Abstract
A technique using a posteriorly based dermoglandular flap as an augmentation of the superior hemisphere of the breast combined with a periareolar mastopexy and vertical mastopexy is presented. The advantages of combining a periareolar mastopexy, in terms of reducing the length of the vertical scar and preventing areolar distortion, are explained.
Keywords: Augmentation, Mastopexy, Periareolar, Ptosis, Vertical
Abstract
On présente ici une technique qui repose sur l’utilisation d’un lambeau dermoglandulaire postérieur pour l’augmentation de l’hémisphère supérieur du sein, combinée à une mastopexie périaréolaire et à une mastopexie verticale. On explique les avantages de combiner une mastopexie périaérolaire, qui permet de réduire la longueur de la cicatrice verticale et de prévenir la distorsion de l’aréole.
ANATOMY
The nipple of the ideal prepartum breast is positioned 5 cm to 7 cm above the inframammary crease (IMC). There is an obtuse angle between the breast and the abdomen. The first sign of breast ptosis is descent of the gland so that it rests on the abdominal wall. The causes of breast ptosis are development, weight loss and, more commonly, pregnancy and breast-feeding. It is caused by stretching of the internal ligaments and the skin envelope.
Using the inferior portion of the breast has been previously described by Graf et al (1) using a weaving technique through the pectoralis major muscle. The technique of using a posterior parenchymal pedicle as an autoaugmentation combined with a vertical mastopexy has also been described by Botti (2). In that technique, the periareolar skin excision was designed according to the Lejour (3) pattern. The technique described in the present paper differs, using a periareolar mastopexy so that the vertical excess can be captured in the larger periareolar skin excision, limiting the vertical skin excision. In addition, the periareolar suture stabilizes the circular shape of the areola, thereby preventing areolar distortion and traction into the vertical closure, and avoiding tension and compromised vascularity of the areola.
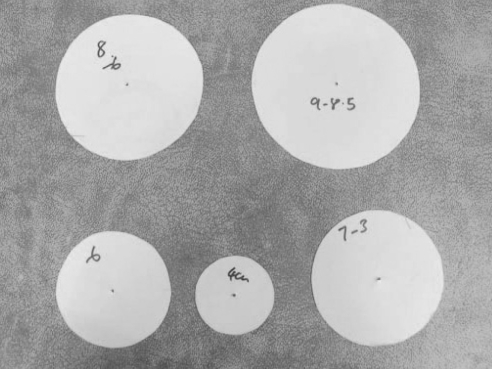
The circumference of the periareolar skin is roughly equal to three times the diameter (eg, if the diameter of the areola is 8 cm then the circumference is 24 cm). For an ideal diameter of 4 cm, the new areolar circumference is 12 cm. If the horizontal elliptical excision in the inferior portion of the breast removes 6 cm to 8 cm of the inferior portion of the periareolar skin excision (Figure 1), then the resulting circumference will be 16 cm to 18 cm, which is equivalent to a diameter of 5 cm to 6 cm when the defect is closed. With the addition of a permanent purse-string suture, the size disparity is accommodated with minimal bunching of the periareolar skin. The only patterns used by the author are a series of circular ones measuring 4 cm, 6 cm, 8 cm and 9 cm (Figure 2)
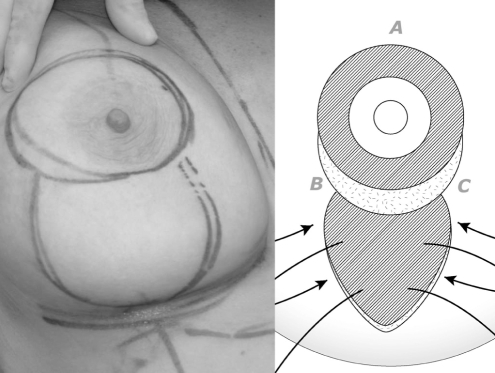
Figure 1).
Diagrammatic representation of vertical mastopexy combined with periareolar skin excision
Figure 2).
Patterns for marking periareolar skin excision
TECHNIQUE
The patient should be standing with the arms at the side. A line is drawn from the suprasternal notch (SSN) to the xiphoid in the midline, and the IMC is outlined. The midline of the breast is marked usually from a point midway between the SSN and the acromioclavicular joint, or approximately 8 cm lateral to the SSN. This line is continued inferiorly across the IMC line.
