Abstract
Background
Following reports of high prevalence of low back pain (LBP) in young physiotherapists [17-22], we investigated whether LBP was a problem for undergraduate physiotherapy students.
Method
Physiotherapy students enrolled in one Australian tertiary institution completed a validated self-administered questionnaire in April 2001, seeking information on LBP prevalence (lifetime, 12 month, one-month, one-week), and its risk factors. The survey incorporated the Nordic back questionnaire, questions on common risks for LBP, and purpose-built questions regarding educational exposures. Univariate logistic regression models were applied to test associations.
Results and Discussion
72% students responded. LBP prevalence was 69% (lifetime), 63% (12-month), 44% (one-month), 28% (one-week). The risk of LBP increased significantly for students once they completed first year. Being aged 20 or 21 years (final year students) was significantly associated with all measures of LBP, compared with the youngest students. Exposure to tertiary study of greater than two years was associated with lifetime, 12 month and one-month LBP prevalence. Spending more than 20 hours in the past month 'sitting looking down' was significantly associated with one-month LBP prevalence. Similar exposure to 'treating patients' was significantly associated with one-month and one-week LBP prevalence.
Conclusions
Physiotherapy students should be alerted to the likelihood of LBP and is potential causes during their training, so that they enter the workforce with reduced risk of LBP. The potential for other undergraduate students to suffer LBP should also be considered.
Keywords: Low back pain, physiotherapy students, risk factors
Background
World-wide estimates of lifetime prevalence of low back pain (LBP) vary from 50 to 84 percent [1-7]. Occupational LBP relates to exposure to workplace hazards [8] and incurs high costs to society in terms of health care, loss of productivity, workplace and family stress, as well as individual pain and suffering [9-11]. Thus prevention of occupational LBP is a key research concern.
Factors associated with occupational LBP are commonly cited as physical (workplace) and personal (individual) [8,9]. Physical factors are proposed as heavy physical work, lifting, bending, twisting and static postures [8,12-14], whilst personal factors are described as non-modifiable (age, gender, anthropometry etc) and potentially modifiable (physical fitness, motor control, strength etc) [13-15].
LBP is commonly treated by physiotherapists [16]. However, physiotherapists themselves have been reported as being LBP sufferers [17-22], with Australian prevalence statistics approximating those from British, Canadian and American surveys (see Table 6for prevalence estimates). Concerningly, all these authors report high LBP prevalence in young physiotherapists (< 30 years) (approximating 30–40%), with up to 60% of LBP events in this age group estimated to result from work-related injuries within the first five years of employment [17,18,20-22]. General population health characteristics in Australia suggest that LBP prevalence for 15–24 year olds, and 25–34 year olds (16%, 18% respectively), which is lower than that reported for young physiotherapists [11].
Table 6.
Comparison with other authors of prevalence estimates
| Authors | Lifetime | 12-Month | 1-Month | 1-Week | |
| Nyland and Grimmer | Students | ||||
| • First year | 57.5% | 51.3% | 31.3% | 15.0% | |
| • Second year | 72.4% | 65.8% | 50% | 35.5% | |
| • Third year | 67.6% | 61.8% | 41.2% | 32.4% | |
| • Fourth year | 81.7% | 76.% | 56.7% | 31.7% | |
| • Overall | 69.2% | 63.2% | 44.4% | 27.6% | |
| West and Gardner [20] | Graduate physiotherapists | 35.0% | 22.0% | ||
| Cromie et al [21] | Graduate physiotherapists | 62.5% | |||
| Scholey and Hair[18] | Graduate physiotherapists | 54.0% | 46.0% | 13.0% | |
| Scholey and Hair [19] | Graduate physiotherapists | 57.0% | 38.0% | 14.0% | |
| Mierzejewski and Kumar [17] | Graduate physiotherapists | 49.2% | 37.0% |
Student physiotherapists are potentially exposed to the same LBP occupational risks as graduates, such as poor working postures and frequent manual handling activities, often undertaken in difficult environments and with variable training regarding personal safety [23,24]. As an example of the risks associated with the physiotherapy occupation, 27% physiotherapy students were reported in one study to have experienced LBP as a direct result of handling patients [23]. In the Australian context, Cromie et al [22] reported from their retrospective survey of physiotherapists' work-related musculoskeletal disorders, that approximately 16% respondents reported LBP commencing during their physiotherapy training, with a further 5.6% physiotherapists reporting LBP that was present prior to training. In light of these reports of student and early career onset of LBP for physiotherapists [17,20-22], and the potential long term costs associated with ongoing LBP [9-11], it seems timely to understand physiotherapy student experiences of LBP and the factors that may be associated with its onset. This paper reports on four measures of the prevalence of LBP in student physiotherapists in one Australian university, and considers the association of LBP prevalence with a number of potential risk factors for LBP.
Method
Ethics Approval
Ethics approval for this study was provided by Human Research Ethics Committee of the researchers' academic institution.
Subject Selection
All students who were enrolled by March 2001 in the four year Bachelor of Physiotherapy program at one Australian university were eligible to participate. There were no exclusion criteria.
Instrument (Questionnaire) Development and Testing
Volunteers from all four student year levels were recruited via notices in the student common room, to assist in the construction, content and construct validity testing of the study instrument (see section on Instrument (Questionnaire) Development and Testing). This group specifically had the responsibility of developing questions on educational exposures that they considered were relevant to their training program. There were 15 participants (3–4 from each year level) (eight males, seven females). A separate set of volunteers was also recruited from the fourth-year physiotherapy students to establish the reliability of responses to items in the final instrument (six females, four males randomly selected from 28 respondents).
Cross-sectional prevalence study
All students enrolled in the physiotherapy undergraduate program at this tertiary institution (N = 346) were invited to participate in a cross-sectional prevalence study using the resultant study instrument.
