Abstract
Context
Hip function has been proposed to be related to low back pain (LBP) because of the anatomical proximity of the hip and lumbopelvic region. To date, findings have been inconclusive, possibly because the samples studied were heterogeneous. Sub-grouping samples based on characteristics such as activity demand, LBP classification, and sex might clarify research findings.
Objective
To describe and summarize studies that examine 3 factors proposed to be important to the study of the hip–LBP relationship.
Design
Review of cross-sectional studies.
Setting
Academic healthcare center and research laboratory.
Subjects
3 groups: athletes with a history of LBP who regularly participate in rotation-related sports, athletes without a history of LBP who are active but do not regularly participate in rotation-related sports, and athletes without a history of LBP who participate in rotation-related sports.
Main Outcome
Hip range of motion and hip–lumbopelvic region coordination.
Measures
Hip range of motion was measured with an inclinometer. Coordination was examined based on kinematics obtained with a 3-dimensional motion-capture system.
Result
Differences among groups were found based on activity demand, LBP classification, and sex.
Conclusion
When assessing athletes with and without LBP, characteristics such as activity demand, LBP classification, and sex should be considered.
Keywords: classification, gender, sex, activity
Various sport-related activities have been associated with a high incidence of low back pain (LBP).1–4 Despite this high incidence, the etiology of LBP is poorly understood. Knowledge of factors that might contribute to LBP could facilitate the development of more effective treatment. Hip function has been proposed to be related to LBP because of the anatomical proximity of the hip and the lumbopelvic region.
A number of investigators interested in LBP have examined the relationship between the hip and the lumbopelvic region.5–15 The primary focus of these studies has been on the relationship between LBP and (1) the amount of active or passive hip range of motion (ROM)5,7–10,16–18 and (2), to a lesser extent, the coordination of hip and back movement during clinical tests, such as forward bending,19,20 as well as functional movements such as sit-to-stand.21,22
A basic assumption of studies of the hip–LBP relationship is that suboptimal function of the hip might result in an alteration of the mechanics of the lumbopelvic region. Such alterations are proposed to contribute to low-magnitude loading of the lumbopelvic region and accumulation of tissue stress that, over time, contributes to tissue injury. For example, limited hip-rotation ROM resulting from shortened muscles, a stiff joint capsule, or a bony abnormality might contribute to compensatory movement in the lumbopelvic region. Such compensation could result in the lumbopelvic region’s moving more often during activities that require hip rotation, such as a golf swing or a racquet stroke. Altered coordination of hip and lumbopelvic-region movement could also result in an increase in lumbopelvic-region movement even when hip ROM is not limited. For example, during a test of active hip lateral rotation, the lumbopelvic region might move early in the hip motion secondary to altered hip- and trunk-muscle-recruitment patterns. In both examples, the increase in lumbopelvic-region movement could contribute to an increase in low-magnitude loading of tissue, microtrauma, LBP symptoms, and potentially macrotrauma.23–25
A number of studies of the hip–LBP relationship have been conducted. As a whole, the findings from these studies suggest there might be a relationship between hip function and LBP. The specific nature of the relationship, however, remains unclear. From our perspective a key reason for the inconclusive findings across studies is that important factors contributing to heterogeneity of the study samples have not been adequately taken into account. The design of a study can be improved by including subjects who are homogeneous with regard to clinically relevant characteristics and by accounting for such characteristics in the study analysis. Identifying and incorporating such factors into the design of these studies should result in a better understanding of the hip–LBP relationship. We consider 3 factors to be of particular importance to improving the sample selection, and, thus, the design of studies of the hip–LBP relationship.
The first important factor that has received minimal attention in prior studies is the demand of the activity in which subjects participate on the hip and lumbopelvic region. In the current context, demand includes the type of activity, as well as the frequency, duration, and intensity of participation. For example, an activity typically places specific directional demands on different segments for satisfactory performance. Those who play golf, a sport that requires adequate hip-rotation ROM, might be particularly at risk for LBP if their hip rotation is limited. Frequency, duration, and intensity of participation likely interact with the directional demand put on the hip and lumbopelvic region to determine whether hip function is an important contributing factor to LBP.
A second important factor that has not been previously considered in studies of the hip–LBP relationship is the need to classify people with LBP. The rationale for classification is that people with nonspecific LBP are a heterogeneous group, consisting of several smaller homogeneous subgroups. A number of classification systems have been described that use mechanical and pain-related variables to subgroup people with LBP.23,26–30 Data also have emerged over the last 10 years to validate the existence of some of the described subgroups. It is possible that the relationship of hip function and LBP might vary in different subgroups of people with LBP.
A final factor we consider important is the sex distribution of the study sample. Sex differences have been described, including differences in anatomy,31,32 hormonal influences,32 muscle properties,33–41 and recruitment patterns.42–45 Specific to the spine, sex differences have been found in muscle-related factors34,38 and hip–low back movement patterns during gait and reaching activities44,45 Such differences between men and women have the potential to contribute to variation in the kinematics, kinetics, and coordination of the hip and lumbopelvic region. Thus, the presence of a relationship between hip function and LBP, as well as the nature of the relationship, might be different for men and women.
We have performed a set of studies that incorporate the 3 factors described.46–49 A key feature of all studies is the examination of a cohort of athletes with a history of LBP who regularly perform rotation-related sports at the recreational level. A rotation-related sport is defined as one that requires repeated rotation of the hips and trunk to perform most aspects of the activity (eg, tennis, racquetball). Subjects also participated in their sport a minimum of 2 times per week and reported an increase in their LBP either during or after play. Such a cohort provides a model for testing the relationship of hip function and LBP in athletes who repeatedly place specific directional demands on the hip and trunk. We compare the athletes with a history of LBP with 2 groups: athletes without a history of LBP who are active but do not regularly participate in rotation-related sports and athletes without a history of LBP who participate in a rotation-related sport.
The purpose of this review is to describe some of the studies we have conducted in the 3 different groups of athletes. Across the various studies we take into account the 3 factors outlined. The studies focus on the relationship between LBP and hip ROM, as well as aspects of coordination of hip and lumbopelvic-region movement. Across studies we use the following measures: self-report questionnaires, a standardized clinical examination, and a 3-dimensional motion-capture system. The self-report questionnaires include demographics, sport-related, and LBP-history information; a numeric rating scale of symptoms50; the Oswestry Disability Index51; and the Baecke Habitual Activity questionnaire.52 We will also describe our future directions in the study of hip function and LBP.
