Abstract
Background:
Extrapancreatic organ dysfunction is the key determinant of mortality in acute pancreatitis (AP). This study aimed to document the frequency and duration of individual organ dysfunction in all fatalities caused by AP in a large, population-based cohort.
Methods:
All deaths caused by AP in Scotland between 2000 and 2006 inclusive were analysed (n = 1024).
Results:
The median time lapse between the onset of AP and death was 6 days (interquartile range [IQR] 17 days); that between the onset of organ dysfunction and death was 3 days (IQR 7 days). There was no apparent bimodal distribution. The majority of patients had single- (384 patients) or two-system (242 patients) extrapancreatic organ dysfunction. Pulmonary dysfunction was most prevalent (30% of organ-specific entries, 198/660), followed by cardiovascular (18%, 117/660), renal (16%, 108/660), liver (11%, 71/660), gastrointestinal (9%, 59/660), haemorrhage (6%, 38/660), coagulopathy (5%, 31/660) and central nervous system (6%, 38/660) dysfunction.
Conclusions:
Death in AP occurs early in the disease course. The present findings support the primacy of pulmonary injury as the modal pattern of organ dysfunction in severe AP, with increased frequencies of cardiovascular and renal compromise in fatal AP.
Keywords: acute pancreatitis, multi-organ failure, epidemiology
Introduction
Acute pancreatitis (AP) is inflammation of the pancreas usually caused by gallstones or excessive consumption of alcohol.1 The natural history of AP is that of a self-resolving clinical course in approximately 80% of episodes.2 Those patients who develop persistent extrapancreatic organ dysfunction (and who are therefore categorized as having severe AP) will usually require level 2 (high-dependency unit) or level 3 (intensive care unit) critical care support, with substantial costs to the health care service.3 The presence of persistent multiple organ failure is the key determinant of mortality in AP and analyses of prospectively collected data, such as those from the West of Scotland Pancreatic Unit, Glasgow,4 or the post hoc analysis of participants in the lexipafant trial reported by Johnson and Abu-Hilal (2004),5 emphasize the fundamental relationship between persistent organ failure and death. This notion is recapitulated in larger, retrospective analyses, including one from our own unit.6 The pathogenesis of systemic complications, specifically extrapancreatic acute organ dysfunction, is incompletely understood and further definition of the mechanisms of AP-associated organ failure is the focus of ongoing preclinical research. To facilitate service planning and to focus translational research studies, epidemiological data for individual organ dysfunction in severe AP are extremely helpful. In this study, we sought to document the frequency and duration of individual organ dysfunction in all fatalities caused by AP in a large national cohort.
Materials and methods
Confirmation that formal ethical approval was not required for this study was obtained following consultation with a local ethics committee representative and the General Register Office for Scotland. All deaths in Scotland between January 2000 and December 2005 inclusive (population: 5.06 million in 2001 and 5.12 million in 2006)7 for which AP (ICD-10 code K85) was registered as the primary or underlying cause of death were extracted from the General Register Office for Scotland. Detailed entries from the death register were computer-searched for the mention of any of the keywords listed below. The spreadsheet of positive hits was scrutinized and the diagnosis of AP and mention of specific organ failure verified manually. The Boolean operators used for the computer search are given in upper case.
Multiple-organ failure, using the terms: ‘multiple (OR multi-) organ failure’; ‘multi-system organ failure’; ‘multi-organ dysfunction (syndrome)’, and ‘systemic inflammatory response syndrome’.
Respiratory system failure or lung injury, using the terms: ‘respiratory failure’; ‘adult (OR acute) respiratory distress syndrome’; ‘(acute) pulmonary oedema’; ‘(broncho-) pneumonia’, and ‘pleural effusion’. Chronic obstructive pulmonary disease and exacerbations thereof were regarded as premorbid conditions and were not included as indicators of acute organ dysfunction.
Cardiovascular compromise, using the terms: ‘acute myocardial ischaemia (OR infarction)’; ‘acute cardiac event’; ‘acute coronary syndrome’; ‘cardiac (OR left ventricular) failure’; ‘cardiac tamponade’, and ‘cardiogenic shock’. ‘Cardiac (OR cardiorespiratory) arrest’ was regarded as the mode of death rather than the cause and not included as an individual organ dysfunction. Ischaemic heart disease, atherosclerosis and hypertension were regarded as comorbid conditions and not included as indicators of acute organ dysfunction.