The postoperative level of the areola is determined by grasping the skin at three o’clock and nine o’clock, transposing the areola to the middle of the breast mound until the inferior mammary skin is taut. A mark is made at the superior point of the transposed areola on the superior skin of the breast. The new nipple-areolar complex (NAC) location is confirmed by measuring the acromio-olecranon distance and then dividing it in half, placing the nipple at a point 4 cm below the midpoint (4). The new position is further checked by evaluating its relationship to the IMC and by measuring the distance from the SSN to the superior point of the neoareola, which should be 15 cm to 17 cm. The new location is visually evaluated as a final check.
The same point is transposed to the midline of the opposite breast using a gynecological caliper, placing one limb at the SSN and the other at the site of the superior point of the neoareola (Figure 1, point A).
A circle, usually 6 cm to 8 cm in diameter, is drawn using a precut pattern (Figure 2), with the superior point of the circle at point A and the inferior portion usually, but not always, at the lower edge of the areola. To confirm that the circles are symmetrical, the distance from the medial aspect of the circle to the midline is measured. If medial and lateral skin laxity is limited, an ellipse rather than a circle is drawn, with the margins abutting the edges of the areola.
The amount of skin excision of the lower breast is evaluated by pinching the skin, as well as by rotating the breast clockwise and counterclockwise, and marking vertical limbs that meet in the midline approximately 2 cm above the IMC. This is performed with the patient’s hands on top the head (Figure 3).
Figure 3).
The amount of skin excision of the lower breast is evaluated, and vertical lines that meet in the midline about 2 cm above the infra-mammary crease are marked. This is performed with the patient’s hands on top the head
Surgery is usually performed under general anesthesia to avoid extensive infiltration of the breast, which may affect intraoperative evaluation of size and shape.
The patient is placed on an operating table that is capable of elevation of the back to a full 90°. The arms are placed at 90°, wrapped to the arm boards. The back is flexed at approximately 30° at the start of the procedure.
The procedure is begun with circumcision of the areola using a 38 mm ‘cookie-cutter’, with the breast supported laterally in a relaxed position. The ideal diameter is 40 mm, so the author often cuts around the outside of the mark, because a 40 mm pattern is currently unavailable.
The remainder of the pattern is then de-epithelialized. Using the cutting cautery, a vertical incision is made at the medial aspect of the lower breast marking, inferior to the areola, down to the underlying deep fascia. A further incision is made in an oblique direction at the lateral edge of the inferior ellipse laterally to preserve the blood supply to the inferior gland. The skin at the inferior portion of the marking is undermined to the IMC, leaving a thin layer of subcutaneous fat measuring approximately 3 mm. Superiorly, the cut extends across the inferior edge of the areola, leaving a 2 cm cuff inferior to the areolar margin.
The incision is then deepened down to the underlying deep fascia deep to the areolar complex, and the superior breast is partially undermined in the retromammary space in a medial superior direction.
The NAC is mobilized on a superior pedicle by making two vertical incisions extending to the superior edge of the deepithialized skin, leaving an intact pedicle between 10 o’clock and two o’clock superiorly. The pedicle thickness is at least 2 cm. Undermining is kept to a minimum to achieve mobilization of the NAC. Once the NAC is mobilized, a 4-0 monofilament glycomer suture is place at the 12 o’clock position, fixing the NAC in its new position.
The inferior gland is then transposed deep to the NAC and sutured with one or two 2-0 monofilament polyglyconate sutures to the deep fascia in the medial superior portion of the breast at about the level of the third intercostal space.
Once this is completed, the wound is irrigated with antibiotic-containing solution and hemostasis is obtained. A 3-0 monofilament polyglyconate suture is then placed at the superior limbs of the inferior epithelialized part (Figure 1, points B and C).
If there is insufficient tension, the suture can be placed more laterally and medially along the circumference of the periareolar skin excision.
Once the stitch is placed, a skin hook is positioned at the superior pole, and the inferior limbs are closed from the bottom up with 3-0 monofilament polyglyconate suture to the dermis or, alternatively, 3-0 nylon sutures to tailor-tack (Figure 4). Once tailor-tacking is completed, three horizontal marks are drawn across the inferior limb and numbered. The sutures are then removed from above downwards, the redundant skin is excised with a number 10 blade and dermal sutures of 3-0 monofilament polyglyconate are placed. When the inferior portion is reached, the dog-ear is excised in a vertical, a ‘J’ or an ‘L’ shape with the limb coursing laterally, or occasionally with a short horizontal scar.
