Abstract
Background/Aims
Although the incidence of T-cell non-Hodgkin's lymphoma (NHL) is higher in Far East Asia than in Western countries, its incidence and clinical course in Korea are not well-defined. Therefore, we assessed the relative frequency and clinical features of T-cell NHL in Korea.
Methods
We performed a retrospetcive analysis of 586 patients with NHL.
Results
101 (17.2%) had T-cell NHL. The most frequent subtypes of T-cell NHL were extranodal NK/T-cell lymphoma, nasal type (NASAL), peripheral T-cell lymphoma, unspecified type (PTCL-U), and anaplastic large cell lymphoma, T/null cell, primary systemic type (ALCL). The seven pathological subtypes could be classified into three prognostic subgroups. When patients with the three most frequent subtypes were grouped together, their survival was reflected in the International Prognostic Index (IPI) scores. Univariate analysis of IPI elements and other clinical features showed that clinical stage and extranodal sites were significant predictors of survival. Cox multivariate analysis showed that the number of extranodal sites was the only independent prognostic indicator.
Conclusions
The relative frequency of T-cell NHL seems to be decreasing in Korea, although NASAL remains frequent. Korean patients with ALCL appear to have an unfavorable prognosis. Large-scale studies are warranted for Korean patients with T-cell NHL.
Keywords: Lymphoma, T-cell, Peripheral
INTRODUCTION
Non-Hodgkin's lymphoma (NHL) is a malignancy that arises from lymphoid tissue. In the United States, NHL is the fifth most commonly diagnosed cancer, accounting for 4% of all cancers, with an estimated 66,120 new cases and 19,160 deaths in 2008. Although the incidence of NHL has stabilized, it is still increasing by 1-2% annually [1]. NHL is more frequent in the elderly than in younger patients and more frequent in men than in women [2].
The incidence of NHL and the patterns of occurrence of its various subtypes vary geographically. According to the World Health Organization International Agency for Research on Cancer (IARC), the rate of NHL is increasing worldwide and is higher in developed countries than in Africa and Asia [3]. The relative frequencies of the various histopathological types of NHL are generally similar among Asian countries. Compared to the United States, Asian countries, including those in the Far East, have higher rates of aggressive NHL, T-cell NHL, and extranodal (EN) diseases [1,4-6].
T-cell NHL is a relatively uncommon malignancy, accounting for approximately 12% of all lymphomas. Its incidence varies widely, from 1.5% in Vancouver, British Columbia, Canada, to 18.3% in Hong Kong. This may in part reflect increased exposure to pathogenic factors, such as human T-cell leukemia virus-1 and Epstein-Barr virus (EBV), in Asia [7-9]. Although NHL accounts for 2.3% of all cancers in Korea, the incidence of T-cell NHL has not been determined accurately.
The International Prognostic Index (IPI) and age-adjusted IPI (AAIPI) are established scoring systems that predict survival in patients with aggressive NHL [4]. However, the data from which these indices were derived were obtained primarily from studies performed in Western countries. Therefore, the IPI may not be directly applicable to Asian populations, in which the incidence of EN disease is higher than in Western populations [6,10]. Therefore, we retrospectively assessed the relative frequency and clinical features of T-cell NHL in Korean patients, and examined the validity and usefulness of the IPI/AAIPI in Koreans.
METHODS
Patients
Between April 1998 and December 2003, 586 patients aged 15 years or older were diagnosed with histologically confirmed NHL at Asan Medical Center, Seoul, Korea. Of these, 101 patients were diagnosed with T-cell NHL and treated with the appropriate modality. We retrospectively reviewed their clinical records, including patient age, sex, date, and site of diagnostic biopsies, histologic subtype and EN sites of involvement, performance status, IPI and AAIPI scores, laboratory/radiological data, and Ann Arbor stage.
Clinical staging and methods
Clinical stage, including patient history and physical examination (including Waldeyer's ring), was determined using the Ann Arbor classification. Laboratory data reviewed included a complete blood count, renal function tests, serum electrolytes, liver function tests, serum lactate dehydrogenase (LDH), β2-microglobulin concentrations, and bone marrow aspiration with a trephine biopsy. Radiological data consisted of chest X-rays and computed tomography (CT) of the chest, abdomen, pelvis, and primary site of presentation. In selected patients, additional evaluations were performed, including magnetic resonance imaging (MRI) of the brain and spine, panendoscopy and gastroscopy, and positron emission tomography (PET).