Hip ROM
Hip ROM has been studied in people with LBP because a limitation in hip motion could alter the mechanical forces on the lumbopelvic region and, as a result, contribute to LBP. In particular, a number of prior studies focused on the relationship between active or passive hip-rotation ROM and LBP.5,7–10,16–18 The findings from these hip-rotation-LBP studies varied, with some investigators reporting a relationship between hip-rotation ROM and LBP5,8,9 and others reporting no relationship.7 Few of these prior studies, however, considered the repeated directional demands placed on the hip by activities in which the study samples were involved. We propose that hip-rotation ROM might be related to LBP in people who repeatedly place rotational demands on the hip. For example, people who participate in an activity that requires repeated hip rotation might be at higher risk for LBP than those who do not repeatedly place these specific directional demands on the hip. We also propose that if people who require repeated hip rotation have a limitation in hip-rotation ROM, their risk for LBP would be increased.
We tested these proposals in our cohort of athletes, comparing a group with a history of LBP with a group without a history of LBP. We focused on hip-rotation ROM for a number of reasons. First, across prior studies it appears there might be a relationship between hip-rotation ROM and LBP.5,7–10,16–18 Second, an asymmetry in hip-rotation ROM would result in an asymmetry in the forces transmitted to the lumbopelvic region. Such asymmetry in lumbopelvic-region forces has been identified as a risk factor for LBP.25,53 Third, a potential compensation for limited hip rotation is an increase in lumbopelvic-rotation motion. Frequent trunk rotation has been identified as a risk factor for LBP.53–56 Finally, small amounts of repeated rotation have been found to produce microscopic injury to spinal structures.57
Passive Hip-Rotation ROM and LBP
To examine the relationship between passive hip-rotation ROM and LBP, we recruited people who participated in rotation-related sports.48 Subjects were divided into 2 groups, athletes without a history of LBP (17 men and 7 women; mean age 26.96, SD = 7.74) and athletes with a history of chronic58 or recurrent58 LBP (18 men and 6 women; mean age 26.17, SD = 7.27).
Passive hip-rotation ROM was measured bilaterally. Subjects were tested in prone with the knee flexed to 90° and a belt stabilizing the pelvis. Using a fluid-filled inclinometer, we obtained 3 passive hip medial- and lateral-rotation measures. Measurements were compared between the 2 groups.
Subjects with and without a history of LBP were similar in all demographic, sport-related, and activity-related variables. As predicted, the only difference in the 2 groups was the amount of available passive hip-rotation ROM. Specifically, the LBP group demonstrated less total hip-rotation ROM than the group without LBP (LBP mean 54.15°, SD = 2.51°; no LBP mean 61.21°, SD = 1.78°; P = .03). Subjects with a history of LBP also demonstrated a difference in total rotation between left and right lower extremities (right mean 56.84°, SD = 2.75°; left mean 51.55°, SD = 2.50°; P = .004) that was not present in the subjects without a history of LBP (right mean 60.26°, SD = 2.03°; left mean 62.17°, SD = 1.20°; P = .31). Specifically, total left hip rotation was less than total right hip rotation in the subjects with a history of LBP.
The data from this study suggest that the specific directional demands imposed on the hip during regularly performed activities might be related to an athlete’s LBP problem. In particular, when an activity required full hip-rotation ROM for adequate performance, the subjects with a history of LBP were also those who displayed limitations in hip rotation. These findings are important because they suggest that the directional demands of the activity in which a person participates repeatedly should be a consideration in both rehabilitation and prevention strategies. In particular, the directional demands should be a factor when deciding which impairments are most relevant to examine and address in rehabilitation and might be potential risk factors when screening athletes for a particular sports activity.
Coordination
To better understand the hip–LBP relationship some investigators have examined the coordination of the hip and lumbopelvic region during trunk movements19,20 and, to a lesser degree, functional movements.21,22 To our knowledge, however, no studies have focused on coordination during lower-limb-movement tests. Coordination in the current context includes the sequencing, timing, and grading of segmental movements to achieve an overall movement goal.59 We propose that an alteration in any aspect of coordination can result in a change in the normal mechanics of the lumbopelvic region. Altered mechanics can contribute to areas of high tissue loading and, if persistent, might contribute to LBP symptoms. We consider these coordination issues with limb movements particularly important because we have found that people often report an increase in LBP symptoms during active lower-limb-movement tests,60 and the symptoms are often associated with changes in aspects of movement coordination.61 Furthermore, when movement coordination is modified during the limb movements, LBP symptoms are decreased.62,63 Because of the repetitive nature of limb movements during everyday activities, altered coordination in the lumbopelvic region with limbmovement tests would suggest the need to assess the coordination of the lumbopelvic region with everyday activities.
We describe the findings from 3 studies in which we examined coordination of hip and lumbopelvic-region movement. In each of these studies, we indexed aspects of the coordination of the hip and lumbopelvic region with kinematic measures. The limb-movement tests examined are hip lateral rotation (HLR) and knee flexion (KF), each performed in prone. The outcomes measured during the HLR test included maximum hip lateral rotation and lumbopelvic rotation, the difference in time between the start of hip and lumbopelvic motions (timing variable), and the percentage of lumbopelvic rotation achieved at 60% of the hip lateral-rotation motion (grading of movement variable). Outcomes measured during the KF test included maximum KF, maximum lumbopelvic rotation in the horizontal plane, maximum lumbopelvic anterior tilt in the sagittal plane, and the difference in time between the start of knee motion and each lumbopelvic motion (timing variables).
Timing of Movement: Athletes With and Without a History of LBP
One aspect of coordination considered important to LBP is the timing of movement of the lumbopelvic region, in particular, early lumbopelvic movement during a limb movement. The proposal is that if the lumbopelvic region moves early in a limb movement, the frequency of lumbopelvic movement might increase across the day. The increased frequency could contribute to accumulation of tissue stress in the lumbopelvic region and, eventually, LBP symptoms. Our studies based on clinical measures indicate that many people with LBP display the early lumbopelvic-movement pattern with limb movements.62 We did not know, however, whether the pattern was specific to people with LBP. We compared our LBP group (22 men, 19 women; mean age 28.2, SD = 8.1) with our group without a history of LBP (32 men, 18 women; mean age 27.9, SD = 7.4) who were active but did not regularly participate in rotation-related sports.49 We predicted that, compared with subjects without a history of LBP, subjects with a history LBP would display earlier lumbopelvic movement during the limb-movement tests.
Subjects were positioned with the hip in neutral abduction and adduction and neutral rotation. For the HLR test, the knee was positioned in 90° of flexion. Subjects were instructed to move as far as they could in each lower extremity test while kinematics were collected.