Renal dysfunction, using the terms: ‘(acute) renal failure’, and ‘(acute) hepato-renal syndrome’. Chronic renal failure or impairment was regarded as a premorbid condition.
Haemorrhage, using the terms: ‘(acute) haemorrhage’; ‘exsanguination’; ‘(upper OR lower) gastrointestinal bleed (OR haemorrhage)’; ‘haematemesis’, and ‘(massive OR uncontrollable) intra-abdominal bleed (OR haemorrhage)’. The term ‘acute haemorrhagic pancreatitis’ without further qualification was not taken to indicate acute bleeding.
Coagulopathy, using the terms: ‘coagulopathy’; ‘disseminated intravascular coagulation’; ‘portal vein thrombosis’, and ‘deep vein thrombosis’.
Gut injury or dysfunction, using the terms: ‘perforated duodenal (OR gastric) ulcer (OR hollow viscus)’; ‘gastrointestinal bleed (OR haemorrhage)’; ‘bowel (OR mesenteric) ischaemia’; ‘colonic infarction’; ‘bowel obstruction (OR perforation)’, and ‘ileus’.
Liver and biliary dysfunction/injury, using the terms: ‘acute (OR ascending) cholangitis’; ‘(acute) liver (OR hepatic) failure’; ‘hepato-renal syndrome’; ‘jaundice’; ‘hepatitis’, and ‘hepatic necrosis’. Alcoholic liver disease was regarded as a comorbid condition.
Central nervous system involvement, using the terms: ‘cerebrovascular accident (OR event)’; ‘stroke’; ‘intracranial bleed (OR haemorrhage)’; ‘anoxic (OR hypoxic) brain injury’; ‘brainstem haemorrhage’, and ‘cerebral infarction (OR infarct)’.
Sepsis or infection, using the terms: ‘abscess’; ‘infected (OR infection)’; ‘sepsis (OR septic)’; ‘septicaemia’; ‘suppurative’, and ‘pus (OR purulent)’.
Assumed aetiology, using the terms: ‘gallstones’; ‘cholelithiasis’, and ‘biliary stones (OR calculi)’ for gallstones, and ‘alcohol’ OR ‘alcoholism’ and ‘endoscopic retrograde cholangiopancreatography’. Chronic pancreatitis was regarded as a premorbid condition and was not included in this analysis.
The statistics presented are largely descriptive. The variable ‘age’ did not follow a normal distribution by the Kolmogorov–Smirnov test and therefore the Mann–Whitney U-test was applied with an assumed significance level of ≤0.05 (spss Version 14.0; SPSS, Inc., Chicago, IL, USA).
Results
In this study, 1024 patients were identified and all records were analysed. The demographics of the cohort are presented in Table 1. Males died at a significantly younger age than females (males: median age at death 67 years, interquartile range [IQR] 23 years; females: median age at death 78 years, IQR 17 years; P < 0.001, Mann–Whitney U-test). The male : female ratio in the cohort by type of organ failure recapitulated that of the cohort as a whole (Table 1). There was no significant difference in number of deaths per year during the period studied (data not shown). The median time interval recorded between the onset of AP and death was 6 days (IQR 17 days); that between the onset of organ dysfunction and death was 3 days (IQR 7 days). Figure 1 depicts the distribution of duration between onset of AP and death and does not appear to show a bimodal distribution in this population-based cohort.
Table 1.
Patient demographics
| Male | Female | Total | Significance | |
|---|---|---|---|---|
| Total number (%) | 502 (49%) | 522 (51%) | 1024 (100%) | |
| Median age, years (IQR) | 67 (23) | 78 (17) | 73 (22) | P < 0.001a |
| Number with organ failure recorded (%) | 351 | 368 | 719 (70%) |
Mann–Whitney U-test
IQR, interquartile range
Figure 1.
