Abstract
Objective
To estimate the impact of a soft cap (a ceiling on utilization beyond which insured enrollees pay a higher copayment) on low-income elders' use of prescription drugs.
Data Sources and Setting
Claims and enrollment files for the first year (June 2002 through May 2003) of the Illinois SeniorCare program, a state pharmacy assistance program, and Medicare claims and enrollment files, 2001 through 2003. SeniorCare enrolled non-Medicaid-eligible elders with income less than 200 percent of Federal Poverty Level. Minimal copays increased by 20 percent of prescription cost when enrollee expenditures reached $1,750.
Research Design
Models were estimated for three dependent variables: enrollees' average monthly utilization (number of prescriptions), spending, and the proportion of drugs that were generic rather than brand. Observations included all program enrollees who exceeded the cap and covered two periods, before and after the cap was exceeded.
Principle Findings
On average, enrollees exceeding the cap reduced the number of drugs they purchased by 14 percent, monthly expenditures decreased by 19 percent, and the proportion generic increased by 4 percent, all significant at p<.01. Impacts were greater for enrollees with greater initial spending, for enrollees without one of five chronic illness diagnoses in the previous calendar year, and for enrollees with lower income.
Conclusions
Near-poor elders enrolled in plans with caps or coverage gaps, including Part D plans, may face sharp declines in utilization when they exceed these thresholds.
Keywords: Prescription drugs, copayments, elasticity of demand, low-income elderly
A spending cap is an insurance design feature that changes out-of-pocket prices faced by the insured after she exceeds a spending limit. Often the cap is a coverage limit, so that plan enrollees must pay full price after their spending has reached a specified level. Studies examining the effects of exceeding prescription drug spending caps on utilization and health have found that exceeding a cap results in greater out-of-pocket costs and self-reported financial burden (Tseng et al. 2003, 2004), reduction in drug utilization (Soumerai et al. 1991; Martin and McMillan 1996; Hsu et al. 2006, 2008; Joyce et al. 2007), and higher use of emergency room, hospital, and nursing home services (Soumerai et al. 1991; Hsu et al. 2006).
Survey responses from enrollees provide most of what is known about the impact of exceeding a spending cap on enrollee prescription drug use. Prior studies have seldom been able to examine the prescription drug utilization of the same individuals before and after they reach an expenditure cap. When insurers pay nothing above an expenditure cap, enrollees are less likely to file claims for drugs purchased after the cap is exceeded.1 Thus, several previous cap studies have not observed actual levels of utilization and out-of-pocket costs after a cap was exceeded but instead have extrapolated past spending to estimate burden on beneficiaries (Tseng et al. 2003, 2004).2 An exception is a study of cost sharing of Medicare+Choice beneficiaries enrolled in a large prepaid integrated delivery system (Hsu et al. 2006). Hsu and colleagues found significantly lower drug utilization and greater nonadherence for beneficiaries subject to a spending cap in comparison with similar enrollees in a plan with no limit; to allay concern that postcap drug use might not be observed, they cite a concurrent survey of their study population reporting that beneficiaries did not buy drugs out of plan even after consumers faced the full drug price.3
For this study, we were able to observe the monthly prescription drug utilization of enrollees in a state pharmacy assistance plan with a soft cap that required enrollees to pay higher copayments (but less than full price) after they incurred total spending (both state coverage and out of pocket) greater than a threshold amount. This allowed us to address the following research questions:
Do enrollees reduce prescription drug utilization and expenses when they face higher copayments after exceeding a soft cap?
Do enrollees increase the proportion of drugs that are generic, as opposed to brand name, when they face higher copayments after exceeding a soft cap?
THE ILLINOIS PHARMACY ASSISTANCE PLAN
Before the implementation of Medicare Part D coverage for prescription drugs, a number of states funded pharmacy assistance programs for low-income seniors not eligible for Medicaid (Safran et al. 2002). Beginning in 2001, states were allowed to seek federal cost sharing through Medicaid 1115 waivers for such programs. In 2002, Illinois was among the first states to obtain a waiver to gain the federal Medicaid match for prescription drugs provided under the program to persons aged 65 and older with incomes up to 200 percent of the Federal Poverty Level (FPL) who do not qualify for Medicaid. Its program, called SeniorCare, was launched in June 2002. At the beginning of the program year, the plan charged most enrollees a copayment of $4 for each brand prescription filled and $1 per generic prescription. However, if the total prescription drug expenditures for an enrollee reached $1,750, copayments increased to 20 percent of drug cost, plus the original $1 or $4.4
METHODS AND DATA
Econometric Specification
Our objectives were to estimate the effect of exceeding the soft cap on prescription drug utilization, measured as the number of prescriptions filled, and to assess effects on total drug spending and the mix of brand and generic drugs. Using individual data observed before and after the cap was exceeded, our econometric approach accounted for unobserved individual heterogeneity while avoiding bias that can arise in panel specifications when an independent variable (exceeding the cap) is a function of lagged values of the dependent variable (use, spending, or proportion generic use) (Bond, 2002).
We estimated models for each of the dependent variables (monthly number of prescriptions, spending, and proportion of prescriptions that were for generic rather than brand-name drugs) among only those beneficiaries who exceeded the cap. The observations were aggregated into two periods for each beneficiary: the average for the months before and for the months after the cap was exceeded. This averaging smoothed out monthly fluctuations, increasing the stability of the observations. This approach also precluded the cap indicator from varying between individuals on the time dimension, which would give rise to endogeneity.
