Abstract
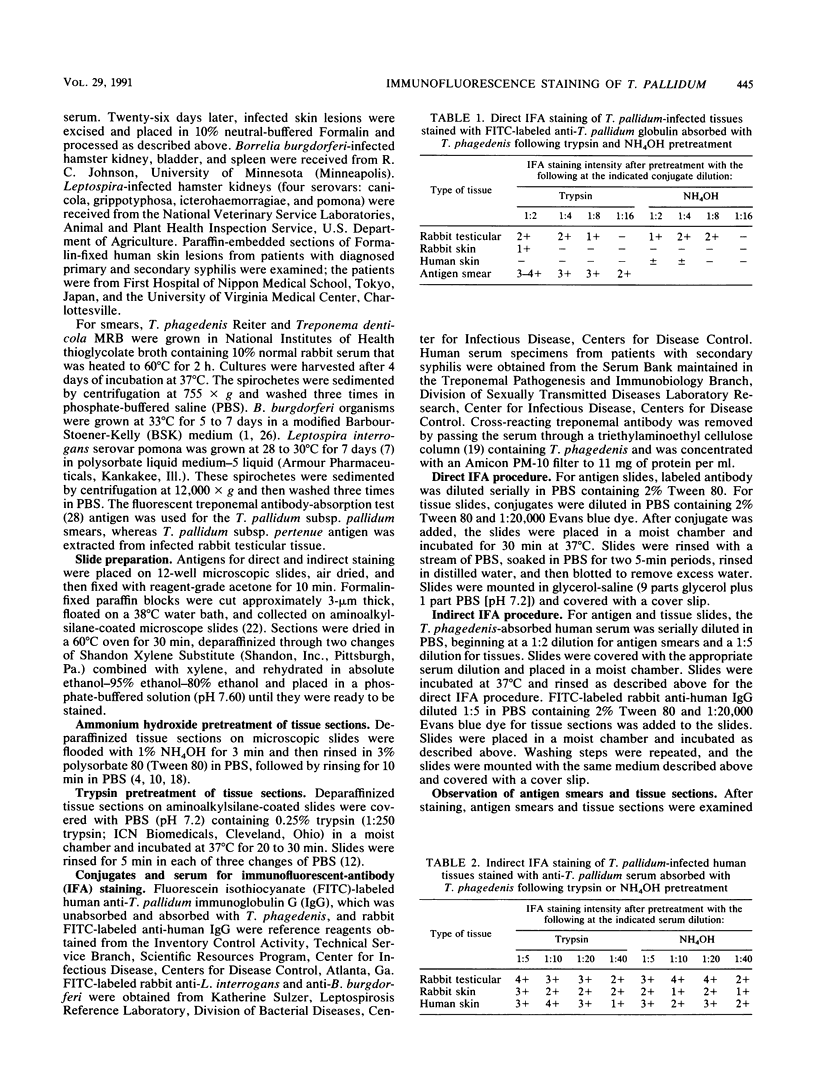
To date, tissue sections prepared from Formalin-fixed tissues have not been successfully stained with Treponema pallidum subspecies-specific antibody in a direct fluorescent-antibody assay. While current methods stain T. pallidum, they do not distinguish T. pallidum from other spirochetes such as Borrelia burgdorferi (E. F. Hunter, P. W. Greer, B. L. Swisher, A. R. Simons, C. E. Farshy, J. A. Crawford, and K. R. Sulzer, Arch. Pathol. Lab. Med. 108:878-880, 1984). Because trypsin pretreatment of tissue sections has enhanced other immunofluorescent-antibody (IFA) applications, we compared the use of the trypsin digestion method with the current 1% ammonium hydroxide (NH4OH) method as a means to obtain specific staining of T. pallidum in tissues by both direct and indirect IFA techniques. Pretreated T. pallidum-infected tissues sections from rabbits, hamsters, and humans were quantitatively examined with the direct fluorescent-antibody-T. pallidum test conjugate absorbed with Treponema phagedenis, the Reiter treponeme. For indirect staining, a serum specimen from a patients with syphilis absorbed by affinity chromatography with T. phagedenis was used as the primary reagent, and a fluorescein isothiocyanate-labeled rabbit anti-human globulin was used as the secondary reagent. Serum specificity was established first by examining antigen smears of T. pallidum subsp. pallidum, T. pallidum subsp. pertenue, B. burgdorferi, T. phagedenis, and Treponema denticola MRB and then by examining tissues infected with these pathogens plus those infected with four Leptospira serovars. When we stained tissue using the direct IFA method that is currently a standard method for the examination of chancre smears, we found it to be unsuitable for use with tissue. Trypsin digestion did not offer an improvement over the NH4OH pretreatment method in the specific identification of T. pallidum by direct IFA. However, specific identification of T. pallidum in tissue sections was obtained by the indirect IFA technique after either trypsin or NH4OH pretreatment.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- COFFIN D. L. Detection of leptospires by fluorescent antibody. Am J Vet Res. 1962 Jan;23:159–164. [PubMed] [Google Scholar]
- Chandler F. W., Gorelkin L. Immunofluorescence staining of adenovirus in fixed tissues pretreated with trypsin. J Clin Microbiol. 1983 Feb;17(2):371–373. doi: 10.1128/jcm.17.2.371-373.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson S., Evans B. A., Lawrence A. G. Benign tertiary syphilis and HIV infection. AIDS. 1988 Aug;2(4):315–316. doi: 10.1097/00002030-198808000-00012. [DOI] [PubMed] [Google Scholar]
- Hicks C. B., Benson P. M., Lupton G. P., Tramont E. C. Seronegative secondary syphilis in a patient infected with the human immunodeficiency virus (HIV) with Kaposi sarcoma. A diagnostic dilemma. Ann Intern Med. 1987 Oct;107(4):492–495. doi: 10.7326/0003-4819-107-4-492. [DOI] [PubMed] [Google Scholar]
- Huang S. N., Minassian H., More J. D. Application of immunofluorescent staining on paraffin sections improved by trypsin digestion. Lab Invest. 1976 Oct;35(4):383–390. [PubMed] [Google Scholar]
