Abstract
OBJECTIVE
Describe U.S. trends in female stress urinary incontinence (SUI) surgery.
METHODS
National Hospital Discharge Survey (NHDS) data was analyzed for ICD-9-CM codes from 1979–2004. Age-adjusted procedure rates were calculated using 1990 census data.
RESULTS
Number of SUI surgeries increased from 48,345 in 1979 to 103,467 in 2004. In women ≥52 years, rates doubled while in women < 52 years rates decreased. Rates for Retropubic urethral suspension decreased from 1979 to 2004. Suprapubic sling procedures rates fell from a peak in 1979–2004. Rates for Other repair of urinary stress incontinence rose from 1979–2004.
CONCLUSIONS
The number of SUI surgeries in women has increased significantly from 1979 to 2004. Ambulatory procedures are not included in NHDS and no ICD-9-CM procedure code exists for midurethral sling procedures. Missed sampling of same-day procedures and non-specific coding may explain decline in suprapubic sling procedures and rise in Other repair of urinary stress incontinence.
Keywords: stress urinary incontinence, hospital discharge data, rate of stress, incontinence surgery
Introduction
Female urinary incontinence is a common, costly and burdensome condition for women in the United States. Over twelve billion dollars each year is spent treating female urinary incontinence.1 Estimated prevalence rates of urinary incontinence among women in community-dwelling populations vary, but have been reported to be as high as 25–50%.2 Stress urinary incontinence (SUI), the most common type of urinary incontinence, affects approximately 15% of the ambulatory adult population including >35% of community-living women over age 60 years in the United States.3,4 SUI can be treated by pelvic muscle strengthening, supportive devices, or surgery. When more conservative measures fail women often choose surgical treatment.
An estimated 30% of women with SUI in the U.S. choose to undergo corrective surgery.5 Previous data has shown that the rate of SUI surgery in the U.S. is increasing, with a near doubling of rates between 1979 and 1997.6 Over one-hundred surgeries have been proposed for the treatment of stress urinary incontinence.7 There are five major types of corrective procedures have been described for SUI: suburethral fascial plication, retropubic urethral suspension, needle suspension, pubovaginal sling, and periurethral bulking. Recent studies suggest that sling procedures have equal efficacy when compared with retropubic colposuspension, and slings continue to increase in popularity.8 With the introduction of the tension-free, midurethral sling in 1995, pubovaginal slings have become a common first line outpatient treatment for SUI.9 The purpose of this study was to assess trends of inpatient surgical procedures for SUI using the most recent update of the National Hospital Discharge Survey (NHDS, 1979–2004) and to examine specifically the effects of popularization of minimally invasive, mid-urethral slings, on SUI inpatient surgical procedures in the United States.
Material and Methods
Data were abstracted from the National Hospital Discharge Survey (NHDS), a federal dataset utilizing a multistate probability sampling of inpatient hospital discharges in the United States. Medical records from 466 non-federal short-stay hospitals (8% of all U.S. hospitals) were selected by systematic random sample and approximately 270,000 discharges were collected per year from January 1979 to December 2004, the current publicly available time period. The survey recorded up to seven discharge diagnosis codes and four procedure codes, using the International Classification of Diseases, 9th review, Clinical Modification (ICD-9-CM) coding system. Other de-identified information collected included patient sex, age, race, marital status, length of hospital stay, hospital size (number of beds), hospital ownership and insurance type or expected source of payment. Within the identified study population, data regarding medical comorbidities, incontinence diagnoses, concomitant surgical procedures, surgical complications, and deaths were recorded. Quality control programs have estimated the error rate for the NHDS at 4.3% for medical coding and data entry, and 1.4% for demographic coding and data entry.10
After obtaining University of Pittsburgh, Institutional Review Board approval - Exempt status, women who underwent surgical correction of incontinence from 1979 to 2004 were identified using the ICD-9-CM codes outlined in Table 1. All women undergoing one or more of these procedures were included in the analysis. These tabulated surgical procedure numbers were then inflated to national averages using specifically designated hospital weights, which are included in the federal dataset for each patient discharge. Age-adjusted rates of procedures per 1000 women were calculated by the direct method of rate adjustment, using the 1990 projected United States Census population data for each year of age. Data were stratified by patient age <52 years old or ≥52 years old, a division chosen based on average age of menopause in the U.S. When the estimated number of cases per year was based on fewer than 60 records in the database, the estimate was considered unreliable.