The month that the cap was exceeded was identified by determining whether the cumulative drug claims paid by the program and the beneficiary through each month exceeded $1,750. Because enrollees face first precap and then postcap out-of-pocket prices in the month they exceed the cap, this month was excluded from the analysis. We also excluded a 1-month adjustment period after the cap was exceeded. We classified the study group of cap exceeders by their precap monthly drug expenditures to investigate systematic differences in effects of the soft cap over types of cap exceeders.
The following equation was estimated for each of the three dependent variables (drug use, spending, and proportion generic):
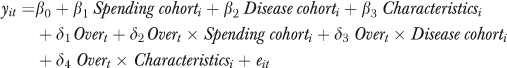 |
(1) |
where Spending cohorti is a vector of three indicator variables for spending quartiles based on precap drug spending, Disease cohorti is a vector of dummy variables for five chronic conditions (diabetes, coronary artery disease, cerebrovascular disease, chronic obstructive pulmonary disease [COPD], and arthritis), Characteristicsi are sociodemographic indicators for age, race, sex, and income, Overt is a period indicator corresponding to the postcap period, and eit is an error term. The cap impact is estimated by the coefficient δ1 for the postcap indicator Overt, and impacts for various subgroups are captured by the coefficients for the interactions terms δ2 and δ3.
Standard regression models were estimated because models accounting for unobserved effects, such as fixed or random effects models, yield identical parameter estimates in this two-period case. The models for use and expenditures were estimated in logs and levels to test whether the relationships between dependent and independent variables were linear or proportional (Wooldridge 1994). To model the proportion generic, we used a generalized linear model (GLM) with a logit link function to account for the bounding of the proportion between 0 and 1.
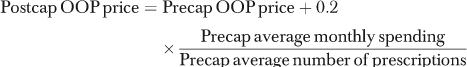
Before computation of the pre- and postcap period monthly means, the data were purged of seasonal and trend effects. Monthly prescription drug use, spending, and generic use rates generally grew over time for all SeniorCare beneficiaries. These patterns were likely the result of a combination of seasonal effects, increasing familiarity with the SeniorCare program, and the aging of beneficiaries. If left unaccounted for, these trends could result in a downward bias in the estimate of the effect of the cap on utilization behavior because the cap was typically exceeded later in the program year at a time when, in the absence of a cap effect, greater utilization would be expected. To adjust for secular trends in utilization patterns, monthly means were calculated for each of the dependent variables among beneficiaries who did not exceed the cap during the program year and who were enrolled for the entire 12-month observation period. The first program month (June 2002) was set as the reference month, and for a given cap exceeder in month t, adjusted monthly utilization behavior (spending in the following example) was calculated as
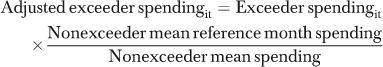 |
(2) |
After adjustment, pre- and postcap means were calculated for each beneficiary for each of the dependent variables.5,6
Semielasticity estimates, estimated percentage changes in the dependent variable associated with exceeding the cap, were calculated by dividing the marginal effect of the cap for beneficiaries with a given characteristic by the precap level of the dependent variable for that cohort. Marginal effects for the GLM specifications were calculated using the methods described by Ai and Norton (2003) for nonlinear models. To estimate the price elasticity of demand, the average precap out-of-pocket price per prescription and the price that enrollees would have paid for the same drugs postcap were computed for the full study group and each subgroup as follows:
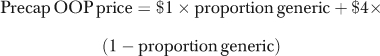 |
(3) |
 |
(4) |
Price elasticity of demand was then estimated by dividing the estimated percent change in number of prescriptions, based on the cap effect estimated in (1), by the estimated percentage change in beneficiaries' out-of-pocket price for prescription drugs, basing the percentage at the midpoint of the pre- and postcap quantities and prices (arc elasticity).7
Data
Prescription drug claims provided by the Illinois Department of Public Aid, allowed computation of number of prescriptions, drug spending, and proportion prescriptions that were generic rather than brand for individual enrollees. A total of 41,914 SeniorCare beneficiaries, 32.8 percent of all beneficiaries observed during the first program year, had total drug spending >$1,750, indicating that they exceeded the cap. Beneficiaries were excluded from the analysis if they did not have at least 1 month of enrollment before the cap month, and/or 1 month of nonzero spending after the adjustment period, or if they were not in fee-for-service Medicare throughout 2001, the reference year for capturing diagnostic information. After these exclusions, the analytic sample numbered 33,397; enrollees with no or 100 percent generic use in either the pre- or the postcap period were omitted from the analysis of generic utilization because the logistic is undefined for these values, resulting in an analytic sample of 32,722 for this analysis.
Prescription drug data for the seventh program month, December 2002, were incomplete. Spending for this month was imputed using data from the adjoining months (November 2002 and January 2003) to support our estimates of whether and when the spending cap was exceeded; but this month's data were excluded from the calculation of the pre- and postcap means.
Demographic characteristics were available from Medicare eligibility files and the presence of five specific chronic illness diagnoses was determined using the beneficiary's previous year's Medicare claims. Income was reported on SeniorCare enrollment forms. Additional details of the data development are presented in supporting information Appendix SA2, which is available online. Data were analyzed using SAS version 9.3 and Stata version 10.0.
