Abstract
Erectile dysfunction (ED) is a highly prevalent disease associated with aging as well as with several risk factors including hypertension, heart disease, obesity, dyslipidemia, diabetes, hypogonadism, drugs-related, and pelvic surgery. Many of these factors are components of the metabolic syndrome, a multiplex risk factor for cardiovascular disease (CVD). ED shares common risk factors with CVD. Endothelial dysfunction seems to be the early underlying pathophysiology across both conditions. The efficacy, tolerability and cardiovascular safety of sildenafil has been evaluated in numerous large, randomized, double-blind, placebo-controlled clinical studies in the broad population of men with ED including men with several co-morbid conditions. Sildenafil is effective in several specific patient populations including the difficult-to-treat subpopulations such as diabetes mellitus and after radical prostatectomy. It is associated with rapid onset of action – within 14 minutes for some men – and an extended duration of action for up to 12 hours. Sildenafil improves quality of life and satisfaction for treated men and is well tolerated with a favorable safety profile. New data suggest that sildenafil has beneficial effects in several chronic conditions. It has been approved for the treatment of idiopathic pulmonary hypertension. Numerous articles have suggested that it improves endothelial function and a possible role on premature ejaculation or treatment of lower urinary tract symptoms has been suggested.
Keywords: erectile dysfunction, phosphodiesterase inhibitors, safety, treatment outcome
Introduction
Erectile dysfunction (ED) is a highly prevalent disease, as well as a major sexual concern for men (Braun et al 2000; Martin-Morales et al 2001; Papaharitou et al 2006). The prevalence of ED is increasing with age. The Massachusetts Male Aging Study (MMAS) demonstrated a 40% prevalence of ED in men aged 40 years that increased to almost 70% in men aged 70 years (Feldman et al 1994). As the proportion of older people in the population increases, it has been estimated that the worldwide prevalence of ED will double from 152 million men in 1995 to 322 million men in 2025 (Aytac et al 1999). ED is also associated with other conditions such as age, smoking, hypertension, heart disease, diabetes, and as a consequence of radical prostatectomy. Cardiovascular disease (CVD) and ED share common risk factors and reflect endothelial dysfunction (Kostis et al 2005). There is an increasing body of evidence that ED is the first sign of CVD in men with free medical history and may present well before CVD with a mean time-interval of even 3 years (Montorsi et al 2003).
The availability of phosphodiesterase type 5 inhibitors (PDE5i) has resulted in increasing numbers of patients seeking medical help for erectile function problems, but has also altered dramatically the medical management of ED (Hatzichristou and Pescatori 2001; Lewis et al 2001; Steers et al 2001). More physicians are treating ED, especially in the primary care setting, including minimal patient work-up and prescription of PDE5i due to their proven efficacy and safety profile. The management of ED by non-specialists includes minimal patient work-up and prescription of exclusively first-line treatment options in most cases, mainly due to the lack of time and background knowledge (Hatzichristou 2002). Sildenafil was the first available PDE5i that revolutionized ED treatment (Goldstein et al 1998). More than 30 million of men are treated worldwide with sildenafil accompanied by vast experience and research with more than 2600 papers published in Medline as of July 2006. Furthermore, new data suggest that sildenafil has beneficial effects in several chronic conditions. It has been recently approved for the treatment of idiopathic pulmonary hypertension (Galie et al 2005), and numerous articles have suggested that PDE5i may improve endothelial function (Katz et al 2000; Desouza et al 2002; Halcox et al 2002; Vlachopoulos et al 2003; Vlachopoulos et al 2004; Gori et al 2005; Hirata et al 2005). PDE5i have been also suggested to be beneficial for patients with premature ejaculation (Abdel-Hamid 2004). However, clinical studies have shown controversial results so far (Salonia et al 2002; Chen et al 2003; Atan et al 2006) and it remains uncertain, whether PDE5i act on the physiologic process of ejaculation, or indirectly, improving erectile function and therefore, reducing performance anxiety in men with ED.
The aim of this review is to provide an overview of the clinical evidence associated with sildenafil in the treatment of ED as well as to present data from ongoing basic and clinical research in other chronic diseases.
Pharmacological profile: time to onset and duration of action
Sildenafil is a highly selective inhibitor of PDE type 5 (Boolell et al 1996; Gbekor et al 2002). It enhances NO-mediated relaxation of human corpus cavernosum in vitro (Ballard et al 1998; Stief et al 1998; Gemalmaz et al 2001). Sildenafil, by inhibiting phosphodiesterase, increases the intracellular concentrations of cyclic guanosine 3’,5’ monophosphate (cGMP), causing an amplification of the endogenous NO-cGMP signaling pathway.
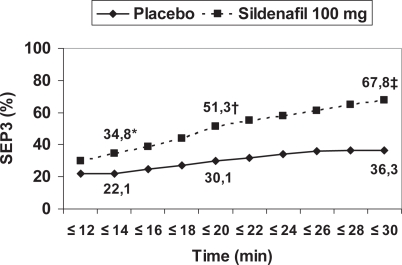
The time to maximum plasma concentration is about 1 h while the plasma half-life is about 4–5 h. It is administered orally on demand in 25 mg, 50 mg, and 100 mg doses. The recommended starting dose is 50 mg and adapted according to efficacy and tolerability. Patients are instructed to take sildenafil approximately 1 h before sexual intercourse with a maximum dosing frequency of once daily. Sexual stimulation is a prerequisite for sildenafil as well as for the other PDE5i. The window of opportunity to engage in sexual intercourse is maintained from 30 min to 4–5 h from administration. However, the onset of action can be 14 min for about 35% of patients (Figure 1) (Padma-Nathan et al 2003) and efficacy may be maintained for up to 12 h (Moncada et al 2004). A heavy fatty meal results in reduced and prolonged absorption. Alcohol does not have an impact on absorption in regular doses. Contraindications for the use of sildenafil and need for dose adjustments are summarized in Table 1 (Langtry and Markham 1999).
Figure 1.
Time to onset of erection resulting in successful intercourse. *P=0.0343, †P=0.0011, ‡P=0.0001. Copyright © 2003. Reproduced with permission from Padma-Nathan H, Stecher VJ, Sweeney M, et al. 2003. Minimal time to successful intercourse after sildenafil citrate: results of a randomized, double-blind, placebo-controlled trial. Urology, 62:400–3.
Abbreviations: SEP3, Sexual Encounter Profile question 3.
Table 1.
Contraindications and dose adjustments for sildenafil (as well as for the other phosphodiesterase type 5 inhibitors)
|
Efficacy in broad populations of men with ED
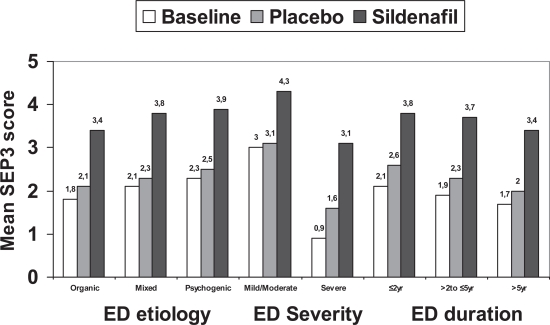
The first data on efficacy of sildenafil were published by Goldstein and colleagues (1998) Sexual intercourse was successful in 69% of all attempts for the men receiving sildenafil, as compared with 22% for those receiving placebo (p<0.001). The mean numbers of successful attempts per month were 5.9 for men receiving sildenafil and 1.5 for those receiving placebo (p<0.001). Efficacy parameters for sildenafil in 11 double-blind, placebo controlled, pre-marketing studies included the International Index of Erectile Function (IIEF) erectile function domain score and especially the questions 3 and 4 (ability to attain and ability to maintain an erection sufficient for intercourse respectively) as well as the general efficacy question (GEQ). In 6 of the 11 trials, patients maintained an event log of sexual activity. Patients were stratified in subgroups in terms of age, race, body mass index (BMI), duration of ED, ED etiology, smoking status, and concomitant conditions/medications (Figure 2). All subgroups were well balanced between placebo and sildenafil. After 12 weeks of treatment, 46.5% to 87% of patients in the subgroups receiving sildenafil indicated that treatment had improved their erections compared with 11.3% to 41.3% of patients in subgroups receiving placebo. In the 6 trials in which sexual event log data were collected, significantly greater percentages of successful attempts at intercourse were reported by patient subgroups receiving sildenafil (52.6% to 80.1%) compared with patient subgroups receiving placebo (14.0% to 34.5%). All differences were statistically significant (Carson et al 2002).