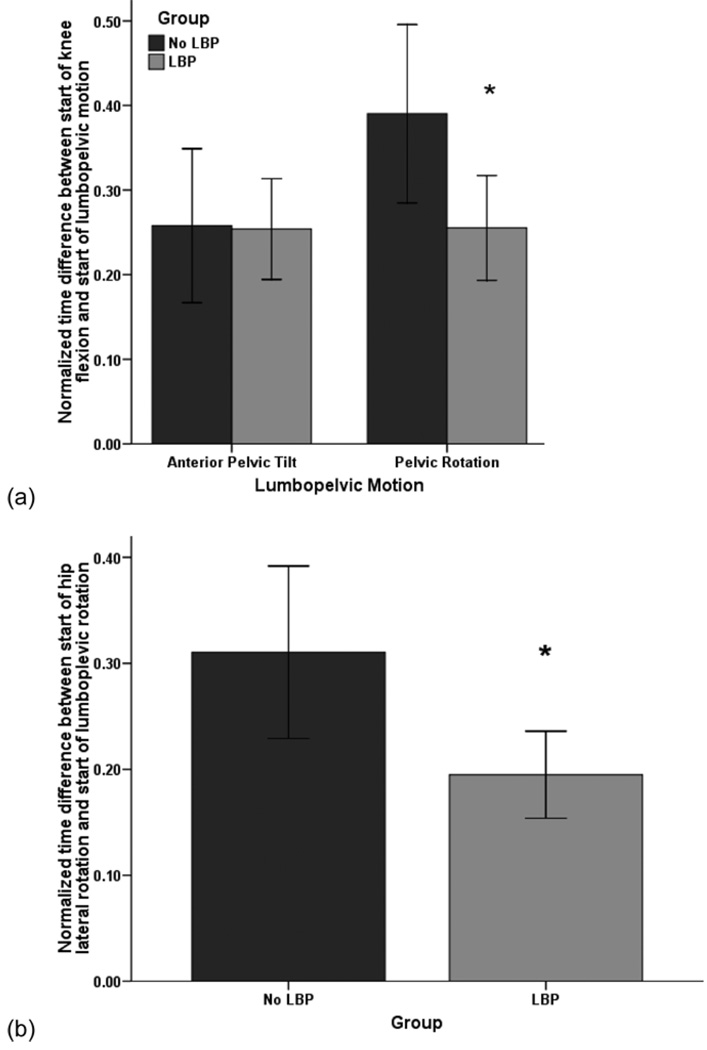
The groups were the same with regard to demographic, sport-related, and activity-related variables. Overall, compared with the subjects without a history of LBP, those with a history of LBP moved the lumbopelvic region earlier during both lower-limb-movement tests (Figure 1[a] and 1[b]). In addition, the early movement was lumbopelvic rotation. There were no differences between the groups for timing of lumbopelvic tilt during KF (Figure 1[a]). The groups were the same with regard to maximal HLR angle (LBP mean 44.3°, SD = 6.4°; no LBP mean 41.6°, SD = 6.6°; P = .52). The group without a history of LBP displayed a greater maximal KF angle than the group with a history of LBP (LBP mean 114.3°, SD = 8.6°; no LBP mean 120.0°, SD = 9.3°; P = .003). The LBP group displayed a greater maximal lumbopelvic-rotation angle than the subjects without a history of LBP in both lower-limb-movement tests (HLR: LBP mean 5.8°, SD = 3.0°; no LBP mean 4.5°, SD = 2.5°; P = .02; KF: LBP mean 3.2°, SD = 1.7°; no LBP mean 2.3°, SD = 1.5°; P = .009).
Figure 1.
(a) Difference in start time of knee flexion and lumbopelvic motion during the test of knee flexion for people with a history of low back pain (LBP) and people without a history of low back pain (no LBP). *Significant difference between groups, P = .009. (b) Difference in start time of hip lateral rotation and lumbopelvic motion during the hip lateral-rotation test for people in the LBP group and the no-LBP group. *Significant difference between groups, P = .02.
The data from this study suggest that the specific directional demands of a regular activity might contribute to direction-specific changes in hip and lumbopelvic-region coordination. Compared with those without a history of LBP, those with a history of LBP displayed earlier lumbopelvic motion during both limb movements, and the movement was rotation. These findings are important because limb-movement tests might index how people move during everyday activities. Because most everyday movements are performed in early and midranges of motion, the frequency of lumbopelvic-region motion across the day might be increased in people with LBP, particularly when the motion is always in the same direction. Thus, when designing a management strategy for athletes with LBP, one should consider the directional demand of a person’s regular activities and the potential impact of activity demands on timing of motion of the hip and lumbopelvic region during all activities.
Timing of Movement: LBP Subgroups
The differences between people with and without LBP suggest that the identified movement patterns might be specific to people with LBP, in particular, people who put regular rotational demands on the hip and trunk. It is possible, however, that the lumbopelvic-movement patterns vary with different subgroups of people with LBP. We classify people with LBP into subgroups based on the Movement System Impairment (MSI) classification system.23,26,27,47,60,62–64 The basis for classification is the symptoms and signs with tests that appear to contribute to the LBP problem.23 The reliability of examiners64 to classify a patient’s LBP has been reported to be moderate to substantial (k = .57–.75).26,65,66 The subgroups include lumbar rotation, lumbar extension, lumbar flexion, lumbar extension with rotation, and lumbar flexion with rotation. We have observed on examination that the lumbar-rotation (Rot) subgroup tends to display symmetric movement patterns, whereas the lumbar-extension-with-rotation (ExtRot) subgroup tends to display asymmetric movement patterns. We predicted that, compared with the ExtRot subgroup, the Rot subgroup would display more symmetry in coordination (right vs left) of timing of hip and lumbopelvic-region motion.
Subjects included athletes with a history of LBP classified into the Rot subgroup (6 men, 7 women; mean age 29.0, SD = 7.9) and into the ExtRot subgroup (17 men, 9 women; mean age 27.7, SD = 8.2).47 The methods46 of testing and the timing variable with HLR were the same as previously described. To examine symmetry of coordination, we examined the correlation between the timing-variable values for right and left HLR, for each LBP subgroup. The larger the correlation the more symmetry there was in coordination of timing of movement of the hip and lumbopelvic region (right vs left) during the HLR test.
