Abstract
Objective
Octreotide is used to treat patients with neuroendocrine tumors. Previous reports show that octreotide long-acting repeatable (LAR) dose and patient body weight affect nadir plasma octreotide levels (approximately 1250, 2500, 5000, and 11,000 pg/mL for LAR doses of 10, 20, 30 and 60 mg/mo). However, plasma octreotide levels have decreased over time in patients receiving these doses of LAR.
Methods
From November 2004 until July 2007, trough plasma octreotide levels were determined in 86 patients on long-term octreotide LAR therapy at doses of 30, 60, and 120 mg/mo. Changes in plasma drug levels were analyzed over time using random effects models.
Results
Current plasma octreotide levels for octreotide LAR doses of 30, 60, and 120 mg/mo are approximately 2200, 5200, and 6500 pg/mL, respectively, representing a decrease of approximately 50% to 70% compared with previously reported plasma octreotide levels. The decreases in octreotide levels over time with the 30- and 60-mg/mo LAR doses are highly statistically significant (P = 0.0067, 0.0149, respectively).
Conclusions
Current plasma octreotide values are significantly lower than previously reported for 30-, 60-, and 120-mg/mo LAR doses. Serial plasma octreotide value measurements should be used to determine if increasing symptoms or tumor growth are associated with suboptimal octreotide levels.
Keywords: somatostatin analogs, somatostatin receptors, symptoms, plasma drug levels, sustained release preparations, carcinoid syndrome, tachyphylaxis
Octreotide is one of the most commonly used medications in the treatment of symptomatic neuroendocrine tumors (NETS). Traditionally, the vast majority of NETS patients receiving this medication have prompt and effective relief of their symptoms. We have previously shown that plasma octreotide levels correlate with both patient weight and the monthly dose of medication administered.1 In that study, trough plasma octreotide values were reported to be approximately 1250, 2500, 5000, and 11,000 pg/mL for long-acting repeatable (LAR) doses of 10, 20, 30, and 60 mg/mo, respectively.1
Octreotide acetate (Sandostatin; Novartis Pharmaceutical Company, East Hanover, NJ) is an octapeptide congener of native somatostatin that is widely used for the control of the symptoms associated with functionally active NETS.1–3 Octreotide acetate controls symptoms by inhibiting the secretion of peptides and amines associated with these functional tumors. Octreotide binds preferentially to sst 2, one of a family of somatostatin receptors (sst 1–sst 5).3 Octreotide acetate binds to the sst 2 receptor with an affinity (Kd, 50% receptor saturation) of approximately 1 nM (≅1000 pg/mL). Nearly complete saturation of the sst 2 receptor should occur, with circulating drug levels approximately 10 times higher than the Kd (1 nM, or ≅10,000 pg/mL).4–6 Subsequent inhibition of G-protein–associated signal transduction pathways block secretory vesicle exocytosis and the release of the target peptide or amine, thus effectively controlling symptoms. Clinically, the LAR form of octreotide is widely used for long-term symptom control, and the aqueous form of octreotide is commonly used (40%–70% of patients) as “rescue” medication for the acute control of symptoms.1–3
Long-acting repeatable octreotide is currently available in 3 doses: 10, 20, and 30 mg. These doses are most commonly administered once a month; however, patients receiving a dose of more than 30 mg/mo often have more frequent administration of 30-mg dose rather than multiple injections at the same time. Dosing this medication is at the discretion of the physician; however, the recommended starting dose of this drug is 20 mg/mo.1–3 Few, if any, physicians currently choose an alternative starting dose of LAR based on the patient's weight, height, body surface area, or body mass index. In the registration trials for this drug, up to 40% of patients required rescue medication several times a week, independent of the monthly LAR dose (10, 20, or 30 mg/mo) used for long-term symptom control.3 This implies that circulating drug levels produced by these doses of this medication are inadequate to completely saturate sst 2, and thus, the drug levels are not adequate to maximally suppress symptoms or tumor growth.4–6 Recently, Anthony et al7 showed that in current clinical practice, 20% to 40% of patients received LAR doses higher than the maximal dose (30 mg/mo) approved by the Food and Drug Administration to adequately control symptoms or to suppress tumor progression.