Figure 2.
Mean score for the Sexual Encounter Profile question 3 (SEP3) for subgroups by erectile dysfunction (ED) characteristics. *p<0.001, †p<0.02, ‡p<0.0002. Copyright © 2002. Carson CC, Burnett AL, Levine LA, et al. 2002. The efficacy of sildenafil citrate (Viagra) in clinical populations: an update. Urology, 60:12–27.
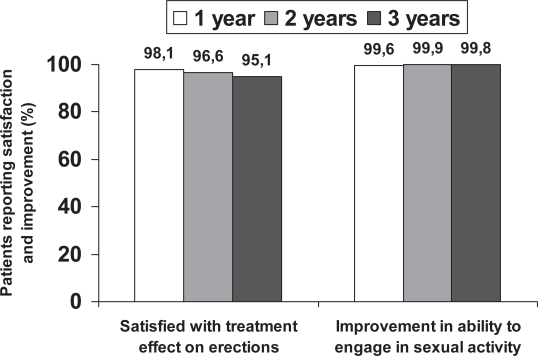
Long-term effectiveness of sildenafil was assessed in 3 open-label, flexible-dose (25 mg to 100 mg) studies. After 12 months of treatment (3 years in one study) or at the time of discontinuation, patients were asked if they were satisfied with the effect of the medication on erections, and if the treatment improved their ability to engage in sexual activity. Satisfaction and improvement in ability to engage in sexual activity reported in 96% and 99% of patients respectively. Of the 11% of patients who discontinued treatment, 2% discontinued for treatment-related reasons (1.6% for insufficient response, 0.4% for adverse events). These satisfaction rates maintained for 3 years in one study. Over the 3-year period, 32% of patients discontinued treatment. Only 6.7% of discontinuations were treatment related (5.7% for insufficient response, 1% for treatment-related adverse events). The remaining 25.3% of patients discontinued for reasons not related to treatment (eg, non–treatment-related adverse events, lost to follow-up evaluation, withdrawn consent, and protocol violations). Most patients were receiving 100 mg sildenafil doses (88% at 3 years) (Carson et al 2002). Similar efficacy rates for sildenafil were reported in clinical practice setting. An improvement in ability to achieve erections was reported by 68% and 71% of patients with ED (Marks et al 1999; McMahon et al 2000). Success with sildenafil, defined as 75% successful intercourse, was reported by 82% of patients with 77% being successful at every attempt (Guay et al 2001).
Despite the proven long-term efficacy of PDE5i, it has been suggested that tachyphylaxis to this therapy may develop. Long-term treatment with PDE5i and excessive cGMP accumulation may up-regulate PDE5 (El-Galley et al 2001). Such hypothesis however, has not been proven in the existing clinical trials with chronic PDE5i therapy (Behr-Roussel et al 2005; Musicki et al 2005). Currently, there are no evidence-based data to support tachyphylaxis in patients treated with sildenafil or any other PDE5i.
Efficacy in subpopulations of men with ED
The efficacy of sildenafil in almost every subgroup of patients with ED is more than established. Response rates in elderly men (≥65 years) are comparable with general population regardless of age (Wagner et al 2001). No differences in response rates were demonstrated in ethnic groups (Young et al 2002). In type 1 diabetic patients, 66.6% reported improved erections (GAQ) and 63% reported successful intercourse attempts compared with 28.6% and 33% by those taking placebo, respectively (Stuckey et al 2003). In another multicenter, randomized, double-blind, placebo-controlled, flexible dose-escalation study in diabetic patients, 56% of patients reported improved erections and 61% reported at least 1 successful intercourse attempt compared with 10% and 22% in the placebo group, respectively (Rendell et al 1999). Diabetic patients are one of the most difficult to treat subgroups (Behrend et al 2005). In patients after bilateral nerve-sparing radical prostatectomy, 76% responded to sildenafil (defined as successful vaginal intercourse) (Raina et al 2004). A favorable response to sildenafil in patients with ischemic heart disease (GEQ and IIEF Q3 and Q4) who were receiving b-blockers and/or angiotensin-converting enzyme inhibitors and/or calcium channel blockers has been observed (Olsson and Persson 2001). Similar results presented in patients with hypertension (taking different or multiple antihypertensive drugs). High efficacy rates presented in patients on chronic dialysis for renal failure (lower doses and longer intervals between treatments are usually required) (Chen et al 2001; Mahon et al 2005), after renal transplantation (Prieto Castro et al 2001; Sharma et al 2006), in spinal cord injuries (Derry et al 2002; Deforge et al 2006) and patients with depression (treated with selective serotonin reuptake inhibitors [SSRIs] or not) (Seidman et al 2001; Nurnberg et al 2002) or patients treated with antipsychotic agents (Gopalakrishnan et al 2006).
Treatment satisfaction and quality of life
Both patients and partners report higher levels of satisfaction (assessed with the Erectile Dysfunction Inventory of Treatment Satisfaction [EDITS] questionnaire) after sildenafil treatment relative to placebo (Lewis et al 2001). Patients receiving sildenafil had significantly higher scores (73.6 ± 3.2) than did those receiving placebo (48.4 ± 3.2, p<0.001). The scores on the partner version of the EDITS were also significantly higher among the partners of men who received sildenafil (63.9 ± 8.1) than among the partners of those who received placebo (33.3 ± 7.5, p<0.001). A high level of treatment satisfaction (65%) reported in another clinical practice study (assessed by 5-item scale) (Jarow et al 1999). Treatment satisfaction was correlated with ED severity (41% in severe, 78% in moderate, and 100% in mild ED) and etiology (56% in neurologic causes, 58% in diabetes, 35% in radical prostatectomy, 89% in psychogenic causes, and 86% in vasculogenic causes). However, no particular characteristic predicted absolute failure with sildenafil. Sildenafil also improved all aspects of health-related quality of life (assessed by SF-36 or Q13 and Q14 of the IIEF) in general ED population or subgroups such as spinal cord injuries (Hultling et al 2000; Giuliano et al 2001; Fujisawa et al 2002). Significant improvements in self-esteem, confidence, sexual relationship satisfaction, and overall relationship satisfaction after treatment of ED with sildenafil were reported by Althof and colleagues (2006) using the self-esteem and relationship questionnaire (SEAR) in a cross-cultural double-blind, placebo controlled, flexible dose study (Althof et al 2006; Cappelleri et al 2006). Treatment satisfaction is also maintained through time (Figure 3) (Carson et al 2002).
Figure 3.
Patients reporting satisfaction with treatment effect on erections and improvement in ability to engage in sexual activity at end of 1 year, 2 years, and 3 years of open-label treatment with sildenafil. Copyright © 2002. Carson CC, Burnett AL, Levine LA, et al. 2002. The efficacy of sildenafil citrate (Viagra) in clinical populations: an update. Urology, 60:12–27.
Data on partner satisfaction support the patients’ satisfaction. For the partners of sildenafil-treated patients, 74% (younger than 65 years) and 67% (65 years or older) were satisfied with the treatment compared with the partners of placebo-treated patients (35% and 22% respectively) (Montorsi and Althof 2004). Satisfaction defined as EDITS score of greater than 50. The quality of partnership as perceived by both the men and their female partners is significantly better in ED patients treated with sildenafil than in untreated controls (Muller et al 2001). More than 90% of partners reported satisfaction with treatment in an open prospective study of men with ED receiving sildenafil for 10 weeks (Gil et al 2001).
