Abstract
AIM: To evaluate the influence of preoperative biliary drainage on morbidity and mortality after surgical resection for ampullary carcinoma.
METHODS: We analyzed retrospectively data for 82 patients who underwent potentially curative surgery for ampullary carcinoma between September 1993 and July 2007 at the Singapore General Hospital, a tertiary referral hospital. Diagnosis of ampullary carcinoma was confirmed histologically. Thirty-five patients underwent preoperative biliary drainage (PBD group), and 47 were not drained (non-PBD group). The mode of biliary drainage was endoscopic retrograde cholangiopancreatography (n = 33) or percutaneous biliary drainage (n = 2). The following parameters were analyzed: wound infection, intra-abdominal abscess, intra-abdominal or gastrointestinal bleeding, septicemia, biliary or pancreatic leakage, pancreatitis, gastroparesis, and re-operation rate. Mortality was assessed at 30 d (hospital mortality) and also long-term. The statistical endpoint of this study was patient survival after surgery.
RESULTS: The groups were well matched for demographic criteria, clinical presentation and operative characteristics, except for lower hemoglobin in the non-PBD group (10.9 ± 1.6 vs 11.8 ± 1.6 in the PBD group). Of the parameters assessing postoperative morbidity, incidence of wound infection was significantly less in the PBD than the non-PBD group [1 (2.9%) vs 12 (25.5%)]. However, the rest of the parameters did not differ significantly between the groups, i.e. sepsis [10 (28.6%) vs 14 (29.8%)], intra-abdominal bleeding [1 (2.9%) vs 5 (10.6%)], intra-abdominal abscess [1 (2.9%) vs 8 (17%)], gastrointestinal bleeding [3 (8.6%) vs 5 (10.6%)], pancreatic leakage [2 (5.7%) vs 3 (6.4%)], biliary leakage [2 (5.7%) vs 3 (6.4%)], pancreatitis [2 (5.7%) vs 2 (4.3%)], gastroparesis [6 (17.1%) vs 10 (21.3%)], need for blood transfusion [10 (28.6%) vs 17 (36.2%)] and re-operation rate [1 (2.9%) vs 5 (10.6%)]. There was no early mortality in either group. Median survival was 44 mo (95% CI: 34.2-53.8) in the PBD group and 41 mo (95% CI: 27.7-54.3; P = 0.86) in the non-PBD group.
CONCLUSION: Biliary drainage before surgery for ampullary cancer significantly reduced postoperative wound infection. Overall mortality was not influenced by preoperative drainage.
Keywords: Ampullary carcinoma, Preoperative biliary drainage, Postoperative complications
INTRODUCTION
In patients with ampullary cancer who undergo surgical resection, obstructive jaundice is associated with a higher risk of postoperative complications than in non-jaundiced patients[1]. The impact of jaundice on postoperative morbidity and mortality is well known. However the routine use of preoperative biliary drainage (PBD) remains controversial. The potential advantages of preoperative stenting include improved nutritional, metabolic and immune function and the possibility of reduced postoperative morbidity and mortality[1]. Opponents of PBD argue that it increases infective complications and morbidity[2,3]. However, there are certain clinical situations such as acute suppurative cholangitis and severe malnutrition in which urgent biliary drainage is indicated and can be life-saving[4]. It is not clear whether the procedure itself or its complications influence the morbidity after surgical resection. The optimal duration of preoperative drainage also remains unknown. Although several reports have been published, there are still no clear guidelines regarding the use of PBD in these patients. We analyzed our patients to assess the influence of PBD on postoperative outcome following pancreaticoduodenectomy (PD) for ampullary tumors.
MATERIALS AND METHODS
We reviewed retrospectively the records of all patients who underwent definitive surgery for carcinoma involving the ampulla of Vater between and September 1993 and July 2007 at the Singapore General Hospital, a tertiary care referral and teaching hospital.
Ampullary cancer was defined as a tumor arising from the ampulla, with evidence of invasion and histopathological signs of neoplasia. In the case of large tumors with involvement of adjacent duodenum or pancreas, the tumor was classified as ampullary if it was centered on the ampulla. Cancers of pancreatic, duodenal and choledochal origin were excluded.
Details of patients who underwent PD (Whipple’s operation) or pylorus-preserving pancreaticoduodenectomy (PPPD) for ampullary tumors were entered into a database that included patient characteristics, details of biliary stenting, procedure-related infective complications, surgery, morbidity and mortality. The operations were performed in the Department of Surgery, Singapore General Hospital.
