Abstract
We report here on a case of extrahepatic biliary cystadenoma arising from the common hepatic duct. A 42-year-old woman was evaluated by us to find the cause of her jaundice. Ultrasonography and CT showed a cystic dilatation of the common hepatic duct and also marked dilatation of the intrahepatic duct. Direct cholangiography demonstrated a large filling defect between the left hepatic duct and the common hepatic duct; dilatation of the intrahepatic duct was also demonstrated. Following excision of the cystic mass, it was pathologically confirmed as a unilocular biliary mucinous cystadenoma arising from the common hepatic duct.
Keywords: Bile ducts, extrahepatic; Cyst, choledochal cyst; Cyst, unilocular
Biliary cystadenomas are rare cystic neoplasms of the liver (1). There are relatively few reports of extrahepatic biliary cystadenomas; less than 10% of the reported cases of biliary cystadenoma were extrahepatic in origin (2). Most of the extrahepatic biliary cystadenomas have presented as a well-encapsulated, multiseptated cystic masses on CT and ultrasonography (2). We report here on a case of unilocular biliary cystadenoma arising from the common hepatic duct, and this tumor was initially mistaken as a choledochal cyst on CT and ultrasonography.
CASE REPORT
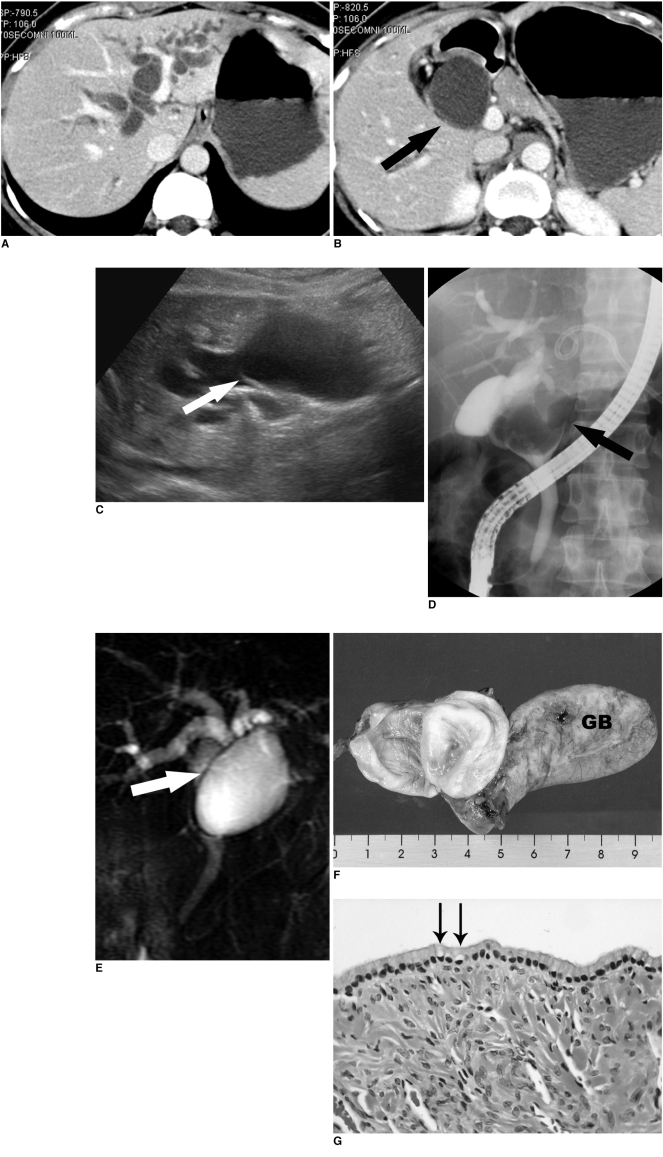
A 42-year-old woman had presented to the local clinic with jaundice of two months duration and she was suspected of having periampullary cancer; she was then referred to us and admitted to our hospital for further evaluation. The physical examination revealed no abnormality. The serum total bilirubin level was 3.1 mg/dl and the aspartate aminotransferase/alanine aminotransferase levels were 80/180 U/L. Abdominal CT showed a cystic dilatation of the common hepatic duct and a marked dilatation of the intrahepatic bile duct (Figs. 1A, B). Abdominal ultrasonography also revealed these lesions, but there was a partial thin septum-like structure within the upper aspect of the cystic dilated common hepatic duct (Fig. 1C). However, neither definite septation nor an enhancing portion within the dilated duct was noted, and so this was considered to be a choledochal cyst. Percutaneous transhepatic biliary drainage (PTBD) was done through the left hepatic duct, and the subsequent tubogram showed obstruction of the left hepatic duct by a large filling defect. On endoscopic retrograde cholangiopancreatography (ERCP), a well-demarcated filling defect was seen in the common hepatic duct and this did not communicate with the bile duct. The distal portion of the common hepatic duct showed a beaking appearance near this mass and the left hepatic duct was not opacified (Fig. 1D). Any anomalous pancreaticobiliary ductal union was not found. Before surgery, magnetic resonance cholangiopancreatography (MRCP) was performed, and it showed a well-defined cystic mass extending from the left hepatic duct to the common hepatic duct with a definite thin wall displaying a dark signal intensity. Magnetic resonance cholangiopancreatography also showed a bile duct variation; the right posterior segmental duct drained into the left hepatic duct (Fig. 1E). The patient underwent resection of the extrahepatic biliary tract including the cystic mass, and hepaticojejunostomy was next performed. During surgery, the cystic mass was noted to arise from the common hepatic duct, yet it had no communication with this duct. Pathologically, this unilocular cystic mass arose from the serosal surface of the common hepatic duct, which was bulging into the common hepatic duct (Fig. 1F). It was lined by a single layer of tall columnar mucin-secreting cells with focal evidence of mucinous secretion (Fig. 1G). Our case was diagnosed as a biliary mucinous cystadenoma in the common hepatic duct. The patient has been alive with no tumor recurrence for one year after surgery.
