Abstract
PURPOSE
To examine the challenges of recruiting women for a 5-year cardiac rehabilitation randomized clinical trial; the aims of the study were to describe the range of recruitment sources, examine the myriad of factors contributing to ineligibility and nonparticipation of women during protocol screening, and discuss the challenges of enrolling women in the trial.
METHODS
The Women’s-Only Phase II Cardiac Rehabilitation program used an experimental design with 2 treatment groups. Eligible participants included women who were (1) diagnosed with a myocardial infarction or stable angina or had undergone coronary revascularization within the last 12 months; (2) able to read, write, and speak English; and (3) older than 21 years. Responses to multiple recruitment strategies including automatic hospital referrals, physician office referrals, mass mailings, media advertisements, and community outreach are described. Reasons for ineligibility and nonparticipation in the trial are explored.
RESULTS
Automatic hospital order was the largest source of referral (n = 1,367, 81%) accounting for the highest enrollment rate of women (n = 184, 73%). The barriers to enrollment into the cardiac rehabilitation clinical trial included patient-oriented, provider-oriented, and programmatic factors. Of the referral sources, 52% were screened ineligible for provider-oriented reasons, 31% were ineligible due to patient-oriented factors, and 17.4% were linked to the study protocol. Study nonparticipation of those eligible (73.8%) was largely associated with patient-oriented factors (65.2%), with far less due to provider-related factors (4%) or study-related factors (3.4%).
CONCLUSION
Standing hospital orders facilitated enrollment to the cardiac rehabilitation clinical trial, yet women failed to participate predominantly due to significant patient-oriented biopsychosocial barriers.
Keywords: cardiac rehabilitation, coronary heart disease, randomized clinical trial, recruitment, women
Cardiac rehabilitation (CR), a multidisciplinary secondary prevention program of prescriptive exercise, comprehensive education, and psychologic counseling, produces well-documented reductions in coronary heart disease (CHD) risk factors, morbidity, and mortality.1–9 Despite compelling evidence for clinical, psychosocial, and economic benefits of CR, these services are profoundly underutilized after acute coronary syndromes, particularly for women and minorities. Participation rates among eligible women range from about 15% to 20%.6,10–16 The underutilization rates largely stem from low referral rates for women despite abundant scientific and clinical evidence of improved patient outcomes.7,8,11,17,18
Physician referral and endorsement is an acknowledged powerful predictor of CR participation,13,19–24 but suboptimal referrals of women are compounded by various patient-oriented, provider-oriented, and programmatic factors.6,16,25,26 Women particularly underrepresented in CR include the elderly, the obese, the depressed, nonwhites, and those with greater comorbidity, lower exercise capacity, less social support,6,14,17,26–28 and incomplete medical insurance coverage.29,30 Furthermore, researchers have identified mismatches between preferences and programmatic offerings for women eligible for CR,28,31–33 mismatches that largely remain today.
Women are as underrepresented in behavioral and risk reduction clinical trials as they are in CR programs. Typically high protocol burden and extensive time commitments required of many behavioral studies pose a significant barrier to participation. Gender role expectations necessitate creative recruitment efforts that are often underestimated. Given the integral role of efficient recruitment to the success of intervention trials, elucidating strategies that produce optimum recruitment yields for specific study populations may aid researchers in more accurately estimating recruitment costs and staff time. Although research methodology textbooks offer principles of sampling and recruitment plans, researchers planning similar research efforts could benefit from real world lessons learned during recruitment experiences of their peers. In this article, we describe the recruitment strategies used and the screening process for a 5-year randomized trial of 2 methods of delivering CR to women with CHD. The aims of this article were to (1) describe the range of study recruitment sources; (2) examine the myriad of factors contributing to ineligibility and nonparticipation of women during protocol screening; and (3) discuss the challenges of enrolling women in the clinical trial.
METHODS
Recruitment data of women within the Women’s-Only Phase II Cardiac Rehabilitation program were used in this study; the study design34 and baseline data of a subset of this cohort35 are described elsewhere. Briefly, an experimental design employed 2 treatment groups, both receiving a comprehensive, 12-week, CR program, with 1 group receiving a motivational behavioral enhancement exclusively for women with CHD. The hypothesis being tested is that women completing a gender-sensitive, behavior change intervention will demonstrate greater improvements in biopsychosocial outcomes compared with women attending a traditional or “usual care” CR program. It is additionally hypothesized that women completing the gender-sensitive intervention, compared with women attending the traditional CR program, will demonstrate greater maintenance of these improvements 6 months after program completion. The Institutional Review Boards of the university and the study hospital approved the study.
The cohort of women (older than 21 years of age) was drawn from those referred to a hospital-based outpatient CR program from January 2004 to March 2008. Inclusion criteria were (1) diagnosis of acute myocardial infarction, stable angina, or coronary artery bypass graft surgery or percutaneous coronary intervention within the last year; (2) able to read, write, and speak English; and (3) willing and able to participate. The exclusion criteria were (1) health insurance coverage for less than 36 electrocardiogram-monitored exercise sessions; (2) cognitive impairment; (3) inability to ambulate; or (4) insertion of an automatic internal cardiac defibrillator in the last year.
