Abstract
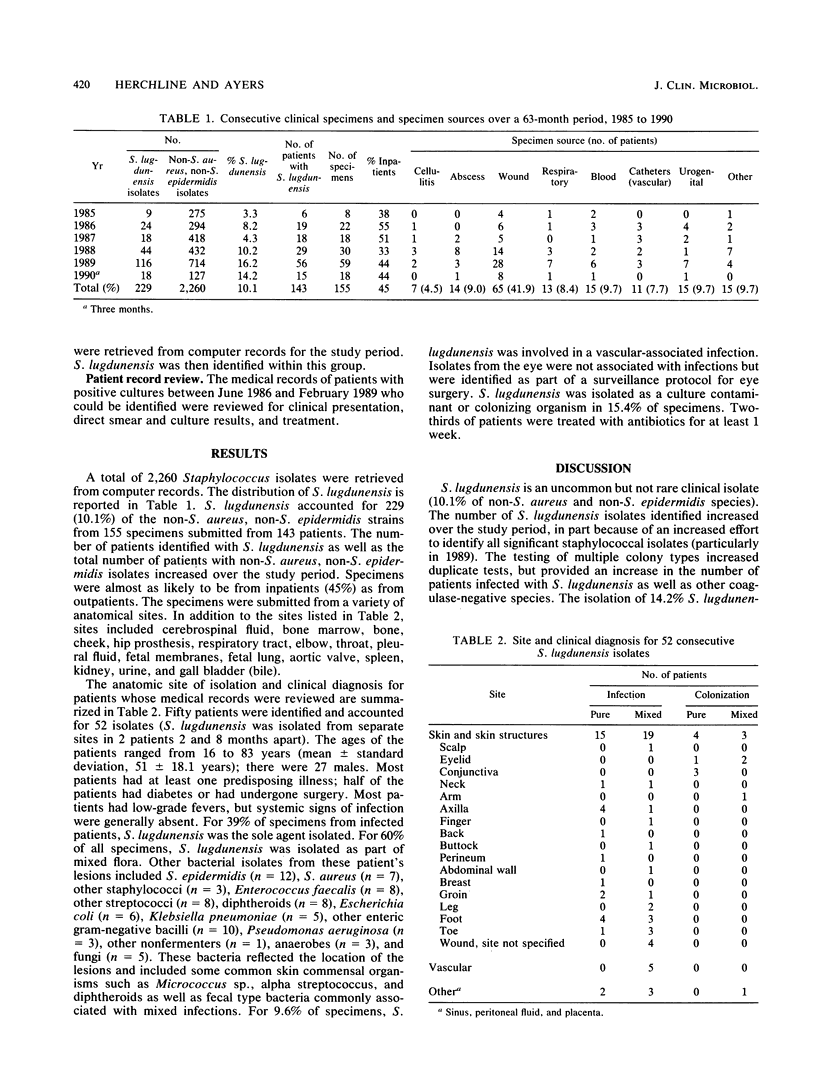
Consecutive record review over a 63-month period revealed 229 Staphylococcus lugdunensis isolates, or 10.1% of the staphylococcal species that were not Staphylococcus aureus or Staphylococcus epidermidis. A total of 155 S. lugdunensis specimens were isolated from sites over the entire bodies of the 143 patients studied. The most common clinical diagnoses were skin and skin structure infections (55.4%) and blood and vascular catheter infections (17.4%). For 40% of the reviewed specimens, S. lugdunensis was the sole agent isolated, and for 60% of specimens, S. lugdunensis was isolated as part of mixed flora. In only 15.4% of clinically reviewed specimens was S. lugdunensis clearly a culture contaminant or colonizing organism. The pattern of human infection identified in this study emphasizes the predominance of skin and soft tissue S. lugdunensis infections over deep serious infections such as endocarditis, peritonitis, infected hip prosthesis, and osteomyelitis and vascular-associated infections. S. lugdunensis should be included along with S. epidermidis, Staphylococcus haemolyticus, and Staphylococcus saprophyticus as a coagulase-negative species of Staphylococcus pathogenic for humans.
