Abstract
Purpose
We determine the rate of nursing home closures for 7 years (1999–2005) and examine internal (e.g., quality), organizational (e.g., chain membership), and external (e.g., competition) factors associated with these closures.
Design and Method
The names of the closed facilities and dates of closure from state regulators in all 50 states were obtained. This information was linked to the Online Survey, Certification, and Reporting data, which contains information on internal, organizational, and market factors for almost all nursing homes in the United States.
Results
One thousand seven hundred and eighty-nine facilities closed over this time period (1999–2005). The average annual rate of closure was about 2 percent of facilities, but the rate of closure was found to be increasing. Nursing homes with higher rates of deficiency citations, hospital-based facilities, chain members, small bed size, and facilities located in markets with high levels of competition were more likely to close. High Medicaid occupancy rates were associated with a high likelihood of closure, especially for facilities with low Medicaid reimbursement rates.
Implications
As states actively debate about how to redistribute long-term care services/dollars, our findings show that they should be cognizant of the potential these decisions have for facilitating nursing home closures.
Keywords: Nursing homes, closures, quality, OSCAR
Since the implementation of the Medicaid program in 1965, nursing homes have been the predominant institutional providers of long-term care. However, in recent years, there has been growth in alternative sources of long-term care, such as assisted living and home care services (Hawes et al. 2003). Furthermore, public policy makers have expanded the coverage of home- and community-based services (primarily under Medicaid waivers) in order to keep those in need of long-term care in the community (Wiener, Tilly, and Alecxih 2002). Not surprisingly, the expansion of these long-term care alternatives has influenced nursing homes. We have seen a drop in the nursing home occupancy rates (Bishop 1999) from an average of 91 percent in 1991 (Online Survey, Certification and Reporting [OSCAR] 1992) to 85 percent in 2006 (OSCAR 2007). Although the number of nursing homes has increased over this time period, we expect that the expansion of long-term care alternatives may have influenced nursing home closures in recent years.
We first look at the rate of nursing home closures over a recent 7-year period (1999–2005) and, second, examine internal (e.g., quality), organizational (e.g., hospital affiliation), and external (e.g., competition) factors associated with these closures. Examining internal, organizational, and external factors is important because we expect that some types of nursing homes (e.g., hospital based) may be more likely to close than others and some external forces (e.g., a high degree of competition) may influence closure more than others.
LITERATURE REVIEW
We identified five empirical studies examining nursing home closures. Dalton and Howard (2002) used the administrative database, the OSCAR data, to provide descriptive analyses of exit and entry in the nursing home market from 1982 to 1998. They found that entry exceeded exit until 1998 and that the market expansion then ceased in 1998. Kitchener, Bostrom, and Harrington (2004), using data from the California Office of Statewide Healthcare Planning and Development, provided more detailed insights into the causes and effects of nursing home closures from 1990 to 2000 by examining nursing homes in California. They found that low Medicaid reimbursement rates, lower levels of private-pay residents, and relatively small size were associated with the likelihood of closure. More recently, using the OSCAR data and data from a survey of state nursing home regulators, Castle (2006) examined facility and market characteristics associated with closures. He found that lower Medicaid reimbursement rates, lower occupancy, higher competition, and lower quality of care were significantly associated with closure. On additional research, he found that nursing home competition (Castle 2005a) and quality of care (Castle 2005b) were major determinants of nursing home closures from 1992 to 1999. Over this time period, 0.7 percent of the facilities closed each year (Castle 2005b).
In summary, these prior studies identified several internal (e.g., quality; Castle 2006), organizational (e.g., bed size; Kitchener, Bostrom, and Harrington 2004), and external (e.g., competition; Castle 2005a) factors to be associated with nursing home closures. However, various internal, organizational, and external factors have changed considerably since the completion of these studies. Medicare implemented a nursing home prospective payment system, the Centers for Medicare and Medicaid Services (CMS) has published data on nursing home quality, Medicaid payments have not kept up with inflation, and there is increasing competition from other long-term care providers. Furthermore, many nursing homes are in financial difficulty and many are operating under bankruptcy proceedings (Kitchener, O'Neill, and Harrington 2005).
Closure of nursing homes may have important implications for residents and the nursing home market. Reports detailing the circumstances surrounding nursing home closures (Castle 1997; Wood 2002) highlighted the resident stress involved and the possible negative health consequences. Moreover, one empirical study of 301 residents relocated from one closed nursing home to 40 other facilities identified significant detrimental effects of this relocation on residents' cognitive performance, depression, social engagement, and activities of daily living (Castle 2005c). For the nursing home market, the threat of closure may influence provider behavior in a positive way—nursing homes may improve quality of care or the types of services they provide (Castle 2005b).
CONCEPTUAL FRAMEWORK
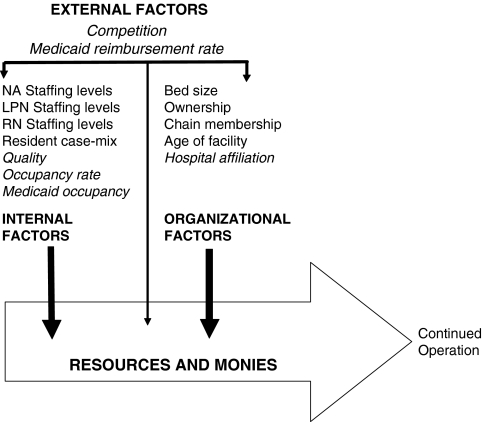
In prior research on nursing home closures, Castle (2005b) developed a conceptual framework based on the more extensive hospital closure literature. He proposed that external, organizational, and internal factors influenced closure. External factors are characteristics external to the organization, such as regulation. These factors help define the context in which the facility operates. Organizational factors are characteristics of the facility itself, such as chain membership. These factors are the relatively stable attributes of the facility. Internal factors are operating characteristics of the facility, such as the occupancy rate. These factors reflect operating decisions within the facility and, for many facilities, can vary over time.