Fig. 1.
Unilocular extrahepatic biliary cystadenoma in a 42-year-old woman.
A, B. Abdominal CT scans show marked dilatation of the intrahepatic duct and the cystic dilatation of the common bile duct (arrow).
C. Ultrasonography also shows cystic dilatation of the extrahepatic duct. On retrospective review, the thin partial septum like structure (arrow) is seen at the upper aspect of the cystic dilatation of the extrahepatic duct.
D. Endoscopic retrograde cholangiopancreatography shows a well-demarcated large filling defect (arrow) in the common hepatic duct with dilatation of the intrahepatic duct. It does not communicate with the bile duct. The PTBD tube, which is not filled with contrast material, is also seen in the left hepatic duct.
E. Magnetic resonance cholangiopancreatography clearly shows the thin wall (arrow) of the cystic lesion in the common hepatic duct. It also shows a bile duct variation; the right posterior segmental duct drained into the left hepatic duct.
F. The surgical specimen shows a unilocular cystic mass arising from the common hepatic duct (incised). GB; gallbladder
G. Microscopically (H & E staining, ×200), the cyst wall is lined by a single layer of columnar mucin-secreting cells (arrows). The epithelium is supported by ovarian-like stroma.
DISCUSSION
Biliary cystadenoma is a rare benign cystic neoplasm that usually occurrs in middle-aged women (1, 3, 4). The majority of biliary cystadenomas are entirely intrahepatic, and the rest of them arise from extrahepatic ducts and the gall bladder (1, 5). More than 90% of extrahepatic biliary cystadenomas occur in women (2). Most of the patients with intrahepatic cystadenomas present with abdominal swelling or with an abdominal mass (1). However, the most common presenting symptom of extrahepatic biliary cystadenoma has usually been jaundice, and our case also presented with jaundice (2).
Extrahepatic biliary cystadenomas are cystic neoplasms lined by mucin-secreting columnar epithelium (5). It was previously proposed that cystadenomas were congenital and they were thought to develop from either an aberrant hamartomatous bile duct or from an ectopic remnant of embryonal gallbladder (1, 5). Recently, peribilliary glands distributed around the large bile ducts have also been suggested to be the origin (6). Davies et al. (2) reviewed the 19 cases of extrahepatic benign biliary cystadenoma that were reported on between 1943 and 1993. They noted that extrahepatic biliary cystadenomas were uniformly distributed throughout the extrahepatic bile duct. In their study, the location was the right hepatic duct in 14.3% of the cases, the left hepatic duct in 28.6%, the common hepatic duct in 32.1%, the common bile duct in 21.4%, and a cystic duct in 3.6%. Complete surgical resection is required for both intrahepatic and extrahepatic cystadenomas because cystadenocarcinomas are believed to arise from benign cystadenomas (1, 5, 7).