Morbidity
Pancreatic leakage was diagnosed when > 50 mL of drainage fluid, with a serum amylase concentration > 3 times the upper limit of normal was obtained on or after postoperative day 5, or when pancreatic anastomotic disruption was demonstrated radiologically[3]. Wound infection was defined as spontaneous or surgically released purulent discharge that was positive for bacterial growth on culture. Bile leakage was defined as a bilirubin concentration in the drainage fluid that exceeded that in the serum, which resulted in a change of clinical management or the occurrence of a bilioma that required drainage. Infectious morbidity was defined as any complication with evidence of associated localized or systemic infection indicated by fever, leukocytosis and positive culture.
Intra-abdominal or gastrointestinal bleeding was defined as bleeding with either hemodynamic instability or patients who required > 2 U blood transfusion or who required re-operation. Intra-abdominal abscess was defined as purulent discharge with positive cultures from abdominal drains placed at surgery, or as fluid collection that required a drainage procedure. Delayed gastric emptying was defined as inability to tolerate a regular diet for more than seven postoperative days, the need for nasogastric tube drainage for seven or more days postoperatively, or the need for tube reinsertion after removal.
Mortality
Hospital deaths were defined as those that occurred within 30 d of operation or as a direct result of postoperative complications. Late mortality was defined as mortality after 30 d during the follow-up period.
Pathological data
Pathological data were obtained from the patients’ medical records and the surgical pathology files. Histological grade, type and the presence of malignant change were noted.
Statistical analysis
Results were expressed as medians and ranges or as numbers and percentages of patients. Two-tailed t test and χ2 test were used for data analysis. SPSS version 13.0 statistical software was used (Chicago, IL, USA) for analysis. Differences were considered statistically significant at P < 0.05. The major statistical endpoint of this study was patient survival. Event time distributions for this endpoint were estimated using the method of Kaplan and Meier[5] and compared using the log-rank statistic.
RESULTS
Eighty-two patients were included in the study. Seventy-nine had Whipple’s operation and three had PPPD for ampullary tumors. Forty patients (48.8%) were male and 42 (51.2%) were female. Thirty-five (42.7%) patients underwent preoperative biliary plastic stent insertion. There were no inherent differences between the two groups with regard to the decision to proceed with PBD stent insertion. Demographics of the 82 patients with ampullary cancer are summarized in Table 1. The two groups were comparable with regard to sex, age, stage and grading of the ampullary cancer, and diabetes mellitus. Patients who underwent PBD had a significantly higher level of hemoglobin (11.8 ± 1.5 g/dL) on preoperative laboratory evaluation compared with non-stented patients (10.9 ± 1.6 g/dL) (P < 0.05). The majority of biliary stents were placed endoscopically, with two patients having percutaneous transhepatic biliary drainage. Numbers were too small to undergo statistical analysis between the types of biliary decompression; thus, “stents” included all patients who underwent PBD. The time interval between biliary drainage and surgery was 39 d (range: 10-89 d). There was a decrease in bilirubin in all patients, with the mean reduction being 47.6 μmol/L. All patients were given intravenous antibiotics at the time of surgery.
Table 1.
Patient variables in the PBD and non-PBD groups
| PBD | Non-PBD | Significance | |
| Patients | 35 | 47 | |
| Median age (yr) | 65 (23-84) | 62 (38-84) | 0.91 |
| Sex ratio (M/F) | 14/21 | 26/21 | 0.28 |
| Mean serum bilirubin | 112.4 ± 116.1 | 91.6 ± 110.2 | 0.39 |
| Mean hemoglobin | 11.8 ± 1.5 | 10.9 ± 1.6 | 0.03 |
| Diabetes mellitus | 7 | 12 | 0.66 |
| Mean albumin | 30.5 ± 5.7 | 31.1 ± 6.2 | 0.77 |
All postoperative complications and subpopulation analyses between PBD and non-PBD groups are shown in Table 2. Postoperative sepsis occurred in 29.3% (24/82) of the patients. Six patients had postoperative bleeding that required re-exploration. There were 13 (15.7%) patients with wound infection (one in the PBD and 12 in the non-PBD group), and analysis demonstrated a significantly higher occurrence of wound infection in the non-PBD group (P = 0.01).
Table 2.
