Abstract
Objective To examine whether preschool children with Attention deficit/hyperactivity disorder (ADHD) utilize more speech and language therapy (ST), occupational therapy (OT), and physical therapy (PT) services and are more likely to be placed in special education (SPED) classrooms as compared to their peers. Corresponding financial consequences were also examined. Methods The amount of ST, OT, and PT, as well as SPED placements, was examined in 3- and 4-year-old children with and without ADHD (n = 109 and n = 97, respectively) during the baseline portion of an ongoing, 5-year longitudinal study. Costs for individual services and aggregate cost were determined per child and compared across groups. Results Preschool children with ADHD were more likely to receive individual and multiple services. Higher rates of service utilization translated into increased costs for each individual service with the exception of PT. Conclusions A comprehensive understanding of service utilization in the early years of development is important in addressing the increased service use in the preschool years and assist in guiding allocation of resources.
Keywords: attention deficit hyperactivity disorder, economic impact, preschool children, service utilization
Introduction
Attention deficit/hyperactivity disorder (ADHD) is one of the most commonly diagnosed psychiatric disorders in childhood, affecting 3–7% of school-age children (American Psychiatric Association, 2000). The core symptoms (i.e., hyperactivity, impulsivity, and inattention) typically begin at an early age and result in substantial impairment across multiple domains of functioning (Barkley, 2006). Relative to their typically developing counterparts, children with ADHD often have difficulties relating to peers and adults, experience significant family conflict (Barkley, 2006), and underachieve academically (Barkley, Fisher, Edelbrock, & Smallish, 1990; Barry, Lyman, & Klinger, 2002; DuPaul, McGoey, Eckert, & VanBrankle, 2001; Hinshaw, 1992). For many children, these difficulties persist into adolescence and adulthood (Arons, Katz-Leavy, Wittig, & Holden, 2002; Loe & Feldman, 2007; Mannuzza, Klein, Bessler, Malloy, & LaPadula, 1998). Given the high prevalence of ADHD, the chronic nature of the disorder, and the multiple areas of psychosocial impairment, it is not surprising that there has been a growing interest in characterizing the breadth and frequency of service utilization and economic burdens associated with the disorder (Leslie & Wolraich, 2007; Pelham, Foster, & Robb, 2007). Documenting the extent to which children with ADHD utilize services can lead to more comprehensive and effective treatment and intervention programs, illustrate trends in service use for children with ADHD, and enhance communication among service providers. Moreover, detailed cost assessments may shed light on the economic impact of the illness and assist policy makers in funding allocation.
Currently, three major sectors provide adjunctive services to children with ADHD: the medical health care sector, the mental health care sector, and the educational sector (Leslie & Wolraich, 2007). Within the medical health care sector, children with ADHD have been shown to average significantly more emergency department (ED) visits compared to children without the disorder (Guevara, Lozano, Wickizer, Mell, & Gephart, 2001; Kelleher, 1998). Within the mental health care sector, children with ADHD have been shown to have twice the rate of contact with mental health care providers (Bussing, Zima, Perwien, Belin, & Widawski, 1998) and nearly 10 times more visits to outpatient mental health clinics (Guevara et al., 2001) compared to children without ADHD. Finally, within the educational sector, it is estimated that ∼50% of children receiving special education (SPED) services are diagnosed with ADHD (Bussing et al., 1998; Forness & Kavale, 2002). Moreover, ∼77% of children with ADHD are reported to utilize school services, including tutoring, specialized class placements, school counseling, and classroom monitoring (Kendall, Leo, Perrin, & Hatton, 2005).
In light of the above service utilization disparities between children with ADHD and their non-ADHD classmates, considerable effort has been directed toward ascertaining the economic impact of service utilization among individuals with ADHD. In a review examining the financial burdens associated with ADHD, Pelham and colleagues (2007) conservatively estimated the annual cost of illness for a child with ADHD to be $14,576 greater than that for comparison controls. In addition, Guevara and colleagues (2001) reported primary care costs, outpatient mental health costs, pharmacy costs, and ED costs to be significantly greater among youth with ADHD.
In many respects, the financial toll exacted by ADHD appears to meet, and in some cases exceed, that of certain chronic medical illnesses such as asthma (Chan, Zhan, & Homer, 2002; Kelleher, Childs, & Harman, 2001). In particular, Kelleher (2001) observed that children with ADHD incurred 32% higher mental health costs and 42% higher prescription costs compared to children with asthma. When examining the excess cost associated with ADHD over a 1-year period, Birnbaum and colleagues found that treatment and other health care costs for children with ADHD (aged 7–18) totaled $3.3 billion. Further, when the health care costs of family members of children with ADHD were taken into account as a measure of genetic psychopathological risk, the total cost was estimated to be $5.1 billion (Birnbaum et al., 2005). Thus, not only is the cost of providing services to children with ADHD astounding, but the cost of health care provided to their family members adds considerably to the already staggering economic burden.
