Abstract
We report a case of severe obstructive sleep apnea (OSA) in a patient with symptomatic daytime cardiac bradyarrhythmia. Continuous positive airway pressure therapy prevented atrioventricular blocks that emerged after cardiac pacing for sick sinus syndrome. OSA could be associated with daytime bradyarrhythmia.
Citation:
Ji KH; Kim DH; Yun CH. Severe obstructive sleep apnea syndrome with symptomatic daytime bradyarrhythmia. J Clin Sleep Med 2009;5(3):246–247.
Keywords: Arrhythmia, cardiac; pacemaker, artificial; continuous positive airway pressure
Obstructive sleep apnea (OSA) is characterized by repetitive upper airway obstruction or narrowing during sleep, resulting in cyclic fluctuations in sympathovagal balance, surges in blood pressure, repetitive hypoxemia or CO2 retention, and cardiac hemodynamic changes.1 Various cardiac arrhythmias are known to be associated with OSA. OSA-related cardiopulmonary responses may underlie that association. However, the arrhythmias previously reported occurred exclusively during sleep.2,3 We report a case of severe OSA in a patient with symptomatic daytime bradyarrhythmias.
CASE REPORT
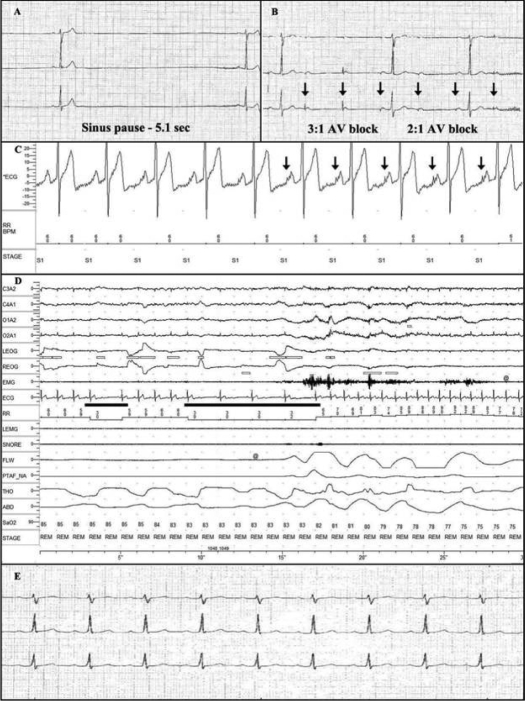
An obese 46-year-old man (body mass index: 35.8 kg/m2) presented with a one-year history of chest discomfort and dizziness lasting 10–20 sec. Symptoms occurred mainly during the daytime with an average frequency of 4 to 5 times week. He also occasionally awoke during sleep because of these symptoms. His blood pressure was under control, less than 130/90 with lercanidipine 10 mg a day for more than one year. There was no change in medication during admission and follow-up. He was a smoker (1–2 pack a day) and social alcohol drinker. Routine laboratory workup, electrocardiography, coronary angiography, cardiac echocardiography, and a treadmill test showed no abnormality. Twenty-four hour Holter monitoring demonstrated symptomatic sinus pauses (2.0–7.1 s). They were associated with chest discomfort and dizziness and were documented during both daytime and nighttime (day: 2 times; night 1 time) (Figure 1A). Under a diagnosis of sick sinus syndrome, he received a cardiac pacemaker implant with atrial single chamber pacing. Despite atrial pacing, his symptoms persisted. After 2 days, follow-up Holter monitoring showed occasional 2:1 and 3:1 atrioventricular (AV) block during wakefulness and sleep (Figure 1B). In his history, he complained of snoring every night and excessive daytime sleepiness (Epworth Sleepiness Scale score: 12). He underwent nocturnal polysomnography (PSG) that revealed severe OSA (apnea-hypopnea index, AHI, 55.5; minimum SpO2, 67%). Electrocardiography on PSG showed frequent atrial pacing (Figure 1C) and 2:1 AV block during NREM and REM sleep (NREM, 3 times; REM, 19 times) (Figure 1D). Continuous positive airway pressure (CPAP) titration was conducted during the following night. CPAP at 15 cm H2O resolved obstructive sleep disordered breathings, atrial pacing, and AV block. After application of CPAP therapy, his chest discomfort subsided with improvement of daytime sleepiness. One week after ongoing CPAP, no further atrial pacing or AV block was present on Holter monitoring (Figure 1E). The patient was free from symptoms with no atrial pacing and AV block on Holter monitoring 6 months after CPAP therapy (AHI, 6.3; average nocturnal usage, 6 hours; Epworth Sleepiness Scale score, 7).
Figure 1.
Electrocardiographic findings. A: Recurrent sinus pauses during daytime and nighttime on the first Holter monitoring. B: Atrial pacing and 3:1 AV block and 2:1 AV block marked with arrows. C: Atrial pacings (arrows) on polysomnography. D: Sleep apnea-related AV block in REM sleep. E: Resolution of cardiac pacing and AV blocks after CPAP therapy.