Recruitment Procedures to Identify Trial Participants
Multiple methods were employed to identify women eligible for both CR and this randomized clinical trial. Several strategies were extant in the study hospital including standing hospital orders, a phase I CR visit by an exercise physiologist prior to hospital discharge, provision of an education manual outlining risk factors for CHD and a CR information packet, and an appointment for phase II CR orientation. The research team implemented supplementary recruitment strategies that included development and distribution of recruitment brochures and posters, recruitment letters to relevant physician practices, community outreach initiatives, and media advertisements. Women referred to the CR program were scheduled for an individualized orientation conducted by the study recruiter.
Automatic Hospital Referrals
Women were recruited to CR, and then to the study, primarily through automatic physician standing orders in 1 community hospital. Whereas all cardiovascular surgical and cardiac catheterization laboratory patients had preprinted standing hospital orders for CR, other cardiology patients required a written physician order. The exercise physiologist facilitated referrals of cardiology patients by flagging the hospital chart for a referral request during hospital rounds. Consequently, CR referral rates of women from this source were equivalent to those from interventional cardiology and surgery.
Recruitment Materials
To expand the referral base beyond hospital standing orders, the research team designed recruitment brochures utilizing recommendations for photographs, colors, and wording from 8 women who had participated in the pilot study. The brochure, written at a sixth-grade level in collaboration with the university health media department, described the study inclusion criteria and schedule of activities, the potential benefits of participation, and contact information for the research team. The brochure targeted patients in physician waiting rooms; physician office practices were also encouraged to distribute brochures to outpatients with qualifying diagnoses within the prior year who had not previously participated in CR. Colorful posters advertising the study were also displayed in physician offices and the hospital foyer. The research team maintained a current mailing list of physicians in the specialties of family medicine, internal medicine, cardiovascular surgery, and cardiology, mailing letters to physicians once or twice each recruitment year requesting referrals of eligible women to CR with the potential for study participation. Study brochures accompanied the letters and physicians were reassured of principal control of the medical management of their patients. Also, the trial coinvestigators who were cardiologists sent a letter to all physicians seeking referrals. The most current evidence-based guidelines for CHD prevention in women9 were included in the physician referral letter. A letter of appreciation was sent to the referring physician after each successful study recruit. A monthly newsletter, produced by the research team, was mailed to all study participants and physician office practices, and referring physicians were acknowledged for their patient referrals.
Community Initiatives
Community recruitment initiatives included media (television, radio, newspapers) advertisements, and presentations to women’s community groups, American Heart Association functions, health fairs, cardiology grand rounds, and physician office practices. Brochures were also placed in libraries, grocery stores, public health offices, and senior citizen recreation centers. Brief television appearances and radio interviews highlighting the study were conducted an average of 4 times yearly. Advertisements in local and regional newspapers, some with a circulation of 300,000, ranged from 6 times yearly in the first year to biweekly by year 5 of recruitment. Articles featuring the study appeared 3 times in the largest metropolitan newspaper servicing central Florida.
Screening Protocol
A physician referral to CR, whether a standing order or a physician office referral, was required for initiating the screening protocol for CR, and subsequently, the study. Hospital inpatient referrals were received by the exercise physiologist who delivered phase I CR, scheduled an outpatient CR orientation appointment to qualified patients, and delivered the referral to the CR patient care representative. The exercise physiologist screened patients for CR eligibility by examining the medical records and assessing patients. The study recruiter conducted an individualized orientation with every eligible woman referred to CR. Women received a reminder telephone call from the study recruiter the day prior to the orientation appointment. Individuals missing appointments were called for rescheduling with a maximum of 6 callbacks. The recruiter began the orientation session with a general overview of the purpose, content, and time commitment of CR. After determining eligibility for CR, the recruiter screened for study eligibility. Women eligible and interested in attending CR were invited to study participation. The study protocol was explained, questions were answered, and ambivalence to participation was explored using motivational interviewing strategies.36 The recruiter assessed the women’s understanding and acceptance of random allocation and explored possible therapeutic misconceptions regarding either study treatment arm. Women were presented 2 options for CR participation; their first option was study participation with the understanding of an equal chance of randomization to either the women’s-only or the usual care treatment group. Alternatively, women were free to choose usual care CR and decline study participation. Women choosing either option for CR completed documentation necessary to begin processing the phase II referral. The patient care representative then determined eligibility for medical insurance coverage or for financial assistance. With confirmation of insurance coverage and medical director clearance to begin CR, the charts of women interested in study participation were delivered to the research assistant.
Informed Consent Procedures and Baseline Data Collection
The research assistant scheduled appointments for the consenting procedures and the comprehensive health evaluation. At the comprehensive health evaluation, the research assistant again assessed for acceptance of random allocation and reviewed the informed consent in detail. Before consent signing, women verbalized a commitment to attending CR 3 times weekly for 12 weeks followed by 6 monthly follow-up booster sessions. This participation commitment involved about 52 hours over 9 months. Monetary reimbursement for study-related travel and time investments were reviewed. Following the consent signing, the research assistant conducted the comprehensive health evaluation and scheduled a symptom-limited exercise treadmill test (ETT) within 1 week. After completion of the ETT, the project director randomized the participants to either traditional CR or the women’s-only group.
