Abstract
Background:
To report the indications and clinical outcomes of all capsular tension ring (CTR) implantations in a large series of consecutive cataract surgeries during a five year interval in a university eye hospital.
Methods:
The study was designed as a restrospective analysis of a consecutive series of 9528 cataract surgeries. The records were checked for cases in which a CTR was implanted. The indications and clinical outcomes of CTR implantation were documented and an evaluation of posterior chamber intraocular lens (PCIOL) insertion, position, and centration.
Results:
In this series, a CTR was implanted in 69 eyes of 67 patients. The indications were advanced or mature cataract in 40, post-traumatic cataract in 23, pseudoexfoliation syndrome in 4 and subluxated lens in 2 eyes. PCIOL implantation in the capsular bag was possible in 61 (90%) of these 69 eyes. In 5 (7%) additional eyes, PCIOL implantation in the ciliary sulcus was accomplished. In one eye (1%) no IOL implantation was performed because of high myopia. In only two of 69 eyes (2%), an anterior chamber intraocular lens had to be inserted despite prior CTR implantation. In 5 eyes (5%), a slight dislocation of the IOL was noted postoperatively, but none of these patients complained of visually relevant symptoms (eg, monocular diplopia).
Conclusions:
According to our experience CTRs are used very infrequently (0.7%), but remain useful in cataract surgeries with difficult preoperative or intraoperative conditions. If zonulolysis is less than two quadrants in extent, implantation of a PCIOL was possible in 98% of cases. Implantation of CTRs with special designs may have additional advantages (eg, inhibition of posterior capsule opacity) and warrant further investigation.
Keywords: capsular tension ring, mature cataract, PEX, cataract surgery, IOL luxation
Introduction
The capsular tension ring (CTR) was first described in 1991 by Hara and coauthors (1991). They named it an “equator ring”, designed to maintain the circular contour of the capsular bag after lens removal during cataract surgery. However, their flexible silicon ring did not adapt to the different capsular bag sizes. In 1993, a different design was introduced allowing for an individual expansion and therefore being applicable for eyes with different dimensions (Nagamoto 2001). Since then, the first polymethylmethacrylate (PMMA) open capsular ring was produced by Morcher® (Stuttgart, Germany). Soon others (Ophtec®, Ioltech®, Acrimed®, etc.) began to produce similar devices. Nowadays, various designs have been developed for average individuals (Morcher® type 14, 10.0 mm closed diameter), highly myopic patients (Morcher® type 14A, 12.0 mm), and for children (Morcher® type 1C, 9.00 mm). In addition special CTRs were designed for cases with severe zonular dehiscence and an additional fixation hook for scleral fixation (Cionni and Osher 1995, 1998; Lam et al 2000; Ahmed and Crandall 2001). Coloboma shield CTRs and multisegmental coloboma rings have been suggested for large sector iris defects or congenital aniridia. Nishi and Menapace (1998, 2001) recently developed a square edged CTR to prevent posterior capsule opacification (Dick and Schwenn 1999).
Originally the CTR was designed to stabilize the capsule in eyes with zonular weakness or dehiscence (Gimbel et al 1997; Sun and Gimbel 1998; Gimbel and Sun 2002), intraocular lens (IOL)-luxation (Groessi and Anderson 1998; Dietlein et al 2000), pseudoexfoliation syndrome (Menapace et al 2000; Bayraktar et al 2001), and highly myopic eyes not receiving a posterior chamber intraocular lens (PCIOL). In past years the CTR has been widely used throughout Europe, but this far was not FDA-approved in the USA. The purpose of our study was to evaluate the frequency, indications, and clinical outcome of CTR implantation in a large series of consecutive cataract surgical cases performed during the years 1997 through 2001 in our institution.
Patients and methods
Surgical technique
After preoperative dilation of the pupil the conjunctival sac was flushed with 10 ml 10% povidone iodine rinsing solution. Superior, either a sclerocorneal or a clear corneal incision, was created using a diamond blade followed by a 2.75 mm steel keratome (Alcon, Fort Worth, TX). Further two 1.2 mm clear corneal incisions were performed with a 15° keratome (Alcon) and the anterior chamber was expanded with a viscoelastic substance (Healon, AMO, Santa Ana, CA). For cataract surgery of mature cataracts, Trypan blue (vision blue, DORC, Netherlands) was used to enhance visualization of the anterior lens capsule. Capsulotomy was performed using a 25 gauge needle. After hydrodissection cataract extraction was performed using the divide and conquer technique. The Megatron S3 (Geuder, Heidelberg, Germany) phacoemulsification unit was used, with an ultrasound power set 50% to 100% and a phaco tip angled at 30 degrees.