Safety
Adverse events and discontinuation rates
Sildenafil has been on the market for more than 8 years. Morales and colleagues (1998) provided summarized safety until 1998 and Padma-Nathan and colleagues (2002) provided long-term safety data (>4 years). The most commonly reported treatment-related adverse events are headache, facial flushing, dyspepsia, dizziness, nasal congestion, abnormal vision, and palpitation (Table 2). Other adverse events uncommonly or rarely reported include back pain, influenza-like syndrome, rash, vomiting, diarrhea, cardiac arrhythmia, and hypersensitivity reactions. Adverse events are dose related, mild in nature, self-limited by continuous use. The drop-out rate due to adverse events is similar to placebo (2% for sildenafil vs 2.3% for placebo). Post-marketing case series reported higher incidence of adverse events, especially for headache (9%–39%), flushing (7%–33%) and abnormal vision (5%–11%) (Zippe et al 1998; Jarow et al 1999; Marks et al 1999; McMahon et al 2000; Moreira et al 2000; Fagelman et al 2001; Guay et al 2001; Martinez-Jabaloyas et al 2001; Palumbo et al 2001). Patients may tolerate sildenafil differently based on existing comorbidities. Ischemic heart disease and hypertension are associated with higher incidence of adverse events than diabetes (3.6%, 2.3%, and 1.9%, respectively) (Padma-Nathan et al 2002). Visual disturbances (blurred vision, flashing lights, blue haze, and change in color perception) occur due to weak inhibition of PDE6 in the retina. They are coincident with peak plasma concentrations of sildenafil and are transient and fully reversible. None persisted 6 hours after taking sildenafil and rarely consist a reason to discontinue treatment.
Table 2.
Common adverse events (>1%) of sildenafil (from European Medicine Agency statements on product characteristics)
| Adverse event | Sildenafil | Placebo |
|---|---|---|
| Headache | 10.8% | 2.8% |
| Flushing | 10.9% | 1.4% |
| Abnormal vision | 3.6% | 0.4% |
| Dyspepsia | 3% | 0.4% |
| Nasal congestion | 2.1% | 0.3% |
| Dizziness | 2.9% | 1% |
| Palpitation | 1% | 0.2% |
Cardiovascular safety
Clinical trials and post marketing data of sildenafil demonstrated no increase in myocardial infarction rates in patients that received these agents as part of either double blind, placebo controlled trials or open label studies or compared to expected rates in aged matched populations of men (Boshier et al 2004). Sildenafil does not adversely affect total exercise time or time to ischemia during exercise testing in men with stable angina. In fact, it may actually improve exercise tests. Sildenafil does not alter cardiac contractility, cardiac output or myocardial oxygen consumption based on evidence reviewed to date (Gillies et al 2002; Vlachopoulos et al 2003; Kukreja et al 2004; Webster et al 2004).
Several new studies have proven not only the cardiovascular safety of sildenafil, but have also suggested that sildenafil may have a cardioprotective role. PDE5A inhibition by sildenafil blunts systolic responses to beta-adrenergic stimulation suggesting a possible role in modifying stimulated cardiac function (Borlaug et al 2005). Chronic inhibition of cGMP phosphodiesterase 5A by sildenafil prevents and reverses cardiac hypertrophy (Takimoto et al 2005). Finally, sildenafil is the only PDE5i that improved arterial oxygenation in patients with pulmonary hypertension (Ghofrani et al 2004) and it has been recently approved in doses of 20 mg and 40 mg, taking every 8 h life-long by patients with pulmonary hypertension (Galie et al 2005).
Princeton guidelines on use of PDE5i
The Princeton Consensus Recommendations were developed to provide instructions to physicians who treat men with CVD and ED and answer the most common question: is it safe to take PDE5i and engage in sexual activity? (Kostis et al 2005). Physicians should consider the cardiovascular status of their patients seeking treatment for ED since there is a degree of risk associated with sexual activity. Three risk categories of CVD were described. Patients in the low risk category (controlled hypertension, stable angina, successful coronary revascularization, history of uncomplicated myocardial infarction, mild valvular disease, and no symptoms with <3 cardiovascular risk factors) can be safely encouraged to initiate or resume sexual activity or receive treatment for their sexual dysfunction. Patients in the intermediate-risk category include those with moderate angina, recent myocardial infarction (<6 weeks), left ventricular dysfunction and/or class II congestive heart failure, non-sustained low-risk arrhythmias and ≥3 risk factors for coronary artery disease. These patients should receive further cardiologic evaluation to determine if they can be restratified into the low- or highrisk cardiovascular categories. Finally, patients in the high-risk category should be stabilized for their cardiac condition before resuming sexual activity or receiving treatment for their sexual dysfunction. It is important to emphasize that the use of any form of nitrate with all PDE5i is contraindicated because of the increased likelihood of hypotension.
Sildenafil and alpha adrenergic antagonists
Alpha adrenergic antagonists are commonly used drugs in patients with BPH-related LUTS. Although the adverse event profile of sildenafil is not worsened by a background of anti-hypertensive medicines, even when the patient is on multiple antihypertensive agents, it appears to have some interaction with alpha blockers, which may result in clinically significant orthostatic hypotension under some conditions (Kostis et al 2005). This is most likely to occur in patients treated with doxazosin (a long-acting alpha blocker). Today, alpha blockers are no longer considered a contraindication for sildenafil, but precautions in the use of these drugs are listed. Patients who demonstrate hemodynamic instability on alpha-blocker therapy alone are at increased risk of symptomatic hypotension with concomitant use of sildenafil. Therefore, patients should be stable on alpha-blocker therapy prior to initiating sildenafil. Treatment with sildenafil must be initiated at the lowest recommended dose, while it should be taken 3–4 h apart from antihypertensive administration.
Sildenafil and non-arteritic anterior ischemic optic neuropathy (NAION)
Non-arteritic anterior ischemic optic neuropathy (NAION) is characterized by acute ischemia of the anterior portion of the optic nerve in the absence of provable arteritis, which may result in visual field defect or vision loss. No effective treatment is available and prevention is limited to the treatment of risk factors mainly aiming at decreasing the risk of a similar event in the fellow eye. Numerous risk factors have been reported for NAION, mainly cardiovascular risk factors, including hypertension, diabetes, and hypercholesterolemia. Lastly, the potential relationship between non-arteritic anterior ischemic optic neuropathy (NAION) and PDE5i use has raised important questions and a strong reaction not only among regulatory agencies, but also within the scientific community and mass media as well.
There are 16 NAION case reports published in association with sildenafil. A few of the cases associated with sildenafil use experienced temporary partial visual loss that became a fixed visual loss upon rechallenge (Hatzichristou 2005). As sildenafil has been used by more than 30 million men worldwide and the incidence of NAION has been reported as 2.3 per 100 000 persons, we would expect far more than the reported 16 cases associated with the use of sildenafil. According to the European Medicines Agency (EMEA) labeling however, patients taking or considering taking PDE5i should inform their healthcare professionals if they have ever had severe loss of vision, which might reflect a prior episode of NAION, as such patients are at an increased risk of developing NAION again and they should be referred to the ophthalmologist (Wespes et al 2006).
Management strategy for treatment failures
Definition of treatment failure to sildenafil
Although the term ‘treatment failure’ to oral drugs is widely used, there is no precise definition of what exactly means. Treatment failure may be due to medication, clinician and patient issues (Table 3). Based on these issues a definition of a non-responder to oral pharmacotherapy is proposed: “an inadequate erectile response after at least 4 attempts of the highest tolerated drug dose in accordance with manufacturer’s guidelines with respect to timing relative to meals, alcohol ingestion, use of concomitant medications, and adequate sexual stimulation/arousal” (Carson et al 2004).
Table 3.
Factors leading to an inadequate trial of oral pharmacotherapy
| Medication issues | Clinician issues | Patient issues |
|---|---|---|
| Published efficacy rates | Inadequate administration instructions | Unrealistic expectations |
| Special populations reflect variable responses (difficult-to-treat subgroups) | Inappropriate dosing | Lack of persistence |
| Side-effects | Misdiagnosis
Lack of follow up |
Fear
Unaddressed psychological issues Partner issues |
Besides these reasons for inappropriate intake of sildenafil, one of the most common causes of discontinuation of a drug that is considered as treatment failure is the lack of follow-up of the patients. Erectile dysfunction is a chronic disease. Follow-up visits are essential to improve physician–patient communication, solve treatment problems that may have occurred, identify any change in potency status or new medical conditions and offer continuing education to patients and their partners. These essential aspects in managing ED patients can be easily remembered by the acronym, FAST (Follow-up of patients, Adjustment of time of administration, Sexual stimulation, and Titration to the maximum tolerated dose) (Hatzichristou 2002).