In this paper, we enrich this framework. We speculate that institutional viability is highly dependent on available resources. State policies and regulations (external factors) can significantly impact the financial resources of an organization. Medicaid reimbursement, for example, varies based on state policies. Likewise, organizational factors and internal factors can significantly impact resources for operation. Chain membership (organizational factor) can provide a facility in financial difficulty, with resources needed to maintain operations. A high occupancy rate (internal factor) can help improve the revenue of a facility.
Our conceptual framework is shown in Figure 1. The external, organizational, and internal factors included in Figure 1 include all of those initially proposed by Castle (2005b) as well as those examined in prior research discussed above. In addition, we have included hospital affiliation and interactions. Each of the factors is expected to have a direct association with resources and, therefore, closure. We also raise the possibility that external, organizational, and internal factors may act jointly on closure (i.e., interaction effects). Interaction effects are implied by the indirect pathways of some of the arrows in the figure. However, we note that many interactions are possible and, in this study, we focus on one interaction between Medicaid reimbursement rates and Medicaid occupancy.
Figure 1.
Proposed Conceptual Model
Note: Variables presented in italics are the independent variables of interest in the analyses. External factors are defined as characteristics external to the organization, such as regulation. Organizational factors are defined as characteristics of the facility itself, such as chain membership. Internal factors are defined as operating characteristics of the facility, such as the occupancy rate.
Several of the factors in the conceptual model, including hospital affiliation, are further discussed below. We focus on specific factors (italicized in the figure) because they likely reflect recent changes in internal, organizational, and external factors of nursing homes.
Some further justification for this conceptual model is provided by recent qualitative analyses. Examining keywords from the text of 192 different newspaper articles (from January 1, 1999, to June 1, 2005) describing nursing home closures, Fisher and Castle (2008) identified financial concerns as the most frequently cited reason for nursing home closure. All of the factors presented in the conceptual model were also significant in this prior analysis, with Medicaid occupancy and Medicaid reimbursement being frequently cited.
FACTORS INFLUENCING NURSING HOME CLOSURES
Medicare introduced a prospective payment system for nursing homes in 1998. The new payment system led to a decrease in the Medicare payments in many facilities, but it had a relatively more negative impact on hospital-based skilled nursing facilities than freestanding facilities (Konetzka, Norton, and Sterns 2006). Nursing homes reliant on Medicare payments, such as hospital-based nursing homes, may have experienced overall financial losses. Thus, hospital-based nursing homes may be more likely to close than freestanding facilities due to these cuts in the Medicare payments. Moreover, hospital-based nursing homes may be more inclined to close than freestanding facilities because their closing would represent the closing of a single unit of a much larger facility rather than the closing of the whole organization. We hypothesize as follows:
Hypothesis 1: Hospital-based nursing homes are more likely to close than freestanding nursing homes.
Many nursing homes are reliant on Medicaid payments (Grabowski 2001). State Medicaid programs account for about approximately 50 percent of all expenditures on nursing home services (Grabowski 2001). Because payments to nursing homes make up a significant portion of the states' Medicaid budgets, the states pay considerable attention to these costs. In recent years, Medicaid payments for nursing homes have not kept up with the rate of inflation (Grabowski et al. 2004). While facilities may be able to adapt to some reduction in reimbursements, at some point, the total revenue may not be sufficient for a facility to remain viable. Thus, Medicaid reimbursement rates may be associated with nursing home closures, and this association becomes more apparent over time as states ratchet-down their reimbursements. Moreover, the influence of Medicaid reimbursement rates is likely greater in facilities with a higher Medicaid occupancy. Facilities with higher Medicaid occupancy may be more likely to close and this association is likely to become more apparent over time as reimbursement rates decline. Thus, we hypothesize as follows:
Hypothesis 2a: Nursing homes with high Medicaid occupancy are more likely to close than those with low occupancy.
Hypothesis 2b: Nursing homes with low Medicaid reimbursement rates will be more likely to close than those with high reimbursement rates.
Hypothesis 2c: Nursing homes with both high Medicaid occupancy and low Medicaid reimbursement rates will be more likely to close than would be expected based on either factor individually.
Quality concerns with nursing homes are a chronic issue. For example, Lexus-Nexus lists 754 newspaper articles over the past 3 years describing the poor quality of nursing homes. These press reports may have sensitized consumers to the quality issues associated with choosing a nursing home. Furthermore, CMS has made improvements to the certification process (General Accounting Office [GAO] 1999). These improvements include greater consistency of inspections and more attention to resident quality issues (GAO 1999). In addition, more information on the quality of individual nursing homes is posted on the CMS website. With more attention on nursing home quality and with potentially stricter enforcement of rules and regulations, poor-quality nursing homes may be more likely to close. The influence of poor quality may also be cumulative. That is, as a facility gains a reputation for poor-quality resident, census may decline, fines may be levied, and the numbers of more profitable private-pay residents may decline. Thus, the association between poor quality and closure may become stronger over time. We hypothesize as follows:
Hypothesis 3a: Nursing homes with poor quality are more likely to close than nursing homes with high quality.
Hypothesis 3b: Nursing homes with poor quality are at increased risk for closure over time than those with high quality.
In many markets, nursing homes compete with each other for residents (Mukamel, Spector, and Bajorska 2005). Competition can promote innovation and quality improvement. Nevertheless, facilities that do not compete successfully risk closure. Thus, we propose that higher levels of competition will be associated with nursing home closures. As we have argued above, with respect to quality and Medicaid reimbursement, the influence of competition may be cumulative; that is, the association between higher competition and closure may become stronger over time. We hypothesize as follows:
Hypothesis 4a: Nursing homes operating in more competitive markets are more likely to close than nursing homes operating in less competitive markets.
Hypothesis 4b: Nursing homes operating in more competitive markets are at increased risk for closure over time than those operating in less competitive markets.
Others have reported on the declining occupancy rates of nursing homes (Bishop 1999). Analyses of the OSCAR data show that occupancy rates have continued to decline in recent years. As occupancy rates fall, it is likely that profitability also decreases. Thus, nursing homes with lower occupancy rates may be more likely to close. In some cases, facilities may continue to operate as occupancy rates decline. Facilities may use existing resources and reserves to continue to operate. However, this depletion of resources cannot occur indefinitely and the association between low occupancy and closure may become stronger over time. We hypothesize as follows:
Hypothesis 5a: Nursing homes operating with low occupancy rates are more likely to close than nursing homes with high occupancy rates.