Study Recruitment-Tracking Log
The recruiter established an Excel recruitment-tracking log to document the source and outcome of referrals, referring physician, referral data, date of telephone calls, and orientation appointments. Reasons for study ineligibility, nonparticipation, and missed orientations were recorded. Women deemed temporarily ineligible for CR due to impending surgical procedures or experiencing current participation barriers were encouraged to return for screening within 10 months. Recruiting reports were created, updated, and presented weekly to the study investigators.
RESULTS
Recruitment Sources
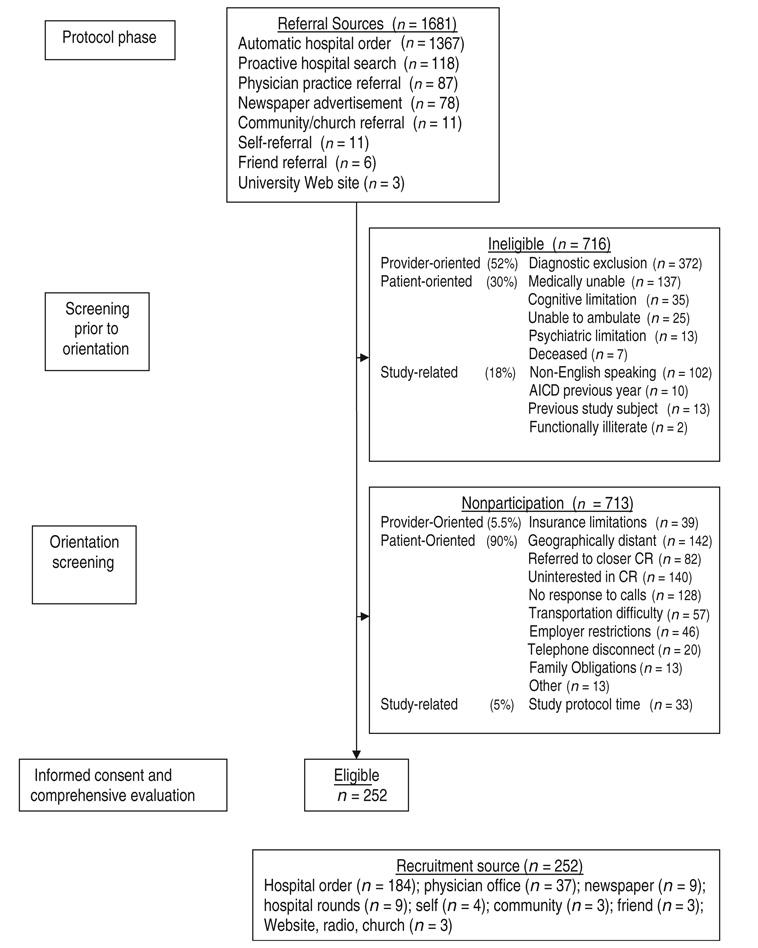
Between 2004 and 2008, 1,681 patients were referred and screened for study participation. The majority of these referrals (n = 1,367, 81%) resulted from automatic hospital orders (Figure 1). In 2004, the study recruiter made hospital rounds seeking eligible patients inadvertently without an automatic referral. This recruitment strategy was halted in 2006 because of resource intensiveness and low yield (Table 1). Costly newspaper advertisements and feature articles in major metropolitan and smaller community newspapers also resulted in few potential participants (n = 78). Only 87 (5%) patients were referred from physician offices and a few patients approached the CR facility seeking participation (n = 11).
Figure 1.
Flow diagram of patient recruitment. AICD indicates automatic internal cardiac defibrillator; CR, cardiac rehabilitation.
Table 1.
Recruitment and enrollment of women in clinical trial 2004 to March 2008
| n | |||||||
|---|---|---|---|---|---|---|---|
| 2004 | 2005 | 2006 | 2007 | 2008 | Total | % of screened | |
| Recruitment sources | |||||||
| Automatic hospital order | 325 | 416 | 338 | 246 | 42 | 1,367 | 81.3 |
| Proactive hospital search | 74 | 38 | 6 | 0 | 0 | 118 | 7.0 |
| Physician practice referral | 20 | 16 | 12 | 33 | 6 | 87 | 5.2 |
| Newspaper ad/article | 2 | 22 | 44 | 8 | 1 | 78 | 4.6 |
| Community/church referral | 1 | 1 | 1 | 7 | 1 | 11 | 0.7 |
| Self-referral | 1 | 6 | 4 | 0 | 0 | 11 | 0.7 |
| Friend referral | 0 | 0 | 5 | 1 | 0 | 6 | 0.4 |
| University Web site | … | 0 | 1 | 2 | 0 | 3 | 0.2 |
| Total referrals | 423 | 499 | 411 | 298 | 50 | 1,681 | |
| Exclusions before orientation | % of exclusions | ||||||
| Diagnostic exclusion criteria | 85 | 140 | 89 | 54 | 4 | 372 | 52.0 |
| Medically unable | 29 | 24 | 39 | 42 | 3 | 137 | 19.0 |
| Non-English speaking | 26 | 27 | 28 | 17 | 4 | 102 | 14.2 |
| Cognitive limitation | 11 | 10 | 11 | 3 | 0 | 35 | 5.0 |
| Unable to ambulate | 3 | 11 | 6 | 4 | 1 | 25 | 3.5 |
| Psychiatric limitation | 2 | 2 | 4 | 4 | 1 | 13 | 1.8 |
| Previous study subject | 0 | 1 | 10 | 2 | 0 | 13 | 1.8 |
| AICD in last year | 4 | 3 | 3 | 0 | 0 | 10 | 1.4 |
| Deceased | 3 | 2 | 1 | 1 | 0 | 7 | 1.0 |
| Functionally illiterate | 1 | 1 | 0 | 0 | 0 | 2 | 0.3 |
| Total exclusions | 164 | 221 | 191 | 127 | 13 | 716 | 42.6% of referrals |
| Total eligible | 259 | 278 | 220 | 171 | 37 | 965 | |
| Nonparticipation at orientation | % of eligible | ||||||
| Geographically distant | 38 | 58 | 36 | 9 | 1 | 142 | 14.7 |
| Uninterested in CR | 36 | 40 | 35 | 24 | 5 | 140 | 14.5 |
| Unresponsive to telephone/letter | 48 | 41 | 25 | 12 | 2 | 128 | 13.3 |
| Referred to closer CR | … | 6 | 32 | 30 | 14 | 82 | 8.5 |
| Transportation difficulty | 18 | 15 | 15 | 9 | 0 | 57 | 6.0 |
| Employment restrictions | 8 | 7 | 12 | 15 | 4 | 46 | 4.7 |
| Insurance limitations | 11 | 11 | 9 | 6 | 2 | 39 | 4.0 |
| Inconvenient study protocol | 20 | 5 | 3 | 4 | 1 | 33 | 3.4 |
| Telephone disconnected | … | 13 | 6 | 1 | 0 | 20 | 2.2 |
| Family obligations | 0 | 5 | 2 | 5 | 1 | 13 | 1.3 |
| Other | 13 | 0 | 0 | 0 | 0 | 13 | 1.4 |