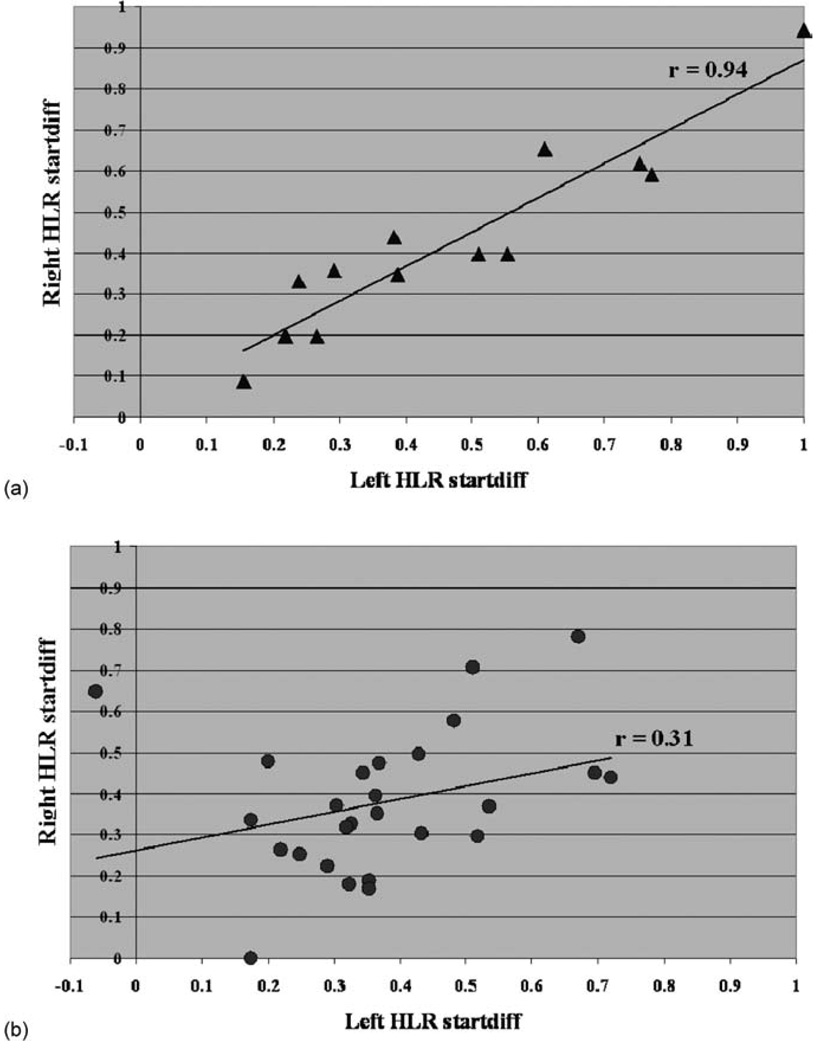
The subgroups were the same with regard to demographic, anthropometric, and activity- and LBP-related variables. There were no differences between the 2 LBP subgroups in maximum hip lateral-rotation (ExtRot mean 44.15°, SD = 1.5° Rot mean 41.9°, SD = 2.10°; P = .40) and lumbopelvic-rotation angles (ExtRot mean 6.05°, SD = 0.7°; Rot mean 4.9°, SD = 0.9°; P = .55). As predicted, the subgroups differed in the coordination of hip and lumbopelvic movement between sides. Subjects in the Rot subgroup demonstrated more symmetry in timing of lumbopelvic rotation during the HLR test (r = .94, P = .00) than the ExtRot subgroup (r = .31, P = .12; Figure 2[a] and 2[b]). Asymmetric timing of lumbopelvic movement indicates that the time when the lumbopelvic region begins to move during HLR is different for the right and left extremities.
Figure 2.
Difference in start time (startdiff) of lumbopelvic rotation (LPR) relative to start time of hip lateral rotation (HLR) during right and left HLR for people in 2 low-back-pain subgroups. Subjects in the lumbar-rotation (Rot) subgroup demonstrated more symmetry in timing of lumbopelvic rotation during the HLR test (r = .94, P = .00) than the lumbar-extension-with-rotation (ExtRot) subgroup (r = .31, P = .12). Startdiff is the difference in time between the start of HLR and LPR. Value was normalized to hip lateral-rotation movement time. (a) Relationship between right and left startdiff values for people in the Rot subgroup. (b) Relationship between right and left startdiff values for people in the ExtRot subgroup.
The data from this study suggest that when people with LBP are subgrouped, different patterns of movement coordination of the hip and lumbopelvic region become evident. In particular, timing of lumbopelvic motion during a hip movement is similar, right versus left, in people in the Rot subgroup. On the other hand, timing of lumbopelvic motion during a hip movement is different side to side in people in the ExtRot subgroup. The differences between subgroups also do not appear to be the result of differences in available hip or lumbopelvic ROM. These findings are important because they suggest that classifying a person’s LBP problem and determining the factors (neural and musculoskeletal) contributing to movement patterns that characterize a person’s LBP are important details to consider in designing a management strategy.
Grading of Movement: Men and Women With a History of LBP
The studies of coordination presented thus far suggest that overall, people with LBP tend to move the lumbopelvic region early during limb-movement tests. As seen in Figure 2(a) and 2(b), however, not all athletes with a history of LBP present with the described movement pattern. One factor that might be related to the movement pattern a person displays is sex. There are documented differences between men and women; in particular, men have greater active and passive stiffness of the lower limbs than women.35,36 We compared the lumbopelvic-movement pattern during HLR in men and women with a history of LBP. In this study we were interested in a different aspect of coordination: the grading of lumbopelvic-region movement during the hip movement. Grading in this context refers to the range through which a segment moves at points across the range of a task. We calculated the percent of lumbopelvic rotation that was attained at 60% of HLR. Considering the sex differences in lower limb stiffness, we predicted that men with a history of LBP would move through more of their lumbopelvic rotation than women at the 60% point of HLR. Thus, compared with women, men would achieve more of their lumbopelvic rotation range early in the HLR motion.
Subjects included 27 men (mean age 29.7, SD = 8.1) and 19 women (mean age 26.6, SD = 7.9) with a history of LBP who reported regular participation in rotation-related sports.46 The methods46 for HLR testing were the same as previously described.