Hypothesis 5b: Nursing homes with low occupancy rates are at increased risk for closure over time than those with high occupancy rates.
DATA AND METHODS
Data Sources
We obtained information on closed nursing homes from a survey of state regulatory agencies. A letter was sent out to the Departments of Ageing, nursing facility regulatory agency, or elder care ombudsman of all 50 states and the District of Columbia asking for assistance in producing a list of the names of all nursing homes that had closed between January 1, 1999, and June 1, 2005. With repeat mailings, e-mail, and phone call follow-up, we achieved a response rate of 100 percent. We noted in our mailings and phone calls that we were interested in closed facilities and not those that were sold or had undergone ownership change. We checked the accuracy of the data received by looking in the 2006 OSCAR data to see if any of the closed facilities were listed therein—none were. We also checked whether phone listings of potentially closed facilities existed. No closed facility had a listed telephone number.
We obtained data on all internal and organizational factors as well as data on some external (i.e., competition) factors from the OSCAR. The OSCAR is conducted by state licensure and certification agencies as part of the Medicare/Medicaid certification process and includes almost all nursing homes in the United States. The few nursing homes that are neither Medicare nor Medicaid certified (approximately 1,000) are not included in the data. The OSCAR data are widely used (e.g., Grabowski et al. 2004). Nevertheless, it should be acknowledged that the reliability of the data has been questioned (Harrington et al. 2000).
Medicaid reimbursement levels from 1999 included in the analyses (as external factors) were obtained from a published source (Grabowski et al. 2004). Additional information for 2000 through 2005 came from primary data collected by the authors.
Model Specification
Table 1 lists the internal, organizational, and external variables, along with their definitions, which are used in this analysis. We used quality of care-deficiency citations as the quality indicator. Deficiency citations were recommended for use by the Institute of Medicine (2001), are readily available, frequently used by researchers (e.g., Harrington et al. 2000), and are used as the basis of the quality information in many nursing home report cards (Castle and Lowe 2005). Deficiency citations indicate whether or not facilities meet regulatory standards (Tsoukalas et al. 2006). However, they do differ in scope and severity and in the areas of care they address (Tsoukalas et al. 2006). Following other research using deficiency citations, we use a group of deficiency citations labeled quality of care citations (listed in the footnote to Table 1) because they are believed to be most closely related to resident care (Harrington et al. 2000).
Table 1.
Dependent and Independent Variables
| Variable | Operational Definition |
|---|---|
| Dependent variable | |
| Closure | If facility closed (1)* or not (0) from 1999 to 2005 |
| Independent variables of interest | |
| Hospital affiliation | Whether the facility was owned and operated by a hospital (1) or not (0) |
| Medicaid reimbursement | The average reimbursement rate for Medicaid residents in the state ($) |
| Medicaid occupancy | Average daily Medicaid occupancy rate |
| Quality indicator | Quality of care-deficiency citations.† We used within-state rankings (percentiles) for the analyses |
| Competition | Herfindahl Index. That is, each facility's percentage share of beds in the county/squared market shares of all facilities in the county (0–1). Higher values indicate a less-competitive market |
| Occupancy rate | Average daily resident occupancy rate |
| Other independent variables | |
| Internal factors | |
| Nurse aide staffing | FTE nurse aides per 100 residents |
| LPN staffing | FTE LPNs per 100 residents |
| RN staffing | FTE RNs per 100 residents |
| Resident case-mix | The score for three ADLs (eating, toileting, and transferring) constructed by giving a score of 1 for low assistance, 2 for moderate assistance, and 3 for high need for assistance summed for each ADL |
| Organizational factors | |
| Bed size | Number of beds in the nursing home |
| Ownership | For-profit (1) or not-for-profit (0) ownership |
| Chain membership | Whether member of a nursing home chain (1) or not (0) |
| New facility | If the facility opened (1) or not (0) from 1999 to 2005 |
Coding used for analyses.
F-tag 309, facility must provide the necessary care and services for each resident to attain or maintain the highest practicable well-being; F-tag 310, a resident's abilities in the ADL must not diminish unless clinical conditions make it unavoidable; F-tag 311, facility must provide appropriate treatment and services to maintain or improve residents' abilities in the ADL; F-tag 312, residents who are unable to perform ADL must receive necessary services to maintain good nutrition, grooming, and hygiene; F-tag 314, facility must ensure that residents entering facility without pressure sores do not develop sores and that residents with sores receive necessary treatment to promote healing, prevent infection, and prevent new sores; F-tag 316, incontinent residents must receive treatment and services to prevent urinary tract infections and restore as much normal function as possible; F-tag 317, residents who enter the facility without a limited range of motion must not experience a decline, unless clinical conditions make it unavoidable; F-tag 318, residents with a limited range of motion must receive appropriate treatment to increase range of motion or prevent further decline; F-tag 319, residents who display mental or psychosocial problems must receive appropriate treatment and services to correct assessed problems; F-tag 321, residents who have been able to eat alone or with assistance must not be fed by nasogastric tubes, unless clinical conditions make it unavoidable; F-tag 322, residents who are tube fed must receive appropriate treatment to prevent aspiration, vomiting, and other complications; if possible, restore normal eating skills; F-tag 323, facility must ensure resident environment is as free of accident hazards as is possible; F-tag 324, facility must ensure that each resident receives adequate supervision and assistance devices to prevent accidents; F-tag 325, facility must ensure that each resident maintains acceptable parameters of nutritional status, such as body weight; F-tag 328, facility must ensure that residents receive necessary treatment and specialized services; F-tag 329, residents have the right to be free from unnecessary drugs; F-tag 330, residents must not be given antipsychotic drugs unless needed to treat a specific condition diagnosed and documented in the clinical record; F-tag 333, facility must ensure that residents are free of any significant medication errors; F-tag 353, facility must have sufficient nursing staff to provide services to attain or maintain the highest practicable well-being for each resident.