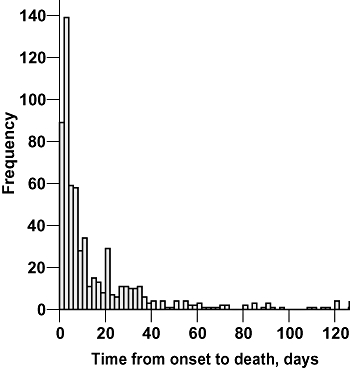
Histogram depicting time from onset of acute pancreatitis to death
Multiplicity of organ failure (number of organs failing in any one individual) is presented in Table 2. The majority of patients had single- (384 patients) or two-system (242 patients) extrapancreatic organ dysfunction. The relative frequencies of specific organ dysfunction are presented in Table 3. Pulmonary dysfunction was most prevalent (30% of patients, 198/660), followed by cardiovascular and renal dysfunction (18%, 117/660 and 16%, 108/660, respectively). Liver and gastrointestinal dysfunction affected 11% (71/660) and 9% (59/660) of patients, respectively, and the remainder of specific organ failures were recorded as haemorrhage, coagulopathy and central nervous system dysfunction (6% [38/660], 5% [31/660] and 6% [38/660], respectively). The aetiology of pancreatitis was not well recorded; reliable entries (as judged by the authors) were available only for 248 of 1024 patients. The relative proportions of gallstone, alcohol and post-endoscopic retrograde cholangiopancreatography aetiology in this group were 50% (124/248), 46% (115/248) and 4% (9/248), respectively. Idiopathic AP was incorporated in the group with unclear aetiology.
Table 2.
Multiplicity of organ failure
| Number of organs failing concurrently | Frequency in cohort | % |
|---|---|---|
| Multiple (number not specified) | 305 | 30 |
| 1 | 384 | 38 |
| 2 | 242 | 24 |
| 3 | 89 | 9 |
| 4 | 3 | <1 |
| 5 | 1 | <1 |
| Total | 1024 |
Table 3.
Specific organ dysfunction
| Number of episodes | % | |
|---|---|---|
| Pulmonary | 198 | 30 |
| Cardiovascular | 117 | 18 |
| Renal | 108 | 16 |
| Liver | 71 | 11 |
| Gut | 59 | 9 |
| Haemorrhage | 38 | 6 |
| Coagulation | 31 | 5 |
| Central nervous system | 38 | 6 |
| Total | 660 | 100 |
Discussion
In this study, we report the incidence of individual organ dysfunction in a large retrospective cohort of all AP fatalities in Scotland registered between 2000 and 2005. The main findings show that 63% of fatalities had dysfunction of at least two organ systems, and that the pulmonary system was most frequently injured, followed by the cardiovascular and renal systems, usually in a cumulative fashion.
Strengths of this study include the fact that we examined all deaths from AP in Scotland over a 6-year period, minimizing any selection and reporting bias that might arise in single-centre reports or in data from prospective trials of potential therapies. Further strengths lie in the large size of the cohort and the fact that it included the entire population of a clearly defined geographical area. The process of data management after initial completion of the death certificate is internally validated at the General Register Office for Scotland and subject to regular quality control.
There are some potential limitations to the approach used in this study. First and foremost, this study relies entirely on the accuracy and completeness of the registration of underlying causes of death on the death certificate, which, although it has been shown to be accurate in the majority of cases, is a potential source of error.8 Indices of agreement between causes of death stated on death certificates vary widely and have been reported to depend on several factors, including: the nature of disease (e.g. the agreement index for neoplastic diseases has been reported to be 83%, compared with 31% for chest diseases);9 the duration of hospitalization before death (longer periods correlate with higher agreement indices), and the involvement of alcohol.10 Acute pancreatitis is an acute disease, usually with a short duration of hospital admission before death, is non-neoplastic and often involves alcohol, and therefore may exhibit a low death certificate agreement index. Despite these limitations, analyses of death certificates have been shown to serve the reporting of mortality statistics and demographics appropriately, as emphasized by Lahti and Penttila (2001),11 and are extremely useful in population-based studies as they minimize selection and reporting bias.