The study instrument
Self-administered written questionnaires are the most common method for establishing the prevalence of back pain [25]. Our study instrument sought standard information on gender, age, height, weight, amount and type of all occupational and sporting activities, and current levels of fitness were self assessed as poor, moderate or good. It also included purpose-built questions on exposure to perceived workplace hazards for physiotherapy students. The time frame of 'the past month' for educational exposure was determined by the students who constructed the questionnaire as being relevant to their training program. The educational exposure questions were derived directly from the student focus group deliberations (i.e. educational risks perceived by students themselves) (see previous, and next section). LBP prevalence questions were taken directly from an established instrument (Nordic Back Pain Questionnaire)[26,27] that captured information retrospectively on lifetime, 12-month, one-month and one-week prevalence.
Low back pain definition
LBP was defined as in the Nordic Back Pain Questionnaire [26,27] as an 'ache, pain or discomfort in the shaded area whether or not it extends from there to one or both legs (sciatica)'. The shaded area is outlined on a body diagram (see page 3 Appendix 1) representing the area between the 12th ribs and gluteal folds. Information on intensity or frequency of individual LBP episodes was not collected.
Instrument (Questionnaire) Development and Testing
Focus groups were conducted to develop and validate questions about educational exposures specific to physiotherapy students. Iterative procedures were used to reach agreement on content, wording and response construction [28-32]. The study instrument was then subjected to reliability testing.
Reliability study
Subjects completed the written instrument and handed it to the investigator. They were interviewed within 24 hours by the principal researcher (LN), providing verbal responses to every questionnaire item (asked out of sequence to minimise recall bias). The two sets of responses were in at least 80% agreement (Kappa scores > 0.77) for all but one item. This was the question about educational exposures. Subsequent revision of its wording, and the way in which responses were captured, produced evidence of improved agreement (90%) (Kappa = 0.87) from two telephone interviews on consecutive days with the reliability subjects (see Question 10, Appendix 1). The study instrument is in Appendix 1.
Cross-sectional prevalence study
Participation in data collection was voluntary and anonymous, and occurred in early April 2001. To collect data from students in program years 1–3, the principal researcher (LN) attended a nominated lecture at which all students could be expected to be present. Students returned the completed questionnaire before leaving the lecture. The fourth year students however, were all absent from campus on clinical placements, thus the questionnaire was posted to the clinical placement address and returned via reply-paid envelope.
Statistical Methods
Data was analysed using SAS Version 8.2.
Sample sensitivity analysis
Sample sensitivity analysis was conducted post-hoc [32,33] to determine the adequacy of the sample to provide robust estimates of differences in LBP prevalence (lifetime, 12 month and one-month) across the four year levels with at least 80% power [34].
Prevalence study
Lifetime prevalence is a general measure of LBP as it takes account of all other measures of prevalence. For instance a student reporting having experienced back pain in the previous week (but not ever before), would also have reported experiencing lifetime LBP, but would not have reported LBP in the past 12 months, or the past month. Conversely, a student who experienced LBP prior to entering university, but not since, would also indicate having a lifetime measure of LBP, but not LBP in the past 12-months, one-month or one-week. Students who reported LBP as a regular feature of their lives may well report lifetime, 12-month, one-month and one-week LBP. This paper reports on all measures of LBP prevalence because of the differential nature of exposure to the range of variables tested.
Table 1 outlines the associations between LBP prevalence measures and the exposure variables chosen for reporting in this paper. Due to the time-period of data capture for exposures, not all were relevant to all LBP prevalence measures. Gender, age, year level of study and length of study were relevant exposures for all measures of LBP. Lifetime occupational and sport participation exposure measures were relevant to lifetime LBP prevalence, but not to more recent LBP prevalence measures. Educational exposures measured over the past month were only relevant to one-month and one-week LBP prevalence. Weight and height were unlikely to be related to one-month or one-week LBP prevalence because of limited potential for change in exposure, but may well be related to 12-month prevalence. On the other hand, the expected major changes to height and weight over a lifetime would reduce the usefulness of these variables as exposures for lifetime LBP prevalence. Self-assessed fitness was potentially relevant to 12-month, one-month and on-week prevalence measures.
Table 1.
Approach to data analysis
| Recall period | ||||
| Lifetime | 12 month | 1 month | 1 week | |
| Disease information | Prevalence | Prevalence | Prevalence | Prevalence |
| Age at initial onset | ||||
| Initial incident | ||||
| Putative associated factors | Year level of study | Year level of study | Year level of study | Year level of study |
| Age | Age | Age | Age | |
| Gender | Gender | Gender | Gender | |
| Occupational exposure | ||||
| Sport exposure | ||||
| Length of study | Length of study | Length of study | Length of study | |
| Height | ||||
| Weight | ||||
| Level of fitness | Level of fitness | Level of fitness | ||
| Educational exposures | Educational exposures | |||
LBP prevalence data was described by year level (overall and in gender strata), using percentages, risk ratios and associated 95% confidence intervals (CI). Linear analysis for trend in proportions was calculated across the four university year levels, and reported as chi-square for trend statistics and associated p values.
Interpretation and application of predictive variables
Associations between potential exposure variables and the four measures of LBP prevalence were tested using univariate logistic regression models, reporting the associations as odds ratios and 95%CI. Significance of association was detected when confidence intervals did not span 1, and where confidence intervals skimmed 1, these are noted as trends towards significance. Gender, university year level and self-reported fitness were tested as independent categories using the classifications of data collection (See Appendix 1). Being male, being in first year of the physiotherapy program, and having poor fitness were the relevant comparison categories. The effect of age was tested in independent year categories relevant to the sample distribution (18 years and younger [the comparison level], 19 through to 22 years as separate categories, and 23+ years). Preliminary testing of the association with LBP of the educational exposure questions indicated that the data could be dichotomised for each question at 20 hours or less (comparison category) (comprising categories 1–3), and more than 20 hours in the past month (exposure category) (the last four categories). Preliminary analysis indicated that the risk of LBP in the categories of 0, 1–10, 11–20 hours was similar (approximating 1) for all the educational exposure questions. The risk of LBP in the last four categories was elevated compared with the first three, with similar risk estimates across the last four categories. All continuous variables were dichotomised at the median value:
 length of time spent studying at university divided at 2 years or less as the comparison group, and greater than two years as the exposure group
length of time spent studying at university divided at 2 years or less as the comparison group, and greater than two years as the exposure group
 height dichotomised at less than 171 cm (comparison category), 171 or more cm (exposure category)
height dichotomised at less than 171 cm (comparison category), 171 or more cm (exposure category)
 weight at less than 63 kgs (comparison category) and 63 kgs or greater (exposure category)
weight at less than 63 kgs (comparison category) and 63 kgs or greater (exposure category)
 body mass index at less than 21.25 (comparison category) and 21.25 or greater (exposure category).
body mass index at less than 21.25 (comparison category) and 21.25 or greater (exposure category).