Recently, we have made several clinical and biochemical observations that led us to hypothesize that there may be an acute loss of bioactivity (decrease in drug release over time) with the current drug formulation of octreotide LAR (Sandostatin LAR). First, we observed a loss of effective symptom control in patients who have used octreotide acetate LAR at a constant dose for prolonged periods of time. In previous studies, approximately 40% of patients needed rescue medication for poorly controlled symptoms. It was our clinical impression that the number of patients requiring rescue and the number of rescue episodes per week increased significantly during the time frame of this study.3 Second, we have observed that patients who are currently using LAR have significantly lower trough plasma levels of octreotide than those previously published in the Novartis LAR drug registration trial or in our previously published plasma octreotide level study.1,2 Third, we have observed that patients who are given LAR at progressively higher doses (60–120 mg/mo) commonly fail to achieve plasma drug levels that will saturate the sst 2 receptors (approximately 10 nM or ≈10,000 pg/mL).
To confirm these observations, patients in our clinical practices who used chronic octreotide LAR therapy had their charts reviewed for their LAR doses (mg/mo) and their plasma octreotide levels (pg/mL). All plasma octreotide levels were measured by a single laboratory (Inter Science Institute, Inglewood, Calif). Finally, we compared current plasma octreotide levels produced by a LAR dose to previously reported plasma levels for that LAR dose and investigated the use of octreotide administered by continuous subcutaneous infusion as a means to restore plasma octreotide levels to those expected for a given octreotide dose (mg/mo).1,3
Materials and Methods
These studies were approved by the University Institutional Review Board of the Louisiana State University Health Sciences Center (protocol #6790), the East Virginia Medical School IRB (protocol #07-04-WC-0095), and the University of Iowa IRB (protocol #199911057). Patients with functional endocrine tumors from our clinical practices formed the basis of this study (n = 86). Twenty-six patients had single plasma octreotide determinations performed during the study period, and 60 patients had multiple plasma octreotide determinations over time. In all cases, patients were instructed to have their plasma octreotide level drawn immediately before their next LAR injection (trough levels). There was no attempt to control for the methods used for drug preparation or for drug injection because of the diverse geographic distribution of these patients. The time frame of this retrospective trial was from November 2004 until April 2007. Patients' charts were reviewed, and all patients on octreotide acetate LAR (Sandostatin LAR) had their plasma octreotide levels (n = 162 measurements) and octreotide LAR doses recorded over time. All octreotide doses were expressed as the number of milligrams of octreotide administered per month (approximately 30 days). Monthly doses of octreotide LAR ranged from 20 to 120 mg/mo. Most LAR doses greater than 30 mg/mo were administered as more frequent (biweekly or weekly) doses rather than once-per-month dosing.
All plasma octreotide levels were determined at Inter Science Institute and were reported in pictograms per milliliter. Based on our initial review of the data from this retrospective trial, we performed several short prospective trials to confirm portions of our data. The first prospective trial was undertaken to control for the personnel who mixed and administered the LAR and to precisely control the timing of the plasma octreotide value determination in relationship to the administration of the LAR. This trial spanned a 6-month period (January 2007–July 2007) and thus was essentially contemporaneous with the later points of the retrospective trial. Patients receiving LAR at a dose of 30 mg/mo during the last 6 months of the retrospective trial had a mean octreotide value of 2205 ± 1739 pg/mL (n = 18) as compared with a mean plasma level of 1996 ± 730 pg/mL (n = 8) in the prospective trial. Thus, in a more limited but precisely controlled study, significantly diminished plasma levels were demonstrated in patients receiving LAR at doses of 30 mg/mo as compared with both the Rubin and Woltering studies.1–3 We conducted one additional prospective study during the later phases of our retrospective trial (January 2007–July 2007). In this study, patients who were receiving their octreotide by continuous subcutaneous infusion (pump) had their plasma octreotide values determined. All plasma values were normalized to represent an octreotide dose of 30 mg/mo. These plasma octreotide values were used as a comparator for the plasma octreotide values seen in patients receiving octreotide LAR during the 2 historic trials and during our retrospective and prospective LAR trials.1,3
