Abstract
OBJECTIVE
To assess whether abdominal adiposity in early pregnancy is associated with a higher risk of glucose intolerance at a later gestational stage.
RESEARCH DESIGN AND METHODS
Subcutaneous and visceral fat was measured with ultrasonography at ∼12 weeks' gestation. A 50-g glucose challenge test (GCT) was performed between 24 and 28 weeks' gestation. The risk of having a positive GCT (≥7.8 mmol/l) was determined in association with subcutaneous and visceral adipose tissue depths above their respective upper-quartile values relative to their bottom three quartile values.
RESULTS
Sixty-two women underwent GCTs. A visceral adipose tissue depth above the upper quartile value was significantly associated with a positive GCT in later pregnancy (adjusted odds ratio 16.9 [95% CI 1.5–194.6]). No associations were seen for subcutaneous adipose tissue.
CONCLUSIONS
Measurement of visceral adipose tissue depth in early pregnancy may be associated with glucose intolerance later in pregnancy.
Maternal obesity is associated with a higher risk of gestational diabetes mellitus (GDM) (1) and adverse perinatal outcomes (2,3). Visceral adiposity (4) may better predict the onset of type 2 diabetes, independent of BMI. Given that GDM and type 2 diabetes share the same risk factors (1) and GDM predates the onset of type 2 diabetes (5), it is logical to question whether high maternal visceral adiposity is associated with GDM.
We determined the reliability of first-trimester ultrasonography for measuring subcutaneous and visceral adipose tissue in pregnancy and whether either is predictive of a positive glucose challenge test (GCT), which is commonly used to screen for GDM later in pregnancy.
RESEARCH DESIGN AND METHODS
We completed a prospective cohort study at a single outpatient ultrasound clinic at St. Michael's Hospital in Toronto, Ontario, Canada, between January and May 2008. Women with a singleton pregnancy were eligible for the study at 11–14 weeks' gestation. Women with type 1 or type 2 diabetes prior to pregnancy or with a previous history of GDM were excluded. Written and informed consent was obtained, and the study was approved by the hospital research ethics board.
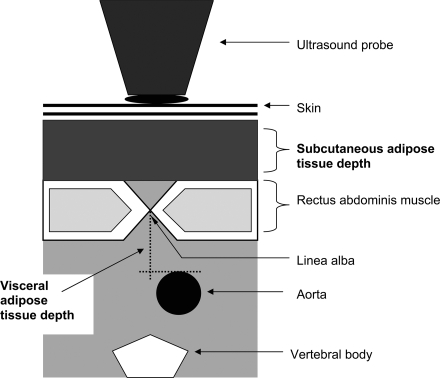
We used the technique of Armellini et al. (6) to measure subcutaneous and visceral abdominal adipose tissue. A total of 62 patients were scanned on a Philips iU22 ultrasound machine using a 5-2 or 9 MHz probe. Subcutaneous fat depth was measured from the subcutaneous fat layer to the outer border of the rectus abdominus muscle at the level of the linea alba (Fig. 1). Visceral fat depth was measured from the inner border of the rectus abdominus muscle at the level of the linea alba to the anterior wall of the abdominal aorta.
Figure 1.
Cross-sectional representation of the abdominal wall and subcutaneous and visceral fat compartments measured by ultrasound.
Two sonographers—one a perinatal obstetrician and the other an experienced ultrasound technologist—each performed three measurements of the subcutaneous and visceral fat depths. Each rater was masked to the other's assessment, and the measurements were recorded on separate data collection sheets.
Intrarater reliability of ultrasonography was determined for each rater using three images of subcutaneous and three images of visceral adipose tissue depth per participant, respectively. Interobserver reliability was separately calculated for subcutaneous and visceral adiposity.
Mean subcutaneous and visceral adipose tissue depths were determined for each participant, with the measures of both sonographers pooled. The upper-quartile value for each was considered elevated, and the three lowest quartile values were treated as the referent. All participants underwent a 50-g GCT at 24–28 weeks' gestation. An abnormal 50-g GCT was defined at a conventional cut point: ≥7.8 mmol/l. Unadjusted and adjusted ORs and 95% CIs expressed the risk of an abnormal GCT in association with an elevated subcutaneous and an elevated visceral adipose tissue depth, respectively.
All P values were two-sided, and significance was set at a value of 0.05. Statistical analyses were performed using SAS (version 9; SAS Institute, Cary, NC).