Identifying truly treatment failures
In order to identify truly treatment failures, the physician need to address all the medication, clinician and patient/partner issues that were previously presented. The probability of a misdiagnosis due to incomplete basic diagnostic evaluation from a non-expert physician must also be investigated (Hatzichristou et al 2002). These are patients with hypogonadism or hyperprolactinemia who need specific hormonal manipulation in order to cure erectile dysfunction (Greenstein et al 2005), patients with Peyronie’s disease who need treatment for penile curvature or pain during intercourse, and patients who do not have erectile dysfunction but they experience ejaculatory dysfunction or sensory disturbances.
After proper counseling and instructions were given, the patient is encouraged for a re-trial of the oral drug for at least 4 attempts for intercourse with the new instructions on administration, as a recent study revealed inappropriate intake of sildenafil in 56% of treatment failures (Hatzichristou et al 2005). After adequate instructions on the proper use of sildenafil, one third of the initially non-responders to sildenafil converted to responders. The most easily reversible factor for treatment failure was the administration of sildenafil just before initiation of sexual activity followed by absence of sexual desire on sildenafil uptake and use of the drug with a full stomach. In this study, 12% of sildenafil failures were not aware that sexual stimulation was mandatory to achieve an erection, but 50% of them converted to responders when they were explained that sildenafil does not possess aphrodisiac properties. Additionally, 63.6% of the patients who initially used the drug just before the initiation of sexual intercourse and 34.4% of those who took sildenafil with a full stomach responded to sildenafil with appropriate timing of administration.
Similar results were presented by other studies. Incorrect administration accounted for 81% of sildenafil failures referred by primary care physicians (Atiemo et al 2003). Reasons included administration after heavy meals, lack of sexual stimulation, short timing to intercourse, and too few attempts for intercourse. The authors were able to salvage 41.5% of nonresponders after reeducation as measured by the General Assessment Question (GAG) and Sexual Health Inventory for Men (SHIM) scores. Gruenwald and colleagues (2006) showed that counseling and dose adjustment were directly influential in achieving an excellent response to a second trial of sildenafil in patients with ED who had previously failed treatment with the drug, and obviated their needing to seek more invasive measures. In this study, 38% of the included patients did not receive any explanations or counseling whatsoever from the prescribing physician. After proper instruction, erectile function domain scores increased significantly and overall 23.6% of the patients had a normal IIEF EF domain score (≥26) at the end of the study.
A patient is considered as truly non-responder, if retrial of oral therapy after proper counseling and instruction administration fails.
Treatment of truly non-responders
Today, it is widely accepted that treatment approach follows a step-wise model. A patient failing oral pharmacotherapy has to go on second line therapies that include intracavernosal injections and combination treatments. If he further fails second line therapies, the only option is a third line therapy that is implantation of a penile prosthesis.
Preliminary data show that higher doses of sildenafil (up to 200 mg) may salvage some patients who where sildenafil nonresponders. McMahon (2002) concluded that sildenafil at doses of up to 200 mg is an effective salvage therapy for 24.1% of previous sildenafil non-responders but is limited by a significantly higher incidence of adverse effects and a 31% treatment discontinuation rate. McMahon and colleagues (1999) also used sildenafil as salvage therapy in intracavernosal injection non-responders (alprostadil or tri-mix). They were able to salvage 31% of patients with combination of sildenafil with intracavernosal injection of tri-mix. However, combination therapy was associated with a 33% incidence of adverse effects, including a 20% incidence of dizziness side effects (McMahon et al 1999). Finally, preliminary data suggest a possible role for combination treatment with cabergoline (Safarinejad 2006) or statins (Herrmann et al 2006; Osborne 2006) in non-responders to sildenafil alone.
Intracavernosal injections remain an excellent treatment option with proven efficacy and safety over time. Baniel and colleagues (2001) treated sildenafil non-responders after radical prostatectomy with intracavernosal injections of vasoactive drugs with 85% success rate. Shabsigh and colleagues (2000) were able to salvage sildenafil non responders with intracavernosal injections of alprostadil. More than 85% improvement in Q3 and Q4 of the IIEF was recorded (Shabsigh et al 2000). The tri-mix combination (papaverine, phentolamine, alprostadil) is certainly the more efficacious drug treatment for erectile dysfunction and can be used in severe cases of erectile dysfunction when intravernous alprostadil fails or it is not preferable due to side effects.
The patient should be given every opportunity to choose among options, and to determine which fits best to his special needs and expectations. The clinician should also provide a supportive environment for shared decision-making. This management strategy must be supplemented by a careful follow-up in order to identify changes in patients’ expectations, possible side effects that may need treatment optimization.
Use of sildenafil in aging men
The normal aging process and age related risk factor accumulation contribute to the increased prevalence of erectile dysfunction in the elderly. Systemic changes and alterations in the structure and function of the penis in elderly men include hormonal changes (mainly testosterone decrease and increase in sex hormone binding globulin that resulting decreased bioavailability of testosterone) (Margolese 2000), decrease in elastic fibers and increase in collagen fibers in the tunica albuginea (Akkus et al 1997) and molecular changes (decrease in nitric oxide synthase) (Andrew and Mayer 1999).
Older men (aged ≥65 years) have higher plasma concentrations of sildenafil compared with younger men (18–45 years), with mean maximum concentration (Cmax) 70% greater in older men and mean area under the curve (AUC) 84% higher compared with the younger age group. Due to age-differences in plasma protein binding, the corresponding increase in free sildenafil plasma concentration was approximately 40%. However, no differences in the safety of any dose of sildenafil were observed in older patients compared with younger men. Therefore, dosage adjustments are not required in elderly patients (Seftel 2003). Sildenafil significantly improves erectile function in elderly patients with erectile dysfunction of broad etiology although efficacy rates may be lower compared with younger men due to the normal aging process and age related risk factor accumulation mentioned before (Rendell et al 1999; Wagner et al 2001; Carson et al 2002).
The need for a patient-centered care model in sexual medicine
Erectile dysfunction is a self-reported condition by the patients and the results of different treatment modalities are also self-evaluated (Hatzimouratidis and Hatzichristou 2005). Recent data on ED treatment outcome have shown that many patients discontinue treatment, despite the availability of efficacious pharmacotherapies, because doctors fail to inform patients properly and to ensure continuity in care, as well as to be routinely involved in asking patients about their needs and expectations (Mulhall et al 1999; Hatzichristou et al 2005). Althof (2002) described several causes that may contribute, including the length of time the couple were asexual before seeking treatment, the man’s approach to resuming a sexual life with his partner, the female partner’s physical and emotional readiness to resume lovemaking, the meaning for each partner of using a medical intervention to enable intercourse and the quality of the nonsexual aspects of the relationship. It becomes apparent that patients’ needs and expectations vary widely and the treatment approach should always be individualized according to their preference for information and involvement in the decision-making process. Patient satisfaction is a complex issue that depends not only on therapeutic outcomes in terms of efficacy and adverse events or complications but also on expectations from treatment and relationship dynamics.
Such observations augment the need for the development of care model in sexual medicine, as it happens with every other chronic condition, such as diabetes mellitus and CVD. In addition, it becomes clear that we are running to the era where personalized medicine will replace traditional schema; diagnosis is integrated with therapy for selection of the treatment as well for monitoring the outcome. Development and adaptation of a patient-centered care model in sexual medicine will increase efficacy and safety of currently and future treatments, as well as patients’ adherence, with certain benefits not only for our patients, but also for the healthcare systems, especially in terms of cost-effectiveness.
Future perspectives
Prophylactic use of sildenafil
Early use of vasoactive agents has been shown to rehabilitate erectile function after nerve sparing radical retropubic prostatectomy (RRP) (Montorsi et al 2004).
In a double-blind, placebo-controlled study, sildenafil (50 mg–100 mg) taken every night for 9 months, starting 1 month after nerve sparing radical prostatectomy was associated with recovery of spontaneous erections in 27% of patients compared with 4% of patients taking placebo (Padma-Nathan et al 2003). Schwartz and colleagues (2004), in a study of 40 potent volunteers with prostate cancer who underwent RRP, showed that sildenafil administration every other night for 6 months, substantially increases corporal smooth muscle content. The most promising prophylactic role of sildenafil is clearly the preservation of the smooth muscle of the corpora cavernosa.