FTE, full-time equivalent; ADL, activities of daily living; RNs, registered nurses; LPNs, licensed practical nurses.
Analyses
The dependent variable in our analysis is facility closure and the independent variables of interest are the internal, organizational, and the external factors discussed above. We used a discrete-time logistic regression to assess the impact of the independent variables on closure. This model calculates each independent variable's effect on the relative odds of closing (coded as 1) versus not closing (coded as 0). The computational formula for the discrete time logit is as follows. Let Pit be the conditional probability that facility i closed at time t, given that the closure has not already occurred to that facility. In this model, Pit is related to the covariates by a logit-regression equation:
where i is the facility index and t the time point. The left side of the equation is the logit of Pit while the right side is the linear function of the covariates plus a constant term, αt.
We used a discrete time approach for several reasons. First, it corresponds to the form in which the data are collected. Discrete time analysis recognizes that OSCAR assessments represent a series of snapshots, each taken at a point in time. Each assessment can be described in terms of the time that has elapsed since the last assessment and in relation to a facility closure. Second, discrete time models easily accommodate time-varying covariates. Moreover, the discrete time logit model uses maximum likelihood methods for estimation (partial likelihood is used in Cox models). Maximum likelihood estimation is advantageous for challenging features of the data (e.g., discrete time, tied data, time-dependent covariates, and truncated data) and is well suited for large datasets (Allison 1995).
We applied the Huber–White robust estimator to all our standard errors to address correlated errors resulting from multiple observations from each nursing home. In addition, to account for time trends in both the risk of closure and in the association between closure and some of the dependent variables of interest, a time trend and a series of interaction terms with the time trend are included in the analyses. The time trend is coded as 1 in 1998, 2 in 1999, and so forth. If an interaction of a variable with time is significant, the implication is that the odds ratio of that variable changes significantly over time.
RESULTS
Table 2 presents descriptive statistics of the nursing homes that were in existence in 1999, depending on whether they had closed or remained open between 1999 and 2005. We found that 1,789 nursing homes had closed between January 1, 1999, and June 1, 2005. This represents 1.9 percent of the facilities closing per year. We also note that 2,034 nursing homes opened over the same time period; however, only 23 percent of these new facilities were in the same market as the closed facilities.
Table 2.
Descriptive Statistics of Closed Nursing Homes and Facilities in Constant Operation from 1999 to 2005
| Closed† |
Not Closed‡ |
|||
|---|---|---|---|---|
| Variables | Mean (or %) | Standard Deviation | Mean (or %) | Standard Deviation |
| Independent variables of interest | ||||
| Hospital-based facility | 27% | — | 10%* | — |
| Average Medicaid reimbursement rate ($) | 91.97 | 22.62 | 94.20* | 24.37 |
| Average Medicaid resident occupancy | 63.65% | 25.19 | 56.91%* | 34.95 |
| Quality of care-deficiency citations | 7.01 | 7.75 | 6.52* | 7.12 |
| Competition (Herfindahl Index) | 0.159 | 0.198 | 0.215* | 0.244 |
| Average occupancy rate | 77.01% | 21.23 | 85.43% | 16.59 |
| Other internal factors | ||||
| FTE nurse aides/100 residents | 32.45 | 16.07 | 32.31 | 13.86 |
| FTE LPNs/100 residents | 13.31 | 12.55 | 10.90* | 8.46 |
| FTE RNs/100 residents | 11.53 | 16.32 | 6.38* | 9.16 |
| Resident case mix (ADL score) | 1.61 | 0.84 | 1.72 | 0.76 |
| Other organizational factors | ||||
| Bed size (number of beds) | 81.22 | 73.33 | 110.35* | 73.48 |
| For-profit ownership | 61% | — | 67%* | — |
| Member of a chain | 53% | — | 52% | — |
N=1,789 facilities (based on the 1999 data).
N=11,652 facilities (based on the 1999 data).
Difference between closed and nonclosed facilities is significant at p<.001.
Note: during the study period, 2,034 nursing homes opened. These are included in the multivariate analyses. Also, the figures presented are for the baseline 1999 data. Thus, the closed column represents the 1999 values for any nursing home that closed from 1999 through 2005, whereas the not closed column represents the 1999 values for any nursing home in constant operation during this same period. The baseline figures are presented for parsimony.
FTE, full-time equivalent; ADL, activities of daily living; RNs, registered nurses; LPNs, licensed practical nurses.
In a bivariate comparison, those nursing homes that closed were smaller, were less likely to be for profit, had a lower occupancy rate, were more likely to be hospital based, had a higher percent Medicaid residents, had more Licensed Practical Nurses per 100 residents, had more quality of care citation deficiencies, and had a lower Medicaid reimbursement rate (see Table 2).
Results from the discrete-time logistic regression are shown in Table 3. We provide the logistic coefficients on the main effects for each variable and on the interactions with the time trend for variables for which we wish to investigate the changing association with closure probability over the 7-year period for which we have data. The main effects are the effect of each variable in 1998. The coefficient on the time trend itself is not significantly different from zero, suggesting that all the change in the closure rates over time can be accounted for by changes in the explanatory variables and changes in their coefficients. Although this table is useful for presenting the statistical significance of the coefficients, we convert these coefficients to odds ratios for ease of interpretation.
Table 3.