Table 1.
Stress Incontinence ICD-9-CM Procedure Codes
| Code | Procedure |
|---|---|
| 57.85 | Cystourethroplasty |
| 57.89 | Other repair of bladder |
| 59.3 | Plication of urethrovesical junction |
| 59.4 | Suprapubic sling operation |
| 59.5 | Retropubic urethral suspension |
| 59.6 | Paraurethral suspension |
| 59.7 | Other repair of urinary stress incontinence |
| 59.71 | Levator muscle operation for urethrovesical junction |
| 59.72 | Injection of implant into urethra and/or bladder neck |
| 59.79 | Other |
| --anterior urethropexy, Tudor urethropexy, repair of stress incontinence NOS |
The linear test of trend was used to assess trends in the age-adjusted rates of procedures from 1979 to 2004. Statistical analysis was performed using SPSS Version 15.0 software (SPSS Inc., Chicago, Illinois, USA). P value <0.05 was considered statistically significant.
Results
According to NHDS data, approximately 2,064,940 stress urinary incontinence inpatient procedures were performed in the United States from 1979 to 2004. The number of women undergoing SUI procedures has increased from 48,345 in 1979 to 103,467 in 2004. Age-adjusted rates of SUI surgery per 1000 women also increased from 0.59 in 1979 to 0.85 in 2004 (Figure 1). However, analysis by age-stratification revealed a more than doubling of the age-adjusted rate for women ≥52 years, 0.64 to 1.60, while in women <52 years of age, the age-adjusted rate declined from 0.57 to 0.47 (Figure 2). Using the test for linear trend, rates of incontinence procedures increased by 1.4% per year (p<0.001) overall and by 4.4% per year (p<0.001) in women ≥52 years during the study time period. In women <52 years there was no significant trend in rates across time.
Figure 1.
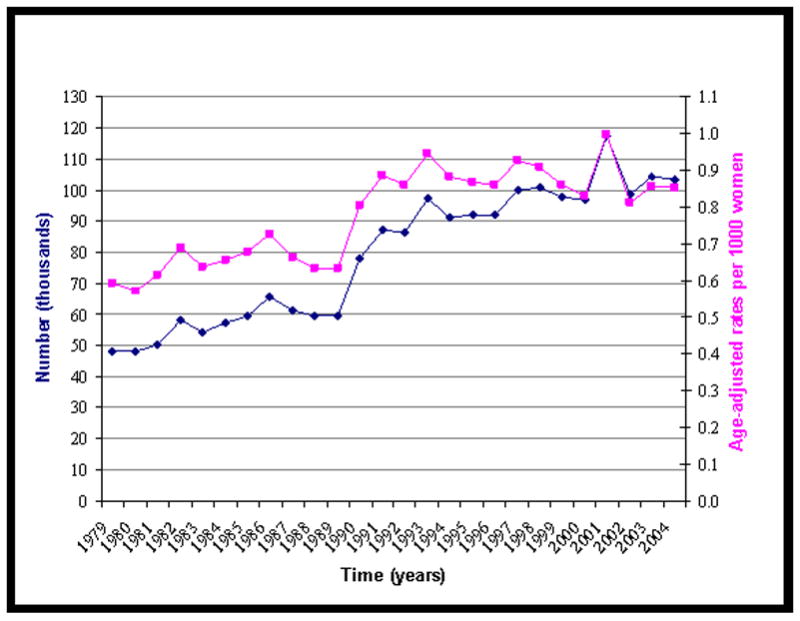
Estimated number of women undergoing incontinence procedures and age-adjusted rates of incontinence procedures per 1000 women from 1979 to 2004 in the United States
Figure 2.