Occupational exposure was calculated as an index, taking account of the total amount of time (hours) estimated by subjects as being spent in each reported occupation, multiplied by an action category of the occupation [35,36] (assigned using a modification of the Ovako Working Posture Analysis System [36]). This provided a cumulative index per subject of action category occupation hours, which was then categorised into tertiles for analysis purposes. Sport was calculated as the cumulative total reported time ever (hours) spent playing each nominated sport, with no difference in ranking given to competition or recreational level of sport. This index was also divided into tertiles for analysis purposes. Dividing index exposure data into tertiles provides a mechanism for assigning individuals into risk categories of high, medium and low, where no other exposure classifications are plausible, logical or commonly used [33,34].
Results
Response rates in the prevalence study
There was an overall response rate of 72%. Table 2 reports response rates in each year university level, and describes the sample by gender, mean age (SD) and mean length of study (range). The gender-specific response rates were not different from the proportion of males and females enrolled in each year level. The average age of onset of LBP was 16.4 years (SD 2.9 years) with 82% of the incidents associated with initial LBP onset being related to sport.
Table 2.
Characteristics of the sample
| Year level | Overall | ||||
| 1 | 2 | 3 | 4 | ||
| Response rate (%) | 80 (N = 80) | 82 (N = 76) | 49 (N = 34) | 71 (N = 60) | 72 (N = 250) |
| Gender (%) | |||||
| • Male | 26 (N = 21) | 49 (N = 36) | 21 (N = 7) | 40 (N = 24) | 36 (N = 90) |
| • Female | 74 (N = 59) | 51 (N = 40) | 79 (N = 27) | 60 (N = 36) | 64 (N = 160) |
| Mean age in years (SD) | 19.1 (2.2) | 20.8 (3.1) | 19.9 (1.6) | 21.6 (1.9) | 20.3 (2.6) |
| Mean length of study in years (Range) | 0 (-) | 1.1 (1–3) | 2 (-) | 3.2 (3–5) | 1.4 (0–5) |
| N available subjects | 100 | 93 | 69 | 84 | 346 |
Sample sensitivity analysis
Considering year level differences in lifetime prevalence over the four years of study, Cohen's tables [34] suggest that at p<0.05, this effect size (0.18) was powered at 89%. Smaller effect sizes were found for differences in 12 month and one-month prevalence over the year levels (0.14 and 0.16 respectively). Cohen's tables [34] indicate that at p < 0.05 the power of this study sample to estimate these differences was 65% and 70% respectively. To produce these same effect sizes with over 80% power would have required a sample of approximately 300. Thus this study sample was appropriately powered to provide robust estimates of differences over the year levels in lifetime prevalence, but less well powered to detect differences in the more recent measures of LBP.
Prevalence
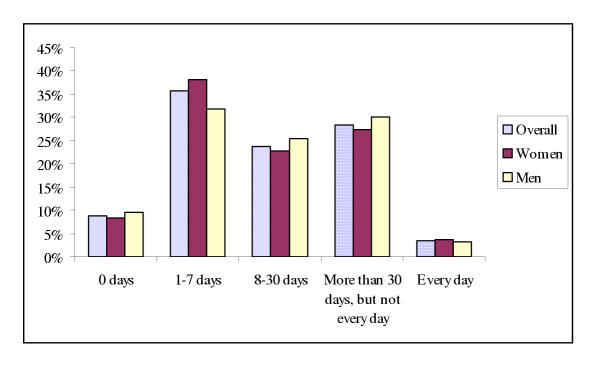
Table 3 presents the prevalence of each measure of LBP (95% CI) for each year level, and in gender strata. A trend towards significantly increasing prevalence of all measures of LBP across the year levels was observed overall, and for females (see Table 3). The frequency with which LBP was experienced within the previous 12 months overall, and by gender strata, is reported in Figure 1, highlighting that most commonly, LBP was suffered between one and seven days in the previous twelve month period, and that there were no gender differences in the frequency with which LBP was suffered.
Table 3.
Prevalence of LBP (95%CI) as a percentage of the total number of respondents (overall, per year level and gender), and evidence of linearity for trend over the year levels (overall and per gender).