RESULTS
Table 1 shows the pre- and postcap monthly use, spending, and proportion generic for all cap exceeders, and it reports chronic disease and demographic characteristics by spending cohort. Before exceeding the cap, enrollees in SeniorCare who exceeded the cap filled on average 5.9 prescriptions per month, of which 40 percent were generic, with average adjusted prescription drug spending of $268 per month; after exceeding the cap, use fell to 5 prescriptions per month, percent generic rose to 42 percent, and the adjusted spending fell to $217 (Table 1). SeniorCare cap exceeders with higher precap use and spending had a greater prevalence of chronic disease than cap exceeders in the lower spending quartiles but were otherwise similar in observable characteristics.
Table 1.
Analytic Sample† Characteristics
| All Cap Exceeders in Analytic Sample | Lowest Quartile Precap Spending | Second Quartile Precap Spending | Third Quartile Precap Spending | Highest Quartile Precap Spending | |
|---|---|---|---|---|---|
| N | 33,397 | 8,350 | 8,349 | 8,348 | 8,350 |
| Adjusted monthly prescription drug utilization (mean number of prescriptions) | |||||
| Precap* | 5.88 | 4.30 | 5.05 | 6.00 | 8.16 |
| Postcap* | 5.04 | 4.05 | 4.48 | 5.18 | 6.43 |
| Adjusted monthly prescription drug spending (mean) | |||||
| Precap* | $268.12 | $168.57 | $211.99 | $270.36 | $421.57 |
| Postcap* | $217.47 | $160.20 | $179.86 | $221.87 | $307.95 |
| Adjusted generic drug utilization proportion (mean) | |||||
| Precap* | 0.400 | 0.422 | 0.407 | 0.394 | 0.379 |
| Postcap* | 0.417 | 0.432 | 0.422 | 0.413 | 0.403 |
| Month in which cap was exceeded (%) | |||||
| Months 2–4 | 9.0 | — | — | — | — |
| Months 5–7 | 42.5 | — | — | — | — |
| Months 8–10 | 48.4 | — | — | — | — |
| Chronic disease diagnosis (%) | |||||
| Diabetes* | 37.4 | 29.2 | 33.4 | 38.8 | 48.4 |
| Coronary heart disease* | 48.1 | 41.1 | 45.7 | 49.4 | 56.0 |
| Cerebrovascular disease* | 18.9 | 15.8 | 16.8 | 18.9 | 23.9 |
| COPD* | 25.9 | 21.9 | 23.6 | 26.0 | 32.1 |
| Arthritis* | 36.1 | 33.2 | 34.5 | 36.6 | 40.1 |
| Age (mean)* | 78.8 | 79.0 | 79.0 | 78.8 | 78.6 |
| Race (%) | |||||
| White | 82.5 | 81.7 | 82.7 | 82.8 | 82.6 |
| Black | 13.1 | 13.7 | 12.9 | 13.1 | 12.8 |
| Other | 4.4 | 4.7 | 4.4 | 4.1 | 4.6 |
| Urban (%) | 63.6 | 63.2 | 62.9 | 63.6 | 64.6 |
| Married (%)* | 21.6 | 22.6 | 22.4 | 20.7 | 20.8 |
| Poverty status (%) | |||||
| <100% FPL | 12.7 | 12.6 | 12.8 | 13.1 | 12.3 |
| 100–134% FPL | 28.8 | 29.3 | 28.7 | 29.3 | 27.8 |
| 135–149% FPL | 15.6 | 15.2 | 15.4 | 15.6 | 16.2 |
| 150%+FPL | 42.9 | 42.9 | 43.1 | 42.0 | 43.7 |
p<.01
Analytic sample excludes enrollees without one month of observed use before exceeding the cap and after the adjustment period; it excludes enrollees who exceeded the cap in months 1, 11, and 12. It also excludes Medicare beneficiaries younger than 67, who did not have Medicare claims data needed to determine chronic disease diagnosis.
Tests of difference in proportions and means across spending quartiles are performed with Wald's test.
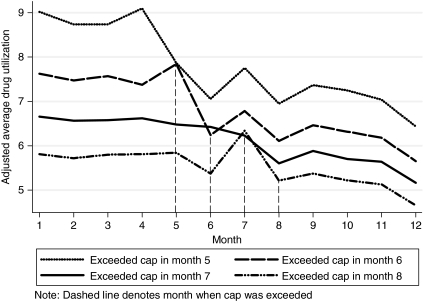
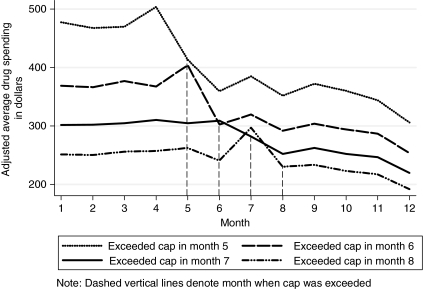
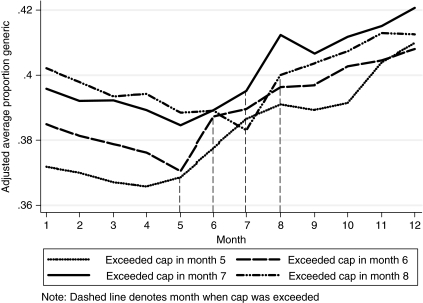
Figures 1, 2, and 3 show adjusted average monthly number of prescriptions, spending, and proportion generic use for cohorts of 12-month enrollees who exceeded the soft cap in program months 4, 5, 6, and 7.8 Figures 1 and 2 show that, for each of the selected cohorts, prescription drug use and spending spiked in the month preceding higher cost sharing, fell sharply the following month when the cap was exceeded and full cost sharing was required, and declined slowly for the remainder of the year. Figure 3 shows that the proportion generic increased steadily after the cap was exceeded.