Full text
PDF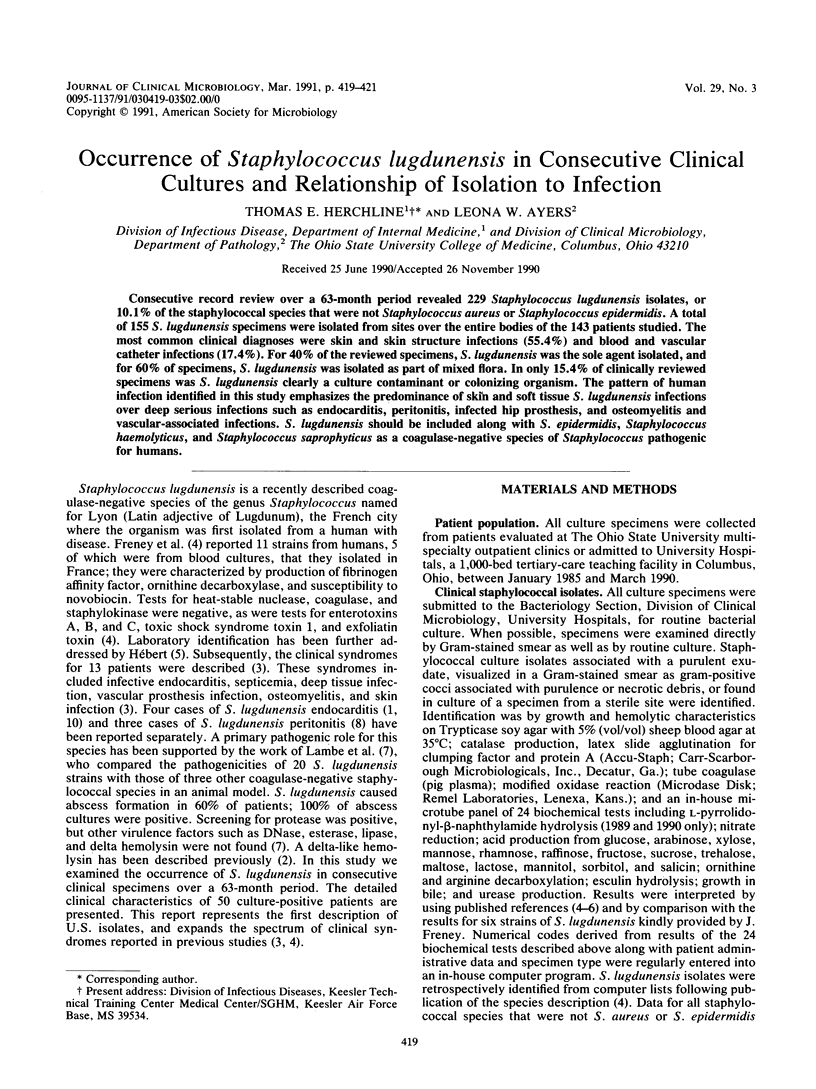

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Etienne J., Pangon B., Leport C., Wolff M., Clair B., Perronne C., Brun Y., Buré A. Staphylococcus lugdunensis endocarditis. Lancet. 1989 Feb 18;1(8634):390–390. doi: 10.1016/s0140-6736(89)91770-4. [DOI] [PubMed] [Google Scholar]
- Fleurette J., Bès M., Brun Y., Freney J., Forey F., Coulet M., Reverdy M. E., Etienne J. Clinical isolates of Staphylococcus lugdunensis and S. schleiferi: bacteriological characteristics and susceptibility to antimicrobial agents. Res Microbiol. 1989 Feb;140(2):107–118. doi: 10.1016/0923-2508(89)90044-2. [DOI] [PubMed] [Google Scholar]
- Hébert G. A. Hemolysins and other characteristics that help differentiate and biotype Staphylococcus lugdunensis and Staphylococcus schleiferi. J Clin Microbiol. 1990 Nov;28(11):2425–2431. doi: 10.1128/jcm.28.11.2425-2431.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfaller M. A., Herwaldt L. A. Laboratory, clinical, and epidemiological aspects of coagulase-negative staphylococci. Clin Microbiol Rev. 1988 Jul;1(3):281–299. doi: 10.1128/cmr.1.3.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh B., Mounsey J. P. Staphylococcus lugdenensis and endocarditis. J Clin Pathol. 1990 Feb;43(2):171–171. doi: 10.1136/jcp.43.2.171-a. [DOI] [PMC free article] [PubMed] [Google Scholar]