The present findings concur with those of previous studies. Individual organ failure (classified using the Marshall score12) in 290 patients recruited to the lexipafant study with a predicted severe attack, using an APACHE II score >6 at presentation, was broken down by Johnson and Abu-Hilal (2004) into transient organ failure (resolving in <48 hours) and persistent organ failure (duration >48 hours).5 Organs involved in patients with transient organ failure (71 patients) were: pulmonary in 86%; renal in 4%; coagulopathy-related in 4%, pulmonary and renal in 4%, and pulmonary and coagulopathy-related in 1%. In the 40 patients who died, organs involved in week 1 were: pulmonary in 25%; renal in 5%; pulmonary and renal in 30%, and three or more systems-related in 33%.5 Similarly, in an analysis of 121 patients with organ failure studied as part of a randomized, controlled trial conducted in the West of Scotland Pancreatic Unit between 1997 and 1999, the following incidences of individual organ dysfunction were noted: pulmonary in 37%; renal in 9%; coagulation-related in 11%; brain in 2%, and cardiovascular in 5%. In that series, the mortality rate in patients with single organ dysfunction was 2.5%, compared with 69% in patients with dysfunction of two or more organs.4,13 It is possible that the increased incidence of renal and cardiorespiratory failure in the present study compared with the aforementioned studies reflects the uniformly fatal nature of the episodes in our series.
With respect to pulmonary failure, the agreement between the data presented in this study and data from other groups reinforces the prime importance of lung injury in severe AP. Pulmonary infiltrates are seen on chest radiographs in 6–26% of all patients with AP14 and an abnormal chest radiograph has been associated with a relative risk of death 15 times that of patients with a normal chest radiograph.15 The reasons why the lung is the most commonly injured organ system in severe AP are not completely understood, but preventing acute lung injury is arguably the most logical target of potential therapy. Several hypotheses regarding the inception of respiratory dysfunction in AP exist, including compromised ventilation,14 impaired alveolar gas exchange16 and increased permeability to plasma proteins.14 Furthermore, AP results in an increased susceptibility to infection,17 and established AP-related organ failure is associated with a diminished pro-inflammatory cytokine response to lipopolysaccharide.18 Current studies are exploring the hypothesis that mesenteric lymph-carrying cytotoxic kynurenine catabolites of tryptophan to the pulmonary capillary bed form an integral component of the complex pathogenesis of pancreatitis-associated organ failure.19
An interesting observation of this population-based study concerned the absence of a bimodal temporal distribution of deaths. It is possible that the bimodal distribution observed in previous studies13 may be a function of the receipt of a tertiary referral cohort from the general hospital population, and thus subject to referral bias. Tertiary referral centres usually also have their own emergency intake, which generates a proportion of early deaths, but also receive a disproportionately greater number of tertiary referrals with infected (or non-infected) necrosis, who die after longer time intervals, giving the impression of two peaks. The absence of a clear bimodal distribution in the present study appears to indicate that using population data (rather than institutional data) might encourage greater emphasis on supporting and preventing organ dysfunction during the critical illness phase and less emphasis on the use of prophylactic therapies for late sepsis.
In conclusion, this population-based study of 1024 deaths from AP occurring over a 6-year period provides epidemiological data regarding patterns of individual organ dysfunction in fatal AP. Death in AP occurs early in the disease course. The findings support the primacy of pulmonary injury as the modal pattern of organ dysfunction in severe AP, with an increased frequency of cardiovascular and renal compromise in fatal episodes.
Acknowledgments
We are extremely grateful to the staff of the General Register Office for Scotland for their kind assistance with the provision of death statistics.
Conflicts of interest
None declared.
References
- 1.Forsmark CE, Baillie J. AGA Institute technical review on acute pancreatitis. Gastroenterology. 2007;132:2022–2044. doi: 10.1053/j.gastro.2007.03.065. [DOI] [PubMed] [Google Scholar]
- 2.Mitchell RM, Byrne MF, Baillie J. Pancreatitis. Lancet. 2003;361:1447–1455. doi: 10.1016/s0140-6736(03)13139-x. [DOI] [PubMed] [Google Scholar]
- 3.Neoptolemos JP, Raraty M, Finch M, Sutton R. Acute pancreatitis: the substantial human and financial costs. Gut. 1998;42:886–891. doi: 10.1136/gut.42.6.886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buter A, Imrie CW, Carter CR, Evans S, McKay CJ. Dynamic nature of early organ dysfunction determines outcome in acute pancreatitis. Br J Surg. 2002;89:298–302. doi: 10.1046/j.0007-1323.2001.02025.x. [DOI] [PubMed] [Google Scholar]
- 5.Johnson CD, Abu-Hilal M. Persistent organ failure during the first week as a marker of fatal outcome in acute pancreatitis. Gut. 2004;53:1340–1344. doi: 10.1136/gut.2004.039883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mofidi R, Duff MD, Wigmore SJ, Madhavan KK, Garden OJ, Parks RW. Association between early systemic inflammatory response, severity of multiorgan dysfunction and death in acute pancreatitis. Br J Surg. 2006;93:738–744. doi: 10.1002/bjs.5290. [DOI] [PubMed] [Google Scholar]
- 7.General Register Office for Scotland. Mid-2006 Population Estimates Scotland. Population estimates by sex, age and administrative area. [Accessed 15 January 2007]. http://www.gro-scotlandgovuk/files1/stats/mid-2006-population-estimates-scotland/j8527pdf.
