Like many complex physiological conditions, obesity results from the interaction of multiple genes and environmental factors. Obesity often runs in families, but since families tend to share lifestyle habits as well as genes, teasing out genetic factors has proved difficult. The search for candidate genes for susceptibility has been further complicated by the likelihood that each gene contributes a small effect and that these genes may differ in different populations. In a large case-control study of nuclear families in France, Philippe Froguel and colleagues used genome-wide scans of a chromosomal region linked with susceptibility to identify a new candidate gene for obesity.
The genetic variation that accounts for the near boundless diversity in human form and behavior arises from an average 0.1% difference in genome sequence among individuals. Much of this variation is due to single nucleotide polymorphisms, or SNPs, which occur on average at one locus per 1,000 DNA basepairs, out of a total 3 billion. Many of these variants occur outside of genes, but those found in or around genes affect everything from individual appearance to susceptibility (or resistance) to disease. Specific gene variants, called alleles, are linked to increased risk for a number of diseases, including “monogenic” obesity, a rare condition in which single genes can cause obesity. But most cases of obesity are “polygenic,” influenced by many genes.
Froguel and colleagues had previously found a strong linkage between a region of chromosome 10 and obesity, with SNPs in the GAD2 gene turning up most frequently. GAD2 codes for an enzyme (glutamic acid decarboxylase, or GAD65) that catalyzes the production of a neurotransmitter (gamma-aminobutyric acid, or GABA) that interacts with a neuropeptide (NPY) in the hypothalamus to help stimulate appetite. In an average-weight individual, the metabolic effects of orexigenic neuropeptides (which stimulate the appetite, decrease energy use, and support fat storage) and those of anorexigenic neuropeptides (which suppress appetite, increase energy use, and help burn fat) are kept in balance. It has long been thought that alleles affecting metabolism may increase susceptibility by inhibiting anorexignic neuropeptides.
Screening genomic data on 575 obese subjects and 646 controls for GAD2 alleles, Froguel et al. identified one group of alleles as “protective” against obesity and another as increasing risk. These links were supported by genetic screens of the nuclear families participating in the study, which showed a higher frequency of the protective group of alleles in the controls. Obese individuals with two copies of one at-risk allele also had more difficulty controlling food intake compared to control subjects, based on a standardized assessment of eating behavior. When the researchers investigated the physiological effect of the “highest risk” GAD2 variant in a mouse cell line, they found it caused a 6-fold increase in transcriptional activity compared to the “wild-type” cells without the variant.
The researchers hypothesize that an overexpression of the GAD2 gene may increase the amount of the neurotransmitter GABA in the hyopothalamus, thereby increasing GABA's orexigenic effects and leading to overeating. Studies in turkeys injected with muscimol, a GABA activator, and mice overexpressing a protein that regulates GABA localization support this notion; the more musimol the turkeys received, the more they ate, while the mice gained more weight and showed higher fat deposits.
Genetic factors can't explain the rapid rise in obesity rates, but they can provide clues to preventive and therapeutic approaches to ease the health burden associated with the condition. The results to date suggest that GAD2 is a promising candidate gene. Future work on the genetics and biology of GAD2 will resolve whether and how the gene influences body weight.
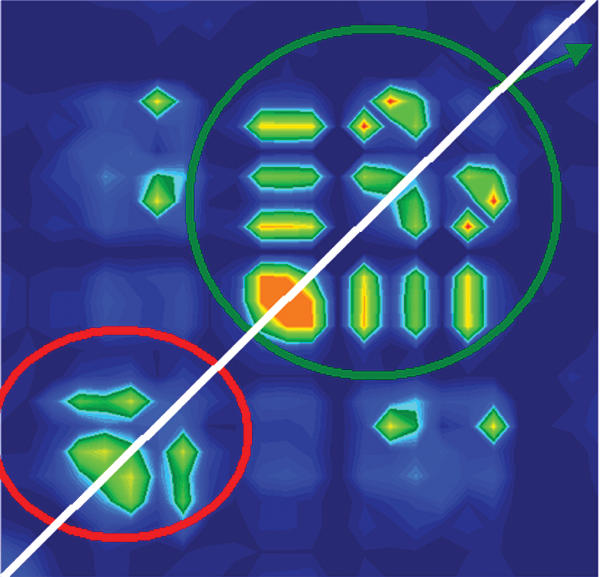
Visualization of linkage disequilibrium.