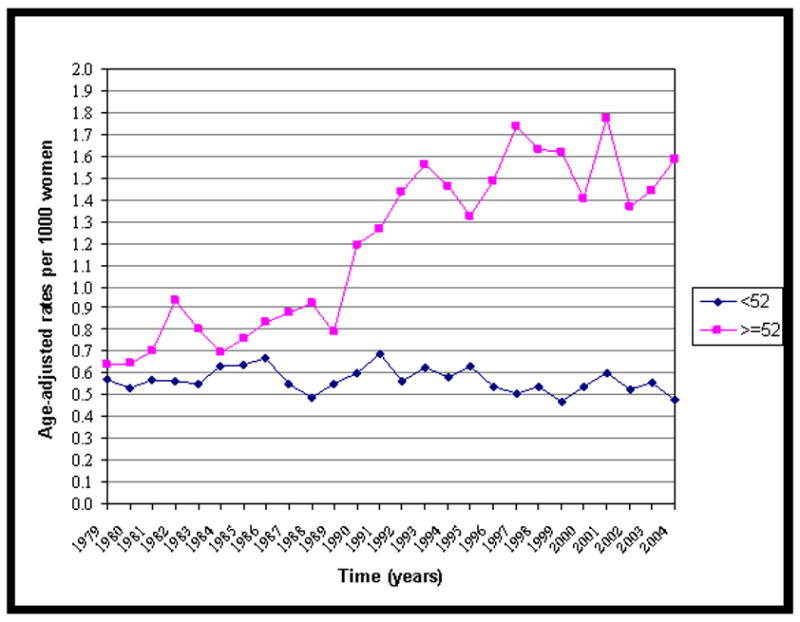
Age-adjusted rates of incontinence procedures per 1000 women from 1979 to 2004 in the United States, stratified by patient age
The mean age of women undergoing SUI procedures in this study was 54 (SD +/− 13.7), with the mean age increasing from 50 to 58 over the twenty-six year time period studied. Seventy-five percent of these women were caucasian, 3% black and 22% other or not stated. Geographical distribution of procedures revealed the largest number of procedures were performed in the Midwest and the South. In 1979 approximately 75% of women undergoing SUI procedures were privately insured, while in 2004 just over half held private insurance. A considerable decrease in length of inpatient hospitalization was observed, with an average stay of 10.5 days in 1979, falling to only 2.3 days in 2004. Detailed demographic data is presented in Table 2.
Table 2.
Demographic Data
| 1979 | 1991 | 2004 | |
|---|---|---|---|
| Age (y) | 50.1±12.2 | 52.6±13.9 | 57.5±13.9 |
| Race (%) | |||
| White | 75.9 | 76.0 | 66.9 |
| African American | 6.6 | 3.3 | 2.2 |
| Other | 17.5 | 20.7 | 30.9 |
| Insurance (%) | |||
| Private | 74.6 | 59.1 | 55.7 |
| Government | 22.5 | 30.4 | 40.9 |
| Other | 2.9 | 10.5 | 3.4 |
| Geographic region (%) | |||
| South | 31.9 | 38.4 | 41.1 |
| Midwest | 36.8 | 31.2 | 24.7 |
| West | 18.8 | 21.8 | 24.2 |
| Northeast | 12.5 | 8.6 | 10 |
| Hospital size (%) | |||
| <100 beds | 12.5 | 19.4 | 17.7 |
| 100–199 beds | 22.3 | 29.3 | 28.7 |
| 200–299 beds | 25.0 | 15.7 | 22.2 |
| 300–499 beds | 22.5 | 28.8 | 17.3 |
| >500 beds | 17.7 | 6.8 | 14.1 |
| Hospital stay (d) | 10.5±4.9 | 4.4±2.2 | 2.3±2.4 |
Retropubic urethral suspension procedures (ICD-9-CM 59.5) decreased over the study time period, from over 30,000 performed in 1979 to less than 17,000 in 2004. The age-adjusted rates for this procedure fell from 0.37 per 1000 women in 1979 to 0.14 per 1000 in 2004. (see Figure 3). Rates of retropubic urethral suspension procedures decreased by 0.08% (p<0.001) per year between 1979 and 2004. Suburethral sling procedures (ICD-9-CM 59.4) increased from 1,591 in 1979 to a peak of 10,212 in 1997, then fell to 4,314 in 2004. Analysis of age-adjusted rates for slings per 1000 women shows a similar trend, rising from 0.02 in 1979 to a peak of 0.10 in 1997, then falling to 0.03 in 2004 (see Figure 4). Suburethral slings increased by 0.01% (p=.022) per year during the study years. Many women underwent procedures coded as other repair of urinary stress incontinence (ICD-9-CM 59.79), recorded as 5,000 women in 1979 and rising to over 77,000 women in 2004. Age-adjusted rates for other repair of urinary stress incontinence also increased steadily from 0.06 in 1979 to 0.64 in 2004 (see Figure 5). Rates of other repair of urinary stress incontinence increased by 2.3% (p<0.001) per year in the study. Fewer women underwent other repair of bladder (ICD-9-CM 57.89), with 7,483 procedures coded in 1979, peaking at 10,910 in 1986, and falling to just 1,637 in 2004. The age-adjusted rates for other repair of bladder also declined from 0.10 per 1000 women in 1979 to 0.01 in 2004. Other repair of bladder procedures declined by 0.03% (p<0.001) per year in the study time period.