Statistical Analysis
All statistical analysis was done by the University of California, Los Angeles, statistics group. Plasma octreotide levels in this study were compared with those reported in previously published studies.1,3 Descriptive statistics were used to compare expected versus current plasma octreotide levels. In the case of LAR administered at a cumulative monthly dose of 120 mg/mo, we estimated plasma octreotide levels based on a multiple of previously published plasma levels for doses of 30 mg/mo (5000 pg/mL × 4) or 60 mg/mo (11,000 pg/mL × 2), respectively. We also compared the Woltering historic values with the data from the last 12 months of the current trial (May 2006–April 2007).1 The analysis was done using SAS PROC MIXED, a general mixed effects regression procedure that is able to handle the within-subject correlation in the data. The natural logarithm transformation was applied to the outcome variable to improve the distribution of the original data.8
Results
One hundred and sixty-two octreotide level determinations were performed in 86 patients from November 2004 until April 2007. These levels comprise the retrospective data analysis. During this time frame, 60 patients had multiple octreotide measurements performed. Thirty-three of these 60 patients' (55%) monthly LAR doses increased over time, none decreased, and 26 patients remained on the same dose of LAR during their entire clinical course. Of the 33 patients whose LAR dose increased over time, plasma octreotide levels decreased in 7, remained constant in 4, and increased in 22. However, these increases were significantly less than expected. In the 30 patients who were on 30 mg of LAR during the entire study, 7 of these patients (54%) exhibited decreasing octreotide plasma levels over time (mean decrease 43.6% ± 10.1%). Five patients were on LAR at monthly doses of 60 mg and remained on this dose during the entire study. Four of these 5 patients exhibited decreases in plasma octreotide levels over time (mean decrease 37.8% ± 11%).
Plasma octreotide levels were sorted by monthly LAR dose and reported over time (Tables 1–3). To facilitate detection of changes in the expected versus observed plasma octreotide levels, we reported mean plasma octreotide levels (±SD) by 3-month time frames and as 6-month averages (±SD) for patients receiving 30, 60, and 120 mg/mo of LAR. Expected octreotide levels for patients receiving 30 and 60 mg of LAR per month were determined from previously published reports.1,3 We anticipated that patients receiving LAR at doses of 120 mg/mo would have plasma levels twice those previously reported for 60 mg/mo (≈22,000 pg/mL) or 4 times those plasma levels reported for 30 mg/mo (≈20,000 pg/mL).
Table 1.
Mean Plasma Octreotide Blood Levels for 30 mg/mo LAR
| Historic Values | Retrospective Trial* | Prospective Trial* | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rubin et al3† | Woltering et al1‡ | 5502 ± 0 | 5609 ± 4763 | 3416 ± 1579 | 3318 ± 1865 | 2205 ± 1739 | 1996 ± 730 | ||||||
| 4247 ± 2733 | 5241 ± 3005 | n = 1 (6-mo values) | n = 18 (6-mo values) | n = 26 (6-mo values) | n = 27 (6-mo values) | n = 18 (6-mo values) | n = 8 (6-mo values) | ||||||
| n = 25§ | n = 19§ | NA§ | 5502 ± 0 | 4484 ± 1848 | 6042 ± 5502 | 2785 ± 798 | 4275 ± 1983 | 2881 ± 1761 | 3668 ± 1931 | 1695 ± 1542 | 2844 ±1857 | NA | NA |
| n = 1 | n = 5 | n = 13 | n = 15 | n = 11 | n = 12 | n = 15 | n = 10 | n = 8 | |||||
| Before June 1998 | Before August 2005 | November 2004– January 2005 |
February 2005– April 2005 |
May 2005– July 2005 |
August 2005– October 2005 |
November 2005– January 2006 |
February 2006– April 2006 |
May 2006– July 2006 |
August 2006– October 2006 |
November 2006– January 2007 |
February 2007– April 2007 |
January 2007– July 2007 |
|
This table shows the 6-month (top set of boxes) mean octreotide levels for patients receiving chronic octreotide LAR therapy at a dose of 30 mg/mo. The middle set of boxes represents the 3-month mean octreotide levels, and the lower set of boxes shows the 3-month time intervals used for data sorting. The 2 far left-hand columns represent the historic plasma octreotide level data reported by Rubin et al.3
Mean plasma octreotide levels ± SD in pg/mL. n = number of blood levels assayed.