DISCUSSION
Pacemaker implantation is generally accepted for patients with symptomatic asystole lasting ≥ 3 sec during wakefulness.4 Following cardiac pacemaker implantation, persistence of symptoms and newly diagnosed AV block warrants further investigation. We performed a diagnostic PSG instead of an electrophysiological study of the cardiac conduction system. Our rationale for giving priority to PSG was as follows: First, the patient had high risk factors for OSA, such as habitual snoring, obesity, and comorbid hypertension. Second, OSA is known to be a reversible cause of cardiac bradyarrhythmias, although bradyarrhythmias had not been documented during daytime.2,3 On follow-up Holter monitoring before OSA intervention, atrial pacing occurred during day and night, suggesting a persistent sinus node dysfunction. In addition to previously observed sinus pauses, there were newly detected AV blocks during both wakefulness and sleep. A plausible explanation is that AV block might coexist initially, but be masked by prolonged sinus pauses before cardiac pacing. OSA might contribute to the development of daytime and nocturnal sinus pauses and AV blocks in this patient. Diagnostic PSG revealed severe OSA, frequent atrial pacing, and AV block, which occurred more frequently during REM sleep. During the night of CPAP titration, atrial pacing and AV blocks disappeared at an optimal pressure at 15 cm H2O. Holter monitoring after CPAP application revealed an absence of atrial pacing and AV block. The patient was free of symptoms and compliant with CPAP therapy with a minimal residual AHI. Lercanidipine selectively blocks l-type calcium channel with no effect on potassium and sodium channels.5 Therefore it is less likely to be arrhythmogenic. Moreover, his symptoms resulted from sinus pauses or AV blocks, not from the vasodilatory effect of lercanidipine. That is supported by reproducibly documented temporal relationship between symptoms and bradyarrhythmias during Holter monitoring. All these findings suggest that lercanidipine is less likely to contribute to the development of arrhythmia in this patient. However, we cannot completely exclude the possible intrinsic abnormality in cardiac conduction system because the cardiac electrophysiologic study was not performed.
Hypoxia and REM sleep are known as pathogenic factors in OSA-related bradyarrhythmias.3 Significant association of bradyarrhythmias with prominent oxygen desaturation and REM sleep supports this mechanism.6 Hypoxia with cessation of airflow during sleep is known to increase vagal tone.7 Increased vagal tone is a predisposing condition for bradyarrhythmias. Besides the role of hypoxia, episodic vagal dominance with the background of sympathetic dominance during REM sleep might trigger the emergence of bradycardia. The effect of REM sleep per se was independent from REM sleep related accentuation of hypoxia and apneas.3 Predominance of AV blocks during REM sleep in this patient supports the impact of REM sleep. Although hypoxia and REM sleep could explain the emergence of bradyarrhythmias during sleep, the exact mechanism of daytime arrhythmia is uncertain in this patient. Sleep apnea related consequences such as hypoxia, sympathovagal imbalance, impaired baroreflex, atrial dilatation, myocardial ischemia, and hemodynamic fluctuation may have persistent impact on cardiac conduction. Chronic impact of OSA on systemic hypertension and atrial fibrillation has been documented.1
This report illustrates that OSA can be associated with daytime cardiac bradyarrhythmia. OSA should be considered one of potential mechanisms for nocturnal and even daytime cardiac arrhythmia, especially in patients with high risk factors for OSA, such as obesity, habitual snoring, or observed apneas.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Caples SM, Gami AS, Somers VK. Obstructive sleep apnea. Ann Intern Med. 2005;142:187–97. doi: 10.7326/0003-4819-142-3-200502010-00010. [DOI] [PubMed] [Google Scholar]
- 2.Guilleminault C, Connolly SJ, Winkle RA. Cardiac arrhythmia and conduction disturbances during sleep in 400 patients with sleep apnea syndrome. Am J Cardiol. 1983;52:490–4. doi: 10.1016/0002-9149(83)90013-9. [DOI] [PubMed] [Google Scholar]
- 3.Becker HF, Koehler U, Stammnitz A, Peter JH. Heart block in patients with sleep apnea. Thorax. 1998;53(Suppl 3):S29–32. doi: 10.1136/thx.53.2008.s29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 Guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline update for implantation of cardiac pacemakers and antiarrhythmia devices): developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. Circulation. 2008;117:e350–408. doi: 10.1161/CIRCUALTIONAHA.108.189742. [DOI] [PubMed] [Google Scholar]
- 5.Cerbai E, Sartiani L, DePaoli P, et al. Electrophysiologic effects of lercanidipine on repolarizing potassium currents. J Cardiovasc Pharmacol. 2000;36:584–91. doi: 10.1097/00005344-200011000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Koehler U, Fus E, Grim W, et al. Heart block in patients with obstructive sleep apnea: pathogenetic factors and effects of treatment. Eur Respir J. 1998;11:434–9. doi: 10.1183/09031936.98.11020434. [DOI] [PubMed] [Google Scholar]
- 7.Zwillich C, Devlin T, White D, Douglas N, Weil J, Martin R. Bradycardia during sleep apnea. Characteristics and mechanism. J Clin Invest. 1982;69:1286–92. doi: 10.1172/JCI110568. [DOI] [PMC free article] [PubMed] [Google Scholar]