Figure 3.
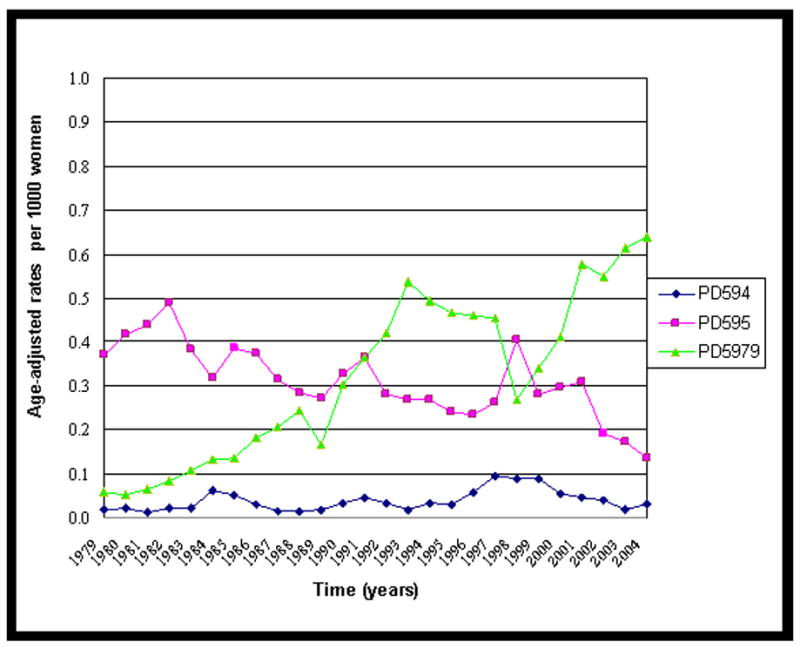
Age-adjusted rates of Retropubic urethral suspension (ICD-9-CM 59.5) per 1000 women from 1979 to 2004 in the United States
For other incontinence procedures identified in this study, numbers were small, making interpretation of trends over time difficult. Rates of cystourethroplasty (ICD-9-CM 57.85) fell from 3,609 in 1979 to just 859 in 2004. For plication of the urethrovesical junction (ICD-9-CM 59.3), rates vacilated with 1,951 performed in 1979, a peak of 4,756 in 1999, and decreasing to 1,211 in 2004. Numbers for paraurethral suspension (ICD-9-CM 59.6) varied across years, with a maximum of 4,356 performed in 1993 and a low of 203 in 1983. Levator muscle operation for urethrovesical junction (ICD-9-CM 59.71) rates ranged from a low of 76 in 1988 to a peak of 4,224 in 1998. Finally, injection of implant into urethra and/or bladder neck (ICD-9-CM 59.72) had no recorded cases until 1996, when 321 were coded, rising to 981 cases in 2004. Each of these less frequently performed procedures had less than 50,000 total recorded cases within the study time period.
Analysis of diagnostic codes revealed that 81% of women undergoing stress urinary incontinence procedures were coded with the diagnosis of stress urinary incontinence (ICD-9-CM 625.6), with 3% coded as mixed incontinence (ICD-9-CM 788.33), and less than 1% coded as urge incontinence (ICD-9-CM 788.31). Intrinsic spincter deficiency (ICD-9-CM 599.82), urethral hypermobility (ICD-9-CM 599.81), and nonspecific urinary incontinence (ICD-9-CM 788.30) were each recorded in 2% of the study population. The diagnosis of pelvic organ prolapse (ICD-9-CM 618) was present in 5% of women. Concomitant procedures were frequent with 14% of women undergoing cystoscopy, 31% undergoing hysterectomy, and 34% undergoing prolapse surgery at the time of incontinence surgery.