Sildenafil in patients with lower urinary tract symptoms (LUTS)
Lower urinary tract symptoms (LUTS) are independent risk factors for sexual dysfunction in older men (Rosen et al 2003). A possible role for PDE5i in the treatment of LUTS has been presented (McVary 2005). Sairam and colleagues (2002) showed that ED treatment with sildenafil improved both sexual function scores (based on IIEF) and LUTS and urinary scores correlated strongly with sexual function scores at 3 months. Mulhall and colleagues (2006), in a group of ED patients treated with sildenafil, similarly noticed that 60% of men improved their IPSS score, and 35% had at least a 4-point improvement in their score. If ongoing clinical research proves these preliminary data, it will open the avenue for innovative therapeutic approaches.
Sildenafil in patients with premature ejaculation
PDE5i have been suggested to be beneficial for patients with premature ejaculation, possibly due to a peripheral inhibition of contractile response of vas deferens, seminal vesicles, prostate, and urethra as well as a reduced central sympathetic output through a prolonged NO effect (Abdel-Hamid 2004). Combination of sildenafil with paroxetine prolongs significantly intravaginal ejaculation latency time (IELT) and is associated with better intercourse satisfaction compared with paroxetine alone (Salonia et al 2002). In a group of nonresponders to other treatments, sildenafil combined with paroxetine and psychological -behavioral counseling alleviated premature ejaculation (Chen et al 2003). On the contrary, sildenafil was not superior to placebo or combination treatment with topical lidocain/prilocain cream. Further placebo-controlled, well designed studies are needed to determine whether there is any role for sildenafil in the treatment of premature ejaculation.
Conclusions
Sildenafil is a highly effective treatment associated with a good safety and tolerability profile in men with ED. It is also effective in several subpopulations although efficacy is lower in the so called difficult-to-treat subpopulations such as patients with diabetes mellitus or after radical prostatectomy, including men in older age groups. Sildenafil significantly improves satisfaction and quality of life for both patients and partners. Furthermore, new data from basic and clinical research suggest a possible role in the future for several other chronic conditions.
References
- Abdel-Hamid IA. Phosphodiesterase 5 inhibitors in rapid ejaculation: potential use and possible mechanisms of action. Drugs. 2004;64:13–26. doi: 10.2165/00003495-200464010-00002. [DOI] [PubMed] [Google Scholar]
- Akkus E, Carrier S, Baba K, et al. Structural alterations in the tunica albuginea of the penis: impact of Peyronie’s disease, ageing and impotence. Br J Urol. 1997;79:47–53. doi: 10.1046/j.1464-410x.1997.26511.x. [DOI] [PubMed] [Google Scholar]
- Althof SE. When an erection alone is not enough: biopsychosocial obstacles to lovemaking. Int J Impot Res. 2002;14(Suppl 1):S99–104. doi: 10.1038/sj.ijir.3900799. [DOI] [PubMed] [Google Scholar]
- Althof SE, O’Leary MP, Cappelleri JC, et al. Sildenafil citrate improves self-esteem, confidence, and relationships in men with erectile dysfunction: Results from an international, multi-center, double-blind, placebo-controlled trial. J Sex Med. 2006;3:521–9. doi: 10.1111/j.1743-6109.2006.00234.x. [DOI] [PubMed] [Google Scholar]
- Andrew PJ, Mayer B. Enzymatic function of nitric oxide synthases. Cardiovasc Res. 1999;43:521–31. doi: 10.1016/s0008-6363(99)00115-7. [DOI] [PubMed] [Google Scholar]
- Atan A, Basar MM, Tuncel A, et al. Comparison of efficacy of sildenafil-only, sildenafil plus topical EMLA cream, and topical EMLA-cream-only in treatment of premature ejaculation. Urology. 2006;67:388–91. doi: 10.1016/j.urology.2005.09.002. [DOI] [PubMed] [Google Scholar]
- Atiemo HO, Szostak MJ, Sklar GN. Salvage of sildenafil failures referred from primary care physicians. J Urol. 2003;170:2356–8. doi: 10.1097/01.ju.0000096221.67967.ae. [DOI] [PubMed] [Google Scholar]
- Aytac IA, McKinlay JB, Krane RJ. The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU Int. 1999;84:50–6. doi: 10.1046/j.1464-410x.1999.00142.x. [DOI] [PubMed] [Google Scholar]
- Ballard SA, Gingell CJ, Tang K, et al. Effects of sildenafil on the relaxation of human corpus cavernosum tissue in vitro and on the activities of cyclic nucleotide phosphodiesterase isozymes. J Urol. 1998;159:2164–71. doi: 10.1016/S0022-5347(01)63299-3. [DOI] [PubMed] [Google Scholar]
- Baniel J, Israilov S, Segenreich E, et al. Comparative evaluation of treatments for erectile dysfunction in patients with prostate cancer after radical retropubic prostatectomy. BJU Int. 2001;88:58–62. doi: 10.1046/j.1464-410x.2001.02254.x. [DOI] [PubMed] [Google Scholar]
- Behr-Roussel D, Gorny D, Mevel K, et al. Chronic sildenafil improves erectile function and endothelium-dependent cavernosal relaxations in rats: lack of tachyphylaxis. Eur Urol. 2005;47:87–91. doi: 10.1016/j.eururo.2004.09.005. [DOI] [PubMed] [Google Scholar]
- Behrend L, Vibe-Petersen J, Perrild H. Sildenafil in the treatment of erectile dysfunction in men with diabetes: demand, efficacy and patient satisfaction. Int J Impot Res. 2005;17:264–9. doi: 10.1038/sj.ijir.3901302. [DOI] [PubMed] [Google Scholar]
- Boolell M, Allen MJ, Ballard SA, et al. Sildenafil: an orally active type 5 cyclic GMP-specific phosphodiesterase inhibitor for the treatment of penile erectile dysfunction. Int J Impot Res. 1996;8:47–52. [PubMed] [Google Scholar]
- Borlaug BA, Melenovsky V, Marhin T, et al. Sildenafil inhibits beta-adrenergic-stimulated cardiac contractility in humans. Circulation. 2005;112:2642–9. doi: 10.1161/CIRCULATIONAHA.105.540500. [DOI] [PubMed] [Google Scholar]
- Boshier A, Wilton LV, Shakir SA. Evaluation of the safety of sildenafil for male erectile dysfunction: experience gained in general practice use in England in 1999. BJU Int. 2004;93:796–801. doi: 10.1111/j.1464-410X.2003.04744.x. [DOI] [PubMed] [Google Scholar]
- Braun M, Wassmer G, Klotz T, et al. Epidemiology of erectile dysfunction: results of the ‘Cologne Male Survey’. Int J Impot Res. 2000;12:305–11. doi: 10.1038/sj.ijir.3900622. [DOI] [PubMed] [Google Scholar]
- Cappelleri JC, Bell SS, Althof SE, et al. Comparison between sildenafil-treated subjects with erectile dysfunction and control subjects on the Self-Esteem And Relationship questionnaire. J Sex Med. 2006;3:274–82. doi: 10.1111/j.1743-6109.2005.00205.x. [DOI] [PubMed] [Google Scholar]
- Carson C, Giuliano F, Goldstein I, et al. The ‘effectiveness’ scale—therapeutic outcome of pharmacologic therapies for ED: an international consensus panel report. Int J Impot Res. 2004;16:207–13. doi: 10.1038/sj.ijir.3901227. [DOI] [PubMed] [Google Scholar]
- Carson CC, Burnett AL, Levine LA, et al. The efficacy of sildenafil citrate (Viagra) in clinical populations: an update. Urology. 2002;60:12–27. doi: 10.1016/s0090-4295(02)01687-4. [DOI] [PubMed] [Google Scholar]