| Total nonparticipation | 192 | 201 | 175 | 115 | 30 | 713 | 73.8% of eligible |
| Total randomized | 67 | 77 | 45 | 56 | 7 | 252 | 26.2% of eligible |
Abbreviations: AICD, automatic internal cardiac defibrillator; CR, cardiac rehabilitation.
Screening Exclusions and Nonparticipation
Of women referred to CR, 716 (42.6%) were ineligible for study participation. The largest exclusion category was failure to meet the diagnostic criteria for CR (n = 372/716, 52%). This was followed by women medically unable to participate (n = 137, 19%) for reasons including unstable medical conditions or impending surgical procedures. The intervention necessitated excluding non–English-speaking women (n = 102, 14.2%), those cognitively impaired (n = 35, 5%), those unable to ambulate (n = 25, 3.5%), previous study participants (n = 13, 1.8%), or those who had received an automatic internal cardiac defibrillator in the previous year (n = 10, 1.4%). Women with an acute psychiatric limitation (n = 13, 1.8%) or who were functionally illiterate (n = 2, 0.3%) were also excluded. Several women died (n = 7, 1%) prior to orientation. Women screened ineligible for the study while still qualifying for traditional CR included the non-English speaking, those with an automatic internal cardiac defibrillator, and previous study participants. These exclusions resulted in 965 women eligible for study participation.
Nonparticipation of eligible women was identified between the first telephone contact by the recruiter and the comprehensive health evaluation appointment when the informed consent was signed. Of the women meeting eligibility criteria but declining study participation, the greatest number indicated that the distance between their home and the study site prohibited trial participation (n = 142, 14.7%). The second most frequently reported reason for nonparticipation was general disinterest in CR participation (n = 140, 14.5%), closely followed by women unresponsive to repeated telephone calls or registered letters (n = 128, 13.3%). A desire to attend a CR program near their home led some to refuse study participation (n = 82, 8.5%), and transportation barriers were cited by 57 (6%) women. The experimental intervention was implemented between 11:00 am and 1:00 pm 3 times weekly and precluded enrollment for 33 women (3.4%). Few women were limited by employment obligations (n = 46, 4.7%) or by high insurance co-payments of $20 to $100 for each of the 36 exercise sessions (n = 39, 4%). Fewer women had disconnected telephones (n = 20, 2.2%) or family/other limitations (n = 26, 2.7%). Thus, 252 women expressing interest in study participation signed the informed consent.
Trial Recruitment Yields
The recruitment efficiency37 revealed that 15% (252/1,681) of women referred and 26% (252/965) of those screened eligible were enrolled in the study. Of those enrolled, 73% (184/252) were recruited from automatic hospital orders, 15% (37/252) were referred from physician practices, 4% (9/252) were identified by the recruiter during hospital rounds, and 4% were recruited through newspaper advertisements. A few patients (1%) were recruited from community initiatives or through a friend (3/252 each). One patient was referred from each of the following sources, Web site, radio advertisement, and a church.
DISCUSSION
Our recruitment efforts illustrate the complexities of adherence to the directives from funding agencies38–40 to recruit women to clinical research. A multifaceted interplay of patient-oriented, provider-oriented, and programmatic barriers challenged the enrollment of women to our trial. The lessons learned concerning the factors that facilitated and hindered study recruitment and enrollment at particular study protocol benchmarks may benefit others designing behavioral interventions for women.