Children with ADHD accrued higher costs in the educational sector as well. Estimating the annual educational costs associated with ADHD, above and beyond the costs of general education, investigators have found the total burden to exceed $4,000 per individual (Forness & Kavale, 2002; Pelham et al., 2007). When considered in the context of ADHD prevalence, the estimated annual aggregate educational cost associated with ADHD is approximately $13.6 billion (Pelham et al., 2007). Thus, the lifetime cost of providing services to children with ADHD is staggering, both to the affected individual/family and to the society at large.
While considerable literature exists regarding service utilization and associated costs in school-aged children with ADHD, limited research has explored patterns of service utilization during the preschool years. This dearth of literature is surprising given that ADHD is the most commonly diagnosed psychological disorder during the preschool period (Armstrong & Nettleton, 2004) and has been associated with deficits in a wide array of cognitive domains (Iwanaga, Ozawa, Kawasaki, & Tsuchida, 2006; Yochman, Ornoy, & Parush, 2006). Thus, while historically unexplored, one could reasonably posit even young children with ADHD utilize more services and require greater expenditures relative to preschoolers without ADHD.
The aim of the current study was to quantify the relative frequency and resultant economic impact associated with ADHD during the preschool period. In particular, efforts were made to determine the extent to which preschool children with and without ADHD differentially utilize more speech and language therapy (ST), occupational therapy (OT), and physical therapy (PT) services along with more frequent SPED placements. Also examined were the corresponding financial consequences of increased service utilization. Given that little is known about the utilization of services and costs associated with these types of services in preschool children with ADHD, examining this area will assist in understanding service use during this developmental period, shed light on the scope of neurodevelopmental impairment associated with ADHD, and create a more comprehensive understanding of the economic impact of ADHD in preschool children. In particular, efforts to monitor service use will help guide allocation of resources and assist in the development of comprehensive assessment protocols for preschool children with the disorder. Moreover, through the use of longitudinal research methods, researchers will be able to systematically gauge the extent to which early receipt of auxiliary services confers protective benefit with respect to the persistence of ADHD and/or subsequent neurocognitive functioning.
Methods
Participants
As part of the initial evaluation for a longitudinal study examining factors associated with the persistence of ADHD in preschoolers, a sample of preschool children was recruited from community preschools; direct clinical referrals were also accepted from schools and local practitioners. Although all baseline data have been collected and preliminary results have been documented elsewhere (Healey, Miller, Castelli, Marks, & Halperin, 2008; Miller et al., 2007), follow-up data are still being acquired, thus precluding efforts to gauge the prognostic benefit(s) of early service utilization. Recruitment of the community-based sample was conducted using a two-step procedure in which principals of local area private and public preschools were contacted and permission was requested to screen the school for children with attention and behavior problems. Sixty-eight preschools agreed to participate, and parents of children in these schools were sent the AD/HD Rating Scale-IV (DuPaul, Power, Anastopoulus, & Reid, 1998), which consisted of the 18 Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) ADHD behaviors listed in DSM-IV, which were rated on a 4-point scale. For both the community-based and clinically referred samples, children whose parent and/or teacher endorsed at least six inattention or six hyperactive/impulsive symptom items (ADHD group) or whose parent and teacher endorsed fewer than three inattention and fewer than three hyperactive/impulsive symptoms on the DSM-IV AD/HD rating scale (Control group) were considered for inclusion in the study. Further inclusion criteria required all eligible participants to be English-speaking and attending school or day care. In addition, participants were required to have a full-scale IQ ≥80, as measured by the Wechsler Preschool and Primary Scale of Intelligence–Third Edition (Wechsler, 2006). Children with a pervasive developmental disorder, posttraumatic stress disorder, or a diagnosed neurological disorder, as well as individuals taking systemic medication for a chronic medical condition (including ADHD), were excluded from participation; individuals with ADHD were required to be unmedicated at the time of the assessment.