Figure 1.
Adjusted Prescription Drug Use (Number of Prescriptions) for Selected Cohorts, 12-Month Enrollees
Figure 2.
Adjusted Prescription Drug Spending for Selected Cohorts, 12-Month Enrollees
Figure 3.
Adjusted Generic Drug Use Rates for Selected Cohorts, 12-Month Enrollees
Table 2 presents the estimated impact of exceeding the cap overall and for the cohort identifiers used in the multivariate analysis. The Wooldridge test of functional form showed that the linear specification for the use and expenditure models was preferred to the logarithmic functional form. Consequently, utilization and spending were modeled in levels. The cap impact for each cohort was estimated at the sample means of other model variables. For each cohort, exceeding the cap resulted in decreases in the number and value of prescriptions filled and increases in proportion generic, all significant at p<.01.
Table 2.
Effect of Exceeding Spending Cap on Monthly Drug Spending, Number of Prescriptions, and Percentage Generic Utilization by Cohort (Standard Errors in Parentheses)
| Number of Prescriptions |
Spending |
Proportion Generic |
|||||
|---|---|---|---|---|---|---|---|
| Cohort Descriptors | Marginal Effect of Cap | Percent Change | Price Elasticity of Demand | Marginal Effect of Cap | Percent Change | Marginal Effect of Cap | Percent Change |
| Overall | −0.84 | −14.28 | −0.12 | −$50.65 | −18.89 | 0.017 | 4.19 |
| (0.01) | (0.18) | ($0.57) | (0.21) | (0.001) | (0.21) | ||
| First month spending | |||||||
| Lowest quartile | −0.26 | −6.00 | −0.05 | −$7.96 | −4.72 | 0.008 | 1.86 |
| (0.02) | (0.50) | ($1.12) | (0.66) | (0.002) | (0.51) | ||
| Second quartile*,†,‡ | −0.57 | −11.37 | −0.10 | −$31.98 | −15.07 | 0.015 | 3.71 |
| (0.02) | (0.36) | ($0.89) | (0.42) | (0.002) | (0.42) | ||
| Third quartile*,†,‡ | −0.81 | −13.57 | −0.12 | −$48.52 | −17.92 | 0.020 | 5.02 |
| (0.02) | (0.31) | ($0.96) | (0.36) | (0.001) | (0.38) | ||
| Highest quartile*,†,‡ | −1.71 | −20.94 | −0.18 | −$114.16 | −27.04 | 0.024 | 6.33 |
| (0.02) | (0.31) | ($1.51) | (0.36) | (0.001) | (0.38) | ||
| Chronic disease cohort | |||||||
| Did not have one of 5 chronic disease diagnoses in 2001 | −0.76 | −15.34 | −0.13 | −$53.45 | −22.17 | 0.019 | 4.99 |
| (0.02) | (0.37) | ($1.02) | (0.43) | (0.002) | (0.42) | ||
| Diabetes†,‡ | −0.81 | −12.44 | −0.11 | −$51.84 | −17.89 | 0.015 | 3.69 |
| (0.02) | (0.34) | ($1.18) | (0.41) | (0.002) | (0.43) | ||
| Coronary heart disease*,† | −0.81 | −12.63 | −0.11 | −$49.33 | −17.58 | 0.019 | 4.44 |
| (0.02) | (0.34) | ($1.20) | (0.43) | (0.002) | (0.42) | ||
| Cerebrovascular disease | −0.76 | −12.13 | −0.10 | −$51.98 | −18.10 | 0.019 | 4.84 |
| (0.03) | (0.50) | ($1.72) | (0.60) | (0.002) | (0.60) | ||
| COPD† | −0.91 | −14.20 | −0.12 | −$55.68 | −19.53 | 0.020 | 4.68 |
| (0.03) | (0.42) | ($1.46) | (0.51) | (0.002) | (0.53) | ||
| Arthritis | −0.74 | −12.11 | −0.10 | −$52.01 | −18.74 | 0.016 | 3.86 |
| (0.02) | (0.37) | ($1.27) | (0.46) | (0.002) | (0.46) | ||
| Sociodemographic characteristics | |||||||
| Male | −0.83 | −14.77 | −0.13 | −$52.59 | −19.82 | 0.018 | 4.43 |
| (0.03) | (0.51) | ($1.64) | (0.62) | (0.002) | (0.58) | ||
| Female | −0.84 | −14.19 | −0.12 | −$50.27 | −18.71 | 0.016 | 4.14 |
| (0.01) | (0.20) | ($0.62) | (0.23) | (0.001) | (0.24) | ||
| Race black | −0.84 | −14.55 | −0.13 | −$51.00 | −19.27 | 0.017 | 4.17 |
| (0.03) | (0.53) | ($1.65) | (0.62) | (0.002) | (0.60) | ||
| Race white | −0.84 | −14.27 | −0.12 | −$50.76 | −18.88 | 0.017 | 4.21 |
| (0.01) | (0.19) | ($0.63) | (0.23) | (0.001) | (0.24) | ||
| Other race | −0.77 | −13.55 | −0.12 | −$47.62 | −17.89 | 0.015 | 3.90 |
| (0.05) | (0.89) | ($2.72) | (1.02) | (0.004) | (1.05) | ||
| Married | −0.85 | −14.80 | −0.13 | −$51.91 | −19.59 | 0.018 | 4.55 |
| (0.02) | (0.42) | ($1.34) | (0.51) | (0.002) | (0.52) | ||
| Unmarried | −0.84 | −14.14 | −0.12 | −$50.31 | −18.70 | 0.016 | 4.09 |
| (0.01) | (0.21) | ($0.68) | (0.25) | (0.001) | (0.25) | ||
| Rural | −0.89 | −14.81 | −0.13 | −$51.31 | −19.25 | 0.017 | 4.26 |
| (0.02) | (0.30) | ($0.96) | (0.36) | (0.001) | (0.34) | ||
| Urban† | −0.81 | −13.96 | −0.12 | −$50.28 | −18.68 | 0.016 | 4.14 |
| (0.01) | (0.23) | ($0.72) | (0.27) | (0.001) | (0.28) | ||
| 64<age<75 | −0.85 | −14.51 | −0.12 | −$52.69 | −19.34 | 0.018 | 4.67 |
| (0.02) | (0.31) | ($1.04) | (0.38) | (0.002) | (0.39) | ||
| 74<age<84* | −0.83 | −14.16 | −0.12 | −$49.95 | −18.69 | 0.016 | 3.88 |
| (0.01) | (0.25) | ($0.79) | (0.30) | (0.001) | (0.30) | ||
| Age 85+* | −0.85 | −14.16 | −0.12 | −$48.48 | −18.53 | 0.017 | 4.11 |