An important insight gained during this study was the identification of factors promoting study enrollment including automatic hospital orders, individualized orientation sessions, and motivational interviewing techniques. Most study participants were referred through standing hospital orders, followed distantly by physician office referrals. This finding may encourage CR medical directors committed to fostering enrollment of women to implement standing hospital orders. Recognizing that physician referral is a necessary determinant of CR participation, others have confirmed the utility of automatic hospital referrals. 13,19,26,33,41–43 Jackson et al22 proposed that the strength of physician endorsement and enthusiasm for CR is the single most powerful predictor of CR attendance. Anecdotal evidence from our study participants supports the assertion that physician recommendation of CR13,44 is a key factor tipping the decision balance favoring CR enrollment. Study participants generally held the opinion of their physicians in high regard, often delaying decision making until the physician confirmed the importance of CR. Physicians play a prominent role in motivating women to attend CR; efforts to enhance physician contributions to maximizing referrals are a vital priority for CR services.
In contrast to the traditional CR group orientations, our study recruiter, trained in motivational interviewing counseling techniques, implemented individual orientation sessions with all women referred to both CR and the study. The vast majority of women attending orientation enrolled in the study. Further research is needed to untangle which component of the orientation was most effective—motivational interviewing, individualized attention, or the clarity with which the study protocol expectations were conveyed. Any verbalized disinterest in CR typically occurred prior to the individualized orientations usually during appointment confirmation telephone calls.
Letters requesting referrals from physician offices resulted in modest responses; this apparent treatment gap requires attention. Mechanisms to streamline communication between physician practices and CR programs to improve referrals are warranted. Competition for revenue-generating patients between hospital-based CR programs, as well as physician concern about losing patients referred outside their practices, represents referral barriers requiring exploration. Perhaps CR directors offering collegial reassurances to referring physicians of clinician autonomy might increase referrals.
Our launch press release led to local radio, television, and newspaper publicity but yielded poor response rates. We found that costly newspaper advertising produced particularly poor recruitment yields and was the most resource intensive. Although feature newspaper articles and use of university press offices were inexpensive recruitment methods, they too produced few participants. Others have found editorials or features in local healthcare magazines to be unsuccessful recruitment strategies.45 Because community recruitment initiatives were labor-intensive, low-yield strategies we would recommend a greater focus on physician practice recruitment materials.
Most study referrals were screened ineligible for provider-oriented reasons beyond our control compared with patient-oriented factors or study protocol–related factors. The largest provider-oriented exclusion category, ineligible diagnoses for CR, precluded more than half of referred women from participating in CR or the study. This category comprised patients with Medicare coverage exclusions, symptomatic congestive heart failure, or uncontrolled comorbid conditions such as chronic renal failure or diabetes. Patient-oriented factors precluding participation included cognitive, psychiatric, or physical health status limitations. Additional study protocol exclusions, intended to increase sample homogeneity and provide a more powerful test of the intervention, included women who were non-English speaking, functionally illiterate, a previous study participant, or those with a recent automatic internal cardiac defibrillator insertion.
As previous researchers have found,26 even with appropriate referral to CR, less than half of eligible patients attended. Although women were largely ineligible for CR due to provider-oriented factors, study nonparticipation was largely associated with patient-oriented factors. Patient-oriented logistical barriers included geographic distance from the rehabilitation center, the intent to attend a CR near their home, and transportation difficulties. Serendipitously, we found that the monetary reimbursement of about $8 for travel to each of the 45 (36 exercise, 6 booster, and 3 data collection) sessions had little impact on enrollment rates. Payer reimbursement and study-related barriers were far less prohibitive than the large nonparticipation category, reflecting disinterest in CR. A deeper understanding of the large patient-oriented nonparticipation categories of expressed disinterest in CR and geographic distance may provide guidance for solutions to these attendance barriers for women. The feasibility of reimbursing community-based CR programs or developing home-based interventions merits investigation.
Despite the added recruitment challenges inherent in any intensive behavioral trial, our recruitment yield mirrors CR participation rates of women in the United States.6 Our recruitment yield of 15% is comparable to several behavioral intervention trials involving women or older adults. The Dietary Approach to Stop Hypertension–Sodium Trial46 reported a recruitment yield of 17% and the Women’s Health Initiative47 reported a randomization yield of 7.3% in the hormone replacement therapy study arm. Moreover, a physical activity intervention for preventing mobility disability in elders had a recruitment yield of 13.5%48 and the Diabetes Prevention program reported a recruitment yield of only 2.5%.49
Our recruitment yield may reflect contemporary medical advances in cardiac care. The current trend of declining hospitalization rates and the shortened length of stay after acute myocardial infarction and coronary revascularization in the United States,50 perhaps, negatively impacts opportunities for CR referrals. Some have suggested that percutaneous coronary intervention patients compared with other cardiac patients are less inclined to attend CR.51,52 The evidence-based use of aspirin, β-blockers, and statins may be shifting CHD from an inpatient to a predominantly outpatient disease management scenario.50 Physicians and patients alike, perhaps, perceive CR as unnecessary. The need to overestimate the number of referrals needed for adequate study enrollment of women in a CR behavioral intervention cannot be emphasized enough.
Limitations
Our findings should be interpreted in context of the following limitations. First, our findings may not generalize from our single site to the larger national community. The priority of this clinical trial was maximizing internal validity admittedly at the expense of external validity, and it was beyond the scope of the study to decrease many of the barriers to participation. For example, we lacked resources to deliver the behavioral intervention in a second language or to provide transportation to the study facility. Instead, we offered reimbursement for travel. Yet, while acknowledging a large geographic variation in CR use in the United States, our recruitment yield represents the CR enrollment rates of women in the southern states.