- Hunter E. F., Greer P. W., Swisher B. L., Simons A. R., Farshy C. E., Crawford J. A., Sulzer K. R. Immunofluorescent staining of Treponema in tissues fixed with formalin. Arch Pathol Lab Med. 1984 Nov;108(11):878–880. [PubMed] [Google Scholar]
- Hunter E. F., Russell H., Farshy C. E., Sampson J. S., Larsen S. A. Evaluation of sera from patients with Lyme disease in the fluorescent treponemal antibody-absorption test for syphilis. Sex Transm Dis. 1986 Oct-Dec;13(4):232–236. doi: 10.1097/00007435-198610000-00005. [DOI] [PubMed] [Google Scholar]
- Ito F. [A study on the demonstration of Treponema pallidum in the tissue of syphilids]. Nihon Ika Daigaku Zasshi. 1987 Feb;54(1):54–62. doi: 10.1272/jnms1923.54.54. [DOI] [PubMed] [Google Scholar]
- Jeerapaet P., Ackerman A. B. Histologic patterns of secondary syphilis. Arch Dermatol. 1973 Mar;107(3):373–377. [PubMed] [Google Scholar]
- Lanska M. J., Lanska D. J., Schmidley J. W. Syphilitic polyradiculopathy in an HIV-positive man. Neurology. 1988 Aug;38(8):1297–1301. doi: 10.1212/wnl.38.8.1297. [DOI] [PubMed] [Google Scholar]
- Maestrone G. The Use of an Improved Fluorescent Antibody Procedure in the Demonstration of Leptospira in Animal Tissues. Can J Comp Med Vet Sci. 1963 May;27(5):108–112. [PMC free article] [PubMed] [Google Scholar]
- McKinney R. M., Thacker L., Wong M. C., Hebert G. A. Improved immunoadsorption procedure with anion-exchange bacterial cell columns. J Immunol Methods. 1978;21(1-2):1–10. doi: 10.1016/0022-1759(78)90218-1. [DOI] [PubMed] [Google Scholar]
- Nakamura S., Ito F., Nakamura S., Onda S. Improved methods for the demonstration of Treponema pallidum in the tissues. J Dermatol. 1983 Oct;10(5):433–437. doi: 10.1111/j.1346-8138.1983.tb01162.x. [DOI] [PubMed] [Google Scholar]
- Radolf J. D., Kaplan R. P. Unusual manifestations of secondary syphilis and abnormal humoral immune response to Treponema pallidum antigens in a homosexual man with asymptomatic human immunodeficiency virus infection. J Am Acad Dermatol. 1988 Feb;18(2 Pt 2):423–428. doi: 10.1016/s0190-9622(88)70062-6. [DOI] [PubMed] [Google Scholar]
- Russell H., Sampson J. S., Schmid G. P., Wilkinson H. W., Plikaytis B. Enzyme-linked immunosorbent assay and indirect immunofluorescence assay for Lyme disease. J Infect Dis. 1984 Mar;149(3):465–470. doi: 10.1093/infdis/149.3.465. [DOI] [PubMed] [Google Scholar]
- Silber T. J., Kastrinakis M., Taube O. Painful red leg nodules and syphilis: a consideration in patients with erythema nodosum-like illness. Sex Transm Dis. 1987 Jan-Mar;14(1):52–53. doi: 10.1097/00007435-198701000-00012. [DOI] [PubMed] [Google Scholar]
- Silber T. J., Niland N. F. The clinical spectrum of syphilis in adolescence. J Adolesc Health Care. 1984 Apr;5(2):112–116. doi: 10.1016/s0197-0070(84)80009-1. [DOI] [PubMed] [Google Scholar]
- Stoenner H. G., Dodd T., Larsen C. Antigenic variation of Borrelia hermsii. J Exp Med. 1982 Nov 1;156(5):1297–1311. doi: 10.1084/jem.156.5.1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Koning J., Hoogkamp-Korstanje J. A. Diagnosis of Lyme disease by demonstration of spirochetes in tissue biopsies. Zentralbl Bakteriol Mikrobiol Hyg A. 1986 Dec;263(1-2):179–188. doi: 10.1016/s0176-6724(86)80121-3. [DOI] [PubMed] [Google Scholar]