Figure 4).
Elevation of apex of vertical closure
The dog-ear excision is performed last, after closure of the NAC.
The NAC is closed with eight interrupted 4-0 monofilament glycomer sutures spaced evenly around the circumference of the areola. A 3-0 polyester suture SH taper needle is placed around the NAC and tied in the mid-lateral position around a 38 mm cookie cutter. The knot is soaked in povidone iodine before cutting. Final closure is performed with further interrupted 4-0 monofilament glycomer sutures to bury the purse-string knot and then finally with a subcuticular suture of the same material.
The inferior limb is closed with deep 3-0 monofilament polyglyconate suture followed by interrupted and subcuticular 4-0 monofilament glycomer sutures. It is vital that this last suture begins or ends at least 1 cm below the point at which the inferior limb meets the areola margin so as to avoid distortion of the areola as it is tightened when shortening the distance of the vertical limb. Before this last suture is placed, final trimming of the inferior dog-ear is performed. The dog-ear may be left until the opposite breast is closed; then, final adjustment can be performed on both breasts at the end of the procedure.
The final shaping and closure of the breast following the suture of the gland in the retromammary space is performed with the patient in the seated position at 60° to 90° of elevation, blood pressure permitting. No drains are used.
RESULTS
Twenty-five patients have been treated with this technique in the past 44 months. Of these, 24 underwent mastopexy only. One patient (Figure 5) had removal of implants and reconstruction with autoaugmentation. Two patients had a revision of the procedure because of inadequate elevation of the NAC, inadequate reduction of the NAC or inadequate elevation of the transposed gland (Figure 6). One patient is scheduled for a revision because of an inadequate lift. No patient complained of a hypertrophic scar. One patient lost 40 pounds after surgery and subsequently had a submuscular breast augmentation. No patient had a partial or complete loss of the NAC. The periareolar mastopexy has been combined with a vertical mastopexy in case of breast reduction, replacement of breast implants and breast augmentation or reduction. Two patients had a prior breast reduction – one with an inferior pedicle technique and one with free nipple graft. Representative cases are shown (Figures 7 and 8).
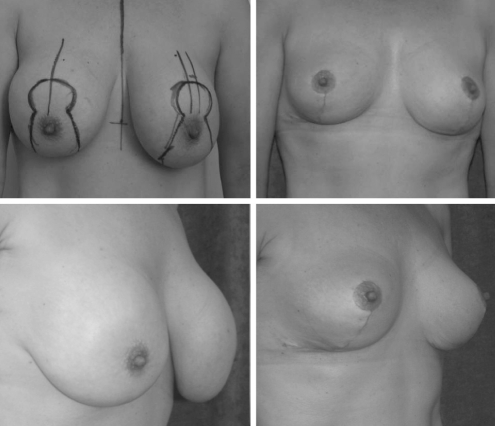
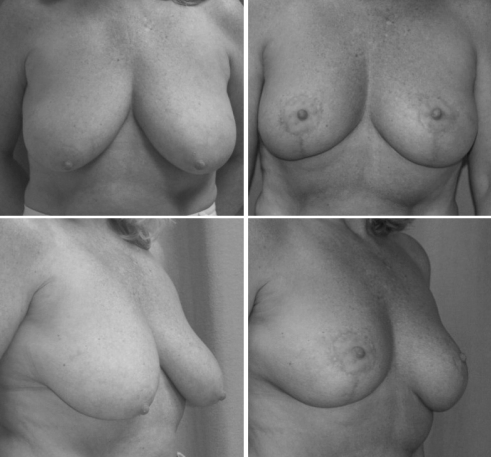
Figure 5).