Definitions of nodal and extranodal lymphoma
Lymphomas with clinically dominant lymph node involvement were considered primary nodal (NL) lymphomas, whereas those with primary extranodal involvement or a manifestation of extensively disseminated systemic disease were considered extranodal (EN). Primary EN lymphomas (PENL) were defined as those presenting with EN involvement and no or only minor lymph node involvement. Lymphomas with extensive disease involving both nodal and EN sites were considered nodal lymphomas [11].
Histological evaluation
All histological specimens were reviewed by a single pathologist (Jooryung Huh) and diagnosed according to the World Health Organization/Revised European-American Lymphoma (WHO/REAL) system [12].
Statistical analysis
The overall survival (OS) was defined as the time from the date of diagnosis to death from any cause or last follow-up visit. Survival curves were estimated according to the Kaplan-Meier method [13] and compared using the log-rank test. The log-rank test was also used for univariate determinations of the correlation between individual clinical features and OS [14]. Multivariate analyses using the Cox proportional hazards model were performed with factors found to be potentially predictive of survival in univariate analyses [15]. A p value <0.05 was considered significant. All statistical analyses were performed using SPSS version 12.0 (SPSS Inc., Chicago, IL).
RESULTS
Patient characteristics
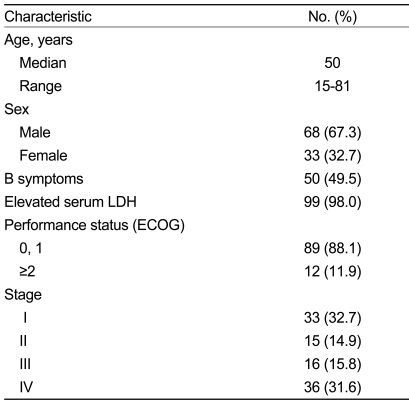
Of the 586 patients with NHL, 101 (17.2%) were diagnosed with T-cell NHL; Table 1 shows their baseline characteristics. Their median age was 50 years (range 15-81 years), and the ratio of males to females was 2.06:1. B symptoms were observed in 50 patients (49.5%) and serum LDH was elevated in 99 (98.0%). Eastern Cooperative Oncology Group (ECOG) performance status was 0-1 in 89 patients (88.1%) and 2-4 in 12 patients (11.9%). According to the Ann Arbor classification, 33 (32.7%), 15 (14.9%), 16 (15.8%), and 36 (31.6%) patients were stage 1 to 4, respectively.
Table 1.
Patient characteristics
LDH, lactate dehydrogenase.
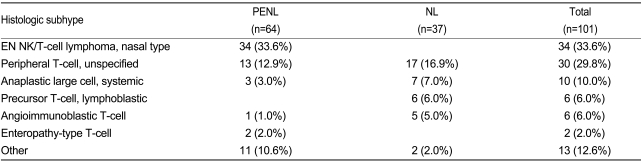
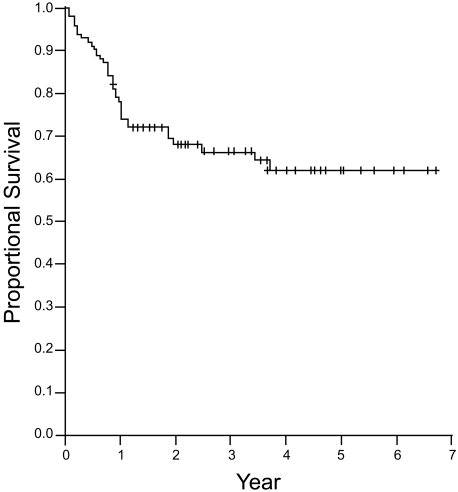
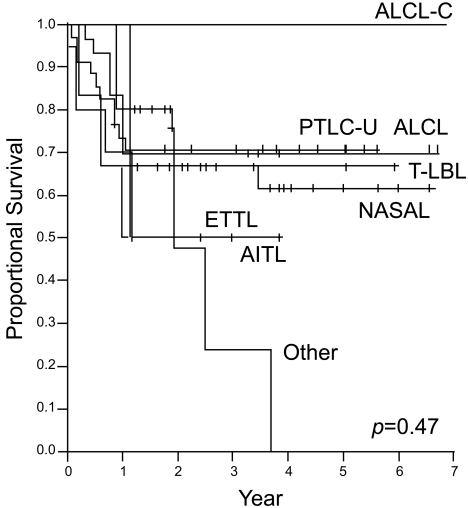
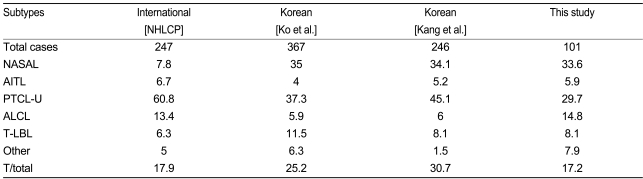
Table 2 and Figure 1 show the baseline histology of the patient population. Thirty-four patients (33.6%) had extranodal NK/T-cell lymphoma, nasal type (NASAL), 30 (29.8%) had peripheral T-cell lymphoma, unspecified (PTCL-U), and 10 (10%) had anaplastic large cell lymphoma, T/null cell, primary systemic type (ALCL). In addition, 64 patients (63.4%) had PENL in T-cell NHL (total of 101 patients), similar to the 294 patients (60.6%) with PENL in B-cell NHL (total of 485 patients).