Chart review
We retrospectively reviewed the cataract database of the Department of Ophthalmology, Ludwig-Maximilians-University, Munich for records indicating implantation of a CTR. Since the first documented implantation of a CTR in our institution, all subsequent records were screened for indication of a CTR implantation, and subsequently clinical outcome was analyzed. In all cases a CTR Morcher®, Type 14 (open diameter 12.3 mm, PMMA) was used (Figure 1). Specific indications included zonulolysis or posterior capsular rupture. In case of a zonulolysis, exogenous (trauma, prior pars-plana-vitrectomy with silicone oil tamponade), or endogenous (pseudoexfoliation syndrome, Marfan syndrome) causes were distinguished. The decision to insert the CTR was made intraoperatively when loose zonules where apparent during capsulorhexis or phacoemulsification, or when a posterior capsular rupture occurred. In case of a posterior capsular rupture, an anterior vitrectomy was performed. Our surgeons mainly used phacoemulsification to extract the cataract; a planned extracapsular cataract extraction was performed only twice. In all cases, the CTR was inserted with a special shooter. If accidental displacement into the vitreous occurred during the procedure, the CTR was removed.
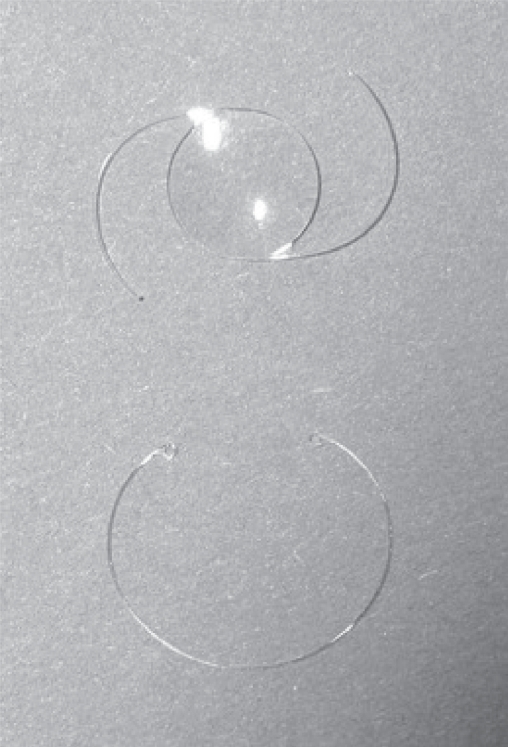
Figure 1.
Morcher® type 14 CTR (open diameter 12.5 mm)(down) and IOL (up).
Abbreviations: CTR, capsular tension ring, IOL, intraocular lens.
The main clinical outcome measurement was a possible PCIOL-implantation with differentiation between implantation in the capsular bag or the ciliary sulcus. In addition, the position of the intraocular lens was noted. In case of IOL subluxation or dislocation, the clinical symptoms (eg, monocular double vision) were evaluated.
Results
During the period of review of 5 years, 9528 cataract surgeries were performed in our department. In 69 of these surgeries (67 patients) a CTR was implanted (Table 1). Among these patients 37 (55%) were male and 30 (45%) were female. The mean age was 62 years with a range from 22 to 101 years. The range of follow up was between one and three years.
Table 1.
Patients with CTR implantation: pre- and post-operative characteristics
| Pre-op characteristics | Post-op characteristics | ||||
|---|---|---|---|---|---|
| Mean age | 62 | CTR and IOL | Capsular bag | 61 | |
| Sex | Male | 37 | Sulcus | 5 | |
| Female | 30 | ||||
| Diagnosis | Mature cataract | 40 | CTR only (no IOL planned) | 1 | |
| Traumatic cataract | 23 | ||||
| Subluxated lens | 2 | No IOL despite CTR | 2 | ||
| PEX | 4 | ||||
Abbreviations: CTR, capsular tension ring, IOL, intraocular lens; PEX, pseudoexfoliation syndrome.