- Chen J, Mabjeesh NJ, Greenstein A, et al. Clinical efficacy of sildenafil in patients on chronic dialysis. J Urol. 2001;165:819–21. [PubMed] [Google Scholar]
- Chen J, Mabjeesh NJ, Matzkin H, et al. Efficacy of sildenafil as adjuvant therapy to selective serotonin reuptake inhibitor in alleviating premature ejaculation. Urology. 2003;61:197–200. doi: 10.1016/s0090-4295(02)02075-7. [DOI] [PubMed] [Google Scholar]
- Deforge D, Blackmer J, Garritty C, et al. Male erectile dysfunction following spinal cord injury: a systematic review. Spinal Cord. 2006;44:465–73. doi: 10.1038/sj.sc.3101880. [DOI] [PubMed] [Google Scholar]
- Derry F, Hultling C, Seftel AD, et al. Efficacy and safety of sildenafil citrate (Viagra) in men with erectile dysfunction and spinal cord injury: a review. Urology. 2002;60:49–57. doi: 10.1016/s0090-4295(02)01690-4. [DOI] [PubMed] [Google Scholar]
- Desouza C, Parulkar A, Lumpkin D, et al. Acute and prolonged effects of sildenafil on brachial artery flow-mediated dilatation in type 2 diabetes. Diabetes Care. 2002;25:1336–9. doi: 10.2337/diacare.25.8.1336. [DOI] [PubMed] [Google Scholar]
- El-Galley R, Rutland H, Talic R, et al. Long-term efficacy of sildenafil and tachyphylaxis effect. J Urol. 2001;166:927–31. [PubMed] [Google Scholar]
- Fagelman E, Fagelman A, Shabsigh R. Efficacy, safety, and use of sildenafil in urologic practice. Urology. 2001;57:1141–4. doi: 10.1016/s0090-4295(01)00984-0. [DOI] [PubMed] [Google Scholar]
- Feldman HA, Goldstein I, Hatzichristou DG, et al. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol. 1994;151:54–61. doi: 10.1016/s0022-5347(17)34871-1. [DOI] [PubMed] [Google Scholar]
- Fujisawa M, Sawada K, Okada H, et al. Evaluation of health-related quality of life in patients treated for erectile dysfunction with viagra (sildenafil citrate) using SF-36 score. Arch Androl. 2002;48:15–21. doi: 10.1080/014850102753385161. [DOI] [PubMed] [Google Scholar]
- Galie N, Ghofrani HA, Torbicki A, et al. Sildenafil citrate therapy for pulmonary arterial hypertension. N Engl J Med. 2005;353:2148–57. doi: 10.1056/NEJMoa050010. [DOI] [PubMed] [Google Scholar]
- Gbekor E, Bethell S, Fawcett L, et al. Selectivity of sildenafil and other phoshodiesterase type 5 (PDE5) inhibitors against all human phoshodiesterase families. Eur Urol Suppl. 2002;1:63. [Google Scholar]
- Gemalmaz H, Waldeck K, Chapman TN, et al. In vivo and in vitro investigation of the effects of sildenafil on rat cavernous smooth muscle. J Urol. 2001;165:1010–14. [PubMed] [Google Scholar]
- Ghofrani HA, Voswinckel R, Reichenberger F, et al. Differences in hemodynamic and oxygenation responses to three different phosphodiesterase-5 inhibitors in patients with pulmonary arterial hypertension: a randomized prospective study. J Am Coll Cardiol. 2004;44:1488–96. doi: 10.1016/j.jacc.2004.06.060. [DOI] [PubMed] [Google Scholar]
- Gil A, Martinez E, Oyaguez I, et al. Erectile dysfunction in a primary care setting: results of an observational, no-control-group, prospective study with sildenafil under routine conditions of use. Int J Impot Res. 2001;13:338–47. doi: 10.1038/sj.ijir.3900782. [DOI] [PubMed] [Google Scholar]
- Gillies HC, Roblin D, Jackson G. Coronary and systemic hemodynamic effects of sildenafil citrate: from basic science to clinical studies in patients with cardiovascular disease. Int J Cardiol. 2002;86:131–41. doi: 10.1016/s0167-5273(02)00421-7. [DOI] [PubMed] [Google Scholar]
- Giuliano F, Pena BM, Mishra A, et al. Efficacy results and quality-of-life measures in men receiving sildenafil citrate for the treatment of erectile dysfunction. Qual Life Res. 2001;10:359–69. doi: 10.1023/a:1012270220064. [DOI] [PubMed] [Google Scholar]
- Goldstein I, Lue TF, Padma-Nathan H, et al. Oral sildenafil in the treatment of erectile dysfunction. Sildenafil Study Group. N Engl J Med. 1998;338:1397–404. doi: 10.1056/NEJM199805143382001. [DOI] [PubMed] [Google Scholar]
- Gopalakrishnan R, Jacob KS, Kuruvilla A, et al. Sildenafil in the treatment of antipsychotic-induced erectile dysfunction: a randomized, double-blind, placebo-controlled, flexible-dose, two-way crossover trial. Am J Psychiatry. 2006;163:494–9. doi: 10.1176/appi.ajp.163.3.494. [DOI] [PubMed] [Google Scholar]
- Gori T, Sicuro S, Dragoni S, et al. Sildenafil prevents endothelial dysfunction induced by ischemia and reperfusion via opening of adenosine triphosphate-sensitive potassium channels: a human in vivo study. Circulation. 2005;111:742–6. doi: 10.1161/01.CIR.0000155252.23933.2D. [DOI] [PubMed] [Google Scholar]
- Greenstein A, Mabjeesh NJ, Sofer M, et al. Does sildenafil combined with testosterone gel improve erectile dysfunction in hypogonadal men in whom testosterone supplement therapy alone failed? J Urol. 2005;173:530–2. doi: 10.1097/01.ju.0000149870.36577.05. [DOI] [PubMed] [Google Scholar]
- Gruenwald I, Shenfeld O, Chen J, et al. Positive effect of counseling and dose adjustment in patients with erectile dysfunction who failed treatment with sildenafil. Eur Urol. 2006;50:134–40. doi: 10.1016/j.eururo.2006.01.042. [DOI] [PubMed] [Google Scholar]
- Guay AT, Perez JB, Jacobson J, et al. Efficacy and safety of sildenafil citrate for treatment of erectile dysfunction in a population with associated organic risk factors. J Androl. 2001;22:793–7. [PubMed] [Google Scholar]
- Halcox JP, Nour KR, Zalos G, et al. The effect of sildenafil on human vascular function, platelet activation, and myocardial ischemia. J Am Coll Cardiol. 2002;40:1232–40. doi: 10.1016/s0735-1097(02)02139-3. [DOI] [PubMed] [Google Scholar]
- Hatzichristou D. Phosphodiesterase 5 inhibitors and nonarteritic anterior ischemic optic neuropathy (NAION): coincidence or causality? J Sex Med. 2005;2:751–8. doi: 10.1111/j.1743-6109.2005.00144.x. [DOI] [PubMed] [Google Scholar]
- Hatzichristou D, Hatzimouratidis K, Bekas M, et al. Diagnostic steps in the evaluation of patients with erectile dysfunction. J Urol. 2002;168:615–20. [PubMed] [Google Scholar]
- Hatzichristou D, Moysidis K, Apostolidis A, et al. Sildenafil failures may be due to inadequate patient instructions and follow-up: a study on 100 non-responders. Eur Urol. 2005;47:518–22. doi: 10.1016/j.eururo.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Hatzichristou DG. Sildenafil citrate: lessons learned from 3 years of clinical experience. Int J Impot Res. 2002;14(Suppl 1):S43–52. doi: 10.1038/sj.ijir.3900805. [DOI] [PubMed] [Google Scholar]
- Hatzichristou DG, Pescatori ES. Current treatments and emerging therapeutic approaches in male erectile dysfunction. BJU Int. 2001;88(Suppl 3):11–17. doi: 10.1046/j.1464-4096.2001.123.x. [DOI] [PubMed] [Google Scholar]
- Hatzimouratidis K, Hatzichristou DG. A comparative review of the options for treatment of erectile dysfunction: which treatment for which patient? Drugs. 2005;65:1621–50. doi: 10.2165/00003495-200565120-00003. [DOI] [PubMed] [Google Scholar]