ADHD and control group status were ultimately determined by applying ADHD criteria (any type) based on a parent interview using the Kiddie Schedule for Affective Disorders and Schizophrenia – Present and Lifetime Version (Kiddie-SADS-PL; Kaufman, Birmaher, Brent, Rao, & Ryan, 1996). The Kiddie-SADS-PL was also used to screen oppositional defiant disorder (ODD) as it is a common comorbidity among preschool children with ADHD (Lavigne et al., 1996). The Kiddie-SADS-PL is a commonly used diagnostic tool that, when administered by trained evaluators, has been shown to have strong psychometric properties (Kaufman et al., 1999). The final sample consisted of 206 children (151 boys and 55 girls) ranging in age from 3.05 to 4.99 years (M = 4.29, SD = 0.48). Among these, 109 met criteria for ADHD and 97 served as a non-ADHD control group (Table I). As can be seen, the groups did not differ with respect to sex distribution; however, a small but significant difference emerged with regard to age (p = 04), such that preschoolers with ADHD were slightly older relative to their typically developing counterparts. In addition, ADHD and control groups differed in racial composition (p =.001; see Table I). Finally, significant group differences were observed for rates of ODD (p <.001), with a greater prevalence of the disorder observed among ADHD probands (42 vs. 11%).
Table I.
Demographic Information for Study Sample, ADHD Group, and Control
| Variable | Entire sample (n = 206) | ADHD (n = 109) | Control (n = 97) | t/x2 | p |
|---|---|---|---|---|---|
| Age (years) | M = 4.29 SD = 0.48 | M = 4.36 SD = 0.49 | M = 4.22 SD = 0.47 | 2.12 | .04 |
| Percent male | 73% | 74% | 72% | 0.35 | 0.73 |
| Race | |||||
| White | 59% | 61% | 57% | 15.92 | .001 |
| Black | 12% | 17% | 7% | ||
| Asian | 10% | 3% | 17% | ||
| Other/Mixed | 19% | 19% | 19% |
This study was approved by the institutional review board of the university in which the research was conducted. Following a complete description of the study, a parent of each child provided written consent for participation.
Procedures
Following screening with parent and teacher ratings, as described above, parents took part in a semistructured interview (K-SADS-PL) and completed a Developmental Demographics form, which acquires demographic and developmental information from birth to the time of the evaluation. On both the Developmental Demographics form and K-SADS-PL interview, parents were queried if the child received auxiliary services and applicable evaluations, received either through the child's school or on a private basis. Pertinent data were collected for PT, OT, ST and SPED. SPED placement was defined as full-time matriculation in any SPED classroom setting. Duration (i.e., how long) and frequency (i.e., how often) of services were collected for OT, PT, and ST; only duration was collected for SPED. Integrating information from both the Developmental Demographics form and the K-SADS-PL interview, duration of services was operationalized as the cumulative number of months since birth in which the service was utilized. Frequency was defined in units, with one unit representing 30 min of service per week. Participants with incomplete duration data (n = 8) were omitted from the analysis; those with incomplete frequency data were included in the analysis, with missing frequency data imputed using the modal frequency score for that particular variable. A service was determined to be utilized if the parent reported duration and/or frequency on either the K-SADS or the Developmental Demographics form.
Total cost of services per child was determined for OT, PT, ST, and SPED. Given that the developmental period in question differs from that of previous investigations, the methods used to estimate services are, to some extent, unique to the current study, but clearly bear resemblance to those used by other researchers (e.g., Pelham et al., 2007). The rate of reimbursement for OT, PT, and ST was provided by the New York City Department of Education (2008) rates of reimbursement during the 2008–2009 school year, which was $45.00 per half-hour of service. The half-hour cost was multiplied by the frequency of service use per week. This figure was multiplied by 4 to obtain a monthly frequency, which was then multiplied by the number of months the service was received. The cost of SPED was determined by the New York City Department of Education, which details the per pupil cost(s) for SPED above those for general education. This yearly cost of $25,427.00 from 2004 to 2005 (later costs were not available) was divided by 9 (number of months in the academic year) to determine the monthly cost for SPED; this figure was then multiplied by the number of months the service had been received. Separate costs were determined for each service (i.e., OT, PT, ST, and SPED) from birth to the time of data collection. In addition, service costs were aggregated to generate a cumulative cost composite, again from birth to the time of data collection.
Data Analysis
In light of the fact that ADHD and control groups differed significantly with respect to age, efforts were undertaken to control for the effect of age on both rates of service utilization and associated costs. Separate binary logistic regression analyses and odds ratio (OR) calculations were performed to examine the impact of group status for receipt of (a) any adjunctive support, (b) specific interventions, and (c) multiple services. For each analysis, age was entered in the first block and group status (ADHD vs. control) in the second block; prevalence of service(s) served as the dependent measure. To determine the extent to which race may have impacted rates of service utilization, group status, race, and the interaction of these factors were submitted to a binary logistic regression using OT, PT, ST, and SPED as dependent measures. In addition, to examine the possible impact of ODD status on patterns of service utilization, chi-square analyses were conducted comparing ADHD-only and ADHD + ODD groups with regard to the prevalence of each service. Finally, multivariate analysis of covariance (MANCOVA; age-controlled) was conducted to examine the impact of group status on costs associated with each service, as well as the aggregate cost.