Discrete Time Logistic Regression Analyses Comparing Closed and Nonclosed Nursing Homes from 1999 to 2005
| Main Effect |
Interaction with Time Trend |
|||
|---|---|---|---|---|
| Coefficient | p-value | Coefficient | p-value | |
| Independent variables of interest | ||||
| Hospital-based facility | 1.010 | <.0001 | ||
| Medicaid reimbursement rate | −2.770 | <.0001 | 0.130 | .002 |
| Medicaid resident occupancy | −0.719 | .017 | 0.222 | .005 |
| Medicaid reimbursement rate × Medicaid resident occupancy rate | 0.201 | .001 | −0.041 | .011 |
| Quality of care-deficiency citations | 0.288 | <.001 | 0.029 | .103 |
| Competition (Herfindahl index) | 0.533 | <.001 | −0.044 | .077 |
| Occupancy rate | −0.519 | <.001 | −0.023 | .151 |
| Other internal factors | ||||
| FTE NAs/100 beds | −0.057 | .219 | 0.005 | .677 |
| FTE LPNs/100 beds | −0.005 | .933 | −0.003 | .830 |
| FTE RNs/100 beds | 0.085 | .117 | 0.015 | .290 |
| Resident case mix (ADL score) | −0.114 | .242 | 0.011 | .661 |
| Other organizational factors | ||||
| Bed size | −1.045 | <.001 | ||
| For-profit ownership | −0.107 | .194 | ||
| Chain membership | 0.299 | <.001 | ||
| New facility | 0.429 | .001 | ||
| Intercept and time trend | 10.532 | <.001 | 0.073 | .759 |
N=173,219 observations.
All continuous variables are divided by their standard deviation.
Time trend=1 in 1998, 2 in 1999, and so forth through 2005.
State dummies also included (not shown).
p-values use standard errors adjusted using the Huber–White robust estimator.
FTE, full-time equivalent; ADL, activities of daily living; RNs, registered nurses; LPNs, licensed practical nurses; NAs, nurse aides.
Table 4 presents the odds ratios. For continuous variables, we present the adjusted odds ratio (AOR) associated with a 1-standard deviation increase in the variable. We present the AORs at three points in time—the first year, the middle year, and the final year of our data. Our interaction of some of the variables with a linear time trend implies that the estimates for the omitted years lie in the interval between the estimates for the years that we report.
Table 4.
Results Showing Discrete Time Logistic Regression Analyses-Adjusted Odds Ratios Comparing Closed and Nonclosed Nursing Homes from 1999, 2002, and 2005
| Year |
|||
|---|---|---|---|
| 1999 | 2002 | 2005 | |
| AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | |
| Independent variables of interest | |||
| Hospital based† | 2.746* | 2.746* | 2.746* |
| (2.174, 3.469) | (2.174, 3.469) | (2.174, 3.469) | |
| Medicaid reimbursement rate‡ | 0.103* | 0.120* | 0.138* |
| (0.073, 0.146) | (0.084, 0.170) | (0.092, 0.208) | |
| Medicaid resident occupancy§ | 1.089 | 1.473* | 1.991* |
| (0.936, 1.267) | (1.235, 1.756) | (1.401, 2.828) | |
| Quality of care-deficiency citations | 1.413* | 1.541* | 1.681* |
| (1.303, 1.533) | (1.427, 1.664) | (1.427, 1.981) | |
| Competition (Herfindahl Index) | 1.559* | 1.364* | 1.194 |
| (1.360, 1.786) | (1.237, 1.505) | (0.968, 1.474) | |
| Occupancy rate | 0.568* | 0.530* | 0.495* |
| (0.527, 0.613) | (0.493, 0.571) | (0.426, 0.576) | |
| Internal factors | |||
| FTE NAs/100 beds | 0.954 | 0.968 | 0.982 |
| (0.904, 1.007) | (0.920, 1.018) | (0.883, 1.092) | |
| FTE LPNs/100 beds | 0.988 | 0.978 | 0.968 |
| (0.920, 1.061) | (0.906, 1.055) | (0.827, 1.132) | |
| FTE RNs/100 beds | 1.122* | 1.175* | 1.230* |
| (1.054, 1.195) | (1.095, 1.261) | (1.066, 1.420) | |
| Resident case mix (ADL score) | 0.912 | 0.941 | 0.972 |
| (0.814, 1.021) | (0.844, 1.049) | (0.775, 1.228) | |
| Organizational factors | |||
| Bed size† | 0.352* | 0.352* | 0.352* |
| (0.313, 0.396) | (0.313, 0.396) | (0.313, 0.396) | |
| For-profit ownership† | 0.898 | 0.898 | 0.898 |
| (0.764, 1.056) | (0.764, 1.056) | (0.764, 1.056) | |
| Chain membership† | 1.348* | 1.348* | 1.348* |
| (1.176, 1.545) | (1.176, 1.545) | (1.176, 1.545) | |
| New facility† | 1.536* | 1.536* | 1.536* |
| (1.182, 1.995) | (1.182, 1.995) | (1.182, 1.995) | |
N=173,219 observations.
Significant at a 5% level.
Variable assumed to have constant impact throughout the 1999–2005 time period.
Adjusted odds ratio for the Medicaid reimbursement rate incorporates the interaction with Medicaid resident occupancy and is evaluated at the mean value for Medicaid resident occupancy.
Adjusted odds ratio for the Medicaid resident occupancy incorporates the interaction with Medicaid reimbursement rate and is evaluated at the mean value for Medicaid reimbursement rate.
All continuous variables are divided by their standard deviation. State dummies also included (not shown).
FTE, full-time equivalent; ADL, activities of daily living; RNs, registered nurses; LPNs, licensed practical nurses; NAs, nurse aides; AOR, adjusted odds ratio; CI, confidence interval.
For the organizational factors, bed size (AOR 0.35; p≤.001) was significant, suggesting that small facilities were more likely to close than large facilities. Chain membership was significantly associated with closure (AOR 1.35; p≤.001). New facilities were significantly more likely to close (AOR 1.54; p≤.001). None of the staffing measures were significantly associated with closing nor did their associations change over time.
Quality of care-deficiency citations and occupancy were the internal factors of interest that were significantly associated with nursing home closure (we discuss percent Medicaid residents below with its interaction with Medicaid reimbursement rates). In 1999, the likelihood of closing was significantly higher for facilities with more quality of care citations (AOR 1.413, p≤.001) and remained relatively stable throughout the period. As shown in Table 3, the increase over time in this relationship was not statistically significant (p=.103). Higher occupancy was associated with a lower likelihood of facility closure (AOR 0.568, p≤.001), and this relationship was also relatively stable over time.
Hospital affiliation was the organizational factor of interest that was significantly associated with nursing home closure. Hospital-based facilities were more than twice as likely to close (AOR 2.746, p≤.001) than freestanding facilities.