- Herrmann HC, Levine LA, Macaluso J, Jr, et al. Can atorvastatin improve the response to sildenafil in men with erectile dysfunction not initially responsive to sildenafil? Hypothesis and pilot trial results. J Sex Med. 2006;3:303–8. doi: 10.1111/j.1743-6109.2005.00156.x. [DOI] [PubMed] [Google Scholar]
- Hirata K, Adji A, Vlachopoulos C, et al. Effect of sildenafil on cardiac performance in patients with heart failure. Am J Cardiol. 2005;96:1436–40. doi: 10.1016/j.amjcard.2005.06.091. [DOI] [PubMed] [Google Scholar]
- Hultling C, Giuliano F, Quirk F, et al. Quality of life in patients with spinal cord injury receiving Viagra (sildenafil citrate) for the treatment of erectile dysfunction. Spinal Cord. 2000;38:363–70. doi: 10.1038/sj.sc.3101011. [DOI] [PubMed] [Google Scholar]
- Jarow JP, Burnett AL, Geringer AM. Clinical efficacy of sildenafil citrate based on etiology and response to prior treatment. J Urol. 1999;162:722–5. doi: 10.1097/00005392-199909010-00024. [DOI] [PubMed] [Google Scholar]
- Katz SD, Balidemaj K, Homma S, et al. Acute type 5 phosphodiesterase inhibition with sildenafil enhances flow-mediated vasodilation in patients with chronic heart failure. J Am Coll Cardiol. 2000;36:845–51. doi: 10.1016/s0735-1097(00)00790-7. [DOI] [PubMed] [Google Scholar]
- Kostis JB, Jackson G, Rosen R, et al. Sexual dysfunction and cardiac risk (the Second Princeton Consensus Conference) Am J Cardiol. 2005;96:313–21. doi: 10.1016/j.amjcard.2005.03.065. [DOI] [PubMed] [Google Scholar]
- Kukreja RC, Ockaili R, Salloum F, et al. Cardioprotection with phosphodiesterase-5 inhibition—a novel preconditioning strategy. J Mol Cell Cardiol. 2004;36:165–73. doi: 10.1016/j.yjmcc.2003.11.001. [DOI] [PubMed] [Google Scholar]
- Langtry HD, Markham A. Sildenafil: a review of its use in erectile dysfunction. Drugs. 1999;57:967–89. doi: 10.2165/00003495-199957060-00015. [DOI] [PubMed] [Google Scholar]
- Lewis R, Bennett CJ, Borkon WD, et al. Patient and partner satisfaction with Viagra (sildenafil citrate) treatment as determined by the Erectile Dysfunction Inventory of Treatment Satisfaction Questionnaire. Urology. 2001;57:960–5. doi: 10.1016/s0090-4295(01)00945-1. [DOI] [PubMed] [Google Scholar]
- Mahon A, Sidhu PS, Muir G, et al. The efficacy of sildenafil for the treatment of erectile dysfunction in male peritoneal dialysis patients. Am J Kidney Dis. 2005;45:381–7. doi: 10.1053/j.ajkd.2004.10.012. [DOI] [PubMed] [Google Scholar]
- Margolese HC. The male menopause and mood: testosterone decline and depression in the aging male – is there a link? J Geriatr Psychiatry Neurol. 2000;13:93–101. doi: 10.1177/089198870001300208. [DOI] [PubMed] [Google Scholar]
- Marks LS, Duda C, Dorey FJ, et al. Treatment of erectile dysfunction with sildenafil. Urology. 1999;53:19–24. doi: 10.1016/s0090-4295(98)00525-1. [DOI] [PubMed] [Google Scholar]
- Martin-Morales A, Sanchez-Cruz JJ, Saenz de Tejada I, et al. Prevalence and independent risk factors for erectile dysfunction in Spain: results of the Epidemiologia de la Disfuncion Erectil Masculina Study. J Urol. 2001;166:569–74. doi: 10.1016/s0022-5347(05)65986-1. [DOI] [PubMed] [Google Scholar]
- Martinez-Jabaloyas JM, Gil-Salom M, Villamon-Fort R, et al. Prognostic factors for response to sildenafil in patients with erectile dysfunction. Eur Urol. 2001;40:641–6. doi: 10.1159/000049850. [DOI] [PubMed] [Google Scholar]
- McMahon CG. High dose sildenafil citrate as a salvage therapy for severe erectile dysfunction. Int J Impot Res. 2002;14:533–8. doi: 10.1038/sj.ijir.3900936. [DOI] [PubMed] [Google Scholar]
- McMahon CG, Samali R, Johnson H. Treatment of intracorporeal injection nonresponse with sildenafil alone or in combination with triple agent intracorporeal injection therapy. J Urol. 1999;162:1992–7. doi: 10.1016/S0022-5347(05)68085-8. [DOI] [PubMed] [Google Scholar]
- McMahon CG, Samali R, Johnson H. Efficacy, safety and patient acceptance of sildenafil citrate as treatment for erectile dysfunction. J Urol. 2000;164:1192–6. [PubMed] [Google Scholar]
- McVary KT. Erectile dysfunction and lower urinary tract symptoms secondary to BPH. Eur Urol. 2005;47:838–45. doi: 10.1016/j.eururo.2005.02.001. [DOI] [PubMed] [Google Scholar]
- Moncada I, Jara J, Subira D, et al. Efficacy of sildenafil citrate at 12 hours after dosing: re-exploring the therapeutic window. Eur Urol. 2004;46:357–60. doi: 10.1016/j.eururo.2004.04.025. [DOI] [PubMed] [Google Scholar]
- Montorsi F, Althof SE. Partner responses to sildenafil citrate (Viagra) treatment of erectile dysfunction. Urology. 2004;63:762–7. doi: 10.1016/j.urology.2003.11.018. [DOI] [PubMed] [Google Scholar]
- Montorsi F, Briganti A, Salonia A, et al. Current and future strategies for preventing and managing erectile dysfunction following radical prostatectomy. Eur Urol. 2004;45:123–33. doi: 10.1016/j.eururo.2003.08.016. [DOI] [PubMed] [Google Scholar]
- Montorsi F, Briganti A, Salonia A, et al. Erectile dysfunction prevalence, time of onset and association with risk factors in 300 consecutive patients with acute chest pain and angiographically documented coronary artery disease. Eur Urol. 2003;44:360–4. doi: 10.1016/s0302-2838(03)00305-1. [DOI] [PubMed] [Google Scholar]
- Morales A, Gingell C, Collins M, et al. Clinical safety of oral silde-nafil citrate (VIAGRA) in the treatment of erectile dysfunction. Int J Impot Res. 1998;10:69–73. doi: 10.1038/sj.ijir.3900354. [DOI] [PubMed] [Google Scholar]
- Moreira SG, Jr, Brannigan RE, Spitz A, et al. Side-effect profile of sildenafil citrate (Viagra) in clinical practice. Urology. 2000;56:474–6. doi: 10.1016/s0090-4295(00)00649-x. [DOI] [PubMed] [Google Scholar]
- Mulhall JP, Guhring P, Parker M, et al. Assessment of the impact of sildenafil citrate on lower urinary tract symptoms in men with erectile dysfunction. J Sex Med. 2006;3:662–7. doi: 10.1111/j.1743-6109.2006.00259.x. [DOI] [PubMed] [Google Scholar]
- Mulhall JP, Jahoda AE, Cairney M, et al. The causes of patient dropout from penile self-injection therapy for impotence. J Urol. 1999;162:1291–4. [PubMed] [Google Scholar]
- Muller MJ, Ruof J, Graf-Morgenstern M, et al. Quality of partnership in patients with erectile dysfunction after sildenafil treatment. Pharmacopsychiatry. 2001;34:91–5. doi: 10.1055/s-2001-14277. [DOI] [PubMed] [Google Scholar]
- Musicki B, Champion HC, Becker RE, et al. In vivo analysis of chronic phosphodiesterase-5 inhibition with sildenafil in penile erectile tissues: no tachyphylaxis effect. J Urol. 2005;174:1493–6. doi: 10.1097/01.ju.0000173006.47623.2c. [DOI] [PubMed] [Google Scholar]
- Nurnberg HG, Seidman SN, Gelenberg AJ, et al. Depression, anti-depressant therapies, and erectile dysfunction: clinical trials of sildenafil citrate (Viagra) in treated and untreated patients with depression. Urology. 2002;60:58–66. doi: 10.1016/s0090-4295(02)01691-6. [DOI] [PubMed] [Google Scholar]
- Olsson AM, Persson CA. Efficacy and safety of sildenafil citrate for the treatment of erectile dysfunction in men with cardiovascular disease. Int J Clin Pract. 2001;55:171–6. [PubMed] [Google Scholar]