Morbidity and mortality in the two groups
| Morbidity | PBD | Non-PBD | Significance |
| Sepsis | 10 | 14 | 0.91 |
| Wound infection | 1 | 12 | 0.01 |
| Intra-abdominal bleeding | 1 | 5 | 0.36 |
| Intra-abdominal abscess | 1 | 8 | 0.09 |
| Gastrointestinal bleeding | 3 | 5 | 0.95 |
| Bile leakage | 2 | 3 | 0.73 |
| Pancreatic leakage | 2 | 2 | 0.73 |
| Delayed gastric emptying | 6 | 10 | 0.85 |
| Reoperation | 1 | 5 | 0.36 |
| Hospital death | 0 | 0 | 0.00 |
| Late mortality | 10 | 13 | 0.15 |
Tumor grading and histology
Of the 82 infiltrating carcinomas, 21 (25.6%) were well-differentiated, 49 (59.8%) were moderately differentiated, and 12 (14.6%) were poorly differentiated. The most common histological type was intestinal (52/82, 63.4%), followed by pancreaticobiliary (22/82, 26.8%) and colloid (3/82, 3.7%). Five carcinomas had a histological type that was classified as “other”.
Mortality and survival
There were no hospital deaths in either group. Twenty-three patients died (28%) during the study period. Median survival was 44 mo (95% CI: 34.2-53.8) in the PBD group and 41 mo (95% CI: 27.7-54.3; P = 0.86) in the non-PBD group. There was no significant difference in terms of survival between the groups (Figure 1).
Figure 1.
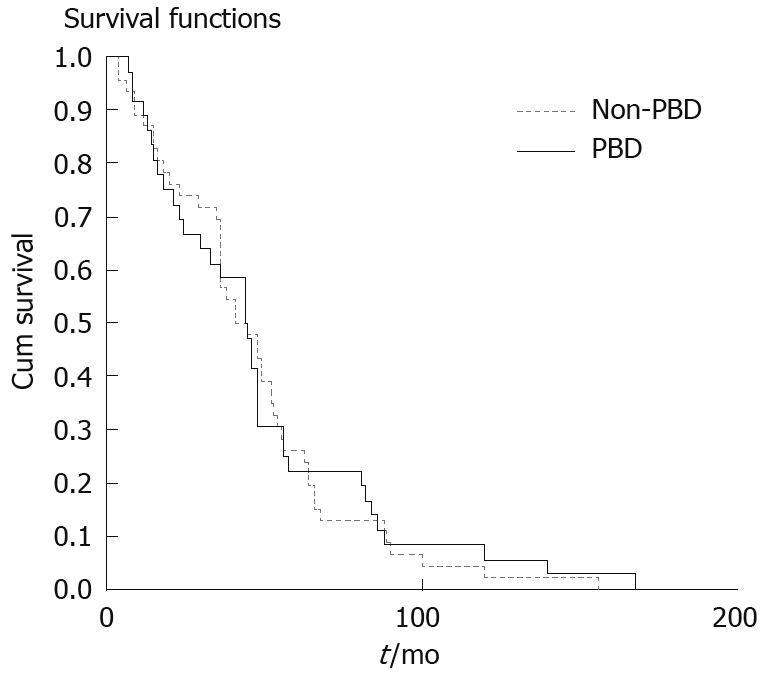
Survival functions for PBD and non-PBD groups.
DISCUSSION
Ampullary tumors share a similar clinical presentation in which jaundice is the predominant symptom. The main initial objectives in these patients are to obtain a precise diagnosis and resolution of jaundice. In an attempt to reach these goals, many treatment modalities have been proposed and applied in recent years. All have been oriented to the necessity of reducing jaundice preoperatively and to preventing perioperative complications, in most cases caused by cholestasis. We found an increase in the rate of wound infection in the perioperative period in the non-PBD group. Malnourishment and malignant obstructive jaundice predispose a patient to wound dehiscence by slowing healing, and increasing the rate of wound infection. A study by Irvin et al[6] has suggested that malignant disease may be an important factor in the pathogenesis of wound complications in patients with jaundice. Wound dehiscence or incisional hernia occurred in 59.1% of patients with obstructive jaundice that resulted from malignant disease, but patients with jaundice caused by biliary stones or benign pathology did not develop these complications.
