Abstract
Background:
Nowadays, there is increasing awareness about the frequent chronic comorbidities in patients with chronic obstructive pulmonary disease (COPD) but little information is available to quantify the burden of illness that these conditions cause in this population. We aimed to identify and describe a population suffering from COPD highlighting the co-morbid conditions that may contribute to poor clinical outcomes.
Design:
Epidemiological cross-sectional study conducted using administrative heath services databases.
Results:
A cohort of 126,283 COPD patients was identified. The estimated prevalence in adult population was 3.6%. Ninety-eight percent of these patients (123,603) received at least one prescription of “non-respiratory drugs” and, considering chronic specific comorbidities (cardiovascular disease, diabetes and depression) 86,351 patients (68.4% of COPD patients) suffered from at least one of these conditions. 80,840 pts (64.4%) were treated for cardiovascular diseases, 17,091 subjects for diabetes (12.4%) and 10,292 for depression (8%). About 16% of COPD subjects (19,168 patients) had two out of the three considered comorbid conditions and 1352 patients (1.1%) all three.
Conclusion:
This study highlights the complex spectrum of comorbidities in COPD patients. The prevalence of main chronic diseases increases with age, in particular among female group. An enhanced public awareness about these conditions is necessary, just as a more comprehensive approach in their management.
Keywords: COPD, administrative database, prevalence, comorbidity
Introduction
Nowadays, chronic obstructive pulmonary disease (COPD) is considered a major cause of morbidity and mortality worldwide. In contrast to the trend for cardiovascular diseases, cancer and stroke, death rates from COPD have been rising steadily over the last decade (Hurd et al 2005) and, according to estimates of the World Health Organization (WHO), by 2020 this condition shall become the third most frequent cause of death, following coronary and cerebrovascular disease (Murray et al 1997).
Although these figures on COPD morbidity and mortality are alarming, they are only a “tip of the iceberg” because COPD is often part of a much more complex profile of comorbidities (Hansell et al 2003).
Over the last few years, there has been an increased awareness about the systemic nature of COPD (Augusti 2005; Shapiro et al 2005) and the frequent and important chronic comorbidities that may contribute significantly to its severity and mortality (van Manen et al 2001; Boyd et al 2005; Sin and Man 2005a; Soriano et al 2005), and that might be affected by treatment (Liao 2005; Sin and Man 2005b).
Several studies suggest that cardiovascular diseases (CVD) are more frequent in COPD patients than in the general population and may represent a burden greater than that of lung disease itself (Burney et al 2003; Holguin et al 2005; Huiart et al 2005). Moreover, Antonelli and colleagues documented that in the presence of ischemic heart diseases CVD becomes an important factor, predicting all-cause mortality on COPD patients (Antonelli et al 1997).
In addition, among COPD comorbidity, depression deserves particular attention. COPD (especially at severe levels) leads to impairments in activities of daily living, social and psychological functioning and recreational activities. Depression has been found to occur in 7%–42% of COPD patients up to four times more frequently than in subjects without COPD (Kunik et al 2005).
These observations highlight the fragmentary nature of available information, and at the same time the importance of studying COPD comprehensively, considering often-associated concomitant conditions and quantifying the burden of illness that these conditions cause in this population.
With this study we intend to identify a population suffering from COPD, assessing COPD prevalence in a large sample of Italian population (about 8 millions of inhabitants) and describing the general profile of COPD patients, in whom comorbidity plays an important role.
Methods
This is an epidemiological cross-sectional study, conducted using administrative heath services databases from 22 Italian Local Health Units (LHU) participating in the ARNO project (Clavenna et al 2003). The population comprised 7,731,628 inhabitants. The observation was carried out between January 1st and December 31st, 2004.
Data sources
This study used the outpatients’ prescriptions database (PD) of drugs totally or partially reimbursed by the National Health System (NHS), and the Civil Registry Database (CRD), in each LHU.
These databases have been extensively used for epidemiological studies including drug-exposure and chronic disease (Clavenna et al 2003; Anecchino et al 2005) as well as to study population-based health outcomes (Monte, Fanizza, et al 2006; Monte, Macchia, et al 2006). Besides, the use of this source limits bias selection as these databases cover the whole population. 69% of residents were eligible for outpatient prescription drug benefits.