Mean plasma octreotide levels reported by Rubin et al as pg/mL ± SD. n = number of blood levels assayed.
Mean plasma octreotide levels reported by Woltering et al as pg/mL ± SD. n = number of blood levels assayed.
NA indicates not applicable.
Table 3.
Mean Plasma Octreotide Blood Levels for 120 mg/mo LAR
| Retrospective Trial* | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| NA | 3499 ± 0 | 7418 ± 1663 | 8631 ± 4755 | 6354 ± 2097 | |||||
| n = 1 (6-mo values) | n = 3 (6-mo values) | n = 10 (6-mo values) | n = 4 (6-mo values) | ||||||
| NA | NA | NA | 3499 ± 0 | 7657 ± 0 | 7299 ± 2334 | 9527 ± 4943 | 8035 ± 4998 | 5333 ± 578 | 9419 ± 0 |
| n = 1 | n = 1 | n = 2 | n = 4 | n = 6 | n = 3 | n = 1 | |||
| November 2004– January 2005 |
February 2005– April 2005 |
May 2005– July 2005 |
August 2005– October 2005 |
November 2005– January 2006 |
February 2006– April 2006 |
May 2006– July 2006 |
August 2006– October 2006 |
November 2006– January 2007 |
February 2007– April 2007 |
This table shows the 6-month (top set of boxes) mean octreotide levels for patients receiving chronic octreotide LAR therapy at a dose of 120 mg/mo. The middle set of boxes represents the 3-month mean octreotide levels, and the lower set of boxes shows the 3-month time intervals used for data sorting. No historic data are available for comparison. To estimate an expected value for comparison purposes, we used a value of 4 times the 30-mg/mo plasma octreotide levels (4 × 5000 pg/mL = 20,000 pg/mL) or 2 times the 60-mg/mo LAR plasma levels (2 × 11,000 pg/mL = 22,000 pg/mL).
Mean plasma octreotide levels ± SD in pg/mL. n = number of blood levels assayed.
NA indicates not applicable.
In our patients treated with octreotide LAR at doses of 30 mg/mo, we expected plasma octreotide levels of 4200 to 5200 pg/mL based on 2 previously published reports.1,3 However, our most recent 6-month set of retrospective plasma octreotide determinations was 2205 ± 1793 pg/mL (n = 18) for the 30-mg/mo LAR doses (Table 1). This is a decrease of 48% to 58% over previously reported values. For the LAR dose of 30 mg/mo, the current plasma octreotide levels are significantly lower than the historic octreotide levels (P = 0.0067). The average plasma octreotide level in the most recent 12-month period is 49% lower than the historic values reported by Woltering et al.1 In contrast, patients who received 30 mg/mo of aqueous octreotide by continuous subcutaneous infusion achieved plasma octreotide levels of 5819 ± 3105 pg/mL. Thus, it seems that the use of subcutaneous infusions of octreotide can restore plasma octreotide levels in patients who cannot obtain or sustain high plasma octreotide values on the LAR preparation.
In comparison, patients receiving LAR at doses of 60 mg/mo have had previously reported plasma octreotide levels of approximately 11,000 pg/mL. In our current study, the most recent 6-month set of plasma octreotide values was 5792 ± 3166 pg/mL, a decrease from expected levels of approximately 50% (Table 2). For the LAR dose of 60 mg/mo, the average plasma octreotide level during the most recent 12-month period is 43% lower than the historic values (P = 0.0149).
Table 2.