Other factors have been confirmed as having a significant effect on the development of postoperative wound infection, in terms of patient characteristics including diabetes and anemia[7]. Patients with diabetes are more susceptible to wound infection because of impaired neutrophil chemotaxis and phagocytosis. In our series, 25% of non-PBD patients had diabetes compared to 20% in the PBD group, which, although not statistically significant, may have influenced the outcome of surgery. Furthermore the non-PBD group had a hemoglobin level that was significantly lower than that in the PBD group. Impaired wound healing in patients with obstructive jaundice has also been postulated to be caused by an altered immune response, with elevated tumor necrosis factor α activity secondary to circulating endotoxemia[8].
Grande et al[9] have compared wound healing in the presence and absence of obstructive jaundice. They used prolyl hydroxylase activity as a marker for collagen synthesis, and found it to be significantly elevated in patients who underwent biliary drainage for benign or malignant biliary obstruction. These patients had better wound healing.
Three common methods of PBD are percutaneous, endoscopic and surgical instrumentation. The endoscopic insertion of a stent through the papilla is a method of draining an obstructed biliary system during endoscopic retrograde cholangiopancreatography (ERCP). In animal studies comparing internal and external biliary drainage, animals undergoing internal drainage experienced increased survival[10,11], decreased sepsis[12], renal failure[11], and more rapid recovery of immune function[13,14], compared with those undergoing external drainage. Endoscopic biliary drainage is now considered an effective, if not the preferable, treatment for the palliation of malignant biliary tract obstruction[15,16].
To the best of our knowledge, this is the first study to analyze ampullary cancer in the context of PBD. Previous studies have looked at peri-ampullary cancer. Trede and Schwall’s[17] retrospective analysis of 150 patients with jaundice undergoing partial or total pancreatectomy revealed a complication rate of 31% and four deaths in 68 patients with no drainage, compared with 17% complications and one death in 82 patients with PBD. Evidence in support of preoperative biliary drainage comes from a prospective randomized trial by Lygidakis et al[18], which assigned 38 patients to either PBD (15 ± 2 d) by endoscopic internal stenting, or no PBD. The authors reported a 16% complication rate and no deaths in 19 patients undergoing PBD, compared with 70% complications and two deaths in 19 patients without drainage. Although this difference was highly significant, the investigators scored positive intraoperative blood and bile cultures as a complication. The clinical relevance of such findings is not clear. Smith et al[19] have identified prospectively 155 patients who underwent partial PD and found no survival difference between PBD and non-PBD groups. However, the authors concluded that the presence of jaundice at the time of resection had an adverse impact on early postoperative survival. Therefore, preoperative resolution of jaundice following biliary stenting predicted more favorable early survival outcome.
In contrast, a prospective randomized study by Lai et al[20] revealed no significant benefit in patients undergoing PBD, and included a wide variety of pathologies, but details of specific complications were not delineated clearly. Choi et al[21] have shown that PBD compromised hepatic excretory function, as represented by a slow rate of decrease in serum bilirubin. Limongelli et al[22] have revealed that PBD predisposes to a positive intraoperative bile culture, which increases the risk of developing infectious complications and wound infection after pancreatic surgery. Povoski et al[23] have reviewed retrospectively 240 consecutive cases of PD. Postoperative morbidity and mortality rates were higher in the PBD group, and they have suggested that PBD should be avoided whenever possible in patients with potentially resectable pancreatic and peripancreatic lesions. Therefore, based on data that, at best, provide mixed results, why should the patients still undergo PBD? First, most patients with ampullary cancer at the time of diagnosis have symptomatic jaundice with pruritus, and some degree of abdominal pain. To some extent, it is hoped that stenting will provide symptomatic improvement. Second, patients who present with acute cholangitis require prior PBD before undergoing definitive surgery.
In contrast, endoscopic biliary drainage before surgery is not a widely accepted procedure among pancreatic surgeons. Potential disadvantages of PBD include those inherent to ERCP such as pancreatitis, bleeding, cholangitis and duodenal perforation. In addition, endoscopic biliary stenting has been shown to generate a severe inflammatory reaction in the bile duct[24], which may make surgical resection more difficult. This was not substantiated by our study, with its comparable mortality and significantly reduced wound infection in the PBD group.
In conclusion, our experience confirms that PBD in patients with obstructive jaundice due to ampullary cancer results in a reduction in wound infection following surgical resection compared with patients not undergoing PBD. Morbidity other than wound infection and mortality were similar with or without PBD. We believe that a detailed prospective randomized trial including a cost analysis in a well-defined and well-matched group of patients undergoing operation for ampullary cancer is warranted, to further evaluate the effectiveness of routine preoperative PBD.