The indications for CTR implantation were as follows: In 35 eyes, a zonular dehiscence or weakness of different origin was observed before surgery, with exogenous causes of zonulolysis being evident in 29 eyes (23 with prior trauma and 6 with history of pars plana vitrectomy and silicone oil tamponade) and endogenous zonulolysis being apparent in 6 eyes; specifically, 4 eyes (6%) with pseudoexfoliation syndrome and 2 eyes (3%) of one patient with Marfan syndrome. In 23 eyes, a zonular rupture occured during cataract surgery itself. In the remaining 11 eyes, no underlying predisposition could be identified before surgery. Most likely in these cases the zonulolysis occured during the procedure. An advanced or mature cataract was present in 40 eyes (58%).
All in all, implantation of a CTR was chosen because of zonular dialysis in 61 eyes (88%), rupture of the posterior capsule in one eye (2%), or both zonular dialysis and rupture of the posterior capsule in 7 eyes (10%).
In 67 eyes (98%), an implantation of a posterior chamber intraocular lens (PCIOL) was performed without complication following the implantation of a CTR. In 61 cases (90%), an implantation into the capsular bag could be accomplished, whereas in 5 eyes (7%), the PCIOL had to be implanted into the ciliary sulcus. In one eye (1%) no IOL implantation was performed because of high myopia.
Thus, in only two of 69 eyes (2%) an IOL implantation into the capsular bag or ciliary sulcus was not possible despite prior CTR insertion: In one eye IOL implantation into capsular bag or ciliary sulcus was not possible due to extensive zonulolysis. In the second case an implanted PCIOL and the CTR dislocated into the vitreous 5 days after surgery and had to be removed. Both of these eyes received an anterior chamber IOL.
The PCIOL remained in a centered position in 61 eyes (92%) whereas in 5 eyes (8%) a dislocation of the IOL was observed during slit lamp biomicroscopy. However none of these patients complained of any symptoms such as monocular diplopia and the decentration was stable and did not progress further during follow up.
Discussion
The present study was performed to address two subjects: First, to evaluate the frequency of CTR implantation in a large consecutive series of cataract surgeries. Second, to investigate whether an anatomically reasonable outcome could be reached by the insertion of a CTR in a variety of complicated cataract surgeries. Final visual outcome was not investigated in our study as the group of patients investigated was rather heterogenous with a large spectrum of additional diseases such as macular degeneration and diabetic retinopathy that would have significantly biased any evaluation of functional outcome. Therefore, the present study aimed at an anatomical or morphological evaluation of the surgical results and focused on the applicability of CTR implantation during cataract surgery.
Since the first insertion of a CTR in our institution, 9528 cataract surgeries have been performed during the following period of 5 years. Despite the fact that predominantly severe forms of cataracts and complicated cases are relatively frequent in our tertiary care center university setting, only relatively few cases (0.7%) required the implantation of a CTR, probably because the surgeries were done by experienced anterior segment surgeons. The predominant indication for CTR implantation was determined by an unstable intraoperative condition either caused by zonular dehiscence or weakness and/or posterior capsular rupture, or by different conditions including mature cataract (40 eyes, 58%), traumatic cataract (23 eyes, 33%), pseudoexfoliation syndrome (4 eyes, 6%), and subluxated lenses due to Marfan syndrome (2 eyes, 3%). The indications for CTR implantation are in line with other authors who also used the CTR in eyes with intraoperative signs for loose or broken zonules like decentration of the crystalline lens, movement of the lens during capsulorhexis, phacoemulsification or irrigation/aspiration (Gimbel et al 1997; Sun and Gimbel 1998; Menapace et al 2000; Lee et al 2001, 2002; Gimbel and Sun 2002). Like other authors (Menapace et al 2000; Gimbel and Sun 2002), our surgeons inserted the CTR as soon as zonular weekness was seen intraoperatively, for example before or after hydrodissection and prior to phacoemulsification or after complete phacoemulsification and prior to PCIOL insertion.
The PCIOL was successfully implanted in almost all cases (97%), with an implantation in the capsular bag being possible in the majority of cases (91%). Only in two cases no permanent implantation of an PCIOL was possible despite prior insertion of a CTR; in one of these eyes a dislocation of both the CTR and the PCIOL occurred due to extended zonular dehiscence and led to explantation of both implants (Table 1).
In our series one highly myopic eye was left without IOL. The CTR helps in these cases to maintain the circular contour of the capsular bag and the shape of the continuous circular capsulorhexis (Sun and Gimbel 1998). Thus, folds in the posterior capsular bag are minimized.