Second, because the participants in the usual care group received CR from the facility, their healthcare payer was billed. To avoid differential dropout of participants in the experimental group, their payer was also billed for the monitored exercise sessions. This practice was driven by Medicare reimbursement and not clinical efficacy53 or the study protocol. Third, budget constraints prevented a detailed examination of the characteristics of women refusing study enrollment. Finally, all recruitment strategies ran concurrently, making it difficult to differentiate the impact of any single strategy. Although women may have been primed by multiple marketing messages, the primary source of referral was recorded in mutually exclusive categories.
We examined the myriad of factors influencing enrollment in a CR clinical trial for women. Despite evidence-based guidelines underscoring the importance of CR for reducing morbidity and mortality after acute coronary syndromes, women remain in the minority in CR populations. Research efforts utilizing a gender-informed paradigm may aid in eradicating the gender disparities in CR participation.
Acknowledgment
The Women’s-Only Phase II Cardiac Rehabilitation program was funded by the National Institute of Nursing Research Grant R01-07678.
Footnotes
The authors of this article have disclosed no significant ties, financial or otherwise, to any company that might have an interest in the publication of this educational activity.
For more than 80 continuing education articles related to cardiovascular conditions, go to NursingCenter.com/CE
References
- 1.Wenger NK. Current status of cardiac rehabilitation. J Am Coll Cardiol. 2008;51:1619–1631. doi: 10.1016/j.jacc.2008.01.030. [DOI] [PubMed] [Google Scholar]
- 2.Thomas RJ, King M, Lui K, et al. AACVPR/ACC/AHA 2007 performance measures on cardiac rehabilitation for referral to and delivery of cardiac rehabilitation/secondary prevention services endorsed by the American College of Chest Physicians, American College of Sports Medicine, American Physical Therapy Association, Canadian Association of Cardiac Rehabilitation, European Association for Cardiovascular Prevention and Rehabilitation, Inter-American Heart Foundation, National Association of Clinical Nurse Specialists, Preventive Cardiovascular Nurses Association, and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2007;50:1400–1433. doi: 10.1016/j.jacc.2007.04.033. [DOI] [PubMed] [Google Scholar]
- 3.Clark AM, Hartling L, Vandermeer B, McAlister FA. Meta-analysis: secondary prevention programs for patients with coronary artery disease. Ann Intern Med. 2005;143:659–672. doi: 10.7326/0003-4819-143-9-200511010-00010. [DOI] [PubMed] [Google Scholar]
- 4.Taylor RS, Brown A, Ebrahim S, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116:682–692. doi: 10.1016/j.amjmed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 5.Jolliffe JA, Rees K, Taylor RS, Thompson D, Oldridge N, Ebrahim S. Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2001;(1):CD001800. doi: 10.1002/14651858.CD001800. [DOI] [PubMed] [Google Scholar]
- 6.Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, Stason WB. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116(15):1653–1662. doi: 10.1161/CIRCULATIONAHA.107.701466. [DOI] [PubMed] [Google Scholar]
- 7.Smith SC, Jr, Allen J, Blair SN, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood Institute. Circulation. 2006;113:2363–2372. doi: 10.1161/CIRCULATIONAHA.106.174516. [DOI] [PubMed] [Google Scholar]
- 8.Leon AS, Franklin BA, Costa F, et al. Cardiac rehabilitation and secondary prevention of coronary heart disease: an American Heart Association scientific statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity), in collaboration with the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2005;111:369–376. doi: 10.1161/01.CIR.0000151788.08740.5C. [DOI] [PubMed] [Google Scholar]
- 9.Mosca L, Banka CL, Benjamin EJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation. 2007;115:1481–1501. doi: 10.1161/CIRCULATIONAHA.107.181546. [DOI] [PubMed] [Google Scholar]
- 10.Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in US deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 11.Allen JK, Scott LB, Stewart KJ, Young DR. Disparities in women’s referral to and enrollment in outpatient cardiac rehabilitation. J Gen Intern Med. 2004;19:747–753. doi: 10.1111/j.1525-1497.2004.30300.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scott LB, Allen JK. Providers’ perceptions of factors affecting women’s referral to outpatient cardiac rehabilitation programs: an exploratory study. J Cardiopulm Rehabil. 2004;24:387–391. doi: 10.1097/00008483-200411000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Ades PA, Waldmann ML, Polk DM, Coflesky JT. Referral patterns and exercise response in the rehabilitation of female coronary patients aged greater than or equal to 62 years. Am J Cardiol. 1992;69:1422–1425. doi: 10.1016/0002-9149(92)90894-5. [DOI] [PubMed] [Google Scholar]