COMMENTS
Background
The effectiveness of preoperative biliary drainage (PBD) in pancreaticoduodenectomy is still extensively debated because of the various conflicting postoperative outcomes, which include benign or malignant, pancreatic or peripancreatic, and ampullary or periampullary lesions.
Research frontiers
The impact of jaundice on postoperative complications is well recognized. However, whether PBD with improvement of jaundice affects surgical outcomes remains controversial.
Innovations and breakthroughs
This is believed to be the first study to investigate the impact of PBD in resectable ampullary cancer patients. Other studies have shown mixed results with regard to postoperative morbidity and mortality amongst ampullary and periampullary cancer.
Applications
The authors conducted the study amongst 82 patients with ampullary cancer and 35 of them had PBD, with a significant reduction in postoperative wound infection rate. A further randomized prospective control study should be conducted in resectable ampullary cancer patients undergoing PBD to look into this positive outcome.
Peer review
This paper addresses an important clinical issue: whether preoperative biliary drainage influences the outcome of resectional surgery for ampullary carcinoma. The results are presented reasonably clearly. The discussion compares the outcomes of this study with other relevant studies and explores the possible reasons for the findings.
Peer reviewer: Michael A Fink, MBBS FRACS, Department of Surgery, The University of Melbourne, Austin Hospital, Melbourne, Victoria 3084, Australia
S- Editor Tian L L- Editor Kerr C E- Editor Lin YP
References
- 1.Gundry SR, Strodel WE, Knol JA, Eckhauser FE, Thompson NW. Efficacy of preoperative biliary tract decompression in patients with obstructive jaundice. Arch Surg. 1984;119:703–708. doi: 10.1001/archsurg.1984.01390180065011. [DOI] [PubMed] [Google Scholar]
- 2.Povoski SP, Karpeh MS Jr, Conlon KC, Blumgart LH, Brennan MF. Preoperative biliary drainage: impact on intraoperative bile cultures and infectious morbidity and mortality after pancreaticoduodenectomy. J Gastrointest Surg. 1999;3:496–505. doi: 10.1016/s1091-255x(99)80103-6. [DOI] [PubMed] [Google Scholar]
- 3.Sohn TA, Yeo CJ, Cameron JL, Pitt HA, Lillemoe KD. Do preoperative biliary stents increase postpancreaticoduodenectomy complications? J Gastrointest Surg. 2000;4:258–267; discussion 267-268. doi: 10.1016/s1091-255x(00)80074-8. [DOI] [PubMed] [Google Scholar]
- 4.Kumar R, Sharma BC, Singh J, Sarin SK. Endoscopic biliary drainage for severe acute cholangitis in biliary obstruction as a result of malignant and benign diseases. J Gastroenterol Hepatol. 2004;19:994–997. doi: 10.1111/j.1440-1746.2004.03415.x. [DOI] [PubMed] [Google Scholar]
- 5.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [Google Scholar]
- 6.Irvin TT, Vassilakis JS, Chattopadhyay DK, Greaney MG. Abdominal wound healing in jaundiced patients. Br J Surg. 1978;65:521–522. doi: 10.1002/bjs.1800650722. [DOI] [PubMed] [Google Scholar]
- 7.Lilienfeld DE, Vlahov D, Tenney JH, McLaughlin JS. Obesity and diabetes as risk factors for postoperative wound infections after cardiac surgery. Am J Infect Control. 1988;16:3–6. doi: 10.1016/0196-6553(88)90003-x. [DOI] [PubMed] [Google Scholar]
- 8.Dawiskiba J, Kwiatkowska D, Zimecki M, Kornafel P, Tyran W, Czapińska E, Woźniak Z. The impairment of wound healing process is correlated with abnormalities of TNF-alpha production by peritoneal exudate cells in obstructive jaundiced rats. HPB Surg. 2000;11:311–318. doi: 10.1155/2000/82905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grande L, Garcia-Valdecasas JC, Fuster J, Visa J, Pera C. Obstructive jaundice and wound healing. Br J Surg. 1990;77:440–442. doi: 10.1002/bjs.1800770426. [DOI] [PubMed] [Google Scholar]