Mean Plasma Octreotide Blood Levels for 60 mg/mo LAR
| Historic Values* | Retrospective Trial† | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Woltering et al1 | 12,506 ± 4142 | 5655 ± 1513 | 5184 ± 2017 | 6021 ± 3794 | 5792 ± 3166 | |||||
| 10,245 ± 5538 | n = 2 (6-mo values) | n = 2 (6-mo values) | n = 14 (6-mo values) | n = 20 (6-mo values) | n = 16 (6-mo values) | |||||
| n = 11 | 12,506 ± 4142 | NA | 6725 ± 0 | 4585 ± 0 | 4299 ± 1226 | 6069 ± 2341 | 5312 ± 1721 | 6729 ± 5131 | 5760 ± 3417 | 5889 ± 2695 |
| n = 2 | n = 1 | n = 1 | n = 7 | n = 7 | n = 10 | n = 10 | n = 12 | n = 4 | ||
| Before August 2005 | November 2004– January 2005 |
February 2005– April 2005 |
May 2005– July 2005 |
August 2005– October 2005 |
November 2005– January 2006 |
February 2006– April 2006 |
May 2006– July 2006 |
August 2006– October 2006 |
November 2006– January 2007 |
February 2007– April 2007 |
This table shows the 6-month (top set of boxes) mean octreotide levels for patients receiving chronic octreotide LAR therapy at a dose of 60 mg/mo. The middle set of boxes represents the 3-month mean octreotide levels, and the lower set of boxes show the 3-month time intervals used for data sorting. The far left-hand column represents the historic plasma octreotide level data reported by Woltering et al.1
Mean plasma octreotide levels reported by Woltering et al as pg/mL ± SD. n = number of blood levels assayed.
Mean plasma octreotide levels in pg/mL ± SD. n = number of blood levels assayed.
NA indicates not applicable.
We predicted that patients receiving LAR at doses of 120 mg/mo would have plasma levels of 20,000 to 22,000 pg/mL. However, in the most recent 6-month period, we observed plasma octreotide levels of 6354 ± 2097 pg/mL, a decrease in observed versus expected of 67% to 70% (Table 3).
Discussion
This study was prompted by an apparent increase in the number of patients who had been clinically and biochemically stable for months or years, suddenly complaining that their symptoms of flushing, diarrhea, or wheezing were worsening in spite of stable or increasing LAR dosing. These acute changes in clinical symptoms prompted a review of their plasma octreotide levels over time. Previous work has demonstrated that monthly LAR doses of 10 mg/mo led to plasma levels of approximately 1200 pg/mL (levels that approximate the Kd of octreotide for sst 2), whereas doses of 20, 30, and 60 mg/mo led to plasma levels of approximately 2500, 5000, and 11,000 pg/mL, respectively.1–3 Extrapolating from the previously published data, we would predict that doses of 120 mg of LAR per month would have yielded plasma octreotide values of 20,000 to 22,000 pg/mL. In stark contrast, current dosing of LAR at 30, 60, or 120 mg/mo in patients with carcinoid tumors produces significantly lower plasma levels of 2500, 5000, and 7500 pg/mL, respectively, a decrease over previously reported or expected levels of 50% or more.
Several possibilities exist that may explain why we are currently observing lower octreotide plasma levels in patients receiving chronic LAR therapy than previously described. First, with chronic LAR therapy, there may be the development of antibodies to octreotide. The development of these antibodies might interfere with the accurate measurement of octreotide in plasma. Although these antibodies have never been reported with the LAR formulation, anti-octreotide antibodies have been demonstrated in patients receiving chronic octreotide acetate therapy by subcutaneous administration or by transnasal administration.7 Although these antibodies are present in up to 75% of patients receiving long-term octreotide therapy by subcutaneous administration, we have not seen a time-dependent decrease in plasma levels in patients treated with subcutaneous therapy by multiple daily injection or continuous subcutaneous infusion (data not shown). However, we have switched LAR patients who failed to achieve high (greater than 10,000 pg/mL) plasma octreotide levels to continuous subcutaneous infusion octreotide therapy to determine if this change in the route of administration and the change in the formulation would increase plasma levels and improve control of symptoms. We hypothesized that if antibodies were responsible for the acute lowering of plasma octreotide levels, switching the route of administration would not change plasma levels. For example, a 65-year-old woman with metastatic carcinoid and the carcinoid syndrome had been under excellent symptom control for several years on octreotide LAR at a monthly dose of 30 mg/mo. Her concomitant octreotide plasma level was 4035 pg/mL, a value within our previously reported range of plasma octreotide levels in patients receiving 30 mg/mo of LAR. An increase in flushing and a slight increase in her chromogranin A and pancreastatin values prompted an increase in her octreotide dose to 60 mg of LAR per month. After 3 months of LAR therapy at this dose, her octreotide level dropped to 3837 pg/mL. Her flushing and fatigue continued to increase, and her LAR dose was again increased to 120 mg/mo. After 3 months on this high drug dose, her plasma octreotide level rose to only 5581 pg/mL, a level far less than we would have expected on this LAR dose. Her symptoms continued to increase and her biomarkers also increased significantly. Based on our inability to achieve octreotide values greater than 10,000 pg/mL on this very high (120 mg/mo) dose of LAR, we decided to begin octreotide acetate therapy by continuous subcutaneous administration at a dose of 2 mg/d (60 mg/mo). In spite of her receiving only half of the monthly octreotide dose (as compared with her LAR therapy), her plasma octreotide level rose to 25,436 pg/mL after 1 week of infusional therapy and remained more than 15,000 pg/mL even 3 months after the discontinuation of the LAR preparation. She was asymptomatic after starting the octreotide by continuous subcutaneous infusion and has remained totally asymptomatic on this subcutaneous drug dose.