For the external factors of interest, competition from other nursing homes was significantly associated with nursing home closures in 1999 (AOR 1.559; p<.001). Higher levels of competition from other nursing homes were associated with an increased likelihood of nursing home closures, but this relationship was decreasing over time and was not significant in 2005.
The association of percent Medicaid residents and closure changed significantly over time. It was not significant in the early part of the time frame but had a significant positive association with closures by 2005 (AOR 1.991; p≤.001). We found that higher Medicaid reimbursement rates were significantly associated with fewer closures, but this relationship weakens somewhat over time.
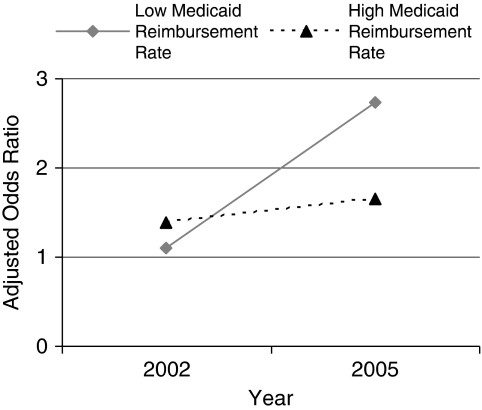
We included an interaction of Medicaid reimbursement rates and Medicaid occupancy rates in the model in order to determine whether lower reimbursement rates had a bigger association with closure for facilities with a high percentage of Medicaid residents. In order to facilitate the interpretation of the interactions that allow for a complex association between Medicaid occupancy and closures as it changes over time and varies by level of Medicaid reimbursement, we present the time trends in the association for two levels of Medicaid reimbursement. Figure 2 shows that Medicaid occupancy 1 standard deviation above average was associated with approximately a 50 percent higher rate of closure in 2002, regardless of the Medicaid reimbursement rate. By 2005, such high Medicaid occupancy was associated with almost a three-fold higher closure probability for facilities with low Medicaid reimbursement rates, but less than a two-fold higher closure probability for facilities with high Medicaid reimbursement rates.
Figure 2.
Association of Medicaid Occupancy Rate and Closure
Notes: Odds ratio reflects the association between a 1 standard deviation increase in Medicaid occupancy and the probability of nursing home closure. Low Medicaid reimbursement rate is set to $60 per day. High Medicaid reimbursement rate is set to $120 per day. These amounts are approximately 1 standard deviation lower and higher, respectively, than the average reimbursement rate. All amounts are adjusted for inflation, using 2000 as the base year. This figure reflects the interaction of Medicaid reimbursement rates and Medicaid occupancy rates in the closure logistic regression. The odds ratio with respect to Medicaid occupancy rate was approximately 1.2 for all nursing homes in 2002, regardless of their Medicaid reimbursement rate. By 2005, the odds ratio with respect to the Medicaid occupancy rate had increased for all nursing homes, but it had increased the most for nursing homes with low Medicaid reimbursement rates.
DISCUSSION
We found that 1,789 nursing homes, or 8 percent of the nursing homes that were in operation in 1999, had closed between 1999 to mid-2005. This indicated that approximately 2 percent of the facilities were closing each year. This rate of closure (using the same methodology) is considerably higher than the previously identified annual closure rate of 0.7 percent, which was experienced between 1992 and 1998 (Castle 2005b).
Policy Implications
Our results suggest that long-term care policies may have a significant influence on nursing home closures. These include policies related to nursing home payments and quality of care.
Nursing Home Payments
Medicare primarily pays for short-stay nursing home residents and accounts for approximately 12 percent of the nursing home revenues. However, these revenues are disproportionately distributed to facilities that specialize in providing short-term care. Hospital-based facilities primarily provide such care. The Medicare Prospective Payment, which replaced a nursing home cost-based system, was associated with a decrease in the Medicare payments to nursing homes by several billion dollars (Konetzka, Norton, and Sterns 2006). Some recent research has shown that these changes in Medicare payment may have adversely influenced quality of care (Zhang, Unruh, and Wan 2008). We are unable to directly examine the influence of these changes in Medicare payment, but our results suggest that the impact of these payment changes may have been most severe on hospital-based facilities, with these facilities having a higher likelihood of closure.
Some freestanding nursing homes specialize in providing short-term care, and most freestanding nursing homes receive some revenues from Medicare. Some research has shown that the Medicare Prospective Payment may have decreased the efficiency of these nursing homes (Zhang, Unruh, and Wan 2008). However, in preliminary analyses, closures were not associated with Medicare resident occupancy rates. Thus, this variable was not included in the final analysis.
Medicaid payments account for approximately 50 percent of the nursing home revenues. Our results show that reductions in the state payment rates are associated with nursing home closures. As would be expected, facilities with a higher Medicaid occupancy are also most likely to close. Furthermore, our interaction of Medicaid occupancy, Medicaid reimbursement, and a time trend demonstrates that the largest increase in closure probability is for facilities with high Medicaid occupancy and low Medicaid reimbursement. These facilities are known to provide care disproportionately to the disadvantaged (i.e., nonwhite populations living in poor communities; Mor et al. 2004). As others have argued (Mor et al. 2004), policy alternatives (such as selectively increasing Medicaid vouchers, training programs for managers, and government rescues) may be needed to mitigate the decrease in the availability of nursing homes to the disadvantaged if these closures result in their not having access to services elsewhere.
Quality
We would expect lower quality facilities to close. Our results show that this may be the case. Deficiency citations issued by state/federal survey inspectors may have influenced closures. Still, the possibility exists that it may be that those nursing homes that seemed likely to close simply paid less attention to the certification survey. We are unable to ascertain the directionality of the impact of deficiency citations; however, in sensitivity analyses (not shown), using deficiency citations lagged by 2 years, closed facilities received more citations than nonclosed facilities. This provides some evidence that deficiency citations do, in fact, influence closures.