Table 2.
Histology of T-cell NHL
EN, extranodal; PENL, primary extranodal lymphoma; NL, nodal lymphoma.
Figure 1.
Histology of T-cell NHL. NASAL, extranodal NK/T-cell lymphoma, nasal; PTCL-U, peripheral T-cell lymphoma, unspecified; ALCL, anaplastic large cell lymphoma, T/null cell, primary systemic type; T-LBL, precursor T-cell lymphoblastic lymphoma; AITL, angioimmunoblastic T-cell lymphoma; ETTL, enteropathy-type T-cell lymphoma; ALCL-C, ALCL-cutaneous.
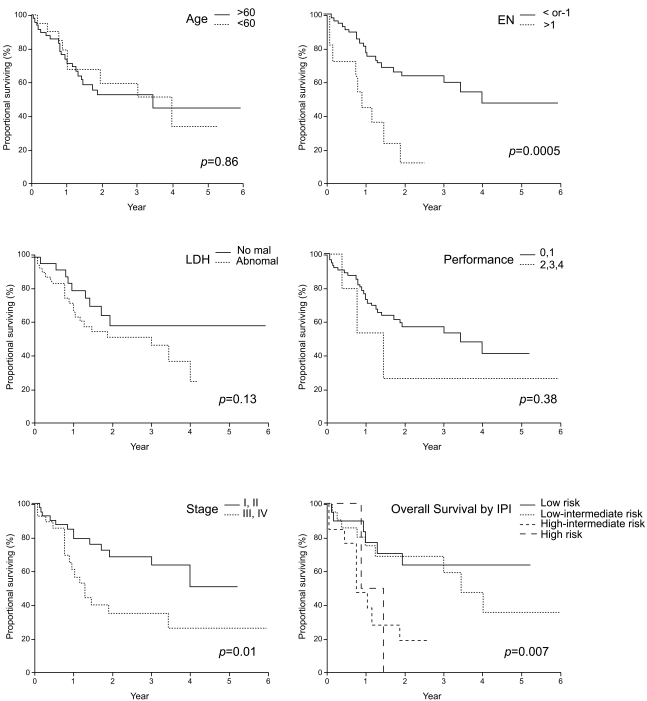
Overall survival
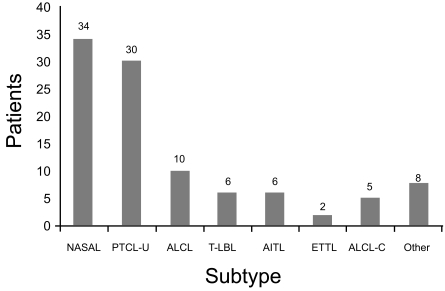
Figure 2 shows the OS for all patients. With a median follow-up of 38.4 months, the median OS was not reached. The 5-year survival rate was 62%. The median follow-up for the 67 surviving patients was 38.4 months (range 7.2-80.4 months). Figure 3 shows the OS according to T-cell NHL subtype. The seven pathological subtypes seen in this study could be classified into three prognostic subgroups: favorable, intermediate, and unfavorable. Patients with cutaneous ALCL (ALCL-C) were classified as favorable, with a 5-year OS of 100%. Patients with PTCL-U, ALCL, precursor T-cell lymphoblastic lymphoma (T-LBL), and NASAL were classified as intermediate, with a 5-year OS of 60-70%. Patients with enteropathy-type T-cell lymphoma (ETTL) and angioimmunoblastic T-cell lymphoma (AITL) were classified as unfavorable, with a 5-year OS of 50%.