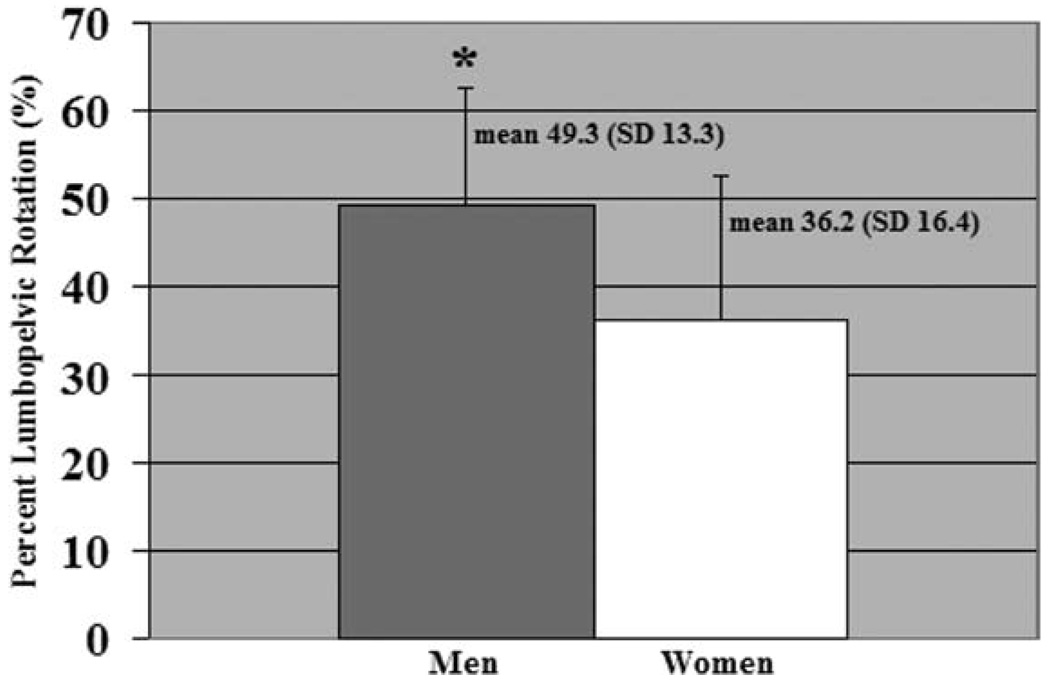
Compared with women, men were heavier and taller and had a slightly longer shank and spine length, a wider pelvis, and a longer history of LBP. When anthropometric measures were normalized to subject height, however, there were no sex differences in spine length (P = .86) or pelvic width (P = .87) and minimal differences in shank length (mean difference 0.01 cm, SD = 0.01; P < .01). There were no sex differences in amount of active hip lateral rotation (men’s mean 44.70°, SD = 7.1°; women’s mean 42.7°, SD = 5.2°; P = .29) or lumbopelvic rotation (men’s mean 6.1°, SD = 3.2°; women’s mean 4.6°, SD = 2.0°; P = .08). As predicted, men completed a greater percentage of their lumbopelvic rotation (mean 49.3%, SD = 13.3%) within the first 60% of HLR than women (mean 36.2%, SD = 16.4%; Figure 3).
Figure 3.
Gender differences in percent lumbopelvic rotation achieved from 0% to 60% of hip lateral rotation. *Significant difference between groups, P < .01.
The data from this study suggest that men and women with a history of LBP do not display the same movement patterns in a limb-movement test. Compared with women, men achieve more of their available lumbopelvic rotation early in the range of HLR. The sex differences also are not caused by differences in anthropometrics or amount of lumbopelvic or HLR motion. These findings are important because sex differences in movement patterns suggest potential differences in contributing factors (neural and musculoskeletal). Determining the nature of the contributing factors will assist in designing a management strategy to address factors that are modifiable and educate athletes about the factors that increase their risk for LBP.
Discussion
Based on prior studies it appears that there is a relationship between hip function and LBP, but the exact nature of the relationship remains unclear. We propose that the lack of clarity is, in part, a result of heterogeneity of the samples studied. To increase sample homogeneity we recommend subgrouping subjects on potentially relevant factors. The specific factors we have used to subgroup people thus far include activity demand, LBP classification, and sex.
The feature common to all of the studies reviewed is the examination of people with a history of LBP who repeatedly place specific rotational demands on the hip and trunk. The rationale is that a limitation in a specific hip function might more likely be related to LBP if the person regularly requires that aspect of hip function. To our knowledge only 1 other group of investigators has accounted for activity demand in examining the hip–LBP relationship. Vad et al13,14 reported that male professional tennis players and golfers with LBP were more limited in lead-hip medial rotation and the FABER test, which the authors described as an index of hip lateral-rotation ROM, than those without LBP. These results are similar to our findings in recreational-level athletes with LBP in that there is an asymmetry of hip rotation, right compared with left, in athletes with LBP versus athletes without LBP. Together these findings support the proposal that activity demands might interact with hip function to increase the risk of LBP. In addition, passive end-range hip motion might be most important to assess in athletes with LBP who participate in activities that require repeated end range of hip motion.
A primary focus of 2 of our studies of coordination was on whether lumbopelvic movement occurred early in the range of lower-limb-movement tests. We use the limb-movement tests during an examination as an index of potential movement coordination during functional activities. The proposal is that because people perform many daily activities in early to midranges of joint motion, the early motion might result in increased frequency of lumbopelvic-region movement across the day. Such an increase could contribute to accumulation of tissue stress in the lumbopelvic region and LBP symptoms, particularly if the movement is always in the same direction, with minimal time off for normal tissue adaptation.
Our athletes with a history of LBP displayed earlier lumbopelvic rotation during 2 lower limb movements than athletes without a history of LBP who did not perform a rotation-related sport. We also found that the early lumbopelvic-movement pattern during HLR differed when the athletes with a history of LBP were classified into subgroups. The Rot subgroup displayed a more symmetric hip- and lumbopelvic-movement pattern (right and left moved similarly) than the ExtRot subgroup. Thus, subgrouping people with LBP provides additional information about alterations in movement coordination that would not be apparent if the athletes with a history of LBP were examined as 1 group. A difference in patterns during the same test suggests that different contributing factors might need to be addressed during treatment. To our knowledge there are no other reports of movement coordination of the hip and lumbopelvic region between LBP subgroups.
A number of systems for subgrouping people with LBP have been described.23,26–30 In particular, the McKenzie (McK) LBP classification system,28 the Treatment-Based Classification (TBC) system,29,30 and the MSI system23,26,27 have been scientifically evaluated to some degree. Our current work suggests that 2 MSI subgroups differ in the coordination of hip and lumbopelvic movement between sides with active HLR. People in the ExtRot subgroup demonstrated a greater asymmetry in timing of lumbopelvic rotation during the HLR test than did people in the Rot subgroup. To our knowledge neither the McK nor the TBC system includes tests of coordination of hip and lumbopelvic movement during active hip movements in the examination used for subgrouping. Thus, the differences we have identified between the ExtRot and Rot subgroups cannot be compared with differences between subgroups identified with the McK or TBC system.