| Lifetime | 12-Month | 1-Month | 1-Week | |
| First year | ||||
| Male | 47.6 (29.8–69.4) | 42.9(21.3–64.5) | 33.3 (12.7–53.9) | 19.0 (1.9–36.1) |
| Female | 61.0 (48.5–73.4) | 54.2 (41.5–76.9) | 30.5 (18.7–42.4) | 13.6 (4.8–22.3) |
| Overall | 57.5 (46.4–68.5) | 51.3(40.1–62.5) | 31.3 (20.9–41.7) | 15 (7.0–22.9) |
| Second year | ||||
| Male | 78.4 (64.9–91.8) | 70.3 (57.6–83.0) | 48.6 (32.3–64.9) | 35.1 (21.2–48.9) |
| Female | 66.7 (52.1–81.3) | 61.5 (46.4–76.6) | 51.3 (35.8–66.8) | 35.9 (21.0–50.8) |
| Overall | 72.4 (62.3–82.4) | 65.8 (55.1–76.5) | 50.0 (38.7–61.2) | 35.5(24.7–46.2) |
| Third year | ||||
| Male | 85.7 (39.4–100) | 85.7 (30.6–100) | 71.4 (12.9–87.0) | 57.1 (0.1–70.9) |
| Female | 63.0 (44.7–81.2) | 55.6 (36.8–74.3) | 33.4 (15.6–51.2) | 25.9 (9.4–42.4) |
| Overall | 67.6 (51.9–83.3) | 61.8 (45.5–83.9) | 41.2 (24.6–57.7) | 32.4 (48.1–16.7) |
| Fourth year | ||||
| Male | 75.0 (57.7–92.3) | 66.7 (47.8–85.5) | 45.8 (25.9–65.7) | 16.7 (1.8–31.6) |
| Female | 86.1 (74.7–97.4) | 83.3 (71.1–95.5) | 63.9 (48.2–79.5) | 41.7 (25.6–57.8) |
| Overall | 81.7 (71.9–91.5) | 76.7 (66.0–77.4) | 56.7 (44.2–69.2) | 31.7 (19.9–43.5) |
| Total sample | 69.2 (63.4–75.0) | 63.2 (57.1–69.3) | 44.4 (38.1–50.7) | 27.6 (21.9–33.2) |
| Chi Square (p value) describing linearity of trend | ||||
| • Overall | 7.9 (0.005) | 8.2 (0.004) | 7.1 (0.008) | 4.1 (0.04) |
| • Females | 5.1 (0.02) | 6.2 (0.01) | 7.1 (0.007) | 7.4 (0.006) |
| • Males | 2.7 (0.09) | 2.0 (0.15) | 0.7 (0.4) | 0.1 (0.7) |
Figure 1.
The frequency of LBP reported in the context of 12 month prevalence of LBP
Considering subjects' responses to all categories of LBP prevalence (LBP ever, LBP in the previous 12 months, LBP in the previous month and LBP in the previous week) we found that 30.8% subjects reported never having experienced LBP, 5.2% students reported experiencing LBP earlier in their life, but not in the last 12 months, 19.6% students reported LBP within the past 12 months (but not in the last month), 17.6% students reported experiencing LBP in the past month (but not the past week), and 27.2% students experienced LBP in the past month as well as the past week.
Year level and gender exposure
Table 4 illustrates that, compared with the first year students, all other year levels of students incurred significantly elevated risk of one-week prevalence of LBP. The fourth year students also demonstrated significant elevation of risk for all other measures of LBP (lifetime, 12-month, one-month as well as one-week prevalence).
Table 4.
Risk ratio of LBP occurring in each year level compared with the first year students (RR = 1)
| Year Level | Prevalence | Overall Risk Ratio (95%CI) | Gender-specific Risk Ratios (95%CI) | |
| Female | Male | |||
| Fourth Year Students | Lifetime | 1.4 (1.1–1.8)++ | 1.4 (1.1–1.8)++ | 1.6 (0.9–2.6) |
| 12-month | 1.5 (1.2–1.9)++ | 2.1 (1.3–3.3)++ | 1.6 (0.9–2.7) | |
| 1-month | 1.8 (1.2–2.7)++ | 1.5 (1.2–2.0)++ | 1.4 (0.6–2.9) | |
| 1-week | 2.1 (1.1–4.0)++ | 1.4 (1.1–1.8)++ | 0.9 (0.2–3.1) | |
| Third Year Students | Lifetime | 1.2 (0.9–1.6) | 1.0 (0.7–1.5) | 1.8 (1.0–3.1)* |
| 12-month | 1.2 (0.9–1.7) | 1.0 (0.7–1.5) | 2.0 (1.1–3.6)++ | |
| 1-month | 1.3 (0.8–2.2) | 1.1 (0.6–2.1) | 2.1 (1.0–4.6)* | |
| 1-week | 2.2 (1.1–4.4)++ | 1.1 (0.8–4.7) | 3.0 (1.0–8.9)* | |
| Second Year Students | Lifetime | 1.3 (1.0–1.6)* | 1.1 (0.8–1.5) | 1.6 (1.0–2.7)* |
| 12-month | 1.3 (1.0–1.7)* | 1.1 (0.8–1.6) | 1.6 (1.0–2.8)* | |
| 1-month | 1.6 (1.0–2.4)* | 1.7 (1.0–2.7)* | 1.5 (0.7–2.9) | |
| 1-week | 3.1 (1.4–7.3)++ | 2.6 (1.2–5.7)++ | 1.8 (0.7–4.9) | |
There were differences in gender-specific risk of LBP. Females in fourth year sustained a significantly elevated risk of all measures of LBP compared with first year females, whilst there was no difference in risk of any measure of LBP for males in these year levels. In contrast, males in second and third year showed a consistent increase in risk in most measures of LBP compared with first year males, whilst females in second and third year levels generally showed no difference in LBP risk. The significant increase in one-week prevalence in second year females compared with first year females may reflect a chance finding, or an artifact of the data.
The significance of the overall, and gender-specific findings needs to be interpreted with caution due to the low number of third year students overall, and the low number of males in the second and third year levels. Moreover, whilst these analyses suggest a significantly increased LBP risk once students complete first year, the general overlap in confidence intervals in years 2–4 of the physiotherapy program for all measures of LBP (overall, and in gender-strata) suggests a non-significant year-by-year increase in risk after first year.
Putative exposures
Table 5 reports on the association between LBP and proposed exposures, highlighting in bold the associations that were significant, or trended towards significance (where confidence intervals skimmed 1). Four were of note.
Table 5.