Results
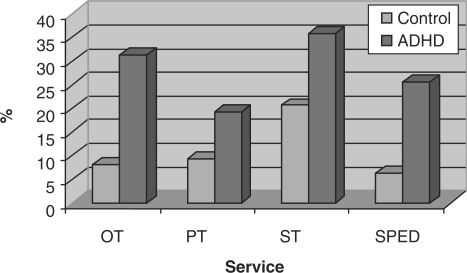
After accounting for age, preschoolers with ADHD were significantly more likely to have received adjunctive support (any service; Wald = 14.35, df = 1, OR = 3.31 p <.001). Examination of individual service areas revealed group differences with regard to rates of OT (Wald = 14.81, df = 1, OR = 5.19, p <.001), PT (Wald = 4.74, df = 1, OR = 2.57, p <.03), ST (Wald = 6.09, df = 1, OR = 2.24, p <.01), and SPED (Wald = 13.93, df = 1, OR = 6.22 p <.001; see Table II). As shown in Fig. 1, preschoolers with ADHD were significantly more likely to have received OT (χ2 = 16.65, p <.001), PT (χ2 = 4.12, p <.005), ST (χ2 = 5.77, p =.02), and SPED placement (χ2 = 14.17, p <.001). Relative to controls, preschool children with ADHD were also more likely to have been recipients of multiple services (Wald = 15.00, df = 1, OR = 4.83 p <.001). Despite the aforementioned differences with regard to rates of service utilization, ADHD and control groups did not differ with regard to the frequency with which the above services were administered (i.e., number of units per week; all p >.05). While group and race impacted the likelihood of service utilization, the interaction of these factors was not statistically significant (p >.05). Finally, no significant differences emerged between ADHD-only and ADHD + ODD groups across all four service areas (ST, OT, PT, and SPED) nor did these latter groups differ with regard to receipt of multiple services (p >.05).
Table II.
Impact of Age and Group Status on Rates of Service Utilization
| Service | Variable | B | Wald | p |
|---|---|---|---|---|
| Any service | Age | 0.38 | 1.40 | >.10 |
| Group | 1.20 | 14.35 | <.001 | |
| Occupational therapy | Age | 0.19 | 0.24 | >.10 |
| Group | 1.65 | 14.81 | <.001 | |
| Physical therapy | Age | 0.61 | 2.20 | >.10 |
| Group | 0.95 | 4.74 | .03 | |
| Speech therapy | Age | 0.27 | 0.67 | >.10 |
| Group | 0.80 | 6.09 | .01 | |
| Special education | Age | 0.89 | 4.72 | .03 |
| Group | 1.83 | 13.93 | <.001 | |
| Multiple services | Age | 0.83 | 5.01 | .03 |
| Group | 1.57 | 15.00 | <.001 |
Figure 1.
Rates of service use among preschoolers with and without ADHD*. * all p <.05.
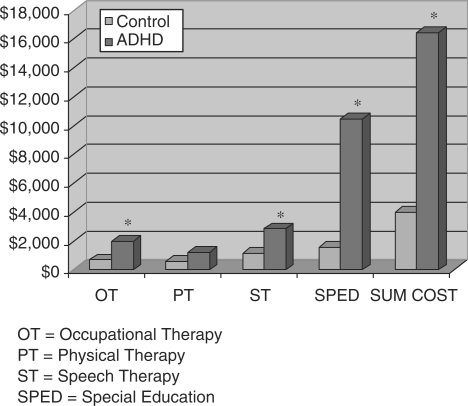
The one-way MANCOVA using cost of services as the dependent variable and age as the covariate revealed a significant main effect for group but not for age and no significant group × age interaction (Wilks’ λ = 0.92, p =.002, ηp2 =.08). Subsequent analysis of variance (ANOVA) revealed significant group differences with regard to costs of OT, F(1, 203) = 7.07, p <.008, ηp2 =.03; ST, F(1, 203) = 8.57, p <.004, ηp2 =.04; and SPED, F(1, 203) = 15.50, p <.000, ηp2 =.07; but not with regard to PT, F(1, 203) = 2.21, p >.05, ηp2 =.011 (see Fig. 2). ADHD and control groups did, however, differ with regard to the aggregate cost index, F(1, 203) = 15.78, p <.001, ηp2 =.07. In addition, a 2 × 4 (Group × Race) ANOVA using service cost as the dependent measure revealed a significant main effect for group (ADHD vs. control); however, the main effect for race and the group × race interaction did not reach statistical significance.
Figure 2.