The only postoperative complication found in our series was minor PCIOL decentration noted biomicroscopically during follow up, but no subjective visual symptoms were noted by the patients. Because this was a retrospective chart review we were unable to determine whether the same results would have been reached without CTR implantation.
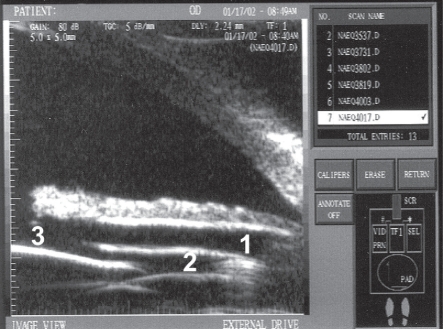
At the moment several clinical studies are also attempting to investigate if routine CTR insertion is reasonable to prevent capsular shrinkage and posterior capsule opacification (Strenn et al 1997; Nishi et al 1998, 2001; Dick and Schwenn 1999; Faschinger and Eckhardt 1999; Sudhir and Rao 2001; Waheed et al 2001). Since the invention of the capsular tension ring in 1991, many authors have reported its advantages in anterior segment surgery. Our results in this large series over a relatively long period of time confirm that CTR implantation is a useful device for cataract surgery in selected cases with difficult pre- or intraoperative conditions (Figure 2).
Figure 2.
UBM findings after CTR and IOL insertion (intraoperative zonulolysis over 4 clock hours) (Fries et al 1998).
Notes: CTR (1), haptic of IOL (2), and IOL (3).
Abbreviations: CTR, capsular tension ring, IOL, intraocular lens; UBM, ultrasound biomicroscopy.
A weakness of the present study is the retrospective nature and the lack of a control group. Obviously, only a prospective randomized study could further elucidate whether the same clincial outcome (eg, possibility of PCIOL implantation) could be achieved without prior implantation of a CTR. However, the following aspects should be considered in this context: First, based on our study with a frequency of CTR implantation of 0.7%, the number of cataract cases included will have to be very large to achieve statistical power. Second, the decision whether to implant a CTR or not is usually made during surgery; this approach interferes with a prospective randomized study setting. Third, patients would have to give their informed consent prior to surgery allowing for the randomized (non-) use of a CTR even in the event of complicated surgery. In the absence of such a randomized study to the best of our knowledge our experience represents the largest series of consecutive cataract surgeries that was evaluated for implantation of a CTR.
Footnotes
Disclosure
The authors have no commercial interest. This study was presented at the annual meeting of the Association for Research in Vision and Ophthalmology, Fort Lauderdale, May 5th 2002.
References
- Ahmed II, Crandall AS. Ab externo scleral fixation of the Cionni modified capsular tension ring. J Cataract Refract Surg. 2001;27:977–81. doi: 10.1016/s0886-3350(01)00924-5. [DOI] [PubMed] [Google Scholar]
- Bayraktar S, Altan T, Kucuksumer Y, et al. Capsular tension ring implantation after capsulorhexis in phacoemulsification of cataracts associated with pseudoexfoliation syndrome. Intraoperative complications and early postoperative findings. J Cataract Refract Surg. 2001;27:1620–8. doi: 10.1016/s0886-3350(01)00965-8. [DOI] [PubMed] [Google Scholar]
- Cionni RJ, Osher RH. Endocapsular ring approach to the subluxed cataractous lens. J Cataract Refract Surg. 1995;21:245–9. doi: 10.1016/s0886-3350(13)80126-5. [DOI] [PubMed] [Google Scholar]
- Cionni RJ, Osher RH. Management of profound zonular dialysis or weakness with a new endocapsular ring designed for scleral fixation. J Cataract Refract Surg. 1998;24:1299–306. doi: 10.1016/s0886-3350(98)80218-6. [DOI] [PubMed] [Google Scholar]
- Dick B, Schwenn O. Capsular bent ring. Improvement of the capsular tension ring. Ophthalmology. 1999;96:114–19. doi: 10.1007/s003470050385. [DOI] [PubMed] [Google Scholar]