Figure 2.
Overall survival of all patients.
Figure 3.
Overall survival (OS) according to histology. The seven pathological subtypes observed could be classified into three prognostic subgroups (favorable, intermediate, and unfavorable) with respect to the OS. NASAL, extranodal NK/T-cell lymphoma, nasal; PTCL-U, peripheral T-cell lymphoma, unspec-ified; ALCL, anaplastic large cell lymphoma, T/null cell, primary systemic type; T-LBL, precursor T-cell lymphoblastic lymphoma; AITL, angioimmunoblastic T-cell lymphoma; ETTL, enteropathy-type T-cell lymphoma; ALCL-C, ALCL-cutaneous.
Prognostic factors
The IPI consists of five risk factors: age >60 years, lactate dehydrogenase (LDH) >upper limit of normal (ULN), ECOG performance status >1, stage III or IV disease, and >1 extranodal site. We assessed the validity and usefulness of the IPI/AAIPI in patients with the three most frequent subtypes of T-cell NHL (NASAL, PTCL-U, and ALCL), which accounted for 78% of our patients with T-cell NHL. Figure 4 shows the OS relative to IPI risk factors. We found that tumor stage (p=0.0133) and EN involvement (p=0.0005) were significantly associated with OS, whereas age (p=0.86), LDH (p=0.13), and performance (p=0.38) were not. We also found that the number of EN sites was significantly related to OS (p=0.0017). The OS of patients with the NASAL, PTCL-U, and ALCL subtypes of T-cell NHL was significantly associated with the IPI score (p=0.007). The median OS of the low-risk group was not reached. The median OS of the low-intermediate, high-intermediate, and high-risk groups was 41, 10, and 10 months, respectively. When we applied the AAIPI to our patients, we found that this index was also significantly associated with OS (p=0.043). Using this index, however, we found that the number of patients was highest in the low-intermediate risk group, followed by the low, high, and high-intermediate risk groups, in decreasing order.
Figure 4.
Overall survival according to the International Prognostic Index (IPI) score. Low-risk, IPI score 0, 1; low-intermediate risk, IPI score 2; high-intermediate risk, IPI score 3; high-risk, IPI score 4, 5.
Univariate analysis showed that factors predicting unfavorable OS included tumor stage, EN involvement, and greater number of EN sites. Multivariate analysis showed that a greater number of EN sites was the only independent prognostic indicator for patients with the three most frequent subtypes of T-cell NHL in Korea (p=0.042).
DISCUSSION
Over the last two decades, the incidence of NHL in Korea has increased. This trend is likely due to improvements in diagnostic techniques, including the widespread use of CT, MRI, endoscopy, and PET. Moreover, the availability of safer anesthetics, leading to more frequent and extended biopsies, including those performed in elderly and frail patients, is also a factor. In addition, immunophenotypic, cytogenetic, and molecular analyses have enhanced diagnostic capabilities and improved the classification and prognostication for patients with T-cell NHL [16].
Assessments of the epidemiology and geographical distribution of NHL in different countries have shown that the relative frequency of different NHL subtypes in Korea was similar to that in other Far East countries, but distinct from that in Western countries [17-22]. For example, follicular lymphoma has a greater incidence in North America, the United Kingdom, and South Africa (31%) than in other countries (14%). Peripheral T-cell lymphoma was most common in London, Cape Town, and Hong Kong (9%), whereas other cities had much lower incidences (average 3%) [12,23]. Less is known about the incidence of NHL subtypes in Korea. Although clinical studies have examined the incidence of B-cell NHL subtypes in Korea, none have examined T-cell NHL. The latter has been reported only as case series, making it difficult to compare the incidence in Korea with that in other countries. Overall, the National Cancer Registry of Korea has reported that NHL accounted for 2.3% (2,246 patients) of all Korean patients with cancer in 2002 (99,025 patients) [24].