RESULTS
There were 62 women recruited in total at mean ± SD gestation 12.4 ± 0.60 weeks and age 31.7 ± 5.0 years. The median gravidity was 2.0, and 31 (50.0%) were of nonwhite ethnicity. Mean prepregnancy BMI was 23.9 ± 5.2 kg/m2. Mean subcutaneous and visceral adiposity tissue depths by ultrasonography were 1.8 ± 0.72 cm (range 0.63–3.7) and 4.0 ± 1.4 cm (1.3–8.2), respectively. The 50-g GCT was completed at 27.4 ± 1.4 weeks' gestation.
Reliability measures were based on all 62 women. The intraclass correlation coefficient for intraobserver agreement of visceral adiposity tissue measurement was 0.94 (95% CI 0.91–0.96) for the physician and 0.97 (0.95–0.98) for the technologist. Similar results were seen for subcutaneous adiposity measurement. Lin's concordance correlation coefficient for interobserver reliability (between physician vs. technologist) was 0.79 (0.69–0.88) for subcutaneous adiposity and 0.87 (0.82–0.93) for visceral adiposity.
Fifty-eight women formed the sample used to analyze the relationship between adiposity and subsequent GCT positivity. No significant associations were observed between the upper-quartile subcutaneous adipose tissue depth and a positive GCT (Table 1). However, an elevated visceral adipose tissue depth was significantly associated with a positive GCT (unadjusted OR 17.3 [95% CI 1.8–163.8]). Even after adjusting for maternal age and prepregnancy BMI, the association remained significant (16.9 [1.5–194.6]).
Table 1.
Elevated subcutaneous and visceral abdominal adipose tissue in the first trimester of pregnancy and associated risk of an elevated glucose challenge test in the second trimester of pregnancy
| Abdominal ultrasound measurement of adipose tissue depth | n | Abnormal glucose challenge test: ≥7.8 mmol/l (n = 6) |
||
|---|---|---|---|---|
| n (%) | Unadjusted OR (95% CI) | Adjusted OR (95% CI)* | ||
| Subcutaneous adipose tissue | ||||
| Bottom three quartiles: <2.18 cm | 42 | 3 (7.1) | 1.0 (ref.) | 1.0 (ref.) |
| Upper quartile: ≥2.18 cm | 16 | 3 (18.8) | 3.1 (0.55–17.4) | 1.7 (0.18–16.5) |
| Visceral adipose tissue | ||||
| Bottom three quartiles: <4.74 cm | 42 | 1 (2.4) | 1.0 (ref.) | 1.0 (ref.) |
| Upper quartile: ≥4.74 cm | 16 | 5 (31.2) | 17.3 (1.8–163.8) | 16.9 (1.5–194.6) |
Complete data are presented for 58 participants.
*Adjusted for maternal age in years (continuous) and prepregnancy BMI in kg/m2 (continuous).
CONCLUSIONS
Since we included only 62 women, our risk estimates were imprecise. We used a 50-g GCT as an indicator of glucose intolerance later in pregnancy rather than a more definitive 2-h 75-g oral glucose tolerance test. However, a positive GCT is a reasonable predictor of GDM-related adverse perinatal outcomes (7). A strength of this cohort study is that we prospectively assessed abdominal adiposity at around the same gestational age using a standardized protocol. All sonographers were masked to each other's measurements, and the GCTs were carried out without knowledge of the abdominal depths.
Visceral adiposity predicts insulin resistance (8) and diabetes (4) independent of BMI, so it was logical for us to use ultrasonography to measure visceral fat in relation to glucose intolerance in pregnancy. When used in nonpregnant patients, ultrasound has a correlation coefficient of between 0.55 (9) and 0.81 (10) and a diagnostic concordance of 74% with computed tomography (9) in the assessment of visceral adiposity.
Maternal obesity, routinely defined as an elevated prepregnancy BMI, is associated with adverse pregnancy outcomes (1–3,11). BMI may not accurately differentiate between the contributions of muscle and fat to body weight or of subcutaneous versus visceral abdominal fat. Epidemiological and metabolic studies have found that the adverse metabolic consequences of excess fat depend largely on the location of the fat (12,13), with centrally located visceral fat more pathogenic than subcutaneous adipose tissue (14). Our results are consistent with this concept.