| (0.03) | (0.48) | ($1.41) | (0.54) | (0.002) | (0.51) | ||
| 150%+FPL | −0.79 | −13.49 | −0.12 | −$47.35 | −17.61 | 0.017 | 4.39 |
| (0.02) | (0.28) | ($0.89) | (0.33) | (0.001) | (0.33) | ||
| 135–149% FPL* | −0.82 | −13.92 | −0.12 | −$51.31 | −18.96 | 0.016 | 4.09 |
| (0.03) | (0.44) | ($1.38) | (0.51) | (0.002) | (0.53) | ||
| 100–134% FPL*,† | −0.88 | −14.95 | −0.13 | −$53.07 | −20.01 | 0.015 | 3.80 |
| (0.02) | (0.34) | ($1.04) | (0.39) | (0.002) | (0.40) | ||
| Less than 100% FPL*,† | −0.94 | −15.84 | −0.14 | −$55.58 | −20.65 | 0.018 | 4.52 |
| (0.03) | (0.53) | ($1.77) | (0.66) | (0.002) | (0.59) | ||
| N | 33,397 | 33,397 | 32,722 | ||||
| R2 | 0.325 | 0.490 | — | ||||
p<.05 for tests of equivalence of marginal effects for expenditure between a given cohort and the reference cohort (denoted by italics).
p<.05 for tests of equivalence of marginal effects for utilization between a given cohort and the reference cohort.
p<.05 for tests of equivalence of marginal effects for % generic between a given cohort and the reference cohort.
Notes: Heteroskedasticity robust standard errors shown in parentheses.
All effects are significant at p<.05.
“Overall” effects are calculated at the mean of chronic disease prevalence, spending categories, and sociodemographic factors.
Effects for spending categories are calculated at the mean of rates of chronic disease prevalence and sociodemographic factors.
Effects for chronic disease categories are calculated assuming no other chronic diseases, at the mean of spending categories, and at the mean of sociodemographic factors.
Effects for sociodemographic factors are calculated at the mean of rates of chronic disease prevalence and spending categories.
Substantial variation in the effect of the cap was observed across spending cohorts. The lowest quartile of precap spenders reduced the number of prescriptions filled by 0.3 on average, while the highest quartile of spenders reduced the number of prescriptions filled by 1.7; prescription drug spending fell by $8 for those with low precap spending and by $114 for those with high precap spending. The computed price (arc) elasticity of demand was −0.12 for the full group, indicating inelastic demand for prescription drugs; utilization was much more responsive to price for those with high initial spending than for those with lower spending. Also, while exceeding the cap resulted in a 1.9 percent increase in the proportion generic for the lowest spending quartile, the effect was a 6.3 percent increase for the highest spending quartile.
The effects of the cap on beneficiaries with specific chronic diseases were generally similar to the effects of the cap on all enrollees. While those who did not exhibit one of the study diagnoses in the previous calendar year experienced significantly greater percentage reductions in use (relative to diabetes, coronary heart disease, and COPD) and spending (relative to coronary heart disease) and significantly greater increases in generic utilization (relative to diabetes), these differences were typically small. Enrollees in the lower income categories exhibited a larger price elasticity of demand, consistent with the significantly greater reduction in use (and spending), than those with incomes above 150 percent of FPL. Also of interest, urban enrollees decreased utilization significantly less than rural enrollees when they hit the cap, and older enrollees reduced their spending significantly less than younger enrollees, but again differences were small.
DISCUSSION
The econometric analysis of monthly prescription and expenditure data for enrollees in a state pharmacy assistance program indicates that near-poor elders responded to an increase in out-of-pocket price by significantly reducing the number of prescriptions they filled. This was accompanied by significantly lower monthly drug expenditures (sum of program and out-of-pocket spending). The percentage decrease in total spending was greater than the percentage decrease in number of prescriptions, suggesting that elders were continuing to meet some prescription needs by shifting to lower-cost medicines. This observation is reinforced by the finding that the proportion of prescriptions that were generic rather than brand increased significantly. It is also noteworthy that these effects were greatest for enrollees in the highest quartile for precap drug spending. On average, these high spenders reduced the number of prescriptions filled by 21 percent and reduced spending by 27 percent.
