Abstract
A pilot study of the use of digital images as an adjunct to telephone referral was undertaken. Hand trauma represented the majority of the twenty patients included in the study, and the system was found to be an effective aid to delivering appropriate management. We have found image analysis to be a useful addition to the telephone referral process already in use in our unit, but it is unlikely to replace the need for real time clinical assessment of the patient.
INTRODUCTION
Recent papers have demonstrated the value of telemedicine in plastic surgery1-3. Most notably, Wallace and colleagues incorporated a three phase trial into their trauma service and found telemedicine to be a valuable method of providing preliminary information, often significantly modifying management1. Richard Wootton has described the success of minor injuries telemedicine, which had been applied to over twenty units in the United Kingdom in 2001. He noted that it would be more economically sensible in rural regions like the highlands and islands of Scotland than in London, for example4.
Our unit provides a plastic surgical service to the whole of Northern Ireland, receiving daily trauma referrals from distant peripheral hospitals and minor injury units. We wished to take advantage of the potential benefits of telemedicine, and decided that the first step should test the reliability of still digital image analysis combined with verbal consultation.
METHODS
A pilot study of twenty trauma patients was undertaken. Each patient in the study was assessed at a trauma clinic by a house officer with very limited plastic surgery experience. This was in order to mirror the limited plastic surgery experience of a doctor in an Accident and Emergency department. Following the assessment, informed consent was taken for digital photography of the injured body part or X-ray. An image of the injured body part or X-ray (on a light-box) was taken using a digital camera. The same camera was used throughout the study, with resolution 3.2 mega pixels and automatic flash. The same room was used for all photography, with standard illumination. The house officer then contacted the registrar, and presented the findings from history and examination. The digital image was viewed on a ward computer. Based on the image and description, a preliminary management decision was made and documented. The registrar then assessed each patient in person. The management decision following face to face consultation was documented and implemented.
RESULTS
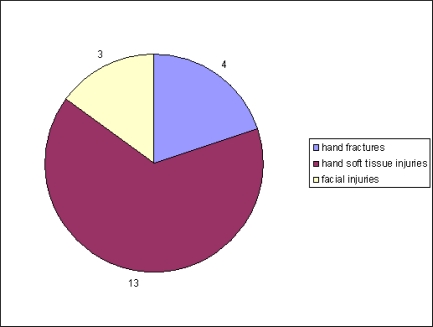
Twenty patients were included in the pilot study. Seventeen of these were hand injuries. The distribution is shown in Figure 1. In only one of the twenty patients did face to face consultation highlight important patient history details that were not obtained from the referral. In one of the cases a discrepancy in examination findings was identified (a house officer diagnosis of “significant skin loss” on a finger was deemed insignificant following registrar review). In one patient there was a difference between the management plan based on history / image analysis and the plan following face to face consultation. Five of the twenty patients could have been adequately managed in a casualty department. Thus for a quarter of patients, image analysis could have led to advice which would have precluded the need for transfer to our department.
Fig 1.
Distribution of trauma clinic injuries
DISCUSSION
Demartines wrote ‘Telemedicine is believed to favour and simplify the exchange and diffusion of information, knowledge and surgical education by permitting broader access to expertise and second opinions without travel’5. He recognised that surgical applications of telemedicine remain limited, probably due to a lack of information and the need for more research. In the planning of research he stressed the need to consider the clinical effectiveness of the service as well as the quality of the technology.
A 2001 systematic review of telemedicine literature6 found that only a few studies compared telemedicine application with conventional service provision (something we attempted to do, albeit on a small scale). Roine felt that more evidence is needed regarding the cost effectiveness of telemedicine, and that implementation of new services should have a sound business case, and a link to data collection and analysis.
Whitten and colleagues echoed the need for better standards of economic analysis within telemedicine studies7. They recognised however that ‘a telemedicine service that is cost effective in the remote highlands of Scotland is unlikely to generate the same cost effectiveness in the middle of Manchester’ (in agreement with Wootton4). Yellowlees has outlined seven core principles which underlie the development of a successful telemedicine service8: (Table 1)
Table 1.
Seven core principles
|
Admittedly, these principles relate more to teams who are setting up more complicated technologies, including video consultations, but they serve as useful reference points. In this study the technology was very simple, with obvious low cost implications. Digital cameras are now commonplace throughout hospitals, and photography departments are generally very facilitative. Our results were encouraging. Face to face consultation by the registrar highlighted only two discrepancies following the referral (one from history and one from examination). In only one instance was management different following face to face consultation (a wound was left to heal, rather than taken to theatre).