Individual and cumulative cost of service use*. * p <.01.
Discussion
The aim of this study was to determine rates of service utilization, as well as the corresponding financial costs associated with ADHD in preschool children. This investigation expands upon previous literature by examining service utilization for non-mental health services and by focusing on preschool children with ADHD. Specifically, we examined rates of ST, PT, and OT, along with SPED placement among preschoolers with and without ADHD. Further, we determined the cost of utilizing each of these services, as well as aggregate cost for preschool children with ADHD compared to preschoolers without ADHD.
Results indicated that preschool children with ADHD were significantly more likely to utilize any service compared to preschool children without ADHD. In addition, preschool children with ADHD were also more likely to utilize ST, PT, and OT along with SPED instruction compared to preschool children without ADHD. Interestingly, preschool children with ADHD received two to four times the services of preschool children without ADHD, demonstrating that the magnitude of these differences is substantial. Notably, a significant minority of preschool children with ADHD utilized services; for instance, up to one-third of preschool children with ADHD in this sample have received ST and OT. Further, a third of preschool children with ADHD in this sample utilize multiple services (e.g., ST and OT), a far greater number compared to preschool children without ADHD. Importantly, post hoc analyses indicated that heightened rates of service utilization among preschoolers with ADHD could not be accounted for by the presence of ODD comorbidity. Although no groupwise differences emerged with regard to the frequency with which adjunctive services were administered, this may reflect the fact that auxiliary interventions, when instituted, are provided with similar degrees of frequency to most recipients.
Collectively, these data suggest that the psychiatric manifestations of ADHD are just part of the overall problems that children with ADHD experience. When juxtaposed with data demonstrating heightened rates of speech, language, and motor problems among youth with ADHD (Yochman et al., 2006), these data suggest that, even as early as the preschool period, these youngsters are multiply handicapped and often exhibit difficulties in speech, language, and/or motor skills. While it is conceivable that the prevalence of these services reflects their accessibility (relative to the availability of other services), it is notable that preschoolers with ADHD made significantly greater use of such interventions relative to controls, who also had access to the same interventions.
These data indicate that assessment for speech, occupational, physical and special education services should be a routine part of initial assessment for preschool children who might have ADHD. These results are consistent with the school-aged literature on service use by children with ADHD (Kelleher, 1998; Kendall et al., 2005; Leslie & Wolraich, 2007; Pelham et al., 2007) in that children with ADHD utilize more and varied services compared to children without ADHD, and that this increased utilization is apparent beginning in early childhood.
With respect to the individual costs of services utilized by preschool children with ADHD, the cost associated with OT, PT, ST, and SPED ranged from two to six times that for preschool children without ADHD. Surprisingly, although preschool children with ADHD more often received PT services, there were no significant differences in cost for this service between these groups. It is likely that although fewer comparison control children received PT services, those who did used these services more frequently and for longer periods.
Moreover, it is not surprising that for preschool children with ADHD, aggregate cost of services utilized was four times greater than that for preschool children without ADHD. The results imply that preschool children with ADHD exact a significant economic burden and tax systemic resources. For example, given that ∼2–6% of preschool children meet diagnostic criteria for ADHD (Keenan, Shaw, Walsh, Delliquadri, & Giovannelli, 1997; Lavigne et al., 1996) and that there are an estimated 48,126 preschool children attending school in the city of New York (New York City Department of Education, 2006), it is estimated that preschool children with ADHD in the New York area, at a mean cost of $16, 547.67, exact approximately $16–48 million in OT, PT, ST, and SPED placements over the course of early childhood. Given that these figures do not include preschool-age children who do not attend school, this estimate is likely conservative. Moreover, it is estimated that there are 19 million preschool-age children in the United States (US Census, 2000) and therefore the aggregate cost of providing these services to preschool children with ADHD over early childhood is substantial. Collectively, this demonstrates the considerable cost associated with ADHD, even at a young age. Importantly, the costs detailed here do not include mental health services for ADHD. Given that there is increased identification and provision of pharmacological and psychosocial interventions during the preschool period for children with ADHD (Conner, 2002; Zito et al., 2000), the overall cost of providing services, both mental and non-mental health, is staggering. Direct comparisons with other investigations that have explored the economic impact of ADHD in school-aged children are, in many respects, challenging, given the variations in services examined and the applicability (or lack thereof) of such interventions/accommodations (e.g., grade retention) to preschool children.