Although the estimated declines in number of drugs purchased and drug expenditure associated with exceeding the cap were substantial, these declines occurred in response to percentage increases in out-of-pocket prices that were much larger. The out-of-pocket price to enrollees in the months before the cap was exceeded was estimated to average $2.82 per prescription filled; in months after the cap was hit the out-of-pocket price per prescription for the same drugs is computed to average $13.04, an increase of 363 percent. This is consistent with inelastic demand, as indicated by the computed (arc) elasticity of demand of −0.12.
The findings may also be put into perspective by considering the impact of the insurance design on enrollee out-of-pocket costs in relation to income. The estimated increase in out-of-pocket price per prescription was not large in dollar terms, and it remained a relatively small portion of the program expenditure per prescription used by SeniorCare enrollees. However, for elders on fixed incomes below 200 percent of FPL, these out-of-pocket price increases were likely very meaningful. If these enrollees were to maintain their rates of use of generic and brand drugs after hitting the cap, they would have experienced total monthly out-of-pocket expenditures that loom large in relation to income. At the out-of-pocket prices computed above, the monthly out-of-pocket expense for the average precap prescriptions would increase from 1.5 to 6.4 percent of a monthly income of $1,100, the estimated mean income for our population. Estimated average precap utilization for enrollees in the high-spending quartile would require 2.1 percent of an $1,100 per month income to be spent out of pocket, rising to 9.5 percent of average monthly income out of pocket after the cap was exceeded. It is no surprise that enrollees faced with these increased out of pocket costs respond by cutting back on utilization, and, to some extent, switching toward generic drugs.
The estimated elasticity of demand is similar to those estimated by others for changes in prescription drug copayments (Ringel et al. 2002; Contoyannis et al. 2005; Gemmill, Costa-Font, and McGuire 2007). Our finding that effects of increased cost sharing are greater for poorer consumers is also consistent with previous research (Newhouse 2004).
Conceptually, a cap effect is different from an exogenous copayment effect in that beneficiaries subject to a cap have the ability to anticipate exceeding the cap and thus to modify their utilization behavior before exceeding the cap. Auxiliary regression analyses of monthly spending for cohorts who hit the cap in different months (not shown) uncovered mixed evidence of a slight down turn in spending before the cap for some cohorts. This phenomenon should be further explored using models that can account for month-to-month revisions of expected future prices. In addition, a second year of data could reveal whether enrollees who exceeded the cap in their first program year exhibited different behavior when their copayments reverted to the precap level as a new insurance year began. Enrollees who learn from past experience with the cap may maintain lower spending in subsequent years in order to make their limited coverage last longer, or they may respond to a reinstatement of the lower copayment by spending at previous rates.
Because our ultimate concern is the health impacts of prescription drug plan design features, of greatest interest is further research detailing drug utilization changes made by enrollees who exceed the soft cap, and the link between these and any health effects. Such an investigation could supplement survey-based studies, which have demonstrated poor health outcomes for elders who report skipping doses, splitting pills, or failing to fill prescriptions due to cost (Heisler et al. 2004; Piette et al. 2004). In-depth investigation could detail whether enrollees who reduced their expenditures on prescription drugs in response to exceeding the cap did so by stretching certain prescriptions over a longer time period, by omitting certain drugs altogether, or by seeking generic substitutes for certain drugs. Follow-up analysis of linked Medicare claims could assess whether any clinical effects resulting from specific patterns of underuse by disease cohort can be observed in future health services utilization.
It is both a strength and a limitation of the current analysis that it relied on data derived from outpatient drug claims filed under an ongoing insurance program. Because out-of-pocket costs to enrollees were substantially below full pharmacy prices both before and after an enrollee exceeded the cap, we can be reasonably sure that we have captured most prescription drug utilization. However, data were missing for some enrollees, and claims were incomplete for one of the 12 program months. Over-the-counter drugs that might substitute for prescription drugs are not observable because they were not covered by SeniorCare.
This paper represents a contribution to the growing literature on the impact of caps and copayments on prescription drug utilization with respect to both data and methods. A previous study that compared Medicare+Choice enrollees with and without a hard cap of $1,000 (Hsu et al. 2006) found increasing differences between the two groups in the months after the spending limit was exceeded but focused on overall differences due to plan design rather than the temporal differences before and after the cap. Other studies of enrollees' response to the cap as a plan design feature have queried enrollees about their responses to a cap, but they have not made use of actual utilization for enrollees before and after they exceed a cap.
POLICY IMPLICATIONS
Near-poor elders are especially vulnerable to increases in out-of-pocket prices for prescription drugs. When faced with a copayment increase amounting to an additional 20 percent of prescription drug cost, on average a more than three-fold price increase, Illinois SeniorCare enrollees reduced the number of prescription drugs they purchased by an estimated 14 percent on average. We cannot assert that the prescription drug utilization of SeniorCare enrollees before they became subject to higher copayments was optimal for their health, but this substantial reduction in use in response to exceeding the expenditure cap does mean that enrollees facing high prices were not purchasing drugs that had previously been prescribed by their physicians. Elders who take less medicine than prescribed because of cost have been found to face significant declines in health (Heisler et al. 2004).
