Abstract
Anisakidae larvae can cause anisakiasis when ingested by humans. Although several groups have reported a gastrointestinal Anisakis allergy among people in Spain and Japan, our report is the first to summarize the clinical features of 10 Anisakis allergy cases in Korea. We enrolled 10 Korean patients (6 men and 4 women) who complained of aggravated allergic symptoms after ingesting raw fish or seafood. Sensitization to Anisakis was confirmed by detecting serum specific IgE to Anisakis simplex. The most common manifestation of anisakiasis was urticaria (100%), followed by abdominal pain (30%) and anaphylaxis (30%). All patients presenting with these symptoms also exhibited high serum specific IgE (0.45 to 100 kU/L) to A. simplex. Nine patients (90%) exhibited atopy and increased total serum IgE levels. The fish species suspected of carrying the Anisakis parasite were flatfish (40%), congers (40%), squid (30%), whelk (10%), and tuna (10%). Anisakis simplex should be considered as a possible causative food allergen in adult patients presenting with urticaria, angioedema, and anaphylaxis following the consumption of raw fish or seafood.
Keywords: Anisakis simplex, Fish, Food allergy
INTRODUCTION
The development of food allergies is an increasingly common concern among consumers worldwide. In the United States, approximately 6% of infants and young children, and 3.7% of adults exhibit some degree of allergic reaction to certain foods. The most common causal foods in young children are cows' milk, eggs, peanuts, wheat, soy, tree nuts, fish, and shellfish; in adults, shellfish, peanuts, tree nuts, and fish lead the list [1].
Anisakis simplex is a nematode belonging to the order Ascaridida, family Anisakidae, and subfamily Ascaridoidea. Any fish or cephalopod species can be parasitized by third-stage Anisakis larvae. Codfish, hake, sardines, anchovies, salmon, tuna, and squid are among the most frequently parasitized species. The ingestion of third-stage Anisakis larvae can cause anisakiasis in humans. Symptoms of anisakiasis arise when the nematode penetrates the gastric mucosa, which leads to serious abdominal and allergic symptoms [2].
Van Thiel et al. [3] reported the first case of anisakiasis, in the Netherlands in 1960. Subsequently, many cases have been reported in Japan and Western Europe, where raw fish are consumed frequently. Kim et al. [4] reported a case of Anisakis larvae present in the human oropharynx as the first case of anisakiasis in Korea, in 1971. Thereafter, several patients suffering acute anisakiasis and presenting mainly with gastrointestinal symptoms such as abdominal pain, nausea, vomiting, and diarrhea have been analyzed via gastroduodenoscopy .
Desowitz et al. [5] described a method for detecting specific IgE against A. simplex in 1985. Since that time, Kasuya et al. [6] have confirmed the allergic potential of A. simplex in two clinical reports and emphasized this species as a causative allergen related to fish consumption in urticaria patients. In Korea, since Kim et al. [7] reported the first case of gastroallergic anisakiasis, which developed after the patient had consumed raw fish on Jeju Island, there have been no published reports on Anisakis-induced allergic reactions, although Koreans freely ingest raw fish. Here, we report the clinical features of 10 Korean patients diagnosed with Anisakis allergies.
CASE REPORT
Ten patients (6 men and 4 women) who developed abdominal pain, acute or chronic urticaria/angioedema, or anaphylaxis less than 24 hours after ingesting seafood were enrolled in our study. Sensitization to A. simplex was assessed by detecting serum specific IgE to A. simplex (ImmunoCAP System; Phadia, Uppsala, Sweden).
We investigated the clinical parameters of each patient, including age, gender, allergic symptoms, fish species ingested, associated allergic diseases including food allergies, atopic dermatitis, bronchial asthma, allergic rhinitis, chronic urticaria, and atopy status. Total eosinophil counts were measured in peripheral blood samples obtained from each patient. We also measured the serum total IgE, specific IgE to A. simplex, and eosinophilic cationic protein (ECP) level using an ImmunoCAP System (Phadia). Specific IgE to Anisakis was considered positive at >0.35 kU/L, according to the manufacturer's instructions. Atopy status was defined in patients showing a positive response to one or more common inhalant allergens such as house dust mites, tree pollen, and weed pollen on an allergic skin prick test.