All databases are managed by the Consorzio Interuniversitario CINECA.
Cohort definition
COPD cohort was identified using the following criteria:
Age of 45 years or above;
Chronic treatment with drugs for obstructive pulmonary diseases (inhaled/oral bronchodilators, inhaled steroids or fixed-dose combinations) (index drugs).
Chronicity was defined linking the number of prescribed packages and the duration of therapy, defined in terms of time from first to last prescription of the index drug. Patients who received more than five boxes of the index drug for over 3 months or more were considered chronically treated.
A treatment with antibiotics and/or oral steroids was assumed as an indicator of disease exacerbations.
To assess the presence of comorbidities, the prescriptions of drugs different from those for COPD were analysed. In particular, we focused on three drugs classes identifying specific co-morbidities: diabetes (insulin, insulin analogues and oral hypoglycaemic therapy), cardiovascular diseases (any cardiovascular drug) and depression (selective serotonin reuptake inhibitors, monoamine oxidase inhibitors, monoamine uptake inhibitors).
Treatment chronicity was explored for cardiovascular and antidepressant drugs, assuming as chronic any treatment with more than three boxes over 3 or more months.
Statistical analysis
We used descriptive statistics to examine the epidemiological and therapeutic characteristics of our sample. Prevalence of estimated COPD was defined as the number of patients receiving one or more COPD index drugs per 100 individuals in the population. Prevalence rates, as well as percentages of patients with comorbidities have been stratified by age and gender.
Results
Among the population examined of 7,731,628 NHS users, 3,535,371 (46%) were of 45 years and over. Of these, 462,894 (13%) patients were exposed to at least one respiratory agent (COPD index drug). The composition of these two populations is reported in Table 1.
Table 1.
General description of the examined population
| Population (≥45 years) | Patients exposed to ≥1 respiratory drugs | |||
|---|---|---|---|---|
| Gender | N pts | % | N pts | % |
| Male | 1,603,364 | 45 | 205,711 | 44 |
| Female | 1,932,007 | 55 | 257,183 | 56 |
| Age | ||||
| 45–64 | 1,965,547 | 56 | 207,721 | 45 |
| 65–74 | 810,721 | 23 | 128,398 | 28 |
| 75–84 | 571,129 | 16 | 99,174 | 21 |
| ≥85 | 187,974 | 5 | 27,601 | 6 |
| Total | 3,535,371 | 100 | 462,894 | 100 |
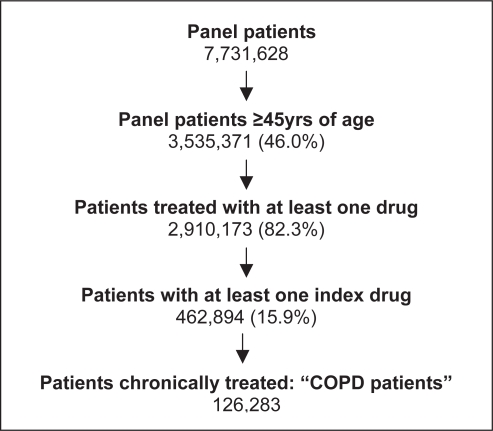
On the basis of the criteria above described and the flow-chart represented in Figure 1, a cohort of 126,283 COPD patients was identified.
Figure 1.
Flowchart of COPD patients’ identification.
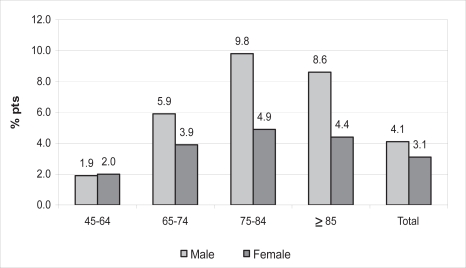
The prevalence of COPD in our adult population (≥45 years) was 3.6% and it increased greatly with age (1.9% in the age group 45–64, 4.8% in 65–74, 6.8% in 75–84 and 5.6% in ≥85 years). COPD appeared more common in males than in females (4.1% in males and 3.1% in females). This difference was particularly evident in the age group 75–84 years, while in the youngest there was no gender difference (Figure 2).
Figure 2.
Prevalence estimated (%) of COPD in subgroups of patients differentiated in age and gender.