Although this study addresses an important understudied question, there are several notable limitations. First, the data collected are retrospective; we relied solely on parental report of their children's utilization of services during a 3- to 5-year period. Although this may have resulted in inaccurate information, given the short period of recall, we estimate this limitation to be minimal. Regardless, prospective data collection constitutes a preferable methodology for exploring such issues. Although logistical constraints precluded the assessment of interrater reliability for the diagnosis of ADHD based on the K-SADS parent interview in the current study, staff underwent rigorous training prior to K-SADS administration (including observations by senior staff) and were supervised by psychologists with expertise in the assessment and diagnosis of disruptive behavior disorders. In addition, an examination of the 1-year stability of the K-SADS for a large portion of the sample (n = 150) was quite respectable (κ = 0.72). In addition, the reliability and validity of methods used to obtain rates of service utilization were not systematically assessed. Future research should validate parent reports of service usage via comparison with objective sources of information [e.g., individualized education programs (IEPs) or progress notes]. Notably, this study did not include in the analysis other services utilized by preschool children [e.g., school counseling and special education itinerant teacher (SEIT)]. These services are an important resource for preschool children, and future efforts should be made to research the breadth of all services that are utilized by this age group.
Additional limitations relate to the inclusion criteria for our sample. The study required that the primary caregiver and the child to be English-speaking. Thus, the findings of this study may not be applicable to non–English speaking families. It may be the case that preschool children with ADHD from non–English speaking families utilize services differently than their English-speaking counterparts, given that these families may not be integrated into existing service systems (Yu, Huang, Schwalberg, & Nyman, 2006). Yu and colleagues found that families with low level of English proficiency were less likely to access health care services for their children. Moreover, children in this study were required to have an IQ above 80. It may be that children with ADHD who have IQs below 80 will have different patterns of service use. Finally, we excluded children with greater than three ADHD symptoms across settings from the comparison control condition. Thus, children with greater frequency of ADHD symptoms but who did not meet study criteria for being at risk for ADHD were excluded from the study. One would expect that including these children in the control condition would result in increased service use and an increase in costs for this group. Although used as an exclusionary criterion, in no instance was a youngster excluded from participation in the baseline assessment on the basis of treatment with stimulant medication. It is, however, conceivable that the absence of such children could bias the sample in favor of a less severe, more neurocognitively intact subgroup of preschoolers. Thus, our estimates of service utilization and economic burden may be somewhat conservative. Collectively, given the criteria for study inclusion, the data may not fully capture the rates of service utilization of preschool children and therefore be an underrepresentation of preschool children utilizing services.
The findings from this study are noteworthy and suggest a closer investigation of the services that preschool children with ADHD utilize. This is the first study, to our knowledge, that has estimated service utilization for preschool children with ADHD, and more specifically, utilization of ST, OT, and PT, as well as SPED classes. Although this study represents an important addition to the literature, future investigation in this area is necessary. Importantly, we did not assess pharmacological and/or psychosocial interventions specifically for ADHD. This is particularly relevant, given the increase in identification of ADHD (Conner, 2002) and provision of mental and nonmental health services for preschool children with the disorder (Hoagwood, Kelleher, Feil, & Comer, 2000; Zito et al., 2000). Capturing the extent to which preschool children use an array of services will provide useful information on whether these children experience difficulties across domains of functioning; such efforts may also assist in the development of assessment protocols that target multiple areas of functioning for preschool children with ADHD.
Given that this study found that up to a third of preschool children with ADHD receive multiple services, determining whether and to what extent utilization of these services impacts functioning is important. If services improve the difficulties preschool children with ADHD experience with speech, language, and motor skills, then it is likely that fewer services will be required when these children enter school. This is particularly important for children affected with ADHD because the multiple difficulties these children experience, when compounded over time, result in poor long-term outcomes for them (e.g., academic failure, peer rejection; Barkley, 2006; Mannuzza et al., 1998). If services provided during early childhood targeting key domains mitigate impairment, then it is likely that children with ADHD will experience greater success and fewer difficulties during childhood and adolescence. Consequently, future efforts should systematically investigate the utility/prophylactic benefit of these services over time. In the interim, such findings suggest that practitioners involved in the assessment of ADHD in preschool children (e.g., pediatricians and psychologists) should look past simple symptom and/or diagnostic profiles and also consider referrals for adjunctive evaluations and/or services, many of which may be provided through the public school system.
In summary, preschool children with ADHD utilize significantly more services and exact a significantly greater cost than their typically developing counterparts. Examining the utilization and associated cost of these services may assist policy makers and shed light on how to distribute limited financial resources to ensure service needs are met.
Funding
National Institutes of Health (R01 MH068286-05, to J.M.H).
Conflicts of interest: None declared.