The diagnostic imaging characteristics of biliary cystadenomas and cystadenocarcinomas have been well described (3, 4, 8). A multiloculated cystic mass with internal septa and mural nodules is the characteristic finding, and this potentially differentiates these tumors from complicated hepatic cysts, liver abscess and hydatid disease of the liver (3, 4, 8). There seems to be no significant difference for the imaging findings between intrahepatic and extrahepatic biliary cystadenomas (1-3). Unilocular biliary cystadenomas may present on rare occasions: however they have been noted to be intrahepatic biliary cystadenomas (3).
On CT and ultrasonography, it is hard to differentiate unilocular extrahepatic biliary cystadenoma from a choledochal cyst. In our case, these imaging modalities showed the intrahepatic bile duct and the common hepatic duct as having marked dilatation, but the common bile duct had a normal appearance. We could find nothing of the wall of the cystic mass, the septation or the mural nodules within the mass. On retrospective review, we had two clues that might have been helpful for diagnosis. One clue was on ultrasonography and CT: the bile duct dilatation was proportional. Choledochal cyst may show dilatation of the intrahepatic duct, however, it shows multiple focal segmental dilatations, smooth fusiform dilatation, or irregular nonuniform ductal dilatation (9). Proportional dilatation of the intrahepatic duct suggests the possibility of an obstructing lesion in the extrahepatic duct, and this is not a usual finding for choledochal cyst. The other clue was the thin wall of the unilocular cyst that was visualized on ultrasonography, although it was seen only as a partial septum-like structure at the upper aspect of the cystic dilated duct (Fig. 1C). On retrospective review of the patient's CT scan, we could not find the cyst wall itself, but the ultrasonography showed a thin cyst wall, which was not detected by us during the examination. From the gross specimen, the cystic mass with the thin wall arose from the common hepatic duct.
In summary, we present here a case of rare cystic neoplasm of the extrahepatic bile duct. Although most of the extrahepatic biliary cystadenomas manifest as a multilocular cystic mass, the tumor in our case presented as a unilocular cystic lesion that mimicked a choledochal cyst.
References
- 1.Ishak KG, Willis GW, Cummins SD, Bullock AA. Biliary cystadenoma and cystadenocarcinoma: report of 14 cases and review of the literature. Cancer. 1977;38:322–338. doi: 10.1002/1097-0142(197701)39:1<322::aid-cncr2820390149>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 2.Davies W, Chow M, Nagorney D. Extrahepatic biliary cystadenomas and cystadenocarcinoma. Report of seven cases and review of the literature. Ann Surg. 1995;222:619–625. doi: 10.1097/00000658-199511000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Choi BI, Lim JH, Han MC, et al. Biliary cystadenoma and cystadenocarcinoma: CT and sonographic findings. Radiology. 1989;171:57–61. doi: 10.1148/radiology.171.1.2648477. [DOI] [PubMed] [Google Scholar]
- 4.Buetow PC, Buck JL, Pantongrag-Brown L, et al. Biliary cystadenoma and cystadenocarcinoma: clinical-imaging-pathologic correlation with emphasis on the importance of ovarian stroma. Radiology. 1995;196:805–810. doi: 10.1148/radiology.196.3.7644647. [DOI] [PubMed] [Google Scholar]
- 5.Wheeler DA, Edmondson HA. Cystadenoma with mesenchymal stroma (CMS) in the liver and bile ducts. A clinicopathologic study of 17 cases, 4 with malignant change. Cancer. 1985;56:1434–1445. doi: 10.1002/1097-0142(19850915)56:6<1434::aid-cncr2820560635>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 6.Terada T, Kitamura Y, Ohta T, Nakanuma Y. Endocrine cells in hepatobiliary cystadenomas and cystadenocarcinomas. Virchows Arch. 1997;430:37–40. doi: 10.1007/BF01008014. [DOI] [PubMed] [Google Scholar]
- 7.Sato M, Watanabe Y, Tokui K, et al. Hepatobiliary cystadenocarcinoma connected to the hepatic duct: a case report and review of the literature. Hepatogastroenterology. 2003;50:1621–1624. [PubMed] [Google Scholar]
- 8.Korobkin M, Stephens DH, Lee JK, et al. Biliary cystadenoma and cystadenocarcinoma: CT and sonographic findings. AJR Am J Roentgenol. 1989;153:507–511. doi: 10.2214/ajr.153.3.507. [DOI] [PubMed] [Google Scholar]
- 9.Savader SJ, Benenati JF, Venire AC, et al. Choledochal cysts: classification and cholangiographic appearance. AJR Am J Roentgenol. 1991;156:327–331. doi: 10.2214/ajr.156.2.1898807. [DOI] [PubMed] [Google Scholar]