Risk estimates of putative exposures (OR and 95%CI)
| N | Lifetime LBP | 12 month LBP | 1 month LBP | 1 week LBP | |
| Age | |||||
| 18 or less years | 51 | 1 | 1 | 1 | 1 |
| 19 years | 62 | 1.6 (0.7–3.4) | 1.7 (0.8–3.5) | 2.2 (0.9–5.0) | 2.0 (0.8–5.1) |
| 20 years | 46 | 2.9 (1.2–7.2) | 3.6 (1.5–8.7) | 4.5 (1.9–10.8) | 3.4 (1.3–9.0_ |
| 21 years | 42 | 3.0 (1.2–7.6) | 3.2 (1.3–7.6) | 3.5 (1.5–8.5) | 2.4 (1.0–6.5) |
| 22 years | 14 | 2.0 (0.6–7.4) | 1.5 (0.4–4.9) | 0.5 (0.1–2.5) | 0.9 (0.7–4.8) |
| 23+ years | 35 | 2.0 (0.8–5.1) | 2.1 (0.9–5.2) | 3.1 (1.2–7.7) | 2.5 (0.9–6.9) |
| Gender | 0.9 (0.5–1.6) | 0.9 (0.5–1.6) | 0.9 (0.5–1.5) | 1.0 (0.5–1.7) | |
| Occupational exposure | |||||
|
|
84 | 1 | |||
|
|
83 | 1.4 (0.5–3.9) | |||
|
|
83 | 1.3 (0.8–1.6) | |||
| Sports Exposure | |||||
|
|
84 | 1 | |||
|
|
83 | 0.9 (0.4–1.8) | |||
|
|
83 | 1.2 (0.9–1.5) | |||
| Length of study >1 | 175 | 2.4 (1.2–5.0) | 2.3 (1.4–2.6) | 2.0 (1.1–3.6) | 1.2 (0.7–2.4) |
| Height >171 cm | 172 | 1.1 (0.3–4.2) | |||
| Weight >63 kgs | 176 | 1.1 (0.5–2.2) | |||
| BMI > 21.25 | 177 | 1.3 (0.7–2.2) | |||
| Fitness | |||||
|
|
29 | 1 | 1 | 1 | |
|
|
132 | 1.8 (0.8–4.1) | 1.7 (0.6–3.7) | 2.2 (0.8–6.1) | |
|
|
89 | 1.6 (0.7–3.7) | 1.3 (0.6–3.2) | 1.7 (0.6–4.9) | |
| Educational exposures | |||||
|
|
55 | 0.8 (0.5–1.4) | 0.7 (0.4–1.3) | ||
|
|
58 | 2.4 (1.4–4.1) | 1.7 (0.9–3.1) | ||
|
|
102 | 1.5 (0.9–2.7) | 1.3 (0.7–2.4) | ||
|
|
98 | 1.9 (0.9–3.6) | 1.7 (0.8–3.4) | ||
|
|
126 | 1.9 (1.1–3.6) | 2.1 (1.1–4.1) |
Age
Students aged 20 and 21 years demonstrated significantly higher risk of all measures of LBP compared with the youngest students (18 years or younger). Gender-specific analysis confirmed the elevated risk for males in both age groups across all measures of LBP prevalence, but females aged 20 and 21 years demonstrated elevated risk of LBP prevalence only in the prevalence categories of one-month and one-week. Further exploring this finding, overall, and in gender-strata, we found no significant difference in age for males or females for any of the prevalence measures of LBP. The overall age of students without pain was 19.8 years (95%CI 19.3–20.3), compared with students with any pain (average age 20.2 years (95%CI 19.5–23.6). Males with, and without any measure of LBP were aged respectively 21.0 years (95%CI 20.2–21.8) and 20.3 years (95%CI 19.3–21.4). Females without LBP were aged 19.6 years (95%CI 19.0–20.1) whilst females with LBP were aged 20.1 (95% 19.5–20.6).
Length of study
Length of university study was significantly associated with lifetime, 12-month and one-month prevalence of LBP, with students reporting LBP being involved in tertiary study for significantly longer. Analysis of the 12-month prevalence data is most meaningful in this instance. Overall, students reporting LBP in the previous twelve months had been studying at university on average for 1.5 years (SD 1.3), which was significantly longer than those without LBP in the previous 12 months (1.0 years (SD 1.1)) (independent Student t-test p-value 0.001). The importance of this finding continued in gender-specific analysis, where for females, the length of total study for students with 12-month LBP prevalence was 1.4 years (SD 1.3) compared with non-LBP sufferers (0.9 years (SD 1.1) (independent Student t-test p = 0.02)). For males, the length of university study for 12-month LBP sufferers was 1.8 years (SD 1.3) compared with non-LBP sufferers (1.2 years (SD 1.2) (independent Student t-test p = 0.03)). This concurs with the previous findings of LBP risk in the university year levels.
Exposure to educational activities
Exposure to the educational activity of 'sitting looking down' for more than 20 hours in the past month was significantly associated with reports of one-month prevalence of LBP. 'Treating patients' for more than 20 hours in the past month was associated with reports of one-month, as well as one-week prevalence of LBP. When considered in gender-specific strata:
 the significance of the finding regarding sitting looking down with one-month LBP prevalence remained significant for both males and females (respectively OR 3.4 (95%CI 1.4–8.4), and OR 2.2 (95% CI 1.1–4.5)).
the significance of the finding regarding sitting looking down with one-month LBP prevalence remained significant for both males and females (respectively OR 3.4 (95%CI 1.4–8.4), and OR 2.2 (95% CI 1.1–4.5)).
 the finding regarding treating patients with one-month LBP prevalence remained significant for males (OR 3.0 (95% 1.0–8.8) but not for females (OR 1.5 (95% 0.7–3.3))
the finding regarding treating patients with one-month LBP prevalence remained significant for males (OR 3.0 (95% 1.0–8.8) but not for females (OR 1.5 (95% 0.7–3.3))
 the finding regarding treating patients for one-week LBP prevalence did not retain its significance for either males (OR 2.0 (95% 0.7–6.5) or females (OR 2.1 (95% 0.9–4.8)).
the finding regarding treating patients for one-week LBP prevalence did not retain its significance for either males (OR 2.0 (95% 0.7–6.5) or females (OR 2.1 (95% 0.9–4.8)).
Discussion
This is the first known study that reports on LBP prevalence and associated exposures in undergraduate physiotherapy students in one Australian tertiary institution. The findings of this study suggest LBP is a reality for many physiotherapy students, and it could be proposed that new graduates from this sample may now be entering the workplace with existing LBP.