Main characteristics of the patients
Table 2 reports the main characteristics of COPD patients including pharmacological treatment and general clinical profile.
Table 2.
Main characteristics of COPD patients
| Characteristics | N pts (126,283) | % |
|---|---|---|
| Gender | ||
| male | 65,869 | 52.2 |
| female | 60,414 | 47.8 |
| Age, yrs | ||
| 45–64 | 38,022 | 30.1 |
| 65–74 | 38,775 | 30.7 |
| 75–84 | 38,929 | 30.8 |
| ≥85 | 10,557 | 8.4 |
| Therapy with index drug | ||
| mono-therapy | 25,778 | 20.4 |
| poly-therapy | 100,505 | 79.6 |
| Antibiotic agent – oral steroid prescription | ||
| yes | 100,430 | 79.5 |
| Non-index drug prescription | ||
| yes | 123,603 | 97.9 |
| Specific comorbid condition | ||
| yes | 86,351 | 68.4 |
The cohort with COPD was older than the reference population (see Table 1). Almost 70% of the patients (88,261) were 65 or older, including 8% ≥85 years. The mean age was 70 years. Fifty-two percent (65,869) were male.
A high proportion of patients (80%) received a poly-therapy as COPD treatment, and, in particular, 67,822 patients (54%) received more than three different drugs.
Likewise, about 80% (100,430 patients) were treated with drugs indicating exacerbations. Antibiotic treatment (with or without oral corticosteroids) was the most common: three fourths of the patients (94,869) were prescribed these drugs.
Comorbidities therapy
Ninety-eight percent of COPD patients (123,603) received at least one prescription of “non-respiratory drugs”; the main therapeutic classes used are presented in Table 3. These data highlight the clinical complexity of the COPD population, highly exposed to different pharmacological agents, from antibiotic or cardiovascular drugs (more than 70%) to nervous system agents (24%).
Table 3.
Main therapeutic classes prescribed to COPD patients
| Therapeutic class | Patients | % of COPD pts |
|---|---|---|
| Antibiotic agents | 95,845 | 75.9 |
| Cardiovascular drugs | 92,367 | 73.1 |
| Gastrointestinal and metabolic disorders | 75,303 | 59.6 |
| Musculoskeletal system | 71,384 | 56.5 |
| Blood and lymphatic system | 55,922 | 44.3 |
| Endocrine system | 53,692 | 42.5 |
| Nervous system | 30,248 | 24.0 |
Considering specific comorbid conditions such as cardiovascular disease, diabetes and depression and applying the chronicity criteria for therapy quoted above (see Method section), 86,351 patients (68.4% of COPD patients) suffered from at least one of these conditions.
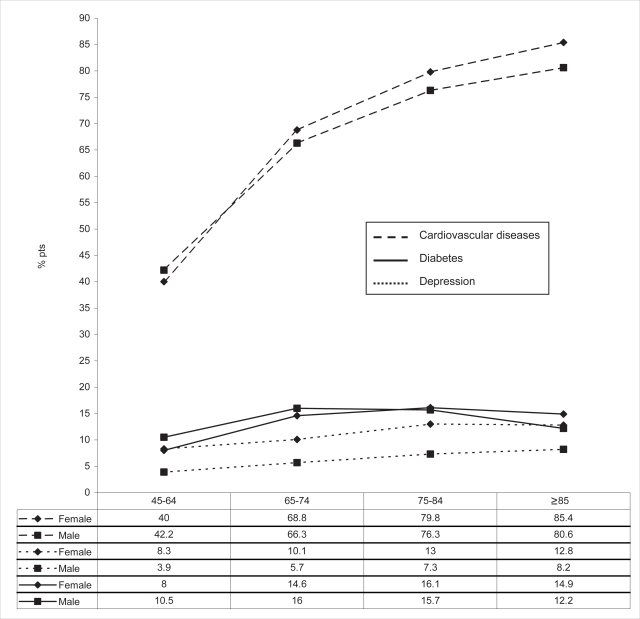
Cardiovascular diseases, as expected in these age groups, were the most common condition coexisting in COPD patients (80,840 pts, 64.4%). 17,091 subjects were treated for diabetes (12.4% of COPD patients) and 10,292 for depression (8%). The percentage of patients suffering from these conditions increased with age (Figure 3).