- Osborne T. Statin treatment improves erectile dysfunction in sildenafil nonresponders. Nat Clin Pract Urol. 2006;3:239–40. [Google Scholar]
- Padma-Nathan H, Eardley I, Kloner RA, et al. A 4-year update on the safety of sildenafil citrate (Viagra) Urology. 2002;60:67–90. doi: 10.1016/s0090-4295(02)01752-1. [DOI] [PubMed] [Google Scholar]
- Padma-Nathan H, Mc Cullough AR, Giulano F, et al. Postoperative nightly administration of sildenafil citrate significantly improves the return of normal spontaneous erectile function after bilateral nerve-sparing radical prostatectomy. J Urol. 2003;169(Suppl):375. [Google Scholar]
- Padma-Nathan H, Stecher VJ, Sweeney M, et al. Minimal time to successful intercourse after sildenafil citrate: results of a randomized, double-blind, placebo-controlled trial. Urology. 2003;62:400–3. doi: 10.1016/s0090-4295(03)00567-3. [DOI] [PubMed] [Google Scholar]
- Palumbo F, Bettocchi C, Selvaggi FP, et al. Sildenafil: efficacy and safety in daily clinical experience. Eur Urol. 2001;40:176–80. doi: 10.1159/000049769. [DOI] [PubMed] [Google Scholar]
- Papaharitou S, Athanasiadis L, Nakopoulou E, et al. Erectile dysfunction and premature ejaculation are the most frequently self-reported sexual concerns: profiles of 9,536 men calling a helpline. Eur Urol. 2006;49:557–63. doi: 10.1016/j.eururo.2005.09.023. [DOI] [PubMed] [Google Scholar]
- Prieto Castro RM, Anglada Curado FJ, Regueiro Lopez JC, et al. Treatment with sildenafil citrate in renal transplant patients with erectile dysfunction. BJU Int. 2001;88:241–3. doi: 10.1046/j.1464-410x.2001.02278.x. [DOI] [PubMed] [Google Scholar]
- Raina R, Lakin MM, Agarwal A, et al. Long-term intracavernous therapy responders can potentially switch to sildenafil citrate after radical prostatectomy. Urology. 2004;63:532–7. doi: 10.1016/j.urology.2003.10.074. [DOI] [PubMed] [Google Scholar]
- Rendell MS, Rajfer J, Wicker PA, et al. Sildenafil for treatment of erectile dysfunction in men with diabetes: a randomized controlled trial. Sildenafil Diabetes Study Group. JAMA. 1999;281:421–6. doi: 10.1001/jama.281.5.421. [DOI] [PubMed] [Google Scholar]
- Rosen R, Altwein J, Boyle P, et al. Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7) Eur Urol. 2003;44:637–49. doi: 10.1016/j.eururo.2003.08.015. [DOI] [PubMed] [Google Scholar]
- Safarinejad MR. Salvage of sildenafil failures with cabergoline: a randomized, double-blind, placebo-controlled study. Int J Impot Res. 2006 doi: 10.1038/sj.ijir.3901476. [DOI] [PubMed] [Google Scholar]
- Sairam K, Kulinskaya E, McNicholas TA, et al. Sildenafil influences lower urinary tract symptoms. BJU Int. 2002;90:836–9. doi: 10.1046/j.1464-410x.2002.03040.x. [DOI] [PubMed] [Google Scholar]
- Salonia A, Maga T, Colombo R, et al. A prospective study comparing paroxetine alone versus paroxetine plus sildenafil in patients with premature ejaculation. J Urol. 2002;168:2486–9. doi: 10.1016/S0022-5347(05)64174-2. [DOI] [PubMed] [Google Scholar]
- Schwartz EJ, Wong P, Graydon RJ. Sildenafil preserves intracorporeal smooth muscle after radical retropubic prostatectomy. J Urol. 2004;171:771–4. doi: 10.1097/01.ju.0000106970.97082.61. [DOI] [PubMed] [Google Scholar]
- Seftel AD. Erectile dysfunction in the elderly: epidemiology, etiology and approaches to treatment. J Urol. 2003;169:1999–2007. doi: 10.1097/01.ju.0000067820.86347.95. [DOI] [PubMed] [Google Scholar]
- Seidman SN, Roose SP, Menza MA, et al. Treatment of erectile dysfunction in men with depressive symptoms: results of a placebo-controlled trial with sildenafil citrate. Am J Psychiatry. 2001;158:1623–30. doi: 10.1176/appi.ajp.158.10.1623. [DOI] [PubMed] [Google Scholar]
- Shabsigh R, Padma-Nathan H, Gittleman M, et al. Intracavernous alprostadil alfadex (EDEX/VIRIDAL) is effective and safe in patients with erectile dysfunction after failing sildenafil (Viagra) Urology. 2000;55:477–80. doi: 10.1016/s0090-4295(99)00612-3. [DOI] [PubMed] [Google Scholar]
- Sharma RK, Prasad N, Gupta A, et al. Treatment of erectile dysfunction with sildenafil citrate in renal allograft recipients: a randomized, double-blind, placebo-controlled, crossover trial. Am J Kidney Dis. 2006;48:128–33. doi: 10.1053/j.ajkd.2006.04.061. [DOI] [PubMed] [Google Scholar]
- Steers W, Guay AT, Leriche A, et al. Assessment of the efficacy and safety of Viagra (sildenafil citrate) in men with erectile dysfunction during long-term treatment. Int J Impot Res. 2001;13:261–7. doi: 10.1038/sj.ijir.3900714. [DOI] [PubMed] [Google Scholar]
- Stief CG, Uckert S, Becker AJ, et al. The effect of the specific phosphodiesterase (PDE) inhibitors on human and rabbit cavernous tissue in vitro and in vivo. J Urol. 1998;159:1390–3. [PubMed] [Google Scholar]
- Stuckey BG, Jadzinsky MN, Murphy LJ, et al. Sildenafil citrate for treatment of erectile dysfunction in men with type 1 diabetes: results of a randomized controlled trial. Diabetes Care. 2003;26:279–84. doi: 10.2337/diacare.26.2.279. [DOI] [PubMed] [Google Scholar]
- Takimoto E, Champion HC, Li M, et al. Chronic inhibition of cyclic GMP phosphodiesterase 5A prevents and reverses cardiac hypertrophy. Nat Med. 2005;11:214–22. doi: 10.1038/nm1175. [DOI] [PubMed] [Google Scholar]
- Vlachopoulos C, Hirata K, O’Rourke MF. Effect of sildenafil on arterial stiffness and wave reflection. Vasc Med. 2003;8:243–8. doi: 10.1191/1358863x03vm509ra. [DOI] [PubMed] [Google Scholar]
- Vlachopoulos C, Tsekoura D, Alexopoulos N, et al. Type 5 phosphodiesterase inhibition by sildenafil abrogates acute smoking-induced endothelial dysfunction. Am J Hypertens. 2004;17:1040–4. doi: 10.1016/j.amjhyper.2004.06.027. [DOI] [PubMed] [Google Scholar]
- Wagner G, Montorsi F, Auerbach S, et al. Sildenafil citrate (VIAGRA) improves erectile function in elderly patients with erectile dysfunction: a subgroup analysis. J Gerontol A Biol Sci Med Sci. 2001;56:M113–19. doi: 10.1093/gerona/56.2.m113. [DOI] [PubMed] [Google Scholar]
- Webster LJ, Michelakis ED, Davis T, et al. Use of sildenafil for safe improvement of erectile function and quality of life in men with New York Heart Association classes II and III congestive heart failure: a prospective, placebo-controlled, double-blind crossover trial. Arch Intern Med. 2004;164:514–20. doi: 10.1001/archinte.164.5.514. [DOI] [PubMed] [Google Scholar]
- Wespes E, Amar E, Hatzichristou D, et al. EAU Guidelines on erectile dysfunction: an update. Eur Urol. 2006;49:806–15. doi: 10.1016/j.eururo.2006.01.028. [DOI] [PubMed] [Google Scholar]
- Young JM, Bennett C, Gilhooly P, et al. Efficacy and safety of sildenafil citrate (Viagra) in black and Hispanic American men. Urology. 2002;60:39–48. doi: 10.1016/s0090-4295(02)01689-8. [DOI] [PubMed] [Google Scholar]
- Zippe CD, Kedia AW, Kedia K, et al. Treatment of erectile dysfunction after radical prostatectomy with sildenafil citrate (Viagra) Urology. 1998;52:963–6. doi: 10.1016/s0090-4295(98)00443-9. [DOI] [PubMed] [Google Scholar]