- 14.Bittner V, Sanderson B, Breland J, Green D. Referral patterns to a University-based cardiac rehabilitation program. Am J Cardiol. 1999;83:252–255. doi: 10.1016/s0002-9149(98)00830-3. A255. [DOI] [PubMed] [Google Scholar]
- 15.Jeger RV, Jorg L, Rickenbacher P, Pfisterer ME, Hoffmann A. Benefit of outpatient cardiac rehabilitation in under-represented patient subgroups. J Rehabil Med. 2007;39:246–251. doi: 10.2340/16501977-0055. [DOI] [PubMed] [Google Scholar]
- 16.Scott LA, Ben-Or K, Allen JK. Why are women missing from outpatient cardiac rehabilitation programs? A review of multilevel factors affecting referral, enrollment, and completion. J Womens Health. 2002;11:773–791. doi: 10.1089/15409990260430927. [DOI] [PubMed] [Google Scholar]
- 17.Witt BJ, Jacobsen SJ, Weston SA, et al. Cardiac rehabilitation after myocardial infarction in the community. J Am Coll Cardiol. 2004;44:988–996. doi: 10.1016/j.jacc.2004.05.062. [DOI] [PubMed] [Google Scholar]
- 18.Clark AM, Barbour RS, White M, MacIntyre PD. Promoting participation in cardiac rehabilitation: patient choices and experiences. J Adv Nurs. 2004;47:5–14. doi: 10.1111/j.1365-2648.2004.03060.x. [DOI] [PubMed] [Google Scholar]
- 19.Caulin-Glaser T, Blum M, Schmeizl R, Prigerson HG, Zaret B, Mazure CM. Gender differences in referral to cardiac rehabilitation programs after revascularization. J Cardiopulm Rehabil. 2001;21:24–30. doi: 10.1097/00008483-200101000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Halm M, Penque S, Doll N, Beahrs M. Women and cardiac rehabilitation: referral and compliance patterns. J Cardiovasc Nurs. 1999;13:83–92. doi: 10.1097/00005082-199904000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Evenson KR, Rosamond WD, Luepker RV. Predictors of outpatient cardiac rehabilitation utilization: the Minnesota Heart Surgery Registry. J Cardiopulm Rehabil. 1998;18:192–198. doi: 10.1097/00008483-199805000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Jackson L, Leclerc J, Erskine Y, Linden W. Getting the most out of cardiac rehabilitation: a review of referral and adherence predictors. Heart. 2005;91:10–14. doi: 10.1136/hrt.2004.045559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lieberman L, Meana M, Stewart D. Cardiac rehabilitation: gender differences in factors influencing participation. J Womens Health. 1998;7:717–723. doi: 10.1089/jwh.1998.7.717. [DOI] [PubMed] [Google Scholar]
- 24.Dolansky MA, Moore SM, Visovsky C. Older adults’ views of cardiac rehabilitation program: is it time to reinvent? J Gerontol Nurs. 2006;32:37–44. doi: 10.3928/0098-9134-20060201-10. [DOI] [PubMed] [Google Scholar]
- 25.Cottin Y, Cambou JP, Casillas JM, Ferrieres J, Cantet C, Danchin N. Specific profile and referral bias of rehabilitated patients after an acute coronary syndrome. J Cardiopulm Rehabil. 2004;24:38–44. doi: 10.1097/00008483-200401000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Cortes O, Arthur HM. Determinants of referral to cardiac rehabilitation programs in patients with coronary artery disease: a systematic review. Am Heart J. 2006;151:249–256. doi: 10.1016/j.ahj.2005.03.034. [DOI] [PubMed] [Google Scholar]
- 27.King KM, Humen DP, Smith HL, Phan CL, Teo KK. Psychosocial components of cardiac recovery and rehabilitation attendance. Heart. 2001;85:290–294. doi: 10.1136/heart.85.3.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Filip J, McGillen C, Mosca L. Patient preferences for cardiac rehabilitation and desired program elements. J Cardiopulm Rehabil. 1999;19:339–343. doi: 10.1097/00008483-199911000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Ades PA, Savage PD, Brawner CA, et al. Aerobic capacity in patients entering cardiac rehabilitation. Circulation. 2006;113:2706–2712. doi: 10.1161/CIRCULATIONAHA.105.606624. [DOI] [PubMed] [Google Scholar]
- 30.Comoss P. Commentary: frequently asked questions … action packed answers. J Cardiopulm Rehabil. 2005;25:67–70. doi: 10.1097/00008483-200503000-00002. [DOI] [PubMed] [Google Scholar]
- 31.Cooper AF, Jackson G, Weinman J, Horne R. Factors associated with cardiac rehabilitation attendance: a systematic review of the literature. Clin Rehabil. 2002;16:541–552. doi: 10.1191/0269215502cr524oa. [DOI] [PubMed] [Google Scholar]
- 32.Moore SM, Kramer FM. Women’s and men’s preferences for cardiac rehabilitation program features. J Cardiopulm Rehabil. 1996;16:163–168. doi: 10.1097/00008483-199605000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Daly J, Sindone AP, Thompson DR, Hancock K, Chang E, Davidson P. Barriers to participation in and adherence to cardiac rehabilitation programs: a critical literature review. Prog Cardiovasc Nurs. 2002;17:8–17. doi: 10.1111/j.0889-7204.2002.00614.x. [DOI] [PubMed] [Google Scholar]