- 10.Gouma DJ, Coelho JC, Schlegel JF, Li YF, Moody FG. The effect of preoperative internal and external biliary drainage on mortality of jaundiced rats. Arch Surg. 1987;122:731–734. doi: 10.1001/archsurg.1987.01400180113022. [DOI] [PubMed] [Google Scholar]
- 11.Greve JW, Maessen JG, Tiebosch T, Buurman WA, Gouma DJ. Prevention of postoperative complications in jaundiced rats. Internal biliary drainage versus oral lactulose. Ann Surg. 1990;212:221–227. doi: 10.1097/00000658-199008000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gouma DJ, Coelho JC, Fisher JD, Schlegel JF, Li YF, Moody FG. Endotoxemia after relief of biliary obstruction by internal and external drainage in rats. Am J Surg. 1986;151:476–479. doi: 10.1016/0002-9610(86)90107-8. [DOI] [PubMed] [Google Scholar]
- 13.Megison SM, Dunn CW, Horton JW, Chao H. Effects of relief of biliary obstruction on mononuclear phagocyte system function and cell mediated immunity. Br J Surg. 1991;78:568–571. doi: 10.1002/bjs.1800780516. [DOI] [PubMed] [Google Scholar]
- 14.Thompson RL, Hoper M, Diamond T, Rowlands BJ. Development and reversibility of T lymphocyte dysfunction in experimental obstructive jaundice. Br J Surg. 1990;77:1229–1232. doi: 10.1002/bjs.1800771112. [DOI] [PubMed] [Google Scholar]
- 15.Smith AC, Dowsett JF, Russell RC, Hatfield AR, Cotton PB. Randomised trial of endoscopic stenting versus surgical bypass in malignant low bileduct obstruction. Lancet. 1994;344:1655–1660. doi: 10.1016/s0140-6736(94)90455-3. [DOI] [PubMed] [Google Scholar]
- 16.Andersen JR, Sørensen SM, Kruse A, Rokkjaer M, Matzen P. Randomised trial of endoscopic endoprosthesis versus operative bypass in malignant obstructive jaundice. Gut. 1989;30:1132–1135. doi: 10.1136/gut.30.8.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trede M, Schwall G. The complications of pancreatectomy. Ann Surg. 1988;207:39–47. doi: 10.1097/00000658-198801000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lygidakis NJ, van der Heyde MN, Lubbers MJ. Evaluation of preoperative biliary drainage in the surgical management of pancreatic head carcinoma. Acta Chir Scand. 1987;153:665–668. [PubMed] [Google Scholar]
- 19.Smith RA, Dajani K, Dodd S, Whelan P, Raraty M, Sutton R, Campbell F, Neoptolemos JP, Ghaneh P. Preoperative resolution of jaundice following biliary stenting predicts more favourable early survival in resected pancreatic ductal adenocarcinoma. Ann Surg Oncol. 2008;15:3138–3146. doi: 10.1245/s10434-008-0148-z. [DOI] [PubMed] [Google Scholar]
- 20.Lai EC, Mok FP, Fan ST, Lo CM, Chu KM, Liu CL, Wong J. Preoperative endoscopic drainage for malignant obstructive jaundice. Br J Surg. 1994;81:1195–1198. doi: 10.1002/bjs.1800810839. [DOI] [PubMed] [Google Scholar]
- 21.Choi YM, Cho EH, Lee KY, Ahn SI, Choi SK, Kim SJ, Hur YS, Cho YU, Hong KC, Shin SH, et al. Effect of preoperative biliary drainage on surgical results after pancreaticoduodenectomy in patients with distal common bile duct cancer: focused on the rate of decrease in serum bilirubin. World J Gastroenterol. 2008;14:1102–1107. doi: 10.3748/wjg.14.1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Limongelli P, Pai M, Bansi D, Thiallinagram A, Tait P, Jackson J, Habib NA, Williamson RC, Jiao LR. Correlation between preoperative biliary drainage, bile duct contamination, and postoperative outcomes for pancreatic surgery. Surgery. 2007;142:313–318. doi: 10.1016/j.surg.2007.04.022. [DOI] [PubMed] [Google Scholar]
- 23.Povoski SP, Karpeh MS Jr, Conlon KC, Blumgart LH, Brennan MF. Association of preoperative biliary drainage with postoperative outcome following pancreaticoduodenectomy. Ann Surg. 1999;230:131–142. doi: 10.1097/00000658-199908000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karsten TM, Coene PP, van Gulik TM, Bosma A, van Marle J, James J, Lygidakis NJ, Klopper PJ, van der Heyde MN. Morphologic changes of extrahepatic bile ducts during obstruction and subsequent decompression by endoprosthesis. Surgery. 1992;111:562–568. [PubMed] [Google Scholar]