Response rates
The response to this survey was reasonable, with the third year student response being attenuated by poor attendance at the data-collection lecture (although over 90% of the third year students who attended the lecture completed the questionnaire). The non-responding students were unable to attend the data collection class because of delays in earlier classes. There was no reason to suspect that the non-responders in any year level would have completed the survey differently than the responders. There is high academic criteria for entering this program, and the highly competitive nature of assessment suggests that all students are similarly committed to the study requirements of their program year. Moreover, the response rate gender-proportions were no different from the gender-proportions of enrolled students in each year level, suggesting no systematic bias in respondents.
Although there were differences in data collection methodology, we do not believe that this influenced the results, as the study instrument, instructions and time frame were the same for all students. The response rates by the fourth year students to the mailed survey did not differ from the response rates of the other students who completed the questionnaire at the end of a lecture. Sensitivity analysis [32,33] indicated that the sample was sufficiently powered to provide robust estimates of difference in lifetime prevalence across the year levels, although it was less well powered to detect differences in more recent estimates of LBP prevalence.
LBP prevalence
The lifetime prevalence of LBP for student physiotherapists in this study is generally higher than that reported in studies on graduate physiotherapists in Australia or internationally (see Table 6). These differences may well relate to the focus of comparison studies on work-related LBP only (using different descriptions of LBP), and collecting LBP experiences from older physiotherapists, which may attenuate the high prevalence of LBP reported by students or young graduates. However, the reported 12-month prevalence in our study is similar to that reported by Cromie et al [22], an Australian study using a similar definition of LBP, and measuring 12 month prevalence of LBP in binary terms. This suggests that once LBP is first experienced, it is a common feature of life for many physiotherapy students and graduates.
Age
In our sample, being aged 20 or 21 years was a significant contributor to LBP prevalence. Considering those students who progressed through the physiotherapy program immediately after leaving high school (aged 17–23 years), the relationship between age and length of study was linear (r2 = 0.21). Thus, the 20–21 year old students would generally be in the final year of the physiotherapy program, and these findings concur with the elevated risk of LBP for the fourth year students compared with the first year students. However, the association with length of study for all subjects in the sample (from 17 to 35 years) is less convincing (r2 = 0.09), as eight percent of students aged 22 and over years commenced study after a number of years in the workforce (on average 6.7 working years (SD 2.4)). The average length of tertiary study for these mature aged students was 1.8 years (SD 1.6). Thus, we contend that while the older students may have been exposed to greater occupational and sport lifetime hazards than their younger counterparts, they may consequently have developed an enhanced ability to withstand workplace injury risk [21-24].
Occupational, sports and educational exposures
Our study found no association with any prevalence of LBP of lifetime recalled cumulative sporting and occupational exposures. Although these exposures were significantly and positively associated with age (r2 values of 0.56 and 0.61 respectively), the method of capturing and calculating exposure may well have attenuated potential associations. Physiotherapy students are believed to be involved in a variety of employment whilst studying, and many of the mature aged students worked at a range of occupations prior to entering the physiotherapy program.
The significance of the association of the educational exposure 'treating patients' at one-month and one-week LBP prevalence is related to increasing years of study only in the sense that none of the first or second year students reported this exposure. This concurs with the structure of the undergraduate physiotherapy program in the participating institution. There was also no increase in risk related to 'sitting looking down' across the years of study, as the students' year of exposure to the physiotherapy program was not significantly related to the association between this educational exposure and LBP in the previous month. Despite being reported to be an important element in undergraduate physiotherapy education [23], manual handling was not specifically measured in this study as an educational exposure. The survey questions related to educational exposures were generated by the students themselves (during the focus groups that developed and validated the questionnaire). The educational questions were based on student perceptions of their common educational activities. Only one educational category, 'treating patients', potentially contained elements of the variable working postures and manual handling activities that are associated with patient care [23,24]. Question construction in this survey potentially highlights students' limited knowledge of workplace exposures.
The strong association between educational posture of 'sitting looking down' and one-month prevalence of LBP suggests that exposure to general undergraduate university student experiences could contribute to student physiotherapist LBP. Thus, further studies are required to test the prevalence of LBP in other undergraduate student groups. Important educational exposures could well incorporate aspects of university life that were not measured in this study, such as repeated exposure to (for instance) poor sitting and standing postures, stress, frequency and severity of injury, eating and recreational habits. It seems important therefore to further test in controlled comparison studies, whether physiotherapy students are more at risk of LBP than any other group of university students when undertaking educational activities.
Potential measurement error
Quantification of exposure, and measurement error in estimating exposures to educational activities, occupation and sport and fitness levels needs to be considered, as the associations with LBP may have occurred by chance, and may reflect artefacts in our estimation of risk. Further research is required to develop better measures of undergraduate physiotherapy training exposures, lifetime occupational and sports exposures, and a better understanding of the forces on the spine resulting from these exposures related to LBP. This study may also have been improved had we been able to quantify exposure to recognised physical risk factors for adult LBP in the undergraduate educational setting (such as twisting, lifting, manual handling etc), and to determine intra- and inter-individual variability in these activities [22,24,41]. The characterisation of exposure to workplace factors is however, frequently constrained by the multiple physical demands of many workplace tasks, whose inter-relationships are not well understood [26,35,36]. Moreover, comparisons of self-reported questionnaire assessments with observational data have shown poor agreement for factors such as the average duration of time spent standing, sitting, lifting and bending and/or rotating the trunk [35-37,42]. Thus it appears that questions on duration of time spent in particular occupational positions may be difficult to answer accurately using any current data collection approach.