Figure 3.
Percentage of COPD patients with comorbid conditions: diabetes, depression and cardiovascular diseases in subgroup of patients differentiated in sex and age.
This is particularly evident for cardiovascular diseases (about 40% in the age group 45–64 and over 80% in those ≥85 years); the same is true also for depression (6.2% among patients 45–64 years old and 10.8% among those ≥85 years) (Figure 3). Although overall depression was more common in females than in males (5.9% in males and 10.6% in females), the increase with age was more marked among male patients (from 3.9% to 8.2% in male vs from 8.3% to 12.8 in female) (Figure 3). A less remarkable increase was observed for diabetes (9.2% in the age group 45–64 and 13.7% in ≥85 years) without important gender differences (Figure 3). Interestingly, about 16% of COPD subjects (19,168 patients) had two out of the three considered comorbid conditions and 1352 patients (1.1%) all three. The details of the different combinations are reported in Table 4.
Table 4.
Detail of chronic comorbidities in COPD patients
| Comorbidities | N pts | % of COPD pts |
|---|---|---|
| – Only one | 65,831 | 52.1 |
| Cardiovascular diseases (CV) | 60,500 | 47.9 |
| Diabetes | 2,711 | 2.1 |
| Depression | 2,620 | 2.1 |
| –Two | 19,168 | 15.2 |
| Diabetes + CV | 12,848 | 10.2 |
| CV + Depression | 6,140 | 4.9 |
| Diabetes + Depression | 180 | 0.1 |
| –Three | 1,352 | 1.1 |
| Diabetes + CV + Depression | 1,352 | 1.1 |
| Total | 86,351 | 68.4 |
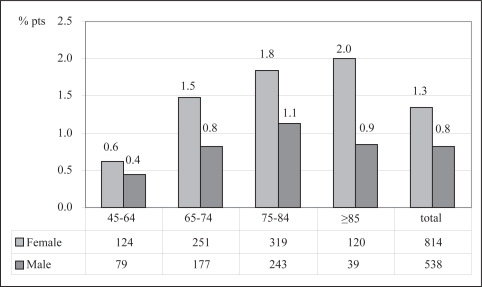
These data document that about twenty thousand patients with impaired pulmonary function had a high risk profile for the spectrum of comorbid diseases. The percentage of patients with the most complex profile (all three diseases considered) indeed increased with age (0.5% of COPD patients 45–64 years old, 1.1% of 65–74, 1.4% of 75–84 and 1.5% of patients ≥85 years). This increase was particularly evident in the female population (from 0.6% in younger patients to 2.0% in older ones) (Figure 4).
Figure 4.
Percentage of COPD patients with all three pathologies (diabetes, depression, cardiovascular diseases) in subgroups of patients differentiated in age and gender.
Discussion
The first and very important result of our study was the size of the sample identified, 126,283 COPD patients, that was higher than any published COPD epidemiological studies (Halbert et al 2003), allowing the quantification of the burden of COPD in the community setting, through an appraisal of the “real dimension” of the problem.
This wide sample of COPD patients, identified through a different methodology respect to the most recent surveys (Kim et al 2005; Menezes et al 2005), made possible to have numerically significant subgroups, generally excluded in randomized clinical trials and not particularly represented in surveys: specifically, elderly subjects (up to 11,000 patients older than 85 years), patients with multiple comorbidities (almost 20,000 patients chronically treated for at least two comorbid conditions); elderly females with very complex profile (814 patients with the three comorbidities considered).
These results are in agreement with the recent recommendations (Curkendall et al 2006; Fabbri et al 2006) advocating efforts to characterize the spectrum of comorbid diseases and to develop a more comprehensive approach both in the study and in the management of COPD patients. In fact, despite the advances in the care of individuals with COPD, some uncertainty remains about how best to manage patients, particularly elderly, with different chronic diseases. The information is limited and available studies tend to exclude patients with complex comorbidity (Boyd et al 2005; Fabbri et al 2006).
In our population we found that nearly all (98%) received other drugs besides respiratory agents. Antibiotic agents were the most common owing to the frequent bacterial infections occurring in these patients, but the high exposure to cardiovascular, anti-inflammatory, gastrointestinal agents highlights the frequent presence of different diseases in the same patient.