- 8.Jorgensen IM, Bulow S, Jensen VB, Dahm TL, Prahl P, Juel K. Asthma mortality in Danish children and young adults, 1973–1994: epidemiology and validity of death certificates. Eur Respir J. 2000;15:844–848. doi: 10.1034/j.1399-3003.2000.15e06.x. [DOI] [PubMed] [Google Scholar]
- 9.Jedrychowski W, Mroz E, Wiernikowski A, Flak E. Validity study on the certification and coding of underlying causes of death for the mortality statistic. Przegl Epidemiol. 2001;55:313–322. [PubMed] [Google Scholar]
- 10.Daula M, Hanzlick R. Evaluation of certifier practices regarding alcohol-related deaths: Fulton County Medical Examiner's Center, Atlanta, Georgia, 2004. Am J Forensic Med Pathol. 2006;27:355–358. doi: 10.1097/01.paf.0000233554.79665.0c. [DOI] [PubMed] [Google Scholar]
- 11.Lahti RA, Penttila A. The validity of death certificates: routine validation of death certification and its effects on mortality statistics. Forensic Sci Int. 2001;115:15–32. doi: 10.1016/s0379-0738(00)00300-5. [DOI] [PubMed] [Google Scholar]
- 12.Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ. Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med. 1995;23:1638–1652. doi: 10.1097/00003246-199510000-00007. [DOI] [PubMed] [Google Scholar]
- 13.McKay CJ, Buter A. Natural history of organ failure in acute pancreatitis. Pancreatology. 2003;3:111–114. doi: 10.1159/000070078. [DOI] [PubMed] [Google Scholar]
- 14.Pastor CM, Matthay MA, Frossard JL. Pancreatitis-associated acute lung injury: new insights. Chest. 2003;124:2341–2351. doi: 10.1378/chest.124.6.2341. [DOI] [PubMed] [Google Scholar]
- 15.Talamini G, Uomo G, Pezzilli R, Rabitti PG, Billi P, Bassi C, et al. Serum creatinine and chest radiographs in the early assessment of acute pancreatitis. Am J Surg. 1999;177:7–14. doi: 10.1016/s0002-9610(98)00296-7. [DOI] [PubMed] [Google Scholar]
- 16.De Troyer A, Naeije R, Yernault JC, Englert M. Impairment of pulmonary function in acute pancreatitis. Chest. 1978;73:360–363. doi: 10.1378/chest.73.3.360. [DOI] [PubMed] [Google Scholar]
- 17.Westerloo DJ, Schultz MJ, Bruno MJ, de Vos AF, Florquin S, van der Poll T. Acute pancreatitis in mice impairs bacterial clearance from the lungs, whereas concurrent pneumonia prolongs the course of pancreatitis. Crit Care Med. 2004;32:1997–2001. doi: 10.1097/01.ccm.0000142658.22254.74. [DOI] [PubMed] [Google Scholar]
- 18.Mole DJ, McFerran NV, Diamond T. Differential preservation of lipopolysaccharide-induced chemokine/cytokine expression during experimental pancreatitis-associated organ failure in rats shows a regulatory expressed phenotype. Pancreatology. 2008;8:478–487. doi: 10.1159/000151775. [DOI] [PubMed] [Google Scholar]
- 19.Mole DJ, McFerran NV, Collett G, O’Neill C, Diamond T, Garden OJ, et al. Tryptophan catabolites in mesenteric lymph may contribute to pancreatitis-associated organ failure. Br J Surg. 2008;95:855–867. doi: 10.1002/bjs.6112. [DOI] [PubMed] [Google Scholar]