Thirty-five percent of women had one or more comorbid conditions at time of surgery, with the most common being cardiovascular disease (16%), malignancy (16%), and pulmonary disease (5%). The overall index hospitalization complication rate was 20%. See Table 3 for a detailed description of complications. One percent of women were discharged to a short or long term care facility. Only 1027 inpatient deaths occurred among the women in this study.
Table 3.
Complications: ICD-9-CM Diagnosis Codes
| Complication | ICD-9-CM code(s) | Number | % |
|---|---|---|---|
| Any Complication | 417,156 | 20.20 | |
| Catheter related infection | 996.64 | 127,278 | 6.16 |
| Uterine/Vaginal inflammation | 615–616 | 126,879 | 6.14 |
| Anemia | 285.1, 280.0 | 78,517 | 3.80 |
| Urinary tract | |||
| infection/cystitis/pyelonephritis | 599.0, 595, 590.1 | 71,084 | 3.44 |
| Urinary retention | 788.2 | 51,377 | 2.49 |
| Urinary Complications | 997.5 | 44,155 | 2.14 |
| Fever | 780.6 | 13,758 | 1.49 |
| Accidental puncture, procedure related | 998.2 | 29,209 | 1.42 |
| Digestive system complication | 997.4 | 24,533 | 1.19 |
Comment
The most important finding of this study is that frequency of surgical procedures for stress urinary incontinence increased dramatically from 1979 to 2004, demonstrated by increasing overall and age-adjusted rates. The most remarkable increase was seen in the population of women age ≥52 years. This trend in increasing age of women was also demonstrated by increase in mean age from 50 years to 58 years during the study timeframe. Increasing surgical rates in older women likely reflects both an aging population and an increase in women seeking care for incontinence. U.S. Census estimates predict that by 2030 approximately 20% of the population will be ≥65 years old, with women comprising a disproportionate part of this older cohort.11 Luber, et. al estimates that the number of women seeking care for pelvic floor disorders will increase dramatically by 2030. 11 With advancing age, presence and number of medical co-morbidities are more common, and can be a factor in planning treatment for SUI. In this study, 35% of women had one or more coexisting medical problems at the time of surgery. Advances in anesthesia and minimally invasive procedures have improved the safety of performing surgery in an older, medically complex population. This aging population will likely comprise a growing portion of the incontinence surgical population. Minimally invasive procedures, such as the midurethral sling which can be performed using intravenous sedation with local analgesia, spinal anesthesia, or general anesthesia, allows reconstructive surgery to be performed more safely in patients with medical comorbidities.
As data continue to support the efficacy and safety of midurethral slings, the popularity of these procedures will probably continue to increase. Since no ICD-9-CM procedure code currently exists specifically for midurethral slings, these procedures appear to be currently coded as Other repair of stress urinary incontinence (ICD-9-CM 59.79), which may explain the increase in coding for 59.79 seen in this study. The relative decline in the more traditional suburethral sling procedure (ICD-9-CM 59.4) and retropubic urethral suspension (ICD-9-CM 59.5), is likely due to increase in use of midurethral slings, replacing these traditional procedures. In order to more accurately capture surgical data, either ICD-9-CM coding software utilized by most hospitals should be reformatted to direct hospital coders to list the midurethral sling as a pubovaginal sling (ICD-9-CM 59.4) or a code specific for midurethral sling operations should be adopted for use in hospital discharge coding.
There are several potential weaknesses to this study. These data are based on cross-sectional sampling, and therefore rely both on accuracy of coding and generalizability of the sampling. As addressed above, the NHDS data have been shown to have reasonable coding accuracy. We chose U.S. Census data from 1990, a time point midway through the study, to calculate the age-adjusted rates. Census data from 1990 may not have accurately reflected year to year population change; however data from a single year was needed to base and compare age-adjusted rates across the entire 26 year time span of the study. Additionally, this study likely underestimates the number of incontinence procedures as the NHDS excluded federal, military and Veteran’s Affairs hospitals and collects no data from same-day surgeries or ambulatory surgical centers. Strengths of this study include a large sample size, well defined inclusion criteria, and standardized use of diagnosis and procedure codes.