Table 3 compares our results, including the clinical features and distribution of histopathology, with those previously reported in Korea and Western countries [5,8,25]. In 1997, the proportion of patients with NHL in Western countries with T-cell NHL was 17.9%, and the three most frequent subtypes were PTCL-U (60.8%), ALCL (13.4%), and NASAL (7.8%). Case series reported in 1997 and 1998 found that the proportion of patients with NHL in Korea who had T-cell NHL was higher (25.2 and 30.7%) than in Western countries. While PTCL-U was the most common subtype in Korea, its relative frequency (34.1-45.1%) was lower than in Western countries. In contrast, the incidence of NASAL was higher (34.1-35%) in Korea than in Western countries. Compared to these earlier findings, we found that the proportion of patients with NHL in Korea who had T-cell NHL was lower (17.2%), similar to that in Western countries, and that NASAL was the most frequent subtype. Moreover, the incidence of PTCL-U decreased, while that of ALCL increased greatly, from 6 to 14.8%. Furthermore, the prognosis of patients with ALCL differed between Korea and Western countries. In Western countries, patients with ALCL have a more favorable prognosis. Moreover, patients with ALCL who are positive for anaplastic lymphoma kinase (ALK) have a significantly more favorable prognosis than those negative for ALK, with 5-year OS rates of 79% and 46%, respectively [26,27]. In contrast, Korean patients with ALCL have a less favorable prognosis [27]. However, these patients were not tested for ALK; therefore, we could not evaluate the significance of a positive ALK.
Table 3.
Relative frequency of T-cell NHL
NASAL, extranodal NK/T-cell lymphoma, nasal; AITL, angioimmunoblastic T-cell lymphoma; PTCL-U, peripheral T-cell lymphoma, unspecified; ALCL, anaplastic large cell lymphoma, T/null cell, primary systemic type; T-LBL, precursor T-cell lymphoblastic lymphoma; NHLCP, Non-Hodgkin's Lymphoma Classification Project.
Primary extranodal lymphomas have a diverse etiology, pathogenesis, pattern of presentation, and outcome [28]. In Western countries, at least one-quarter of NHL arises primarily at EN sites, and these countries show great geographical variation in the incidence of EN lymphomas. Less is known about the incidence of NHL in developing countries [29,30]. In Korea, two-thirds of patients with NHL have EN involvement at the initial presentation, a finding confirmed here (63.4%) [10]. The incidence of PENL was much higher than that observed in the United States, Hong Kong, Japan, and Taiwan [5,18,21,31,32]. In particular, Koreans have higher rates of aggressive NHL and T-cell lymphomas, especially NASAL. This may be due to the higher incidence of EBV infection in Koreans, although further studies are needed to determine the true causes of these geographic differences [7,16].
The IPI scoring system was developed to predict survival in patients with aggressive NHL [4]. We assessed the validity and usefulness of the IPI/AAIPI in patients with the three most frequent subtypes of T-cell NHL: NASAL, PTCL-U, and ALCL. We found that two components of the IPI were significantly associated with the OS: stage (p=0.0133) and EN involvement (p=0.0005). In addition, the OS in patients with the NASAL, PTCL-U, and ALCL subtypes of T-cell NHL was associated with the overall IPI (p=0.007) and AAIPI (p=0.184) scores. Although we do not illustrate the application of the AAIPI, the medial OS according to subgroup was different: low-risk, high-risk, low-intermediate, and high-intermediate in decreasing order. Since the AAIPI does not include EN involvement as a factor, serious drawbacks exist to its use in Korea, where the incidence of EN involvement is higher than in Western populations. We found that the number of EN sites was significantly related to the median OS (p=0.0017), and multivariate analysis showed that a greater number of EN sites was the only independent prognostic indicator of OS among Korean patients with the NASAL, PTCL-U, and ALCL subtypes of T-cell NHL (p=0.042).
Our study has several important limitations, including its retrospective design and the inclusion of patients from a single center. Therefore, to confirm our results, performing a prospective, multicenter study is necessary. A second limitation was the absence of immunophenotypic, cytogenetic, and molecular analyses, including assays for ALK and abnormal cytogenetics. A third limitation was our inability to calculate the progression-free survival time, since the patients were treated using various modalities. For the same reason, we could not estimate treatment-related toxicities and mortalities.
ALCL subtype have a more favorable prognosis than Korean patients. In assessing patient prognosis, the IPI scoring system should not be applied uniformly to Korean populations, although this system was developed to predict survival in patients with aggressive NHL. In addition, our results indicate that the number of EN sites is a significant factor. Therefore, our findings suggest the need for large-scale studies of Korean patients with T-cell NHL.