- Dietlein TS, Jacobi PC, Konen W, et al. Complications of endocapsular tension ring implantation in a child with Marfan’s syndrome. J Cataract Refract Surg. 2000;26:937–40. doi: 10.1016/s0886-3350(00)00318-7. [DOI] [PubMed] [Google Scholar]
- Faschinger CW, Eckhardt M. Complete capsulorhexis opening occlusion despite capsular tension ring implantation. J Cataract Refract Surg. 1999;25:1013–15. doi: 10.1016/s0886-3350(99)00070-x. [DOI] [PubMed] [Google Scholar]
- Fries U, Hoffmann PC, Hut WW, et al. IOL-calculations and ultrasonic biometry: Immersion and contact procedures. Klin Monatsbl Augenheilkd. 1998;213:162–5. [PubMed] [Google Scholar]
- Gimbel HV, Sun R, Heston JP. Management of zonular dialysis in phacoemulsification and IOL implantation using the capsular tension ring. Ophthalmic Surg Lasers. 1997;28:273–81. [PubMed] [Google Scholar]
- Gimbel HV, Sun R. Clinical applications of capsular tension rings in cataract surgery. Ophthalmic Surg Lasers. 2002;33:44–53. [PubMed] [Google Scholar]
- Groessl SA, Anderson CJ. Capsular tension ring in a patient with Weill-Marchesani syndrome. J Cataract Refract Surg. 1998;24:1164–5. doi: 10.1016/s0886-3350(98)80114-4. [DOI] [PubMed] [Google Scholar]
- Hara T, Hara T, Yamada Y. “Equator ring” for maintenance of the completely circular contour of the capsular bag equator after cataract removal. Ophthalmic Surg. 1991;22:358–9. [PubMed] [Google Scholar]
- Lam DS, Young AL, Leung AT, et al. Scleral fixation of a capsular tension ring for severe ectopia lentis. J Cataract Refract Surg. 2000;26:609–12. doi: 10.1016/s0886-3350(99)00403-4. [DOI] [PubMed] [Google Scholar]
- Lee DH, Lee HY, Lee KH, et al. Effect of a capsular tension ring on the shape of the capsular bag and opening and the intraocular lens. J Cataract Refract Surg. 2001;27:452–6. doi: 10.1016/s0886-3350(00)00610-6. [DOI] [PubMed] [Google Scholar]
- Lee DH, Shin SC, Joo CK. Effect of a capsular tension ring on intraocular lens decentration and tilting after cataract surgery. J Cataract Refract Surg. 2002;28:843–6. doi: 10.1016/s0886-3350(01)01174-9. [DOI] [PubMed] [Google Scholar]
- Menapace R, Findl O, Georgopoulos M, et al. The capsular tension ring: designs, applications, and techniques. J Cataract Refract Surg. 2000;26:898–912. doi: 10.1016/s0886-3350(00)00446-6. [DOI] [PubMed] [Google Scholar]
- Nagamoto T. Origin of the capsular tension ring. J Cataract Refract Surg. 2001;27:1710–11. doi: 10.1016/s0886-3350(01)01202-0. [DOI] [PubMed] [Google Scholar]
- Nishi O, Nishi K, Menapace R, et al. Capsular bending ring to prevent posterior capsule opacification: 2 year follow-up. J Cataract Refract Surg. 2001;27:1359–65. doi: 10.1016/s0886-3350(01)00892-6. [DOI] [PubMed] [Google Scholar]
- Nishi O, Nishi K, Menapace R. Capsule-bending ring for the prevention of capsular opacification: a preliminary report. Ophthalmic Surg Lasers. 1998;29:749–53. [PubMed] [Google Scholar]
- Strenn K, Menapace R, Vass C. Capsular bag shrinkage after implantation of an open-loop silicone lens and a poly(methyl methacrylate) capsule tension ring. J Cataract Refract Surg. 1997;23:1543–7. doi: 10.1016/s0886-3350(97)80027-2. [DOI] [PubMed] [Google Scholar]
- Sudhir RR, Rao SK. Capsulorhexis phimosis in retinitis pigmentosa despite capsular tension ring implantation. J Cataract Refract Surg. 2001;27:1691–4. doi: 10.1016/s0886-3350(01)00869-0. [DOI] [PubMed] [Google Scholar]
- Sun R, Gimbel HV. In vitro evaluation of the efficacy of the capsular tension ring for managing zonular dialysis in cataract surgery. Ophthalmic Surg Lasers. 1998;29:502–5. [PubMed] [Google Scholar]
- Waheed K, Eleftheriadis H, Liu C. Anterior capsular phimosis in eyes with a capsular tension ring. J Cataract Refract Surg. 2001;27:1688–90. doi: 10.1016/s0886-3350(01)00766-0. [DOI] [PubMed] [Google Scholar]