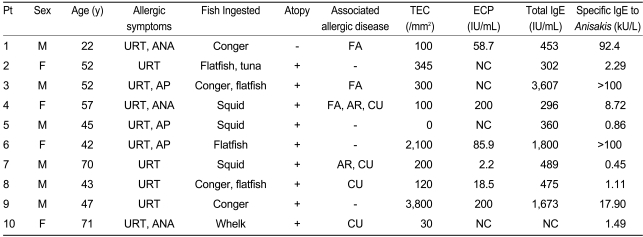
Clinical features and laboratory findings
The clinical features and laboratory findings of the 10 patients with Anisakis allergy are summarized in Table 1. The mean age of the patients was 50 years (range, 22-71 years). All 10 patients had high serum specific IgE to A. simplex, ranging from 0.45-100 kU/L, and this was not related to the severity of the allergic reactions. Nine of the 10 patients (90%) had atopy. The levels of total serum IgE of these nine patients were increased. The total peripheral eosino-phil counts were above baseline in two patients, and all but one of the patients in whom the serum ECP level was assessed exhibited an increased ECP levels.
Table 1.
Clinical features and laboratory findings of the 10 patients with Anisakis allergy
Pt, patient; M, male; F, female; URT, urticaria; ANA, anaphylaxis; AP, abdominal pain; +, present; -, absent; FA, food allergy; AR, allergic rhinitis; CU, chronic urticaria; TEC, total eosinophil count; ECP, eosinophilic cationic protein; NC, not checked.
Chronic urticaria was noted in four patients (40%), food allergy was recorded in three (30%), and allergic rhinitis was exhibited by two (20%). Bronchial asthma and atopic dermatitis symptoms were not identified in any of the Anisakis allergy patients.
Clinical symptoms and the implicated seafood source
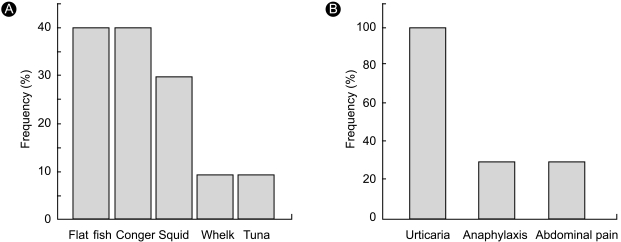
The most common manifestation of anisakiasis in our study was urticaria/angioedema (100%), followed by abdominal pain (30%) and anaphylaxis (30%). The fish implicated in transmitting the parasites were flatfish (40%), congers (40%), squid (30%), whelk (10%), and tuna (10%) (Fig. 1).
Figure 1.
The fish species ingested (A) and the common allergic symptoms (B) in the patients with Anisakis allergies.
DISCUSSION
Parasitic A. simplex can infest humans and cause anisakiasis when ingested with fish in its raw or undercooked form [2]. Since Kasuya et al. [6] first reported on Anisakis allergies in mackerel-induced urticaria patients in 1990, many Anisakis-induced allergic reactions have been reported, especially in Japan and Spain. Infestation with A. simplex causes direct tissue damage following an invasion of the gut wall, the development of an eosinophilic granuloma, the perforation of the gut, and strong allergic reactions [2]. The most frequent clinical manifestation of an Anisakis allergy is urticaria with or without facial angioedema [2]. Occasionally, anaphylactic shock occurs in patients exhibiting an Anisakis allergy.
Audicana et al. [8] reported the clinical manifestations of allergies attributable to A. simplex in 67 cases in Spain: urticaria/angioedema was observed in all patients, gastrointestinal symptoms occurred in 40% of the patients, and anaphylactic shock was observed in 12%. Overall, 88% of the patients expressed increased serum total IgE levels. Uncommon manifestations of anisakiasis include Anisakis-induced eosinophilic gastroenteritis, occupational disease, rheumatic manifestations, and contact dermatitis [9]. In our patient cases, we determined the most common allergic symptoms to be acute or chronic urticaria/angioedema, which was observed in all patients; abdominal pain and anaphylaxis occurred in three (30%) patients. Most patients presented with atopy and high total serum IgE levels. This study represents the first report on the clinical features of 10 cases of Anisakis allergy in Korea. We suggest that Anisakis allergy should be considered in the differential diagnosis of Korean patients presenting with a range of allergic symptoms, from urticaria to anaphylactic shock, especially if these patients present with atopy and recent seafood ingestion.
Anisakis simplex is the most common hidden allergen in food [10]. Añíbarro et al. [10] described the role of hidden allergens in allergic reactions, reporting that of 530 allergic reactions to food, 119 (22.4%) cases were considered to be responses to hidden allergens. Furthermore, 65 reactions (12%) were anaphylaxis, and 38 (58.5%) of those were the result of hidden allergens. Añíbarro and colleagues [10] also showed that A. simplex was the cause of 58% of their anaphylaxis cases and was the most common cause of hidden food reactions (45%), followed by nuts (13%) and fish (7.9%). Thus, A. simplex should be considered a prevalent hidden allergen involved in food allergic reactions.
