatowski S, Gagner M, et al. Trends in bile duct injuries from laparoscopic cholecystectomy. J Gastrointest Surg. 1998;2:458–462. doi: 10.1016/s1091-255x(98)80037-1. [DOI] [PubMed] [Google Scholar]
- 11.Dolan JP, Diggs BS, Sheppard BC, Hunter JG. Ten-year trend in the national volume of bile duct injuries requiring operative repair. Surg Endosc. 2005;19:967–973. doi: 10.1007/s00464-004-8942-6. [DOI] [PubMed] [Google Scholar]
- 12.Richardson MC, Bell G, Fullarton GM. Incidence and nature of bile duct injuries following laparoscopic cholecystectomy: an audit of 5913 cases. West of Scotland Laparoscopic Cholecystectomy Audit Group. Br J Surg. 1996;83:1356–1360. doi: 10.1002/bjs.1800831009. [DOI] [PubMed] [Google Scholar]
- 13.Archer SB, Brown DW, Smith CD, Branum GD, Hunter JG. Bile duct injury during laparoscopic cholecystectomy: results of a national survey. Ann Surg. 2001;234:549–558. doi: 10.1097/00000658-200110000-00014. discussion 558–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Reuver PR, Wind J, Cremers JE, Busch OR, van Gulik TM, Gouma DJ. Litigation after laparoscopic cholecystectomy: an evaluation of the Dutch arbitration system for medical malpractice. J Am Coll Surg. 2008;206:328–334. doi: 10.1016/j.jamcollsurg.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 15.Kern KA. Medicolegal analysis of bile duct injury during open cholecystectomy and abdominal surgery. Am J Surg. 1994;168:217–222. doi: 10.1016/s0002-9610(05)80189-8. [DOI] [PubMed] [Google Scholar]
- 16.Chandler JG, Voyles CR, Floore TL, Bartholomew LA. Litigious consequences of open and laparoscopic biliary surgical mishaps. J Gastrointest Surg. 1997;1:138–145. doi: 10.1016/s1091-255x(97)80101-1. discussion 145. [DOI] [PubMed] [Google Scholar]
- 17.Van de Sande S, Bossens M, Parmentier Y, Gigot JF. National survey on cholecystectomy-related bile duct injury – public health and financial aspects in Belgian hospitals – 1997. Acta Chir Belg. 2003;103:168–180. doi: 10.1080/00015458.2003.11679403. [DOI] [PubMed] [Google Scholar]
- 18.Kern KA. Malpractice litigation involving laparoscopic cholecystectomy. Cost, cause, and consequences. Arch Surg. 1997;132:392–397. doi: 10.1001/archsurg.1997.01430280066009. discussion 397–398. [DOI] [PubMed] [Google Scholar]
- 19.Physician Insurers Association of America. Rockville, MD: Physician Insurers Association of America Laparoscopic Procedure Study; [Google Scholar]
- 20.Carroll BJ, Birth M, Phillips EH. Common bile duct injuries during laparoscopic cholecystectomy that result in litigation. Surg Endosc. 1998;12:310–313. doi: 10.1007/s004649900660. discussion 314. [DOI] [PubMed] [Google Scholar]
- 21.Slater K, Strong RW, Wall DR, Lynch SV. Iatrogenic bile duct injury: the scourge of laparoscopic cholecystectomy. Aust N Z J Surg. 2002;72:83–88. doi: 10.1046/j.1445-2197.2002.02315.x. [DOI] [PubMed] [Google Scholar]
- 22.Olsen D. Bile duct injuries during laparoscopic cholecystectomy. Surg Endosc. 1997;11:133–138. doi: 10.1007/s004649900315. [DOI] [PubMed] [Google Scholar]
- 23.McLean TR. Monetary lessons from litigation involving laparoscopic cholecystectomy. Am Surg. 2005;71:606–612. [PubMed] [Google Scholar]
- 24.Dunn D, Nair R, Fowler S, McCloy R. Laparoscopic cholecystectomy in England and Wales: results of an audit by the Royal College of Surgeons of England. Ann R Coll Surg Engl. 1994;76:269–275. [PMC free article] [PubMed] [Google Scholar]