Commencement of LBP
It is of note that most LBP in our sample was reported as commencing in mid-teens, with the most common onset related to sport. As the teenage years are often a time of intense physical growth [39,40], the potential for lifetime experiences of LBP to commence at this time needs to be carefully considered with a view to reducing adulthood LBP incidence. Thus, a better understanding is required of how age-related experiences, environmental factors, physical activity and individual physical growth relate to LBP, before the effect of 'age' alone can be understood. In retrospect, we should have asked for more recent information about sport and occupational exposures that could have allowed us to calculate not only lifetime exposure for both measures (for association with the lifetime LBP measure), but more recent exposures to correlate with the relevant LBP prevalence measures. In this way we may have gained a more robust understanding of LBP related to sport and occupation.
Time frame of data collection
Ideally in studies such as this, data should be collected at the one point in time, and in the same manner, to ensure the same length of exposure to the demands of each physiotherapy student year, and the same potential for error (or bias) in response. This was not possible for this study due to timetable constraints. We recommend that future surveys of this nature should be conducted at the end of the student year, possibly in examination week. This would ensure a full year of educational exposures for each year level and recognition by students of all likely workplace occupational exposures, thus enabling all students to have the opportunity to participate in data collection in the same manner at the same time.
Conclusion
LBP was experienced regularly by a significant number of physiotherapy students in each year level of one university undergraduate training program. The risk of LBP for students in years 2–4 of the program was significantly greater compared with that for students in the first year of the program. Students aged 20 and 21 were more at risk of LBP than younger or older students. Students aged 20–21 mostly reflected those students who had entered the physiotherapy program straight from high school, and were in the final year of the program. They had thus been enrolled in the undergraduate program for the longest. Concurring with this was that students with more than two years of tertiary education were significantly more likely to experience LBP in the previous 12 months than students with less exposure. Educational exposures of 'sitting looking down' and 'treating patients' were related to recent occurrence of LBP.
It thus seems sensible that training is offered at the commencement of the first year of the physiotherapy program on profession-specific and personal aspects of occupational health and safety. On the basis of the data presented in this paper, the high frequency of LBP reportedly suffered by young graduate physiotherapists, and the high personal, medical and societal costs of workplace injury, every effort should be made to ensure that graduates enter the physiotherapy profession not only with minimum experience of LBP, but also being aware of the risks entailed in working in the physiotherapy profession. Given that 'sitting looking down' could also be a risk factor for LBP for other university students, further investigation of LBP causes in university students is required. It may well be found that all undergraduate students require similar instruction related to their chosen profession.
Competing Interests
The authors have received no reimbursements, fees, funding, or salary from an organization for the research reported in this paper, now will they gain from publication of this paper. The authors have not held any stocks or shares in an organization that may in any way gain or lose financially from the publication of this paper. The authors have no other financial competing interests. The authors have no non-financial competing interests in relation to publication of this paper.
Authors Contributions
Both authors contributed equally in the conception and design of this study, the analysis of data, reporting and preparation of the paper.
List of Abbreviations
LBP = low back pain
Pre-publication history
The pre-publication history for this paper can be accessed here:
Supplementary Material
Contributor Information
Leah Jane Nyland, Private physiotherapy practitioner, Email: eahnyland@hotmail.com.
Karen Anne Grimmer, Director, Email: karen.grimmer@unisa.edu.au.
References
- Biering-Sorensen F. A prospective study of low back pain in a general population. Scandinavian Journal of Rehabilitation Medicine. 1983;15:71–79. [PubMed] [Google Scholar]
- Cassidy JD, Carroll LJ, Cote P. The Saskatchewan health and back pain survey: the prevalence of low back pain and related disability in Saskatchewan adults. Spine. 1998;23:1860–1867. doi: 10.1097/00007632-199809010-00012. [DOI] [PubMed] [Google Scholar]
- Leboeuf-Yde C, Klougart N, Lauritsen T. How common is low back pain in the Nordic population? Spine. 1996;21:1518–1526. doi: 10.1097/00007632-199607010-00005. [DOI] [PubMed] [Google Scholar]
- Matsui H, Maeda A, Tsuji H, Naruse Y. Risk indicators of low back pain among workers in Japan: association of familial and physical factors with low back pain. Spine. 1997;22:1242–1248. doi: 10.1097/00007632-199706010-00014. [DOI] [PubMed] [Google Scholar]
- Papageorgiou AC, Croft PR, Ferry S, Jayson MIV, Silman AJ. Estimating the prevalence of low back pain in the general population: evidence from the South Manchester pain survey. Spine. 1995;20:1889–1894. doi: 10.1097/00007632-199509000-00009. [DOI] [PubMed] [Google Scholar]
- Suadicani P, Hansen K, Gyntelberg F. Low back pain in steelplant workers. Occupational Medicine. 1994;44:217–221. doi: 10.1093/occmed/44.4.217. [DOI] [PubMed] [Google Scholar]
- Walsh K, Varnes N, Osmond C, Styles R, Coggon D. Occupational causes of low-back pain. Scandinavian Journal of Work and Environmental Health. 1989;15:54–59. doi: 10.5271/sjweh.1891. [DOI] [PubMed] [Google Scholar]
- Kelsey JL, Golden AL, Mundt DJ. Low back pain/prolapsed lumbar intervertebral disc. Rheumatic Disease Clinics of North America. 1990;16:699–715. [PubMed] [Google Scholar]
- Gluck JV, Oleinick A. Claim rates of compensible back injuries by age, gender, occupation and industry: do they relate to return-to-work experience? Spine. 1998;23:1572–1587. doi: 10.1097/00007632-199807150-00013. [DOI] [PubMed] [Google Scholar]
- Ingemarsson AH, Sivik T, Nordholm L. Sick leave among patients withlumbar and cervical pain: relationship to previous sick leave, education, nationality, sleep disturbance and experience of pain. Physiotherapy Theory and Practice. 1996;12:143–149. [Google Scholar]
- Australian Bureau of Statistics National Health Survey 3464_0. 2001.