References
- 1.Cancer facts and figures [Internet] American Cancer Society. [Cited 2008]. Available from: www.cancer.org .
- 2.Muller A, Ihorst G, Mertelsmann R, Engelhardt M. Epidemiology of non-Hodgkin's lymphoma (NHL): trends, geographic distribution, and etiology. Ann Hematol. 2005;84:1–12. doi: 10.1007/s00277-004-0939-7. [DOI] [PubMed] [Google Scholar]
- 3.Cancer incidence, mortality and prevalence worldwide, version 1.0 IARC Cancer Base No.5 [Internet] IARC. [Cited 2001]. Available from: http://www-dep.iarc.fr/globocan.htm .
- 4.The international Non-Hodgkin's Lymphoma Prognostic Factors Project. A predictvie model for aggressive non-Hodgkin's lymphoma. N Engl J Med. 1993;329:987–994. doi: 10.1056/NEJM199309303291402. [DOI] [PubMed] [Google Scholar]
- 5.Ko YJ, Kim CW, Park CS, et al. Classification of malignant lymphomas in the Republic of Korea: incidence of recently recognized entities and changes in clinicopathologic features. Hematolymphoreticular Study Group of the Korean Society of Pathologists. Revised European-American lymphoma. Cancer. 1998;83:806–812. [PubMed] [Google Scholar]
- 6.Mok TS, Steinberg J, Chan AT, et al. Application of the international prognostic index in a study of Chinese patients with non-Hodgkin's lymphoma and a high incidence of primary extranodal lymphoma. Cancer. 1998;82:2439–2448. doi: 10.1002/(sici)1097-0142(19980615)82:12<2439::aid-cncr19>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 7.Jaffe ES, Chan JK, Su IJ, et al. Report of the Workshop on Nasal and Related Extranodal Angiocentric T/Natural Killer Cell Lymphomas: definitions, differential diagnosis, and epidemiology. Am J Srug Pathol. 1996;20:103–111. doi: 10.1097/00000478-199601000-00012. [DOI] [PubMed] [Google Scholar]
- 8.The Non-Hodgkin's Lymphoma Classification Project. A clinical evaluation of the International Lymphoma Study Group classification of non-Hodgkin's lymphoma. Blood. 1997;89:3909–3918. [PubMed] [Google Scholar]
- 9.Rudiger T, Weisenbruger DD, Anderson JR, et al. Peripheral T-cell lymphoma (excluding anaplastic large cell lymphoma): results from the Non-Hodgkin's Lymphoma Classification Project. Ann Oncol. 2002;13:140–149. doi: 10.1093/annonc/mdf033. [DOI] [PubMed] [Google Scholar]
- 10.Kim HT, Im YH, Suh CI, et al. Malignant lymphomas in Korea. J Korean Cancer Assoc. 1992;24:92–101. [Google Scholar]
- 11.Lopez-Guillermo A, Colomo L, jimenez M, et al. Diffuse lagrge B-cell lymphoma: clinical and biological characterization and outcome according to the nodal and extranodal primary origin. J Clin Oncol. 2005;23:2797–2804. doi: 10.1200/JCO.2005.07.155. [DOI] [PubMed] [Google Scholar]
- 12.Harris NL, Jaffe ES, Diebold J, et al. The World Health Organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues: report of the Clincal Advisory Committee Meeting, Airlie House, Virginia, November 1997. Histopathology. 2000;36:69–86. doi: 10.1046/j.1365-2559.2000.00895.x. [DOI] [PubMed] [Google Scholar]
- 13.Kaplan E, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958:53. [Google Scholar]
- 14.Mantel N. Evaluation of survival data and two new rank test order statistics arising in tis consideration. Cancer Chemother Rep. 1966;50:163–170. [PubMed] [Google Scholar]
- 15.Cox D. Regression models and life-tables. J R Stat Soc. 1972:34. [Google Scholar]
- 16.Rizvi MA, Evens AM, Tallman MS, Nelsoon BP, Rosen ST. T-cell non-Hodgkin lymphoma. Blood. 2006;107:1255–1264. doi: 10.1182/blood-2005-03-1306. [DOI] [PubMed] [Google Scholar]