As discussed above, policies in this area have served to make this survey and certification process more uniform. However, the question still exists regarding how deficiency citations (and quality in general) influence facility closures. Policies that have led to an increase in public information on nursing homes may be the answer. Report cards, for example, may be important market forces in this area. Over the past 5 years, at least 19 states have developed state-based nursing home report cards, which allow consumers to identify the quality of care of facilities (Harrington et al. 2003). Of more importance, in November 2002, the federal nursing home report card, Nursing Home Compare, began making information on quality accessible to the public on a national scope (GAO 2002). We speculate that nursing home report cards may influence some nursing home closures but, in our analyses, we were unable to quantify this influence.
We also noted that the aggregate difference in the number of deficiency citations received between closed and nonclosed facilities is only 0.49 citations. Although statistically significant, the practical significance of this finding would seem tenuous. However, no one measure of overall nursing home quality exists and quality indicators in general are known to have orthogonal relationships (Mor 2005). Thus, deficiency citations are somewhat imprecise proxies for overall quality, and this may be reflected in our findings. Still, it is notable that consistently receiving higher than average numbers of deficiency citations (as was the case for most closed nursing homes) is important for further oversight by CMS. For example, these facilities receive additional inspections as part of the Special Focus Facility Initiative (CMS 2008).
Limitations and Suggestions for Further Research
Consistent results of the earlier research were that small facilities, low occupancy facilities, high Medicaid occupancy, and high levels of competition were associated with closure. We also found that these factors were associated with a higher likelihood of closure. However, there are some differences between our results and those of the earlier studies. Prior analyses identified for-profit ownership to be associated with closure. Our findings show the reverse, with not-for-profit facilities being more likely to close. We are unable to explain this difference.
It is possible that potentially important quality-related variables that may be associated with nursing home closure are not included in the OSCAR data. Using more detailed quality indicators, such as those available from the Minimum Data Set, may lead to a deeper understanding of the association between closure and quality (although as noted above, no one measure of overall nursing home quality exists). A further limitation of our examination of quality is that we do not explicitly disentangle the causal direction between closures and quality.
The facility-level variables that have a significant association with closure probability may reflect unmeasured underlying issues that are the true causal agents. Furthermore, we only collected information on whether a nursing home closed. We did not capture many of the fine-grained details of the closure process. For example, we do not have any information on how long a facility was under threat of closure, when a facility began relocating residents as part of the closure process, and whether some facilities under threat of closure remained in operation.
Our finding of a weakly significant increase in the association between low quality and closure suggests that increased availability of quality information might be having the desired effect of reducing the demand for low-quality facilities. Future research should examine whether this association increases more in states with more aggressive quality reporting activities such as detailed state report cards.
We suggest that occupancy rates have influenced nursing home closures. What are generically called “aging-in-place” programs may be important policy options influencing occupancy rates of nursing homes. For example, Home and Community Based Services (HCBS) Waiver Programs are notable policy options used to move elders away from institutional settings. The HCBS Waiver Program encourages states to “develop alternative options to institutional care for those in need of long-term care services” (U.S. Department of Health and Human Services 2002). In aggregate, these aging-in-place programs could lower occupancy rates for all nursing homes, which in turn may influence the profitability of all nursing homes. For some facilities, this may influence subsequent closure. However, we are unable to examine how much influence aging-in-place programs have had on nursing homes.
A further issue, yet to be examined, is the location of the closed facilities. Access may be influenced if closed nursing homes are sole providers to a community. Moreover, if nursing homes in under-served areas are more likely to close, the known disparities in nursing home care may be further worsened (Mor et al. 2004). Nursing home closures may also be influenced by management. For example, poor facility management may cause poor quality and this same poor management may be unable to keep the facility viable. Examining the role of management may also provide a productive avenue for future research.
CONCLUSION
The purpose of this research was to examine nursing home closures. This is important to understand the impact of regulation and the general state of the industry on nursing home closures. Moreover, closing facilities may have a profound influence on the lives of the current residents (Castle 2005c) and access for future residents. Policies that have likely influenced nursing home closures include Medicaid payment rates, Medicare Prospective Payment System, HCBS waivers, and report cards.
The types of facilities most likely to close include hospital-based facilities, those with a high Medicaid census, low occupancy, and/or poor quality. Most significantly, facilities with high Medicaid occupancy rates and low Medicaid reimbursement rates are most likely to close. It is important to emphasize that the associations between these characteristics and an elevated odds of closure may reflect unmeasured underlying issues rather than a causal relationship. States are actively debating on how to “redistribute” long-term care services/dollars. Some policies, such as HCBS, clearly benefit elders and facilitate their wish to avoid or delay institutionalization. However, our findings show they should be cognizant of the potential these decisions have for facilitating closure of nursing homes (and the impact on residents).
This research also suggests the need for a better understanding of the full cost of closing a facility. Past research has shown that resident relocation at the time of facility closure exacts a great cost on individual residents in terms of deterioration of health status and the need for additional assistance by family members. Our finding that closures are most likely among facilities with low quality and high Medicaid occupancy suggests that these additional costs may be imposed on residents (and family) least able to bear them. Further research should be undertaken on the differential affect of closing on residents with different economic means and support systems.
More nursing homes will likely close in the future. We do not address whether these closures should occur. In some cases, an argument could be made that closing some nursing homes may be beneficial (e.g., those of low quality), while in other cases, an argument could be made that closing other facilities may lead to disparities in care (e.g., for Medicaid residents). Thus, policy makers should be cognizant not only of the numbers of facilities that are closing but also the types of nursing homes that are closing.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: No financial support was received for this project.
Disclaimers: None
Disclosures: None.