Second, all of these patients receive LAR as intramuscular injections in the upper outer quadrants of their buttocks. Repeated injections into these sites may be responsible for progressively lower effectiveness of the drug because there is a well-described association between these injections and the development of a granulomatous reaction in the gluteus muscle. Although we believe this to be possible in an occasional patient, we do not believe that the magnitude of the clinical observations presented here are compatible with this possible explanation. Furthermore, patients who only recently started LAR have plasma levels of octreotide consistent with patients on identical chronic dosing and have levels far lower than those seen in the past with identical LAR doses.
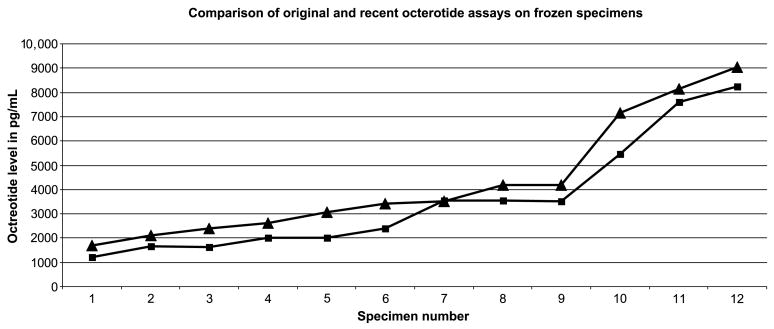
Third, there could be changes in the octreotide radio-immunoassay over time. To ensure that changes in plasma octreotide values over time were due to actual differences in plasma levels and not to differences in the octreotide assay values reported over time, several experiments were performed. Plasma samples from patients previously reported were reassayed for this study by Inter Sciences Institute.1 Octreotide plasma levels reported from assays performed 3 years ago were essentially identical to current reassay values (Fig. 1). These data demonstrate the resistance of octreotide to degradation, even when stored in plasma at −80°C for 3 years. In addition, low, intermediate, and high control standards for each octreotide assay done over the last 3 years were plotted against one another. This comparison showed that over time, low, intermediate, and high octreotide standards produced essentially identical octreotide values over time (data not shown). Thus, we believe that the current report of a reduction in plasma octreotide levels in patients given LAR represents true changes in plasma drug levels rather than changes in the assay measurement of plasma octreotide levels (Fig. 1). These significantly decreased plasma drug levels imply that the bioavailability of LAR must have decreased significantly over time. This is supported by the ability to restore desirable levels of octreotide with continuous subcutaneous infusions of octreotide.
Figure 1.
This figure demonstrates the stability of the octreotide assay over time. The 2 curves represent plasma octreotide values (sorted in ascending order) for individual samples assayed at the time of the Woltering octreotide study (triangles) and reassayed for the current study (squares).1 These 2 sets of assays are not statistically different, indicating the stability of the plasma octreotide assay over time.