The lack of data on same-day surgeries will continue to affect the accuracy of estimates using NHDS data, as incontinence procedures will likely be performed increasingly on an outpatient basis. The National Survey of Ambulatory Surgery (NSAS), a federal database similar to the NHDS, collected data on ambulatory surgical procedures from 1994 to 1996. During this three year period the NSAS estimated that approximately 52,000 urinary incontinence surgeries were performed on an outpatient basis.12 Following introduction of midurethral slings in 1995, the rate of outpatient incontinence surgery would be expected to have increased. The NSAS was reinstituted during 2006 and this data, once released, will be useful to assess more current outpatient incontinence surgery rates. Continued ambulatory surgical data collection is needed to accurately assess future surgical trends.
Acknowledgments
This publication was made possible by Grant Number UL1 RR024153 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. Information on NCRR is available at http://www.ncrr.nih.gov/.
Footnotes
Presentation: Accepted for poster presentation; 29th Annual American Urogynecologic Society Scientific Meeting. Chicago, IL, Sept 4–6, 2008.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Wilson L, Brown J, Shin G, Kim-Oanh L, Subak L. Annual direct cost of urinary incontinence. Obstet Gynecol. 2001 Sep;98(3):398–406. doi: 10.1016/s0029-7844(01)01464-8. [DOI] [PubMed] [Google Scholar]
- 2.Cheater FM, Castleden CM. Epidemiology and classification of urinary incontinence. Ballillieres Clin Obstet Gynecol. 2000;14:183–205. doi: 10.1053/beog.1999.0071. [DOI] [PubMed] [Google Scholar]
- 3.Fantl JA, Wyamn JF, McClish DK, et al. Efficacy of bladder training in older women with urinary incontinence. JAMA. 1991;265:609–13. [PubMed] [Google Scholar]
- 4.Cutner A, Cardozo L. Urinary incontinence: clinical findings. Practitioner. 1990;234:1018. [PubMed] [Google Scholar]
- 5.Kinchen K, Long S, Orsini L, Crown W, Bump R. Healthcare utilization among women who undergo surgery for stress urinary incontinence. Int Urogynecol J. 2004;15:154–9. doi: 10.1007/s00192-004-1133-0. [DOI] [PubMed] [Google Scholar]
- 6.Boyles S, Weber A, Meyn L. Procedures for urinary incontinence in the United States, 1979–1997. Am J Obstet Gynecol. 2003;189:70–5. doi: 10.1067/mob.2003.376. [DOI] [PubMed] [Google Scholar]
- 7.Keane D, Eckford S, Abrams P. Surgical treatment and complications of urinary incontinence. Curr Opin Ostet Gynecol. 1992;4(4):559–64. [PubMed] [Google Scholar]
- 8.Albo M, Richter H, Brubaker L, Norton P, Kraus S, Zimmern P, et al. Burch colposuspension versus fascial sling to reduce urinary stress incontinence. N Engl J Med. 2007;356(21):2143–55. doi: 10.1056/NEJMoa070416. [DOI] [PubMed] [Google Scholar]
- 9.Ulmsten U, Petros P. Intravaginal slingplasty (IVS): An ambulatory surgical procedure for treatment of female urinary incontinence. Scand J Urol Neprol. 1995;29:75–82. doi: 10.3109/00365599509180543. [DOI] [PubMed] [Google Scholar]
- 10.Dennison C, Pokras R. Design and operation of the National Hospital Discharge Survey: 1988 redesign. Vital Health Stat. 2000;1(39) [PubMed] [Google Scholar]
- 11.Luber KM, Boero SB, Choe JY. The demographics of pelvic floor disorders: Current observations and future projections. Am J Obstet Gynecol. 2001;184(7):1496–1503. doi: 10.1067/mob.2001.114868. [DOI] [PubMed] [Google Scholar]
- 12.Boyles S, Weber A, Meyn L. Ambulatory procedures for urinary incontinence in the United States, 1994–1996. Am J Obstet Gynecol. 2004;190:33–6. doi: 10.1016/j.ajog.2003.07.007. [DOI] [PubMed] [Google Scholar]