Medicare Part D beneficiaries with incomes above 135 percent FPL face a copayment only a few percentage points lower than the SeniorCare postcap copayment, 15 percent of cost, from the very first dollar of coverage; if their incomes exceed 150 percent FPL, not only do they face an even higher copayment (25 percent of cost) from their first purchase but also must pay full price after total expenditures reach a threshold, set at $2,700 for 2009. While Part D appears to be increasing older adults' access to the medicines prescribed for them (Madden et al. 2008), if near-poor Medicare beneficiaries respond similarly to out-of-pocket price as did the Illinois SeniorCare enrollees, we can infer that they are purchasing substantially fewer prescription drugs than they would have had out-of-pocket price been minimal, and those who reach the expenditure threshold are cutting back their utilization still further. With estimated effects that are especially large for those with the greatest initial utilization of prescription drugs, the impact on utilization of other health services, and on their health, is likely to be substantial.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The authors gratefully acknowledge the support of the Health Care Financing and Organization (HCFO) initiative of the Robert Wood Johnson Foundation, through the project “The Role of Benefit Design in Enrollment, Drug Use, and Expenditures,” Deborah Rogal (Project Officer) and Cindy Parks Thomas (Principal Investigator); and, for support for data development, the Centers for Medicare and Medicaid Services project, “Evaluation of the Impact of Pharmacy Plus Waivers in Illinois and Wisconsin on Medicare and Medicaid” (CMS 500-00-0031/TO2),William Clark (Project Officer), Donald Shepard (Principal Investigator). Andrew Ryan has been supported by a training grant from Agency for Health Care Research and Quality (grant number 05 T32 HS000062-14) and by the Jewish Healthcare Foundation under the grant “Achieving System-wide Quality Improvements—A collaboration of the Jewish Healthcare Foundation and Schneider Institutes for Health Policy.” Staff of the Illinois Department of Public Aid provided information concerning the ElderCare plan and supported access to data. Melissa Morley assisted with preparation of the data and preliminary analyses.
Disclosures: None.
Disclaimers: None.
NOTES
Enrollees may continue to fill prescriptions through their drug insurance plans after they hit a spending cap in order to benefit from discounted prices negotiated by their plans.
Several survey studies have found that enrollees in managed care plans report lower drug use after they exceed a drug spending cap (Balkrishnan et al. 2001; Cox et al. 2001; Cox and Henderson 2002).
Analysis of the effects of exceeding a cap on enrollees' prescription drug utilization is presented in online material supplementary to Hsu et al. (2006).
Enrollees with incomes below 100% FPL were not subject to the $1/$4 copayments, but they faced the 20% copayment after their annual expenditures reached $1,750. The plan charged no premium or enrollment fee. Prescriptions were covered only if filled by participating pharmacies, which did not include mail order pharmacies, for a maximum of 34 days' supply; the pharmacy network included most pharmacies in the state. The program had a high level of enrollment at startup (reported as 150,889 on day 1, June 1, 2002) in part because qualifying seniors from the preexisting state-funded pharmacy assistance program were automatically enrolled in SeniorCare. The preexisting program, which had no cap, covered only drugs used to treat a specific list of diseases set by the legislature.
The monthly deflators are available from the authors on request.
In addition to these trends, monthly drug utilization under the SeniorCare program might also be affected if an enrollee entered a hospital or another institution during a given month, because drugs might be supplied by those institutions during the institutional days. To determine if an adjustment for institutional days was needed, monthly utilization was regressed on indicators for the proportion of the month that the enrollee was in an inpatient facility paid for by Medicare. Time in an inpatient facility was not a significant predictor of drug utilization or spending.
The arc elasticity computation (Phelps and Newhouse 1972; Gemmill, Costa-Font, and McGuire 2007) is preferred when only specific points on the demand curve are observed. In this case, the point elasticity computation is sensitive to whether the prior or posterior price and quantity are used as the base for the percentage change computation.
