Abstract
Epstein-Barr virus is an unusual pathogen in the aetiology of alveolitis. We describe a case of Epstein-Barr virus induced pneumonitis and its successful treatment with Aciclovir.
Keywords: Epstein-Barr virus, Pneumonitis, Computed Tomography, Lung, Aciclovir
CASE REPORT
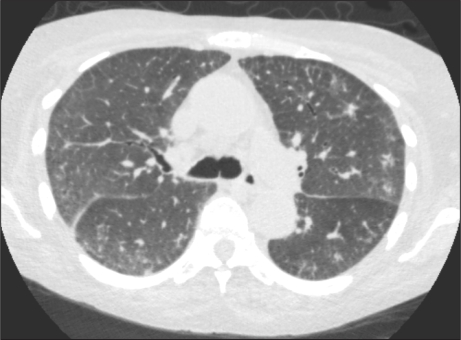
A 62-year-old female with a history of polymyositis was admitted with a four-week history of increasing dyspnoea. She had been treated with maintenance oral steroid therapy over the previous 4 years, augmented with oral cyclophosphamide over the preceding 4 weeks. On examination there were fine crepitations to the mid-zones. The patient was hypoxic with a Pa02 of 10.2 KPa on inspired FiO2 of 0.6. C reactive protein was elevated at 212 mg/L. Echocardiogram was normal. Initial chest X-ray was normal (figure 1). A CT Pulmonary Angiogram (CTPA) was then performed and thrombus excluded, however inspiratory and expiratory high-resolution (HRCT) scans were obtained subsequent to the CTPA due to the grossly abnormal appearance of the lung parenchyma on lung windows. High resolution scan images demonstrated widespread marked ground glass opacity with intra and interlobular septal thickening in keeping with a diffuse alveolitis (figure 2a and 2b). Ground glass opacification describes the findings on HRCT of the lungs in which there is a hazy increased attenuation of lung with preservation of bronchial and vascular margins. This appearance can be caused by partial filling of air spaces, interstitial thickening, partial collapse of alveoli, normal expiration, or increased capillary blood volume1. The presence of numerous intra and interlobular septa almost always indicate the presence of an interstitial abnormality, only a few septa should be visible in normal patients. Septal thickening can be seen in the presence of interstitial fluid, cellular infiltration or fibrosis2. Diffuse alveolitis refers to the combination of these appearances throughout both lung fields suggestive of an acute inflammatory process of the pulmonary alveoli.
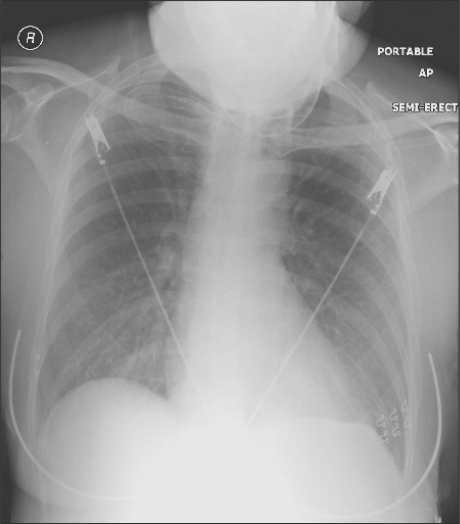
Fig 1.
Normal chest radiograph on admission.
Fig 2a.
Coronal reformat reproduced from CTPA study demonstrating wide spread ground glass opacity (white arrows).
Fig 2b.
Transaxial HRCT image at level of the carina showing intralobular interstitial thickening (black arrow), interlobular septal thickening (grey arrow) and ground glass opacity (white arrow).
The patient subsequently required intubation and ventilation; EBV was identified on endotracheal aspirate with a copy number of 28,420/ml on quantitative PCR. No other bacterial, viral or fungal infection was identified. The patient was then treated with IV Aciclovir with subsequent dramatic clinical and radiological improvement (figure 3). EBV was not detectable on repeat airway aspirate following treatment.
Fig 3.
Follow-up transaxial CT chest image demonstrating marked improvement in interstitial changes.
This patient was predisposed to infection in the setting of chronic disease and ongoing immunosuppression. The normal echocardiogram findings combined with the absence of features of cardiac failure make pulmonary oedema less likely as a contributing factor. This is also supported by the presence of an inflammatory response, which responded to antiviral treatment and associated radiological resolution.
EBV has been proposed in the pathogenesis of cryptogenic fibrosing alveolitis and more recently has been implicated in interstitial lung disease resembling sarcoidosis3. The role of EBV as an infective agent in the development of lung disease is controversial and there are few reports of symptomatic pulmonary involvement directly attributable to EBV infection. There is no single anti-viral agent specifically indicated in the treatment of pulmonary EBV infection. There have been case reports describing favourable outcomes with the use of Aciclovir4. This case supports the use of IV Aciclovir in EBV associated pneumonitis.
The authors have no conflict of interest
REFERENCES
- 1.Collins J, Stern EJ. Ground-glass opacity at CT: the ABCs. Am J Roentgenol. 1997;169(2):355–67. doi: 10.2214/ajr.169.2.9242736. [DOI] [PubMed] [Google Scholar]
- 2.Webb WR, Müller NL, Naidich DP. High-resolution CT of the Lung. Philadelphia: Lippincott, Williams & Wilkins; 2001. [Google Scholar]
- 3.Marzouk K, Corate L, Saleh S, Sharma OP. Epstein-Barr-virus-induced interstitial lung disease. Curr Opin Pulm Med. 2005;11(5):456–60. doi: 10.1097/01.mcp.0000176678.38539.9a. [DOI] [PubMed] [Google Scholar]
- 4.Schooley RT, Carey RW, Miller G, Henle W, Eastman R, Mark EJ, et al. Chronic Epstein-Barr virus infection associated with fever and interstitial pneumonitis. Clinical and serologic features and response to antiviral chemotherapy. Ann Intern Med. 1986;104(5):636–43. doi: 10.7326/0003-4819-104-5-636. [DOI] [PubMed] [Google Scholar]