In our third coordination study we examined the effect of sex on the hip- and lumbopelvic-movement pattern in our athletes with a history of LBP. Movement factors related to sex have been proposed. These include differences in anatomy,31,32 hormonal influences,32 muscle properties,33–41 and recruitment patterns.42–45 Specific to the spine, sex differences have been found in muscle-related factors34,38 and hip-low-back-movement patterns during gait and reaching activities44,45 Our study indicates that sex is an important factor to consider when studying the hip–LBP relationship. In our study,46 compared with women, men achieved a greater percentage of their lumbopelvic rotation within the first 60% of HLR. Thus, men are moving their lumbopelvic region at a faster rate than women during a limb movement. Such findings suggest that men and women might have different movement-related factors that contribute to their LBP.
One direction of our future research will be to examine the factors that contribute to the identified movement patterns in athletes with a history of LBP. Of particular interest is the contribution of neural-control and musculoskeletal factors and how these factors might interact. Neural-control factors of interest include timing and magnitude of recruitment of the hip and trunk muscles. These neural factors will be assessed during test movements, as well as specific functional activities. Musculoskeletal factors of interest include anthropometrics, joint extensibility, passive and active stiffness, structural differences such as bony variation of the pelvis and femur, and imbalances of strength and length of the trunk and hip muscles. We propose that the factors contributing to the identified movement patterns will vary. In some athletes the patterns might be solely the result of neural factors and in other athletes they might be the result of an interaction of neural and musculoskeletal factors. An understanding of contributing factors is important because it provides a rational basis for treatment and prevention strategies. A second direction of our research is to assess the prognostic value of the identified movement patterns to the development and course of LBP. We plan to follow a cohort of athletes longitudinally to examine risk factors for LBP, including hip- and lumbopelvic-movement patterns. The 3 factors described (demand, classification, and sex) would be important to assess.
Hip function is only 1 potential factor that might affect risk for LBP. There are likely multiple variables that need to interact with hip function to increase an athlete’s risk. We have outlined 3 factors that appear to be important to consider when examining the hip–LBP relationship. Awareness of such factors during assessment should help clinicians identify the most important variables to address in treating athletes with LBP and screening for injury risk. Targeting specific variables found to be related to LBP, among the many variables that potentially could be assessed, should improve the study of LBP, as well as improve efficiency of its examination and treatment.
Acknowledgments
The protocol used for the current study was approved by the Human Studies Committee of Washington University.
This work was supported by grant R01 HD047709 to Dr Van Dillen from the National Center for Medical Rehabilitation Research, National Institute of Child Health and Human Development, and grant K12 HD055931 to Dr Harris-Hayes from the National Center for Medical Rehabilitation Research, National Institute of Child Health and Human Development, and National Institute of Neurological Disorders and Stroke.
The authors would like to acknowledge Dave R. Collins, Sara A. Scholtes, and Sara P. Gombatto for their contributions to this work.
References
- 1.Chard MD, Lachmann SM. Racquet sports—patterns of injury presenting to a sports injury clinic. Br J Sports Med. 1987;21(4):150–153. doi: 10.1136/bjsm.21.4.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hosea TM, Gatt CJ., Jr Back pain in golf. Clin Sports Med. 1996;15(1):37–53. [PubMed] [Google Scholar]
- 3.McCarroll JR. The frequency of golf injuries. Clin Sports Med. 1996;15(1):1–7. [PubMed] [Google Scholar]
- 4.Sward L, Hellstrom M, Jacobsson B, Peterson L. Back pain and radiologic changes in the thoraco-lumbar spine of athletes. Spine. 1990;15(2):124–129. doi: 10.1097/00007632-199002000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Fairbank JC, Pynsent PB, Van Poortvliet JA, Phillips H. Influence of anthropometric factors and joint laxity in the incidence of adolescent back pain. Spine. 1984;9(5):461–464. doi: 10.1097/00007632-198407000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Mellin G. Correlations of hip mobility with degree of back pain and lumbar spinal mobility in chronic low-back pain patients. Spine. 1988;13(6):668–670. [PubMed] [Google Scholar]
- 7.Ellison JB, Rose SJ, Sahrmann SA. Patterns of hip rotation range of motion: a comparison between healthy subjects and patients with low back pain. Phys Ther. 1990;70(9):537–541. doi: 10.1093/ptj/70.9.537. [DOI] [PubMed] [Google Scholar]
- 8.Mellin G. Decreased joint and spinal mobility associated with low back pain in young adults. J Spinal Disord. 1990;3(3):238–243. [PubMed] [Google Scholar]
- 9.Chesworth BM, Padfield BJ, Helewa A, Stitt LW. A comparison of hip mobility in patients with low back pain and matched healthy subjects. Physiother Can. 1994;46(4):267–274. [Google Scholar]
- 10.Cibulka MT, Sinacore DR, Cromer GS, Delitto A. Unilateral hip rotation range of motion asymmetry in patients with sacroiliac joint regional pain. Spine. 1998;23(9):1009–1015. doi: 10.1097/00007632-199805010-00009. [DOI] [PubMed] [Google Scholar]
- 11.Grimshaw PN, Burden AM. Case report: reduction of low back pain in a professional golfer. Med Sci Sports Exerc. 2000;32(10):1667–1673. doi: 10.1097/00005768-200010000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Coplan JA. Ballet dancer’s turnout and its relationship to self-reported injury. J Orthop Sports Phys Ther. 2002;32(11):579–584. doi: 10.2519/jospt.2002.32.11.579. [DOI] [PubMed] [Google Scholar]