- Andersson GBJ. Epidemiologic aspects on low-back pain in industry. Spine. 1981;6:53–60. doi: 10.1097/00007632-198101000-00013. [DOI] [PubMed] [Google Scholar]
- Riihimaki H. Low-back pain, its origin and risk indicators. Scandinavian Journal of Work and Environmental Health. 1991;17:81–90. [PubMed] [Google Scholar]
- Shelerud R. Epidemiology of occupational low back pain. Occupational Medicine: State of the Art Reviews. 1998;13:1–22. [PubMed] [Google Scholar]
- Magora A. Investigation of the relation between low back pain and occupation. 6. Medical history and symptoms. Scandinavian Journal of Rehabilitation Medicine. 1974;6:81–88. [PubMed] [Google Scholar]
- Grimmer K, Kerr J, Hughes K, Trott P, Pitt M. An Overview of the Australian Physiotherapy Association Accredited Practice Data Collection 1995–6. Australian Journal of Physiotherapy. 1998;44:61–63. doi: 10.1016/s0004-9514(14)60367-6. [DOI] [PubMed] [Google Scholar]
- Mierzejewski M, Kumar S. Prevalence of low back pain among physicaltherapists in Edmonton, Canada. Disability and Rehabilitation. 1997;19:309–317. doi: 10.3109/09638289709166544. [DOI] [PubMed] [Google Scholar]
- Molumphy M, Unger B, Jensen GM, Lopopolo RB. Incidence of work-related low-back pain in physical therapists. Physical Therapy. 1985;65:482–486. doi: 10.1093/ptj/65.4.482. [DOI] [PubMed] [Google Scholar]
- Scholey M, Hair MD. The problem of back pain in physiotherapists. Physiotherapy Practice. 1989;5:183–192. [Google Scholar]
- Scholey M, Hair MD. Back pain in physiotherapists involved in back care education. Ergonomics. 1989;32:179–190. doi: 10.1080/00140138908966078. [DOI] [PubMed] [Google Scholar]
- West D, Gardner D. Occupational injuries of physiotherapists in North and Central Queensland. Australian Journal of Physiotherapy. 2001;47:179–185. doi: 10.1016/s0004-9514(14)60265-8. [DOI] [PubMed] [Google Scholar]
- Cromie JE, Robertson VJ, Best MO. Work-related musculoskeletal disorders in physical therapists: prevalence, severity, risks and responses. Physical Therapy. 2000;80:337–351. doi: 10.1093/ptj/80.4.336. [DOI] [PubMed] [Google Scholar]
- Ellis BE. Moving and handling patients: an evaluation of current training for physiotherapy students. Physiotherapy. pp. 323–326.
- Jackson J, Liles C. Working postures and physiotherapy students. Physiotherapy. pp. 432–436.
- Bombadier C. Outcome assessments in the evaluation of treatment of spinal disorders: summary and general recommendations. Spine. 2000;25:3100–3103. doi: 10.1097/00007632-200012150-00003. [DOI] [PubMed] [Google Scholar]
- Holmstrom E, Moritz U. Low back pain – correspondence between questionnaire, interview and clinical examination. Scandinavian Journal of Rehabilitation Medicine. 1991;23:119–125. [PubMed] [Google Scholar]
- Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sorenson F, Andersson G, Jorgensen K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Applied Ergonomics. 1987;18:233–237. doi: 10.1016/0003-6870(87)90010-X. [DOI] [PubMed] [Google Scholar]
- Carmines EG, Zeller RA. Reliability and validity assessment: Quantitative applications in social science. Beverly Hills: Sage Publications; 1979. [Google Scholar]
- Staples D. Symposium on methodology: Questionnaires. Clinical Rehabilitation. 1991;5:259–264. [Google Scholar]
- Sudman S, Bradburn NM. Asking Questions: a practical guide to questionnaire design. San Fransisco: Jossey-Bass. 1983.
- Del Greco L, Walop W. Questionnaire development: 1. Formulation. CMAJ. 1987;136:583–585. [PMC free article] [PubMed] [Google Scholar]
- Del Greco L, Walop W, McCarthy RH. Questionnaire development: 2. Validity and reliability. CMAJ. 1987;137:699–700. [PMC free article] [PubMed] [Google Scholar]
- Anthony D. Understanding advanced statistics: A guide for nurses and health care researchers. Churchill Livingstone, London. 1999. pp. 208–209.
- Cohen J. Statistical power analysis for the behavioural sciences. Academic Press, New York. 1977. pp. 109–144.
- Lloyd MH, Gauld S, Soutar CA. Epidemiologic study of back pain in miners and office workers. Spine. 1986;11:136–140. doi: 10.1097/00007632-198603000-00006. [DOI] [PubMed] [Google Scholar]
- Karhu O, Kansi P, Kuorinka I. Correcting postures in industry. A practical methods for analysis. Applied Ergonomics. 1977;8:199–201. doi: 10.1016/0003-6870(77)90164-8. [DOI] [PubMed] [Google Scholar]
- Deyo RA, Tsui-Wu Y. Descriptive epidemiology of low-back pain and its related medical care in the United States. Spine. 1987;12:264–268. doi: 10.1097/00007632-198704000-00013. [DOI] [PubMed] [Google Scholar]
- Hildebrandt VH. Back pain in the working population: prevalence rates in Dutch trades and professions. Ergonomics. 1995;38:1283–1298. doi: 10.1080/00140139508925188. [DOI] [PubMed] [Google Scholar]
- Malina RM. Growth and Development: the first twenty years. Minnesota, Burgess Publishing Company. 1975.
- Tanner JM, Whitehouse RH, Marubini E, Resele LF. Adolescent growth in boys and girls. Annals of Human Biology. 1976;3:109–126. doi: 10.1080/03014467600001231. [DOI] [PubMed] [Google Scholar]
- Burdorf A. Exposure assessment of risk factors for disorders of the back in occupational epidemiology. Scandinavian Journal of Work and Environmental Health. 1992;18:1–9. doi: 10.5271/sjweh.1615. [DOI] [PubMed] [Google Scholar]
- Rossignol M, Baetz J. Task-related risk factors for spinal injury: validation of a self-administered questionnaire on hospital employees. Ergonomics. 1987;30:1531–1540. doi: 10.1080/00140138708966045. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.