The fish species most frequently involved in Anisakis allergy are hake, anchovy, and cod, although studies have reported these fish in different orders of importance [2,9]. In our study, flatfish and congers were implicated most often, followed by squid, whelk, and tuna. These results differed from those of other studies [2]. We postulate that the differences result from variations in the fish species consumed in Korea. Flatfish and conger are the fish most frequently consumed raw in Korea; Seol et al. [11] stated that the main source of Anisakis infection in their patients was Conger myriaster.
The diagnosis of Anisakis allergy is based on three criteria: a compatible history such as urticaria, angioedema, or anaphylaxis that developed following fish consumption; a positive skin prick test or the presence of serum specific IgE to A. simplex; and the lack of a reaction to proteins from the host fish [8,9]. In the present study, all of the patients had a history compatible with Anisakis allergy and had high serum specific IgE to A. simplex. All of the patients, with the exception of three who refused the test, showed negative responses to host fish extracts in skin prick tests. The failure to perform the skin test in three cases may be a limitation of our study.
The best treatment for anisakiasis is prophylaxis. The larvae cannot survive in temperatures above 60℃ for 10 min or below -20℃ for 24 h [9]. We requested that our patients avoid eating raw fish while we were monitoring allergic symptoms and serum specific IgE to A. simplex.
In conclusion, we recommend that A. simplex be considered as a possible causative food allergen in adults presenting with urticaria, angioedema, or anaphylaxis following raw fish or seafood consumption.
Footnotes
This study was supported by a grant from the Korean Health 21 R&D Project, Ministry of Health and Welfare, Republic of Korea (03-PJ10-PG13-GD01-0002).
References
- 1.Sampson HA. Update on food allergy. J Allergy Clin Immunol. 2004;113:805–819. doi: 10.1016/j.jaci.2004.03.014. [DOI] [PubMed] [Google Scholar]
- 2.Moreno-Ancillo A, Caballero MT, Cabañas R, et al. Allergic reactions to Anisakis simplex parasitizing seafood. Ann Allergy Asthma Immunol. 1997;79:246–250. doi: 10.1016/S1081-1206(10)63009-8. [DOI] [PubMed] [Google Scholar]
- 3.Van Thiel PH, Kuiper FK, Roskam RTH. A nematode parasitic to herring causing acute abdominal syndromes in man. Trop Geogr Med. 1960;12:97–113. [PubMed] [Google Scholar]
- 4.Kim CH, Chung BS, Moon YI, Chun SH. A case report on human infection with Anisakis sp. in Korea. Korean J Parasitol. 1971;9:39–43. doi: 10.3347/kjp.1971.9.1.39. [DOI] [PubMed] [Google Scholar]
- 5.Desowitz RS, Raybourne RB, Ishikura H, Kliks MM. The radioallergosorbent test (RAST) for the serologic diagnosis of human anisakiasis. Trans R Soc Trop Med Hyg. 1985;79:256–259. doi: 10.1016/0035-9203(85)90351-7. [DOI] [PubMed] [Google Scholar]
- 6.Kasuya S, Hanano H, Izumi S. Mackerel-induced urticaria and Anisakis. Lancet. 1990;335:665. doi: 10.1016/0140-6736(90)90455-e. [DOI] [PubMed] [Google Scholar]
- 7.Kim SH, Kim HU, Lee JC. A case of gastroallergic anisakiasis. Korean J Med. 2006;70:111–1166. [Google Scholar]
- 8.Audicana M, Garcia M, del Pozo MD, et al. Clinical manifestations of allergy to Anisakis simplex. Allergy. 2000;55(S59):28–33. [Google Scholar]
- 9.Audicana MT, Ansotegui IJ, de Corres LF, Kennedy MW. Anisakis simplex: dangerous-dead and alive? Trends Parasitol. 2002;18:20–25. doi: 10.1016/s1471-4922(01)02152-3. [DOI] [PubMed] [Google Scholar]
- 10.Añíbarro B, Seoane FJ, Múgica MV. Involvement of hidden allergens in food allergic reactions. J Investig Allergol Clin Immunol. 2007;17:168–172. [PubMed] [Google Scholar]
- 11.Seol SY, Ok SC, Pyo JS, et al. Twenty cases of gastric anisakiasis caused by Anisakis type I larva. Korean J Gastroenterol. 1994;26:17–24. [Google Scholar]