Acknowledgments
The authors wish to acknowledge the valuable contributions of Katia Castelli, Bipasha Basu, and Taneka Wellington. During the preparation of this manuscript, Dr Chacko was supported by a Klingenstein Third Generation ADHD Fellowship.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed., Text Revision). Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Armstrong MB, Nettleton SK. Attention deficit hyperactivity disorder and preschool children. Seminars in Speech and Language. 2004;25:225–232. doi: 10.1055/s-2004-833670. [DOI] [PubMed] [Google Scholar]
- Arons BS, Katz-Leavy J, Wittig AC, Holden WE. Too young for ADHD: The potential role of system of care. Developmental and Behavioral Pediatrics. 2002;23:57–63. doi: 10.1097/00004703-200202001-00010. [DOI] [PubMed] [Google Scholar]
- Barkley RA. Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment (3rd ed.). New York: Guilford; 2006. [Google Scholar]
- Barkley RA, Fisher, M. Edelbrock CS, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria: I. An 8-year prospective follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry. 1990;29(4):546–557. doi: 10.1097/00004583-199007000-00007. [DOI] [PubMed] [Google Scholar]
- Barry TD, Lyman RD, Klinger LG. Academic underachievement and attention-deficit/hyperactivity disorder: The negative impact of symptom severity on school performance. Journal of School Psychology. 2002;40:259–283. [Google Scholar]
- Birnbaum HG, Kessler RC, Lowe SW, Secnik K, Greenberg PE, Leong SA, et al. Costs of attention deficit-hyperactivity disorder (ADHD) in the US: Excess costs of persons with ADHD and their family members in 2000. Current Medical Research and Opinion. 2005;21(2):195–205. doi: 10.1185/030079904X20303. [DOI] [PubMed] [Google Scholar]
- Bussing R, Zima BT, Perwien AR, Belin TR, Widawski M. Children in special education program: Attention deficit hyperactivity disorder, use of services, and unmet needs. American Journal of Public Health. 1998;88(6):880–886. doi: 10.2105/ajph.88.6.880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan E, Zhan C, Homer CJ. Health care use and costs for children with attention-deficit/hyperactivity disorder. Archives of Pediatric Medicine. 2002;156:504–511. doi: 10.1001/archpedi.156.5.504. [DOI] [PubMed] [Google Scholar]
- Conner DF. Preschool attention deficit hyperactivity disorder: A review of prevalence, diagnosis, neurobiology, and stimulant treatment. Developmental and Behavioral Pediatrics. 2002;23:S1–S9. doi: 10.1097/00004703-200202001-00002. [DOI] [PubMed] [Google Scholar]
- DuPaul GJ, McGoey KE, Eckert TL, VanBrankle J. Preschool children with attention-deficit/hyperactivity disorder: Impairments in behavioral, social, and school functioning. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(5):508–515. doi: 10.1097/00004583-200105000-00009. [DOI] [PubMed] [Google Scholar]
- DuPaul GJ, Power TJ, Anastopoulus AD, Reid R. ADHD Rating Scale IV: Checklists, norms, and clinical interpretation. New York: Guildford; 1998. [Google Scholar]
- Forness SR, Kavale KA. Impact of ADHD on school systems. In: Jensen PS, Cooper JR, editors. Attention deficit hyperactivity disorder: State of the science—best practices. Kingston, NJ: Civic Research Institute; 2002. pp. 24–1. [Google Scholar]
- Guevara J, Lozano P, Wickizer T, Mell L, Gephart H. Utilization and cost of health care services for children with attention-deficit/hyperactivity disorder. Pediatrics. 2001;108:71–78. doi: 10.1542/peds.108.1.71. [DOI] [PubMed] [Google Scholar]
- Healey DM, Miller CJ, Castelli KL, Marks DJ, Halperin JM. The impact of impairment criteria on rates of ADHD diagnoses in preschoolers. Journal of Abnormal Child Psychology. 2008;36:771–778. doi: 10.1007/s10802-007-9209-1. [DOI] [PubMed] [Google Scholar]
- Hinshaw S. Externalizing behavior problems and academic underachievement in childhood and adolescence: Causal relationships and underlying mechanisms. Psychological Bulletin. 1992;111:127–155. doi: 10.1037/0033-2909.111.1.127. [DOI] [PubMed] [Google Scholar]
- Hoagwood K, Kelleher JK, Feil M, Comer DM. Treatment services for children with ADHD: A national perspective. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39(2):198–206. doi: 10.1097/00004583-200002000-00020. [DOI] [PubMed] [Google Scholar]