Our study has, however, some limitations. Administrative databases lack clinical and diagnostic information. We identified COPD patients and comorbidities only by prescription patterns and the distinction between COPD and asthma is difficult in this context.
We limited misdiagnosis by including only subjects 45 years or older and requiring more than occasional treatment. Misdiagnosis, therefore, certainly exists in our study but likely represents only a small portion of examined population.
Another limitation is that COPD may be under-diagnosed and therefore under-treated (Price et al 2003). Symptomatic and more severe patients are more likely to be chronically treated. Although the use of a general population protects from selection bias, our cohort likely comprised mostly patients with clear COPD, since we considered only intensive drug exposure (about 80% of patients received two or more index drugs).
In people aged 45 years and older, we measured a COPD prevalence of 3.6%. These estimates could seem to be lower than those obtained in other population-based studies of COPD.
In Italy, Viegi and colleagues measured respectively a general COPD prevalence of 12.2%, 57.0% and 28.7% using three different COPD definitions (ERS, ATS and clinical) (Viegi et al 2000). However, this study included patients of every severity stage. Considering only moderate/severe COPD, the Viegi study rates result very similar to our data: 3.6%, 5.2% and 4.4% respectively.
Our estimate is also lower than the range of 4%–10% derived from an international review of COPD prevalence (Halbert et al 2003), and than prevalence reported in the other European studies. In Greek people older than 35 years, Tzanakis reported a prevalence of 8.4% (Tzanakis et al 2004); in IBERPOC, a multicenter survey in Spain (Pena et al 2000), the prevalence was 13.1% for men and 10.5% for women. The explanation of these differences lies in the variety of criteria used to define COPD.
The data available come from studies ad hoc with actively screened patients (using diagnostic methods, like spirometry), while our data derive from an analysis of treatment specifically of chronically treated patients.
If we apply less strict criteria, excluding chronicity or considering only older patients, our prevalence estimates increase and become very close to literature estimates (see Table 1).
With respect to specific chronic comorbidities such as diabetes and cardiovascular diseases, our data are in perfect agreement with the literature. A recent study using administrative databases and identifying COPD patients according to our criteria, found a diabetes prevalence of 14.5% (Curkendall et al 2006); Gudmundsson and colleagues (Gudmundsson et al 2006) reported a prevalence of 10.6% and 65% for diabetes and cardiovascular disease respectively.
On the contrary, our results on depression are difficult to compare because of the wide variability in the available prevalence estimates (up to 42% in moderate to severe COPD, Yohannis et al 2000; Kunik et al 2005), even if van Manen et al who investigated prevalence of comorbidity in patients with COPD over 40 years of age (van Manen et al 2001), found a depression prevalence of 8.7%, very similar to our data.
In summary, this study, besides confirming previous evidence, documents that COPD is a health problem also in Italy and that public awareness of its burden is important. From a broader perspective, it highlights the complex spectrum of comorbidities in COPD patients, underlining the importance of a comprehensive approach in their management. Redelmeier and colleagues demonstrated that when the central focus of care is a serious condition, the care for other chronic disorders is compromised (Redelmeier et al 1998). This could be a real problem considering the high frequency of chronic comorbidities that may drastically worsen COPD severity and mortality and of complex elderly patients, whose management is still uncertain (Fabbri et al 2006).
In conclusion, we think that comorbidities should be considered when estimating the social and economic burden of disease and we hope that our results will increase the attention and the initiatives on COPD, possibly in agreement with more general actions on respiratory illness (WHO 2006) and chronic diseases (Epping-Jordan et al 2006).
Acknowledgments
The authors thank Mersia Mirandola for her technical assistance in data management.
Footnotes
Conflict of interest
We declare that we have no conflict of interest.