- 13.Vad VB, Gebeh A, Dines D, Altchek D, Norris B. Hip and shoulder internal rotation range of motion deficits in professional tennis players. J Sci Med Sport. 2003;6(1):71–75. doi: 10.1016/s1440-2440(03)80010-5. [DOI] [PubMed] [Google Scholar]
- 14.Vad VB, Bhat AL, Basrai D, Gebeh A, Aspergren DD, Andrews JR. Low back pain in professional golfers: the role of associated hip and low back range-of-motion deficits. Am J Sports Med. 2004;32(2):494–497. doi: 10.1177/0363546503261729. [DOI] [PubMed] [Google Scholar]
- 15.Wong TK, Lee RY. Effects of low back pain on the relationship between the movements of the lumbar spine and hip. Hum Mov Sci. 2004;23(1):21–34. doi: 10.1016/j.humov.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 16.Cibulka MT. Low back pain and its relation to the hip and foot. J Orthop Sports Phys Ther. 1999;29(10):595–601. doi: 10.2519/jospt.1999.29.10.595. [DOI] [PubMed] [Google Scholar]
- 17.Childs JD, Fritz JM, Flynn TW, et al. A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulation: a validation study. Ann Intern Med. 2004;141(12):920–928. doi: 10.7326/0003-4819-141-12-200412210-00008. [DOI] [PubMed] [Google Scholar]
- 18.Flynn T, Fritz J, Whitman J, et al. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine. 2002;27(24):2835–2843. doi: 10.1097/00007632-200212150-00021. [DOI] [PubMed] [Google Scholar]
- 19.Esola MA, McClure PW, Fitzgerald GK, Siegler S. Analysis of lumbar spine and hip motion during forward bending in subjects with and without a history of low back pain. Spine. 1996;21(1):71–78. doi: 10.1097/00007632-199601010-00017. [DOI] [PubMed] [Google Scholar]
- 20.Porter JL, Wilkinson A. Lumbar-hip flexion motion. a comparative study between asymptomatic and chronic low back pain in 18- to 36-year-old men. Spine. 1997;22(13):1508–1513. doi: 10.1097/00007632-199707010-00017. [DOI] [PubMed] [Google Scholar]
- 21.Shum GL, Crosbie J, Lee RY. Three-dimensional kinetics of the lumbar spine and hips in low back pain patients during sit-to-stand and stand-to-sit. Spine. 2007;32(7):E211–E219. doi: 10.1097/01.brs.0000259204.05598.10. [DOI] [PubMed] [Google Scholar]
- 22.Shum GL, Crosbie J, Lee RY. Effect of low back pain on the kinematics and joint coordination of the lumbar spine and hip during sit-to-stand and stand-to-sit. Spine. 2005;30(17):1998–2004. doi: 10.1097/01.brs.0000176195.16128.27. [DOI] [PubMed] [Google Scholar]
- 23.Sahrmann SA. Diagnosis and Treatment on Movement Impairment Syndromes. St Louis, MO: Mosby; 2002. [Google Scholar]
- 24.McGill SM. The biomechanics of low back injury: implications on current practice in industry and the clinic. J Biomech. 1997;30:465–475. doi: 10.1016/s0021-9290(96)00172-8. [DOI] [PubMed] [Google Scholar]
- 25.Adams MA, Bogduk N, Burton K, Dolan P. The Biomechanics of Back Pain. Edinburgh, England: Churchill Livingstone; 2002. [Google Scholar]
- 26.Norton BJ, Sahrmann SA, Van Dillen FL. Differences in measurements of lumbar curvature related to gender and low back pain. J Orthop Sports Phys Ther. 2004;34(9):524–534. doi: 10.2519/jospt.2004.34.9.524. [DOI] [PubMed] [Google Scholar]
- 27.Van Dillen LR, Sahrmann SA, Norton BJ, et al. Movement system impairment-based categories for low back pain: stage I validation. J Orthop Sports Phys Ther. 2003;33(3):126–142. doi: 10.2519/jospt.2003.33.3.126. [DOI] [PubMed] [Google Scholar]
- 28.McKenzie RA. The Lumbar Spine: Mechanical Diagnosis and Therapy. Waikanae, New Zealand: Spinal; 2003. [Google Scholar]
- 29.Delitto A, Erhard RE, Bowling RW. A treatment-based classification approach to low back syndrome: identifying and staging patients for conservative treatment. Phys Ther. 1995;75:470–489. doi: 10.1093/ptj/75.6.470. [DOI] [PubMed] [Google Scholar]
- 30.Fritz JM, George S. The use of a classification approach to identify subgroups of patients with acute low back pain. interrater reliability and short-term treatment outcomes. Spine. 2000;25(1):106–114. doi: 10.1097/00007632-200001010-00018. [DOI] [PubMed] [Google Scholar]
- 31.Neumann DA. Kinesiology of the Musculoskeletal System: Foundations for Physical Rehabilitation. St Louis, MO: Mosby; 2002. [Google Scholar]
- 32.Hewett TE. Neuromuscular and hormonal factors associated with knee injuries in female athletes. strategies for intervention. Sports Med. 2000;29(5):313–327. doi: 10.2165/00007256-200029050-00003. [DOI] [PubMed] [Google Scholar]
- 33.Jorgensen MJ, Marras WS, Gupta P. Cross-sectional area of the lumbar back muscles as a function of torso flexion. Clin Biomech (Bristol, Avon) 2003;18(4):280–286. doi: 10.1016/s0268-0033(03)00027-5. [DOI] [PubMed] [Google Scholar]
- 34.Marras WS, Jorgensen MJ, Granata KP, Wiand B. Female and male trunk geometry: size and prediction of the spine loading trunk muscles derived from MRI. Clin Biomech (Bristol, Avon) 2001;16(1):38–46. doi: 10.1016/s0268-0033(00)00046-2. [DOI] [PubMed] [Google Scholar]
- 35.Blackburn JT, Riemann BL, Padua DA, Guskiewicz KM. Sex comparison of extensibility, passive, and active stiffness of the knee flexors. Clin Biomech (Bristol, Avon) 2004;19(1):36–43. doi: 10.1016/j.clinbiomech.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 36.Granata KP, Wilson SE, Padua DA. Gender differences in active musculoskeletal stiffness. part I. quantification in controlled measurements of knee joint dynamics. J Electromyogr Kinesiol. 2002;12(2):119–126. doi: 10.1016/s1050-6411(02)00002-0. [DOI] [PubMed] [Google Scholar]
- 37.Wojtys EM, Huston LJ, Schock HJ, Boylan JP, Ashton-Miller JA. Gender differences in muscular protection of the knee in torsion in size-matched athletes. J Bone Joint Surg Am. 2003;85A(5):782–789. doi: 10.2106/00004623-200305000-00002. [DOI] [PubMed] [Google Scholar]
- 38.Jorgensen MJ, Marras WS, Granata KP, Wiand JW. MRI-derived moment-arms of the female and male spine loading muscles. Clin Biomech (Bristol, Avon) 2001;16(3):182–193. doi: 10.1016/s0268-0033(00)00087-5. [DOI] [PubMed] [Google Scholar]
- 39.Chow RS, Medric MK, Martin DC, Leekam RN, Agur AM, McKee NH. Sonographic studies of human soleus and gastrocnemius muscle architecture: gender variability. Eur J Appl Physiol. 2000;82(3):236–244. doi: 10.1007/s004210050677. [DOI] [PubMed] [Google Scholar]