Measurement of visceral adiposity during a routine 11–14 weeks' gestation ultrasound might improve the performance of screening for GDM (15). Moreover, identifying women at high risk for GDM because of elevated visceral adiposity could lead to either earlier screening or earlier dietary and lifestyle modifications. Clearly, this opens up a new avenue for research.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Solomon CG, Willett WC, Carey VJ, Rich-Edwards J, Hunter DJ, Colditz GA, Stampfer MJ, Speizer FE, Spiegelman D, Manson JE. A prospective study of pregravid determinants of gestational diabetes mellitus. JAMA 1997; 278: 1078– 1083 [PubMed] [Google Scholar]
- 2. Ehrenberg HM, Mercer BM, Catalano PM. The influence of obesity and diabetes on the prevalence of macrosomia. Am J Obstet Gynecol 2004; 191: 964– 968 [DOI] [PubMed] [Google Scholar]
- 3. Surkan PJ, Hsieh CC, Johansson AL, Dickman PW, Cnattingius S. Reasons for increasing trends in large for gestational age births. Obstet Gynecol 2004; 104: 720– 726 [DOI] [PubMed] [Google Scholar]
- 4. Bray GA, Jablonski KA, Fujimoto WY, Barrett-Connor E, Haffner S, Hanson RL, Hill JO, Hubbard V, Kriska A, Stamm E, Pi-Sunyer FX. the Diabetes Prevention Program Research Group. Relation of central adiposity and body mass index to the development of diabetes in the Diabetes Prevention Program. Am J Clin Nutr 2008; 87: 1212– 1218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Feig DS, Zinman B, Wang X, Hux JE. Risk of development of diabetes mellitus after diagnosis of gestational diabetes. CMAJ 2008; 179: 229– 234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Armellini F, Zamboni M, Rigo L, Todesco T, Bergamo-Andreis IA, Procacci C, Bosello O. The contribution of sonography to the measurement of intra-abdominal fat. J Clin Ultrasound 1990; 18: 563– 567 [DOI] [PubMed] [Google Scholar]
- 7. Stamilio DM, Olsen T, Ratcliffe S, Sehdev HM, Macones GA. False-positive 1-hour glucose challenge test and adverse perinatal outcomes. Obstet Gynecol 2004; 103: 148– 156 [DOI] [PubMed] [Google Scholar]
- 8. Pascot A, Després JP, Lemieux I, Alméras N, Bergeron J, Nadeau A, Prud'homme D, Tremblay A, Lemieux S. Deterioration of the metabolic risk profile in women: respective contributions of impaired glucose tolerance and visceral fat accumulation. Diabetes Care 2001; 24: 902– 908 [DOI] [PubMed] [Google Scholar]
- 9. Ribeiro-Filho FF, Faria AN, Azjen S, Zanella MT, Ferreira SR. Methods of estimation of visceral fat: advantages of ultrasonography. Obes Res 2003; 11: 1488– 1494 [DOI] [PubMed] [Google Scholar]
- 10. Stolk RP, Wink O, Zelissen PM, Meijer R, van Gils AP, Grobbee DE. Validity and reproducibility of ultrasonography for the measurement of intra-abdominal adipose tissue. Int J Obes Relat Metab Disord 2001; 25: 1346– 1351 [DOI] [PubMed] [Google Scholar]
- 11. O'Brien TE, Ray JG, Chan WS. Maternal body mass index and the risk of preeclampsia: a systematic overview. Epidemiology 2003; 14: 368– 374 [DOI] [PubMed] [Google Scholar]
- 12. Pi-Sunyer FX. The epidemiology of central fat distribution in relation to disease. Nutr Rev 2004; 62: S120– S126 [DOI] [PubMed] [Google Scholar]
- 13. Després JP, Lemieux I, Prud'homme D. Treatment of obesity: need to focus on high risk abdominally obese patients. BMJ 2001; 322: 716– 720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Carey DG, Jenkins AB, Campbell LV, Freund J, Chisholm DJ. Abdominal fat and insulin resistance in normal and overweight women: direct measurements reveal a strong relationship in subjects at both low and high risk of NIDDM. Diabetes 1996; 45: 633– 638 [DOI] [PubMed] [Google Scholar]
- 15. Metzger BE, Buchanan TA, Coustan DR, de Leiva A, Dunger DB, Hadden DR, Hod M, Kitzmiller JL, Kjos SL, Oats JN, Pettitt DJ, Sacks DA, Zoupas C. Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes Care 2007; 30 ( Suppl. 1): S251– S260 [DOI] [PubMed] [Google Scholar]