Hypothetically, there may have been an unanticipated change in the drug formulation or its preparation that has been introduced into the LAR manufacturing process. Traditionally, the polymer for this drug encapsulates the octreotide into microspheres. The range of the size of the microspheres is carefully controlled; however, within the range of the microsphere's acceptable diameter, there could be a significant change in size distribution. This could alter the rate of drug release. Alternatively, the thickness of the microsphere's polymer coating could change, significantly altering the drug release characteristics of the LAR preparations.
Based on our tracking of plasma octreotide levels over time in both individual patients and in groups of patients receiving LAR at a given dose per month, it seems that the bioavailability of octreotide LAR has dramatically decreased over time. This may explain the perceived increase in subcutaneous octreotide rescue medication usage that prompted this study. In the drug registration trial for octreotide LAR in carcinoids, approximately 40% of patients used rescue medication on a frequent basis and 70% of patients in the study used rescue at some point during the study.3 Early in our clinical experience with octreotide level measurement, we noticed that patients who had increasing symptoms also had significant decreases in their octreotide plasma levels. Approximately one half of the plasma octreotide levels previously achieved at monthly LAR doses of 30 or 60 mg of LAR per month are now present in our patient population. Even higher monthly doses of LAR (120 mg/mo) show even greater differences between measured and expected octreotide levels. Traditionally, LAR was reported to be 61% bioavailable (drug information insert, Novartis); however, that number no longer seems to be accurate and the bioavailability seems to be in the range of 25% to 30%. To determine if this conclusion was reasonable, we compared the plasma octreotide levels of patients receiving LAR at a dose of 30 mg/mo in the 2 historic studies to the plasma levels seen in patients receiving aqueous octreotide by continuous subcutaneous infusion (n = 15). The mean plasma octreotide level was 5819 ± 3105 pg/mL for patients receiving 30 mg/mo of octreotide by continuous subcutaneous infusion (normalized data). This value is higher than those reported in the Rubin or Woltering studies, no doubt due to the greater bioavailability of subcutaneously administered octreotide.1,3 When we compared the plasma octreotide levels of the patients receiving subcutaneous infusions of octreotide to our more recent retrospective LAR trial values (January 2007–July 2007) or the prospective LAR trial, the decreased plasma octreotide values produced by the current LAR formulation are even more dramatic (Table 4).
Table 4.
Comparison of Plasma Octreotide Levels Achieved by 30-mg/mo Doses of Octreotide LAR and by Continuous Subcutaneous Infusion
| Data source | Rubin et al3—historic LAR at 30 mg/mo | Woltering et al1—historic LAR at 30 mg/mo | Current—retrospective LAR trial | Current—prospective LAR trial | Current—prospective octreotide infusion trial |
|---|---|---|---|---|---|
| Dates of study | Before June 1998 | Before June 2005 | January 2007–July 2007 | January 2007–July 2007 | January 2007–July 2007 |
| N | 25 | 19 | 18 | 8 | 15 |
| Mean trough plasma octreotide levels ± SD | 4247 ± 2733 | 5241 ± 3005 | 2205 ± 1739 | 1996 ± 730 | 5819 ± 3105 |
Clearly, the simplest approach to increasing circulating plasma octreotide levels is to increase the monthly dose of LAR. However, there are several potential reasons not to do this. Toxicity at doses higher than previously reported might be significant, and the expense of extremely high-dose LAR therapy might be cost prohibitive. In our clinical experience, the use of doses of LAR higher than those recommended by the Food and Drug Administration (30 mg/mo) seems to be extremely well tolerated. We have not been able to demonstrate any significant toxicity even when LAR doses of up to 240 mg/mo have been used for longer than 6 months. However, the economic impact of long-term high-dose LAR therapy is substantial.
The data from this study were reviewed to look for individual patient (as compared with group) changes in plasma octreotide levels over time. In patients receiving stable (3 months or longer) LAR doses of 30 mg/mo, 9 of 26 patients had decreases in plasma octreotide levels over time. The mean decrease in drug level was 2165 pg/mL from the first to the last plasma octreotide measurement. In contrast, 7 of 13 patients on stable 60-mg/mo doses of LAR had decreases in plasma octreotide levels over time. The mean decrease in plasma octreotide levels in the 60-mg/mo group was 2495 pg/mL from the first to the last plasma measurement. Finally, 1 of 5 patients on stable 120-mg/mo LAR dose had decreases measured over time. The decrease in plasma octreotide levels in this patient was 2971 pg/mL.