- 40.Staron RS, Hagerman FC, Hikida RS, et al. Fiber type composition of the vastus lateralis muscle of young men and women. J Histochem Cytochem. 2000;48(5):623–629. doi: 10.1177/002215540004800506. [DOI] [PubMed] [Google Scholar]
- 41.Toft I, Lindal S, Bonaa KH, Jenssen T. Quantitative measurement of muscle fiber composition in a normal population. Muscle Nerve. 2003;28(1):101–108. doi: 10.1002/mus.10373. [DOI] [PubMed] [Google Scholar]
- 42.Hewett TE, Myer GD, Ford KR. Decrease in neuromuscular control about the knee with maturation in female athletes. J Bone Joint Surg Am. 2004;86(8):1601–1608. doi: 10.2106/00004623-200408000-00001. [DOI] [PubMed] [Google Scholar]
- 43.Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003;35(10):1745–1750. doi: 10.1249/01.MSS.0000089346.85744.D9. [DOI] [PubMed] [Google Scholar]
- 44.Smith LK, Lelas JL, Kerrigan DC. Gender differences in pelvic motions and center of mass displacement during walking: stereotypes quantified. J Womens Health. 2002;11(5):453–458. doi: 10.1089/15246090260137626. [DOI] [PubMed] [Google Scholar]
- 45.Thomas JS, Corcos DM, Hasan Z. The influence of gender on spine, hip, knee, and ankle motions during a reaching task. J Mot Behav. 1998;30(2):98–103. doi: 10.1080/00222899809601327. [DOI] [PubMed] [Google Scholar]
- 46.Gombatto SP, Collins DR, Sahrmann SA, Engsberg JR, Van Dillen LR. Gender differences in pattern of hip and lumbopelvic rotation in people with low back pain. Clin Biomech (Bristol, Avon) 2006;21(3):263–271. doi: 10.1016/j.clinbiomech.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 47.Van Dillen LR, Gombatto SP, Collins DR, Engsberg JR, Sahrmann SA. Symmetry of timing of hip and lumbopelvic rotation motion in 2 different subgroups of people with low back pain. Arch Phys Med Rehabil. 2007;88(3):351–360. doi: 10.1016/j.apmr.2006.12.021. [DOI] [PubMed] [Google Scholar]
- 48.Van Dillen LR, Bloom NJ, Gombatto SP, Susco TM. Hip rotation range of motion in people with and without low back pain who participate in rotation-related sports. Phys Ther Sport. 2008;9(2):72–81. doi: 10.1016/j.ptsp.2008.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Scholtes Sara A, Gombatto Sara P, Van Dillen Linda R. Differences in lumbopelvic motion between people with and people without low back pain during two lower limb movement tests. Clin Biomech (Bristol, Avon) 2009;24:7–12. doi: 10.1016/j.clinbiomech.2008.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Ann Rheum Dis. 1978;37(4):378–381. doi: 10.1136/ard.37.4.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 52.Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36(5):936–942. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- 53.Marras WS, Lavender SA, Leurgans SE, et al. Biomechanical risk-factors for occupationally related low-back disorders. Ergonomics. 1995;38(2):377–410. doi: 10.1080/00140139508925111. [DOI] [PubMed] [Google Scholar]
- 54.Kelsey JL, Githens PB, White AA, et al. An epidemiologic study of lifting and twisting on the job and risk for acute prolapsed lumbar intervertebral disc. J Orthop Res. 1984;2(1):61–66. doi: 10.1002/jor.1100020110. [DOI] [PubMed] [Google Scholar]
- 55.Marras WS, Lavender SA, Leurgans SE, et al. The role of dynamic three-dimensional trunk motion in occupationally-related low back disorders. the effects of workplace factors, trunk position, and trunk motion characteristics on risk of injury. Spine. 1993;18(5):617–628. doi: 10.1097/00007632-199304000-00015. [DOI] [PubMed] [Google Scholar]
- 56.Skovron ML. Epidemiology of low back pain [review] Baillieres Clin Rheumatol. 1992;6(3):559–573. doi: 10.1016/s0950-3579(05)80127-x. [DOI] [PubMed] [Google Scholar]
- 57.Gordon SJ, Yang KH, Mayer PJ, Mace AH, Kish VL, Radin EL. Mechanism of disk rupture—a preliminary report. Spine. 1991;16(4):450–456. doi: 10.1097/00007632-199104000-00011. [DOI] [PubMed] [Google Scholar]
- 58.Von Korff M. Studying the natural history of back pain. Spine. 1994;19(18) Suppl:2041S–2046S. doi: 10.1097/00007632-199409151-00005. [DOI] [PubMed] [Google Scholar]
- 59.Shumway-Cook A, Woollacott MH. Motor Control: Translating Research Into Clinical Practice. Philadelphia, PA: Lippincott Williams & Wilkins; 2007. [Google Scholar]
- 60.Van Dillen LR, Sahrmann SA, Norton BJ, et al. Effect of active limb movements on symptoms in patients with low back pain. J Orthop Sports Phys Ther. 2001;31(8):402–413. doi: 10.2519/jospt.2001.31.8.402. [DOI] [PubMed] [Google Scholar]
- 61.Scholtes S, Gombatto S, Collins D, Sahrmann S, Van Dillen LR. Differences in lumbopelvic movement during knee flexion in prone between people with and without low back pain. Proceedings of the 6th Interdisciplinary World Congress on Low Back and Pelvic Pain; November 2007; Barcelona, Spain. [Google Scholar]
- 62.Van Dillen LR, Sahrmann SA, Norton BJ, Caldwell CA, McDonnell MK, Bloom NJ. The effect of modifying patient-preferred spinal movement and alignment during symptom testing in patients with low back pain: a preliminary report. Arch Phys Med Rehabil. 2003;84(3):313–322. doi: 10.1053/apmr.2003.50010. [DOI] [PubMed] [Google Scholar]
- 63.Van Dillen Linda R, Maluf Katrina S, Sahrmann Shirley A. Further examination of modifying patient-preferred movement and alignment strategies in patients with low back pain during symptomatic tests. Man Ther. doi: 10.1016/j.math.2007.09.012. In press. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Van Dillen LR, Sahrmann SA, Norton BJ, et al. Reliability of physical examination items used for classification of patients with low back pain. Phys Ther. 1998;78(9):979–988. doi: 10.1093/ptj/78.9.979. [DOI] [PubMed] [Google Scholar]
- 65.Trudelle-Jackson E, Sarvaiya-Shah SA, Wang SS. Interrater reliability of the movement-impairment based classification system for lumbar spine syndromes in patients with chronic low back pain. J Orthop Sports Phys Ther. 2008;38(6):371–376. doi: 10.2519/jospt.2008.2760. [DOI] [PubMed] [Google Scholar]
- 66.Harris-Hayes M, Van Dillen LR. The inter-tester reliability of physical therapists classifying low back pain problems based on the Movement System Impairment classification system. Phys Med Rehabil. doi: 10.1016/j.pmrj.2008.08.001. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]