A larger study of telemedicine in a plastic surgery department (Wallace, 20081) found that, with the technology, significantly fewer patients needed to attend the department for review, and more patients could be put directly onto a day surgery operating list. The authors felt that telemedicine improved the clarity of the communication process, and facilitated earlier and more frequent senior clinician involvement.
In terms of the size of the problem locally, the number of emergency referrals made to our department is not routinely measured. However, we recently surveyed emergency referrals to plastic surgery units throughout the United Kingdom and Ireland9. The ‘average unit’ receives between six and eight referrals each day, and between three and five each night. The ‘average unit’ admits between 1000 and 1500 emergency patients per year. Our emergency admissions are now close to 2000 per year, and our referral rates are almost certainly higher than the ‘average’ above. Most surveyed units received referrals from less than five emergency departments, whereas our unit covers all emergency departments and minor injury units in Northern Ireland. Thus there is a substantial workload and referrals often come from geographically distant locations. Telemedicine would likely be of greatest benefit for such referrals.
This system presents a simple and effective addition to routine trauma management. Due to strict guidelines relating to image storage and transfer10, it would be advisable for images to be transferred via hospital photography departments. Out of hours, for emergency cases, images can be attached to password protected emails (with secure email accounts set up by the photography department).
It is our view that telemedicine will not (and should not) replace face to face consultation for patients who genuinely need to be seen in a plastic surgery department. It has a role in the early management of peripheral referrals, many of which do not require transfer. It seems possible from this pilot study that unnecessary transfer to the department could be reduced by up to twenty-five percent with the use of telemedicine. A robust controlled trial with larger patient numbers would be indicated to validate any significant changes to the current management system. We would hope to start this within the next year.
The authors have no conflict of interest.
REFERENCES
- 1.Wallace DL, Jones SM, Milroy C, Pickford MA. Telemedicine for acute plastic surgical trauma and burns. J Plast Reconstr Aesthet Surg. 2008;61(1):31–6. doi: 10.1016/j.bjps.2006.03.045. [DOI] [PubMed] [Google Scholar]
- 2.Roa L, Gómez-Cía T, Acha B, Serrano C. Digital imaging in remote diagnosis of burns. Burns. 1999;25(7):617–23. doi: 10.1016/s0305-4179(99)00053-4. [DOI] [PubMed] [Google Scholar]
- 3.Jones SM, Milroy C, Pickford MA. Telemedicine in acute plastic surgical trauma and burns. Ann R Coll Surg Engl. 2004;86(4):239–42. doi: 10.1308/147870804344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wootton R. Recent advances: Telemedicine. BMJ. 2001;323(7312):557–60. doi: 10.1136/bmj.323.7312.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Demartines N, Otto U, Mutter D, Labler L, van Weymarn A, Vix M, et al. An evaluation of telemedicine in surgery: telediagnosis compared with direct diagnosis. Arch Surg. 2000;135(7):849–53. doi: 10.1001/archsurg.135.7.849. [DOI] [PubMed] [Google Scholar]
- 6.Roine R, Ohinmaa A, Hailey D. Assessing telemedicine: a systematic review of the literature. CMAJ. 2001;165(6):765–71. [PMC free article] [PubMed] [Google Scholar]
- 7.Whitten PS, Mair FS, Haycox A, May CR, Williams TL, Hellmich S, et al. Systematic review of cost effectiveness studies of telemedicine interventions. BMJ. 2002;324(7351):1434–7. doi: 10.1136/bmj.324.7351.1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yellowlees P. Successful development of telemedicine systems - seven core principles. J Telemed Telecare. 1997;3(4):215–22. doi: 10.1258/1357633971931192. [DOI] [PubMed] [Google Scholar]
- 9.Diver AJ, Tohill MP, Sinclair JS, Gordon DJ. Management of Emergency Referrals to UK and Ireland Plastic Surgery Units. Submitted for publication. [DOI] [PubMed]
- 10.Institute of Medical Illustrators; Law and Ethics Department. A model policy on photography and video recording of patients: Confidentiality and Consent, Copyright and Storage. 2002 Dec; Available from: www.imi.org.uk/lawethics/Model-Consent.pdf.