- Iwanaga R, Ozawa H, Kawasaki C, Tsuchida R. Characteristics of the sensory-motor, verbal and cognitive abilities of preschool boys with attention deficit/hyperactivity disorder combined type. Psychiatric and Clinical Neurosciences. 2006;60:37–45. doi: 10.1111/j.1440-1819.2006.01458.x. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for affective disorders and schizophrenia for school-age children–present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:1065–1069. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Ryan N. The schedule for affective disorders and schizophrenia for school-age children and lifetime version (version 1.0). Pittsburgh, PA: Department of Psychiatry, University of Pittsburgh School of Medicine; 1996. [DOI] [PubMed] [Google Scholar]
- Keenan K, Shaw DS, Walsh B, Delliquadri E, Giovannelli J. DSM-III-R disorders in preschool children from low-income families. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:620–627. doi: 10.1097/00004583-199705000-00012. [DOI] [PubMed] [Google Scholar]
- Kelleher KJ. Paper presented at the NIH Consensus Development Conference on Diagnosis and Treatment of Attention Deficit Hyperactivity Disorder, Bethesda, MD. 1998. Nov, Use of services and costs for youth with ADHD and related conditions. [Google Scholar]
- Kelleher KJ, Childs GE, Harman JS. Health care cost for children with attention-deficit hyperactivity disorder. Economics of Neuroscience. 2001;3:60–63. [Google Scholar]
- Kendall J, Leo MC, Perrin P, Hatton D. Service needs of families with children with ADHD. Journal of Family Nursing. 2005;11:264–288. doi: 10.1177/1074840705278629. [DOI] [PubMed] [Google Scholar]
- Lavigne JV, Gibbons RD, Christoffel K, Arend R, Rosenbaum D, Binns H, et al. Prevalence rates and correlates of psychiatric disorders among preschool children. Journal of American Academy of Child Adolescent Psychiatry. 1996;35(2):204–214. doi: 10.1097/00004583-199602000-00014. [DOI] [PubMed] [Google Scholar]
- Leslie LK, Wolraich ML. ADHD service use patterns in youth. Journal of Pediatric Psychology. 2007;32(6):695–710. doi: 10.1093/jpepsy/jsm023. [DOI] [PubMed] [Google Scholar]
- Loe IM, Feldman HM. Academic and educational outcomes of children with ADHD. Journal of Pediatric Psychology. 2007;32(6):643–654. doi: 10.1093/jpepsy/jsl054. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Klein RG, Bessler A, Malloy P, LaPadula M. Adult psychiatric status of hyperactive boys grown up. American Journal of Psychiatry. 1998;155:493–498. doi: 10.1176/ajp.155.4.493. [DOI] [PubMed] [Google Scholar]
- Miller CJ, Marks DJ, Miller SR, Berwid OG, Kera EC, Santra A, et al. Brief report: Television viewing and risk for attention problems in preschool children. Journal of Pediatric Psychology. 2007;32:448–452. doi: 10.1093/jpepsy/jsl035. [DOI] [PubMed] [Google Scholar]
- New York City Department of Education. School based expenditure reports school year 2004–2005 citywide. 2006 Retrieved July 3, 2008, from http://www.nycenet.edu/offices/d_chanc_oper/budget/exp01/y2004_2005/function.asp?R=2.
- New York City Department of Education. 2008–2009 rate schedule for independent providers of related services for New York City Preschool Students. 2008 Retrieved July 3, 2008, from http://schools.nyc.gov/NR/rdonlyres/1840EAB3-82DD-4630-A307-F98213F24032/38764/200708IRSPAGREEMENTINDIVIDUAL.pdf.
- Pelham WE, Foster EM, Robb JA. The economic impact of attention-deficit/hyperactivity disorder in children and adolescents. Journal of Pediatric Psychology. 2007;32(6):711–727. doi: 10.1093/jpepsy/jsm022. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Census 2000. Retrieved March 20, 2008, from http://www.census.gov/prod/cen2000/dp1/2kh00.pdf.
- Wechsler D. San Antonio, TX: Psychological Corporation; 2006. Wechsler preschool and primary scale of intelligence (3rd ed.) [Google Scholar]
- Yochman A, Ornoy A, Parush S. Co-occurrence of developmental delays among preschool children with attention-deficit-hyperactivity disorder. Developmental Medicine and Child Neurology. 2006;48:483–488. doi: 10.1017/S0012162206001034. [DOI] [PubMed] [Google Scholar]
- Yu SM, Huang ZJ, Schwalberg RH, Nyman RM. Parental English proficiency and children's health services access. American Journal of Public Health. 2006;96(8):1449–1455. doi: 10.2105/AJPH.2005.069500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zito JM, Safer DJ, dosReis S, Gardner JF, Boles M, Lynch F. Trends in the prescribing of psychotropic medications to preschoolers. Journal of the American Medical Association. 2000;283(8):1025–1030. doi: 10.1001/jama.283.8.1025. [DOI] [PubMed] [Google Scholar]