These changes are potentially time dependent. If a patient was on LAR at a dose of 30 mg/mo at the beginning of the study (November 2004) and remained on this dose over time, one might suspect that a drop in plasma octreotide level would be more likely than in a patient who was put on LAR 30 mg/mo during the last 4 months of this study. Unfortunately, fewer octreotide measurements were performed in the early part of the study when the octreotide assay was first offered on a commercial basis. Plasma octreotide levels seemed to fall in late 2005 to early 2006, and those patients who entered the study after that time would be exposed to the conditions that favored lower (but relatively stable during the last 6 months of the study) plasma drug levels.
In conclusion, we have observed that in current studies of octreotide LAR therapy produce plasma octreotide values significantly lower than previously reported.1,3 In addition, the octreotide plasma values have decreased by approximately 29% per year during the last several years. We suggest that patients with progressive symptoms, rising biomarkers or progressive growth of tumors on radiographs should have their octreotide values measured. Patients in whom plasma octreotide levels are less than 10,000 pg/mL should have their LAR dose adjusted, based on serial plasma octreotide determinations. If octreotide levels of 10,000 to 15,000 pg/mL cannot be achieved over time with higher LAR doses, clinicians should consider switching these patients to intermittent dose or continuous subcutaneous infusion octreotide therapy. Clinicians should also be cognizant of the costs associated with high-dose LAR therapy. Subcutaneous octreotide therapy may be a cost-effective alternative in this patient population. Alternatively, lanreotide, a somatostatin receptor subtype 2–preferring somatostatin analog has recently been approved for use in the United States for the treatment of acromegaly. It may be possible to use this medication for the control of symptoms of NETS as out of indication therapy.
References
- 1.Woltering EA, Mamikunian PM, Zietz S, et al. Effect of octreotide LAR dose and weight on octreotide blood levels in patients with neuroendocrine tumors. Pancreas. 2005;31:392–400. doi: 10.1097/01.mpa.0000186249.89081.0d. [DOI] [PubMed] [Google Scholar]
- 2.Harris AG, O'Dorisio TM, Woltering EA, et al. Consensus statement: octreotide dose titration in secretory diarrhea. Management Consensus Development Panel. Dig Dis Sci. 1995;40:1464–1473. doi: 10.1007/BF02285194. [DOI] [PubMed] [Google Scholar]
- 3.Rubin J, Ajani J, Schirmer W, et al. Octreotide acetate long-acting formulation versus open-label subcutaneous octreotide acetate in malignant carcinoid syndrome. J Clin Oncol. 1999;17:600–606. doi: 10.1200/JCO.1999.17.2.600. [DOI] [PubMed] [Google Scholar]
- 4.Weckbecker G, Liu R, Tolcsvai L, et al. Antiproliferative effects of the somatostatin analogue octreotide (SMS 201-995) on ZR-75-1 human breast cancer cells in vivo and in vitro. Cancer Res. 1992;52:4973–4978. [PubMed] [Google Scholar]
- 5.O'Dorisio MS, Chen F, O'Dorisio TM, et al. Characterization of somatostatin receptors on human neuroblastoma tumors. Cell Growth Differ. 1994;5:1–8. [PubMed] [Google Scholar]
- 6.Bertherat J, Chanson P, Dewailly D, et al. Somatostatin receptors, adenylate cyclase activity, and growth hormone (GH) response to octreotide in GH-secreting adenomas. J Clin Endocrinol Metabol. 1993;77:1577–1583. doi: 10.1210/jcem.77.6.7903312. [DOI] [PubMed] [Google Scholar]
- 7.Anthony LB, Stafford S, Cronin M, et al. Octreotide LAR doses used in clinical practice: results from an internet survey and a clinical practice. Proc Am Soc Clin Oncol. 2004;23:4274. [Google Scholar]
- 8.Littell R, Milliken G, Stroup W, et al. SAS System for Mixed Models. Cary, NC: SAS Press; 1996. [Google Scholar]