- 34.Beckie TM. A behavior change intervention for women in cardiac rehabilitation. J Cardiovasc Nurs. 2006;21:146–153. doi: 10.1097/00005082-200603000-00013. [DOI] [PubMed] [Google Scholar]
- 35.Beckie TM, Fletcher GF, Beckstead JW, Schocken DD, Evans ME. Adverse baseline physiological and psychosocial profiles of women enrolled in a cardiac rehabilitation clinical trial. J Cardiopulm Rehabil Prev. 2008;28:52–60. doi: 10.1097/01.HCR.0000311510.16226.6e. [DOI] [PubMed] [Google Scholar]
- 36.Miller WR, Rollnick S, editors. Motivational Interviewing: Preparing People for Change. 2nd ed. New York: Guilford; 2002. [Google Scholar]
- 37.Wilbur J, McDevitt J, Wang E, et al. Recruitment of African American women to a walking program: eligibility, ineligibility, and attrition during screening. Res Nurs Health. 2006;29:176–189. doi: 10.1002/nur.20136. [DOI] [PubMed] [Google Scholar]
- 38.Marshall E. National Institutes of Health. New law brings affirmative action to clinical research. Science. 1994;263(5147):602. doi: 10.1126/science.8303263. [DOI] [PubMed] [Google Scholar]
- 39.Hohmann AA, Parron DL. How the new NIH Guidelines on Inclusion of Women and Minorities apply: efficacy trials, effectiveness trials, and validity. J Consult Clin Psychol. 1996;64:851–855. doi: 10.1037//0022-006x.64.5.851. [DOI] [PubMed] [Google Scholar]
- 40.Vidaver RM, Lafleur B, Tong C, Bradshaw R, Marts SA. Women subjects in NIH-funded clinical research literature: lack of progress in both representation and analysis by sex. J Womens Health Gend Based Med. 2000;9:495–504. doi: 10.1089/15246090050073576. [DOI] [PubMed] [Google Scholar]
- 41.King KM, Teo KK. Cardiac rehabilitation referral and attendance: not one and the same. Rehabil Nurs. 1998;23:246–251. doi: 10.1002/j.2048-7940.1998.tb01794.x. [DOI] [PubMed] [Google Scholar]
- 42.Grace SL, Evindar A, Kung TN, Scholey PE, Stewart DE. Automatic referral to cardiac rehabilitation. Med Care. 2004;42:661–669. doi: 10.1097/01.mlr.0000129901.05299.aa. [DOI] [PubMed] [Google Scholar]
- 43.Grace SL, Evindar A, Kung T, Scholey P, Stewart DE. Increasing access to cardiac rehabilitation: automatic referral to the program nearest home. J Cardiopulm Rehabil. 2004;24:171–174. doi: 10.1097/00008483-200405000-00006. [DOI] [PubMed] [Google Scholar]
- 44.Ades PA, Waldmann ML, McCann WJ, Weaver SO. Predictors of cardiac rehabilitation participation in older coronary patients. Arch Intern Med. 1992;152:1033–1035. [PubMed] [Google Scholar]
- 45.Ellis SD, Bertoni AG, Bonds DE, et al. Value of recruitment strategies used in a primary care practice-based trial. Contemp Clin Trials. 2007;28:258–267. doi: 10.1016/j.cct.2006.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kennedy BM, Conlin PR, Ernst D, Reams P, Charleston JB, Appel LJ. Successfully recruiting a multicultural population: the DASH-Sodium experience. Ethn Dis. 2005;15:123–129. [PubMed] [Google Scholar]
- 47.Fouad MN, Corbie-Smith G, Curb D, et al. Special populations recruitment for the Women’s Health Initiative: successes and limitations. Control Clin Trials. 2004;25:335–352. doi: 10.1016/j.cct.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 48.Katula JA, Kritchevsky SB, Guralnik JM, et al. Lifestyle Interventions and Independence for Elders pilot study: recruitment and baseline characteristics. J Am Geriatr Soc. 2007;55:674–683. doi: 10.1111/j.1532-5415.2007.01136.x. [DOI] [PubMed] [Google Scholar]
- 49.Rubin RR, Fujimoto WY, Marrero DG, et al. The Diabetes Prevention program: recruitment methods and results. Control Clin Trials. 2002;23:157–171. doi: 10.1016/s0197-2456(01)00184-2. [DOI] [PubMed] [Google Scholar]
- 50.Nallamothu BK, Young J, Gurm HS, Pickens G, Safavi K. Recent trends in hospital utilization for acute myocardial infarction and coronary revascularization in the United States. Am J Cardiol. 2007;99:749–753. doi: 10.1016/j.amjcard.2006.10.029. [DOI] [PubMed] [Google Scholar]
- 51.Worcester MU, Murphy BM, Mee VK, Roberts SB, Goble AJ. Cardiac rehabilitation programmes: predictors of non-attendance and drop-out. Eur J Cardiovasc Prev Rehabil. 2004;11:328–335. doi: 10.1097/01.hjr.0000137083.20844.54. [DOI] [PubMed] [Google Scholar]
- 52.Thomas RJ, Miller NH, Lamendola C, et al. National Survey on Gender Differences in Cardiac Rehabilitation programs. Patient characteristics and enrollment patterns. J Cardiopulm Rehabil. 1996;16:402–412. doi: 10.1097/00008483-199611000-00010. [DOI] [PubMed] [Google Scholar]
- 53.Franklin BA. An alternative approach to the delivery of cardiac rehabilitation services: a “hybrid” model for patient care. J Cardiopulm Rehabil. 2004;24:383–386. doi: 10.1097/00008483-200411000-00004. [DOI] [PubMed] [Google Scholar]