References
- Anecchino C, Fanizza C, Romero M. Lo studio della BPCO come modello di analisi dei database amministrativi. Giornale Italiano di Farmacia Clinica. 2005;19(2):70–6. [Google Scholar]
- Antonelli I, Fuso L, De Rosa M, et al. Co-morbidity contributes to predict mortality of patients with chronic obstructive pulmonary disease. Eur Respir J. 1997;10:2794–800. doi: 10.1183/09031936.97.10122794. [DOI] [PubMed] [Google Scholar]
- Augusti AG. Systemic effects of chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2005;2:367–70. doi: 10.1513/pats.200504-026SR. [DOI] [PubMed] [Google Scholar]
- Black N, Payne M. Improving the use of clinical databases. BMJ. 2002;324:1194. doi: 10.1136/bmj.324.7347.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd CM, Darer J, Boult C, et al. Clinical practice guidelines and quality of care for older patients with multiple comorbid disease: implications for pay for performance. JAMA. 2005;294:716–24. doi: 10.1001/jama.294.6.716. [DOI] [PubMed] [Google Scholar]
- Burney P, et al. The pharmacoepidemiology of COPD: recent advances and methodological discussion. Eur Respir J. 2003;2243(Suppl):1s–44s. [PubMed] [Google Scholar]
- Clavenna A, et al. Inappropriate use of anti-asthmatic drugs in the Italian paediatric population. Eur I Clin Pharmacol. 2003;59:565–69. doi: 10.1007/s00228-003-0660-9. [DOI] [PubMed] [Google Scholar]
- Curkendall SM, DeLuise C, et al. Cardiovascular disease in patients with chronic obstructive pulmonary disease, Saskatchewan Canada. Ann Epidemiol. 2006;16:63–70. doi: 10.1016/j.annepidem.2005.04.008. [DOI] [PubMed] [Google Scholar]
- Epping Jordan JE, Galea G, Tukuitonga C, et al. Preventing chronic diseases: taking stepwisw action. Lancet. 2006;366:1667–71. doi: 10.1016/S0140-6736(05)67342-4. [DOI] [PubMed] [Google Scholar]
- Fabbri LM, Luppi F, Beghè B, et al. Update in chronic obstructive pulmonary disease 2005. Am J Respir Crit Care Med. 2006;173:1056–65. doi: 10.1164/rccm.2603005. [DOI] [PubMed] [Google Scholar]
- GOLD Workshop Report Global strategy for the diagnosis, management, and prevention of COPD Update April 2005 [online]. URL: http://www.goldcopd.com.
- Gudmundsson G, Gislason T, Lindberg E, et al. Mortality in COPD patients discharged from hospital: the role of treatment and co-morbidity. Respiratory Research. 2006;7:109–17. doi: 10.1186/1465-9921-7-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halbert RJ, Isonaka S, George D, et al. Interpreting COPD prevalence estimates: what is the true burden of disease? Chest. 2003;123:1684–92. doi: 10.1378/chest.123.5.1684. [DOI] [PubMed] [Google Scholar]
- Hansell AL, Walk JA, et al. What do chronic obstructive pulmonary disease patients die from? A multiple cause coding analysis. Eur Respir J. 2003;22:809–14. doi: 10.1183/09031936.03.00031403. [DOI] [PubMed] [Google Scholar]
- Holguin F, Folch E, Redd SC, et al. Comorbidity and mortality in COPD-related hospitalizations in the United States, 1979 to 2001. Chest. 2005;128:2005–11. doi: 10.1378/chest.128.4.2005. [DOI] [PubMed] [Google Scholar]
- Huiart L, Ernst P, Suissa S. Cardiovascular morbidity and mortality in COPD. Chest. 2005;128:2640–6. doi: 10.1378/chest.128.4.2640. [DOI] [PubMed] [Google Scholar]
- Hurd SS, Lenfant C. COPD: good lung health is the key. Lancet. 2005;366:1832–4. doi: 10.1016/S0140-6736(05)67634-9. [DOI] [PubMed] [Google Scholar]
- Kim DS, Kim YS, Jung KS, et al. Prevalence of chronic obstructive pulmonary disease in Korea: a population-based spirometry survey. Am J Respir Crit Care Med. 2005;172:842–7. doi: 10.1164/rccm.200502-259OC. [DOI] [PubMed] [Google Scholar]
- Kunik ME, et al. Surprisingly high prevalence of anxiety and depression in chronic breathing disorders. Chest. 2005;127:1205–11. doi: 10.1378/chest.127.4.1205. [DOI] [PubMed] [Google Scholar]