Presenting utilization by cohorts defined by month they exceeded the cap rather than for all exceeders centered at the month the cap was exceeded highlights that by definition those who exceed the cap earlier in the program year have higher early spending. Figures showing all cohorts used in the analysis are available from the authors.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Appendix SA2: Analytic File Development.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Ai C, Norton EC. Interaction Terms in Logit and Probit Models. Economics Letters. 2003;80(1):123–9. [Google Scholar]
- Balkrishnan R, Byerly WG, Camacho FT, Shrestha A, Anderson RT. Effect of Prescription Benefit Changes on Medical Care Utilization in a Medicare HMO Population. American Journal of Managed Care. 2001;7(11):1093–100. [PubMed] [Google Scholar]
- Bond SR. Dynamic Panel Data Models: A Guide to Micro Data Methods and Practice. Portuguese Economic Journal. 2002;1(2):141–62. [Google Scholar]
- Contoyannis P, Hurley J, Grootendorst P, Jeon SH, Tamblyn R. Estimating the Price Elasticity of Expenditure for Prescription Drugs in the Presence of Non-Linear Price Schedules: An Illustration from Quebec, Canada. Health Economics. 2005;14(9):909–23. doi: 10.1002/hec.1041. [DOI] [PubMed] [Google Scholar]
- Cox ER, Henderson RR. Prescription Use Behavior among Medicare Beneficiaries with Capped Prescription Benefits. Journal of Managed Care Pharmacy. 2002;8(5):360–4. doi: 10.18553/jmcp.2002.8.5.360. [DOI] [PubMed] [Google Scholar]
- Cox ER, Jernigan C, Coons SJ, Draugalis JL. Medicare Beneficiaries' Management of Capped Prescription Benefits. Medical Care. 2001;39(3):296–301. doi: 10.1097/00005650-200103000-00009. [DOI] [PubMed] [Google Scholar]
- Gemmill MC, Costa-Font J, McGuire A. In Search of a Corrected Prescription Drug Elasticity Estimate: A Meta-Regression Approach. Health Economics. 2007;16(6):627–43. doi: 10.1002/hec.1190. [DOI] [PubMed] [Google Scholar]
- Heisler M, Langa KM, Eby EL, Fendrick AM, Kabeto MU, Piette JD. The Health Effects of Restricting Prescription Medication Use Because of Cost. Medical Care. 2004;42(7):626–34. doi: 10.1097/01.mlr.0000129352.36733.cc. [DOI] [PubMed] [Google Scholar]
- Hsu J, Fung V, Price M, Huang J, Brand R, Hui R, Fireman B, Newhouse JP. Medicare Beneficiaries' Knowledge of Part D Prescription Drug Program Benefits and Responses to Drug Costs. Journal of the American Medical Association. 2008;299(16):1929–36. doi: 10.1001/jama.299.16.1929. [DOI] [PubMed] [Google Scholar]
- Hsu J, Price M, Huang J, Brand R, Fung V, Hui R, Fireman B, Newhouse JP, Selby JV. Unintended Consequences of Caps on Medicare Drug Benefits. New England Journal of Medicine. 2006;354(22):2349–59. doi: 10.1056/NEJMsa054436. [DOI] [PubMed] [Google Scholar]
- Joyce GF, Goldman DP, Karaca-Mandic P, Zheng Y. Pharmacy Benefit Caps and the Chronically Ill. Health Affairs. 2007;26(5):1333–44. doi: 10.1377/hlthaff.26.5.1333. [DOI] [PubMed] [Google Scholar]
- Madden JM, Graves AJ, Zhang F, Adams AS, Briesacher BA, Ross-Degnan D, Gurwitz JH, Pierre-Jacques M, Safran DG, Adler GS, Soumerai SB. Cost-Related Medication Nonadherence and Spending on Basic Needs Following Implementation of Medicare Part D. Journal of the American Medical Association. 2008;299(16):1922–8. doi: 10.1001/jama.299.16.1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin BC, McMillan JA. The Impact of Implementing a More Restrictive Prescription Limit on Medicaid Recipients. Medical Care. 1996;34(7):686–701. doi: 10.1097/00005650-199607000-00003. [DOI] [PubMed] [Google Scholar]
- Newhouse JP. Consumer-Directed Health Plans and the RAND Health Insurance Experiment. Health Affairs (Millwood) 2004;23(6):107–13. doi: 10.1377/hlthaff.23.6.107. [DOI] [PubMed] [Google Scholar]
- Phelps CE, Newhouse JP. Effect of Coinsurance: A Multivariate Analysis. Social Security Bulletin. 1972;35:20–29, 44. [Google Scholar]
- Piette JD, Wagner TH, Potter MB, Schillinger D. Health Insurance Status, Cost-Related Medication Underuse, and Outcomes among Diabetes Patients in Three Systems of Care. Medical Care. 2004;42(2):102–9. doi: 10.1097/01.mlr.0000108742.26446.17. [DOI] [PubMed] [Google Scholar]
- Ringel JS, Hosek SD, Vollaard BA, Mahnovski S. “The Elasticity of Demand for Health Care: A Review of the Literature and Its Application to the Military Health System.” Santa Monica. Rand Corporation. Available at http://rand.org/pubs/monograph_reports/2005/MR1355.pdf.
- Safran DG, Neuman P, Schoen C, Montgomery JE, Li W, Wilson IB, Kitchman MS, Bowen AE, Rogers WH. Prescription Drug Coverage and Seniors: How Well Are States Closing the Gap? Health Affairs. 2002;22:253–68. doi: 10.1377/hlthaff.w2.253. [DOI] [PubMed] [Google Scholar]
- Soumerai SB, Ross-Degnan D, Avorn J, McLaughlin TJ, Choodnovskiy I. Effects of Medicaid Drug-Payment Limits on Admission to Hospitals and Nursing Homes. New England Journal of Medicine. 1991;325(15):1072–7. doi: 10.1056/NEJM199110103251505. [DOI] [PubMed] [Google Scholar]
- Tseng CW, Brook RH, Keeler E, Mangione CM. Impact of an Annual Dollar Limit or ‘cap’ on Prescription Drug Benefits for Medicare Patients. Journal of the American Medical Association. 2003;290(2):222–7. doi: 10.1001/jama.290.2.222. [DOI] [PubMed] [Google Scholar]
- Tseng CW, Brook RH, Keeler E, Steers WN, Mangione CM. Cost-Lowering Strategies Used by Medicare Beneficiaries Who Exceed Drug Benefit Caps and Have a Gap in Drug Coverage. Journal of the American Medical Association. 2004;292(8):952–60. doi: 10.1001/jama.292.8.952. [DOI] [PubMed] [Google Scholar]
- Wooldridge JM. A Simple Specification Test for the Predictive Ability of Transformation Models. Review of Economics and Statistics. 1994;76(1):59–65. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.