- 17.Kadin ME, Berard CW, Nanba K, Wakasa H. Lymphoproliferative diseases in Japan and Western countries: proceedings of the United States-Japan Seminar, September 6 and 7, 1982, in Seattle, Washington. Hum Pathol. 1983;14:745–772. doi: 10.1016/s0046-8177(83)80299-8. [DOI] [PubMed] [Google Scholar]
- 18.Ho FC, Todd D, Loke SL, Ng RP, Khoo RK. Clinico-pathological features of malignant lymphomas in 294 Hong Kong Chinese patients: retrospective study covering an eight-year period. Int J Cancer. 1984;34:143–148. doi: 10.1002/ijc.2910340202. [DOI] [PubMed] [Google Scholar]
- 19.The T- and B-cell Malignancy Group. Statistical analyses of clinico-pathological, virological and epidemiological data on lymphoid malignancies with special reference to adutl T-cell leukemia/lymphoma: a report of the second nationwide study of Japan. Jpn J Clin Oncol. 1985;15:517–535. [PubMed] [Google Scholar]
- 20.The Nationwide Lymphoma Pathology Cooperative Group (NLPCG) A retrospective histological study of 9,009 cases of malignant lymphoma in China using the NLPCG classification. Jpn J Clin Oncol. 1985;15:645–651. [PubMed] [Google Scholar]
- 21.Aozasa K, Tsujimoto M, Sakurai M, et al. Non-Hodgkin's lymphomas in Osaka, Japan. Eur J Cancer Clin Oncol. 1985;21:487–492. doi: 10.1016/0277-5379(85)90042-2. [DOI] [PubMed] [Google Scholar]
- 22.Newton R, Ferlay J, Beral V, Devesa S. The epidemiology of non-Hodgkin's lymphoma: comparison of nodal and extranodal sites. Int J Cancer. 1997;72:923–930. doi: 10.1002/(sici)1097-0215(19970917)72:6<923::aid-ijc1>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 23.Anderson JR, Armitage JO, Weisenbruger DD. Epidemiology of the non-Hodgkin's lymphomas: distrubtions of the major subtypes differ by geographic locations. Non-Hodgkin's Lymphoma Classification Project. Ann Oncol. 1998;9:717–720. doi: 10.1023/a:1008265532487. [DOI] [PubMed] [Google Scholar]
- 24.National Cancer Center, National Cancer Registry of Korea [internet] National Cancer center; c2008. [cited 2008 Oct 1]. Available from: http://www.ncc.re.kr . [Google Scholar]
- 25.Kang YK, Kim BS, Kim TW, et al. Clinicopathologic characteristics of Korean non-Hodgkin's lymphomas based on REAL classification. J Korean Cancer Assoc. 1999;31:641–652. [Google Scholar]
- 26.Falini B, Pileri S, Zinzani PL, et al. ALK+ lymphoma: clinocopathologcial findings and outcome. Blood. 1999;93:2697–2706. [PubMed] [Google Scholar]
- 27.Gascoyne RD, Aoun P, chhanabhai M, et al. Prognostic significance of anaplastic lymphoma kinase (ALK) protein expression in adults with anaplastic large cell lymphoma. Blood. 1999;93:3913–3921. [PubMed] [Google Scholar]
- 28.Gospodarowicz MK, Sutcliffe SB. The extranodal lymphomas. Semi Radiat Oncol. 1995;5:281–300. doi: 10.1054/SRAO00500281. [DOI] [PubMed] [Google Scholar]
- 29.Zucca E, Roggero E, Bertoni F, Cavalli F. Primary extranodal non-Hodgkin's lymphomas: part I. gastrointestinal, cutaneous and genitourinary lymphomas. Ann Oncol. 1997;8:727–737. doi: 10.1023/a:1008282818705. [DOI] [PubMed] [Google Scholar]
- 30.Zucca E, Conconi A, Cavalli F. Treatment of extranodal lymphomas. Best pract Res Clin Haematol. 2002;15:533–547. doi: 10.1053/beha.2002.0218. [DOI] [PubMed] [Google Scholar]
- 31.Shih LY, Liang DC. Non-Hodgkin's lymphomas in Asia. Hematol Oncol Clin North Am. 1991;5:983–1001. [PubMed] [Google Scholar]
- 32.Greiner TC, Medeiros LJ, Jaffe ES. Non-Hodgkin's lymphoma. Cancer. 1995;75(1) Suppl:370–380. doi: 10.1002/1097-0142(19950101)75:1+<370::aid-cncr2820751319>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]