- Liao JK. Clinical implications for statin pleiotropy. Curr Opin Lipidol. 2005;16:624–9. doi: 10.1097/01.mol.0000191913.16321.60. [DOI] [PubMed] [Google Scholar]
- Menezes AMB, Perez-Padilla R, et al. Chronic obstructive pulmonary disease in five Latin American cities (the PLATINO study): a prevalence study. Lancet. 2005;366:1875–81. doi: 10.1016/S0140-6736(05)67632-5. [DOI] [PubMed] [Google Scholar]
- Monte S, Fanizza C, Romero M, et al. Administrative databases as a basic tool for the epidemiology of cardiovascular diseases. G Ital Cardiol. 2006;7:206–16. [PubMed] [Google Scholar]
- Monte S, Macchia A, Pellegrini F, et al. Antithrombotic treatment is strongly underused despite reducing overall mortality among high-risk elderly patients hospitalized with atrial fibrillation. Eur Heart J. 2006;27:2217–23. doi: 10.1093/eurheartj/ehl208. [DOI] [PubMed] [Google Scholar]
- Murray CJ, Lopez AD. Alternative projection of mortality by cause 1990–2020: global burden of disease study. Lancet. 1997;349:1498–504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- Pena VS, Miravitlles M, Gabriel R, et al. Geographic variations in prevalence and underdiagnosis of COPD: results of IBERPOC multicentre epidemiological study. Chest. 2000;118:981–9. doi: 10.1378/chest.118.4.981. [DOI] [PubMed] [Google Scholar]
- Price D, Duerden M. Chronic obstructive pulmonary disease. BMJ. 2003;17(326):1046–7. doi: 10.1136/bmj.326.7398.1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redelmeier DA, Tan SH, Booth GL. The treatment of unrelated disorders in patients with chronic medical diseases. N Engl J Med. 1998;338:1516–20. doi: 10.1056/NEJM199805213382106. [DOI] [PubMed] [Google Scholar]
- Shapiro SD, Ingenito EP. The pathogenesis of chronic obstructive pulmonary disease: advances in the past 100 years. Am J Respir Cell Mol Biol. 2005;32:367–72. doi: 10.1165/rcmb.F296. [DOI] [PubMed] [Google Scholar]
- Sin DD, Man SF. Chronic obstructive pulmonary disease as a risk factor for cardiovascular morbidity and mortality. Proc Am Thorac Soc. 2005a;2:8–11. doi: 10.1513/pats.200404-032MS. [DOI] [PubMed] [Google Scholar]
- Sin DD, Man SF. Can inhaled steroids mend a broken heart in chronic obstructive pulmonary disease? Eur Respir J. 2005b;25:589–90. doi: 10.1183/09031936.05.00005105. [DOI] [PubMed] [Google Scholar]
- Soriano JB, visick GT, Muellerova H, et al. Patterns of comorbidities in newly diagnosed COPD and asthma in primary care. Chest. 2005;128:2005–11. doi: 10.1378/chest.128.4.2099. [DOI] [PubMed] [Google Scholar]
- Tzanakis N, Anagnostopoulou U, et al. Prevalence of COPD in Greece. Chest. 2004;125:892–900. doi: 10.1378/chest.125.3.892. [DOI] [PubMed] [Google Scholar]
- van Manen JG, Bindels PJE, Ijzermans CJ, et al. Prevalence of comorbidity in patients with chronic airway obstruction and controls over the age of 40. J Clin Epidem. 2001;54:287–93. doi: 10.1016/s0895-4356(01)00346-8. [DOI] [PubMed] [Google Scholar]
- Viegi G, Pedreschi M, Pistelli F, et al. Prevalence of airways obstruction in a general population: European Respiratory Society vs American Thoracic Society Definition. Chest. 2000;117:339S–345S. doi: 10.1378/chest.117.5_suppl_2.339s. [DOI] [PubMed] [Google Scholar]
- World Health Organisation Global alliance against chronic respiratory diseases. Accessed 2006. URL http://www.who.int/respiratory/gard/en.
- Yohannis AM, Baldwin RC, Conolly MJ. Depression and anxiety in elderly outpatients with chronic obstructive pulmonary disease: prevalence and validation of the BASDEC screening questionnaire. Int J Gen Psych. 2000;15:1090–6. doi: 10.1002/1099-1166(200012)15:12<1090::aid-gps249>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]