Removal of implant and breast autoaugmentation using residual inferior glandular flap: frontal view (top) and oblique view (bottom)
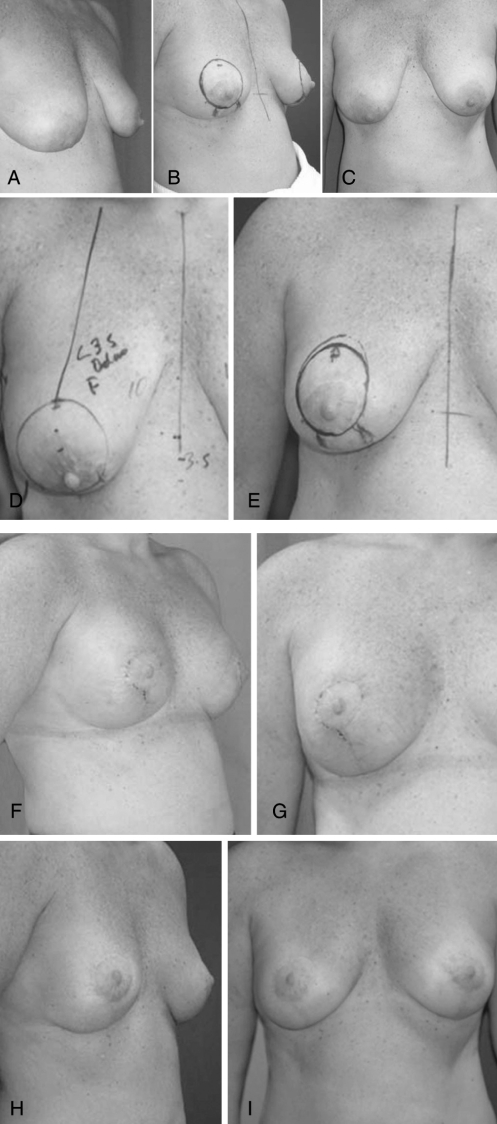
Figure 6).
Patient who underwent revision of autoaugmentation due to inadequate lift: A oblique view, before first surgery; B oblique view, before second surgery; C frontal view, before first surgery; D frontal view, before first surgery (with marking); E frontal view, before second surgery (with marking). The same patient at six-week (F, G) and one-year (H, I) follow-up visits
Figure 7).
Autoaugmentation. Frontal and oblique views of the patient before surgery (left) and at the six-month follow-up visit (right)
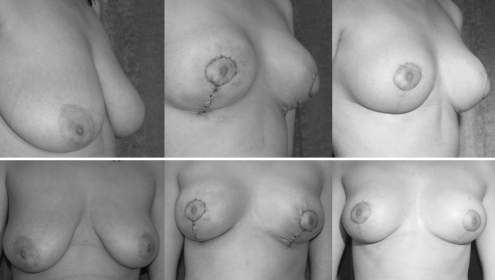
Figure 8).
Autoaugmentation. Frontal and oblique views of the patient before surgery (left), immediately postoperatively (middle) and at the six month follow-up visit (right)
DISCUSSION
This technique addresses the empty upper pole of the ptotic breast and gives the appearance of an augmented breast, hence the term ‘autoaugmentation’. Preoperative marking is simple and can be modified at the time of surgery. The use of a permanent purse-string suture combined with a periareolar mastopexy stabilizes the shape of the areola, thus reducing the possibility of areola ‘creep’ with a vertical elliptical instead of a circular shape. In addition, the circumareolar suture prevents tension and compromised vascularity of the areola. Periareolar skin excision shortens the vertical limb of the pattern, helping to reduce the length of the vertical scar.
Footnotes
NOTE: Presented in part as Lollipop Mastopexy at the 13th International Congress, International Confederation for Plastic, Reconstructive and Aesthetic Surgery, Sydney, Australia, August 14, 2003.
REFERENCES
- 1.Graf R, Reis de Araujo LR, Rippel R, Neto LG, Pace DT, Biggs T. Reduction mammaplasty and mastopexy using the vertical scar and thoracic wall flap technique. Aesthetic Plast Surg. 2003;27:6–12. doi: 10.1007/s00266-002-0111-5. [DOI] [PubMed] [Google Scholar]
- 2.Botti G. Vertical scar mammaplasty: Stable padding of the superior pole by means of posteriorly based pedicle autoprosthesis. Aesthetic Surg J. 1999;19:116–23. [Google Scholar]
- 3.Lejour M. Vertical mammaplasty: Early complications after 250 personal consecutive cases. Plast Reconstr Surg. 1999;104:764–70. doi: 10.1097/00006534-199909030-00023. [DOI] [PubMed] [Google Scholar]
- 4.Lassus C. A 30-year experience with vertical mammaplasty. Plast Reconstr Surg. 1996;97:373–80. doi: 10.1097/00006534-199602000-00015. [DOI] [PubMed] [Google Scholar]