Supporting Information
The following supporting information for this article is available online:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Allison PD. Survival Analysis Using SAS—A Practical Guide. Newbury Park, CA: SAS Press; 1995. [Google Scholar]
- Bishop CE. Where Are the Missing Elders?: The Decline in Nursing Home USE, 1985 and 1995. Health Affairs. 1999;18:146–242. doi: 10.1377/hlthaff.18.4.146. [DOI] [PubMed] [Google Scholar]
- Castle NG. Replaced by Fish: When a Nursing Home Closes What Happens to the Residents? Journal of Long-Term Care Administration. 1997 December: 10,11,24,25. [PubMed] [Google Scholar]
- Castle NG. Closure of Nursing Homes and Quality of Care. Medical Care Research and Review. 2005a;62(1):111–32. doi: 10.1177/1077558704271728. [DOI] [PubMed] [Google Scholar]
- Castle NG. Nursing Home Closures, Changes in Ownership, and Competition. Inquiry. 2005b;42(3):281–92. doi: 10.5034/inquiryjrnl_42.3.281. [DOI] [PubMed] [Google Scholar]
- Castle NG. Changes in Mental Health Status Subsequent to Nursing Home Closure. Ageing International. 2005c;30(3):262–76. [Google Scholar]
- Castle NG. Closure of Nursing Homes. Health Care Management Review. 2006;31(1):78–88. doi: 10.1097/00004010-200601000-00011. [DOI] [PubMed] [Google Scholar]
- Castle NG, Lowe T. Report Cards and Nursing Homes. Gerontologist. 2005;45(1):48–67. doi: 10.1093/geront/45.1.48. [DOI] [PubMed] [Google Scholar]
- CMS. “Action Plan for (Further Improvement of) Nursing Home Quality” [accessed on October 12, 2008]. Available at http://www.cms.hhs.gov/CertificationandComplianc/Downloads/SFFList.pdf.
- Dalton K, Howard HA. Market Entry and Exit in Long-Term Care: 1985–2000. Health Care Financing Review. 2002;24(2):17–32. [PMC free article] [PubMed] [Google Scholar]
- Fisher A, Castle NG. “Why Do Nursing Homes Close?” An Analysis of Newspaper Articles. Journal of Health and Social Policy. 2008 doi: 10.1080/19371910903182823. (in press) [DOI] [PubMed] [Google Scholar]
- General Accounting Office (GAO) Nursing Homes: HCFA Initiatives to Improve Care Are Under Way but Will Require Continued Commitment. T-HEHS-99-155. June 30, 1999.
- General Accounting Office. Nursing Homes: Public Reporting of Quality Indicators Has Merit, but National Implementation Is Premature (GAO-03-187) Washington, DC: General Accounting Office; 2002. [Google Scholar]
- Grabowski DC. Does an Increase in the Medicaid Reimbursement Rate Improve Nursing Home Quality? Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2001;56(2):S84–93. doi: 10.1093/geronb/56.2.s84. [DOI] [PubMed] [Google Scholar]
- Grabowski DC, Feng Z, Intrator O, Mor V. Recent Trends in State Nursing Home Payment Policies. Health Affairs. 2004;W4:363–73. doi: 10.1377/hlthaff.w4.363. [DOI] [PubMed] [Google Scholar]
- Harrington C, O'Meara J, Kitchener M, Simon L, Schnelle JF. Designing a Report Card for Nursing Facilities: What Information Is Needed and Why. Gerontologist. 2003;43:47–57. doi: 10.1093/geront/43.suppl_2.47. [DOI] [PubMed] [Google Scholar]
- Harrington C, Zimmerman D, Karon S, Robinson J, Beutel P. Nursing Home Staffing and Its Relationship to Deficiencies. Journal of Gerontology. 2000;55B:S278–87. doi: 10.1093/geronb/55.5.s278. [DOI] [PubMed] [Google Scholar]
- Hawes C, Phillips CC, Rose M, Holan S, Sherman M. A National Survey of Assisted Living Facilities. Gerontologist. 2003;43(6):875–82. doi: 10.1093/geront/43.6.875. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Improving the Quality of Long-Term Care. Washington, DC: National Academy Press; 2001. [Google Scholar]
- Kitchener M, Bostrom A, Harrington C. Smoke without Fire: Nursing Facility Closures in California, 1997–2001. Inquiry. 2004;41(2):189–202. doi: 10.5034/inquiryjrnl_41.2.189. [DOI] [PubMed] [Google Scholar]
- Kitchener M, O'Neill M, Harrington C. Chain Reaction: An Exploratory Study of Nursing Home Bankruptcy in California. Journal of Aging and Social Policy. 2005;17(4):19–35. doi: 10.1300/j031v17n04_02. [DOI] [PubMed] [Google Scholar]
- Konetzka RT, Norton EC, Sterns SC. Medicare Payment Changes and Nursing Home Quality: Effects on Long-Stay Residents. International Journal of Health Care Finance and Economics. 2006;6:173–89. doi: 10.1007/s10754-006-9000-9. [DOI] [PubMed] [Google Scholar]
- Mor V. Improving the Quality of Long-Term Care with Better Information. Milbank Quarterly. 2005;83:1–20. doi: 10.1111/j.1468-0009.2005.00405.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to Tiers: Socioeconomic and Racial Disparities in the Quality of Nursing Home Care. Milbank Quarterly. 2004;82(2004):1–18. doi: 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukamel DB, Spector WD, Bajorska A. Nursing Home Spending Patterns in the 1990s: The Role of Nursing Home Competition and Excess Demand. Health Services Research. 2005;40:1040–55. doi: 10.1111/j.1475-6773.2005.00394.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsoukalas T, Rudder C, Mollot RJ, Shineman M, Lee HY, Harrington C. The Collection and Use of Funds from Civil Money Penalties and Fines from Nursing Homes. Gerontologist. 2006;46:759–71. doi: 10.1093/geront/46.6.759. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. “Self-Evaluation to Promote Community Living for People with Disabilities” [accessed on August 21, 2003]. Available at http://www.hhs.gov/newfreedom/final/hhsfull.html#self. [DOI] [PubMed]
- Wiener JM, Tilly J, Alecxih LMB. Home and Community-Based Services Support Workers in Seven States. Health Care Financing Review. 2002;23(3):89–114. [PMC free article] [PubMed] [Google Scholar]
- Wood EF. Termination and Closures of Poor Quality Nursing Homes: What Are the Options? Washington, DC: Public Policy Institute, AARP; 2002. [Google Scholar]
- Zhang N, Unruh L, Wan T. Has the Medicare Prospective Payment System Led to Increased Nursing Home Efficiency? Health Services Research. 2008;43(3):1043–61. doi: 10.1111/j.1475-6773.2007.00798.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.