Abstract
This study assessed the effect of a brief intervention aimed at reducing HIV-related stigma among service providers in China. From December 2005 to June 2006, 138 service providers from four county hospitals in the Yunnan province of China were randomly assigned into either an intervention or a control condition. HIV stigma reduction concepts were conveyed through participatory small group activities, including role-plays, games, group discussions, and testimony by an HIV advocate. Participants were assessed at baseline before the intervention, and at 3- and 6-month follow-ups. Data were analyzed using a logistic regression mixed-effects model. Service providers in the brief intervention condition were significantly more likely to report better protection of patients' confidentiality and right to HIV testing, lower levels of negative feelings toward people living with HIV/AIDS, and more accurate understanding and practice of universal precautions. This brief intervention pilot showed potential in reducing HIV stigma and discrimination among service providers in China. Further intervention trials are needed to test the efficacy and long-term outcomes of this intervention.
Introduction
Stigma and discrimination have been identified internationally as main barriers to HIV control and prevention in every country and region of the world, posing challenges to preventing further infections, alleviating the impact, and providing adequate care, support, and treatment.1 In health care settings, HIV-related stigma discourages people living with HIV/AIDS (PLWHA) from seeking care if they previously experienced unwelcoming treatment or if their confidentiality was not respected.2,3 Previous studies have documented service providers' discriminatory attitudes and behaviors toward PLWHA and its direct negative consequences on the quality of life for PLWHA.2,4–6
Factors contributing to these stigmatizing and discriminatory responses include lack of knowledge, such as basic knowledge of HIV/AIDS and universal precautions, provider attitudes, and perceptions that caring for PLWHA is pointless because HIV/AIDS is incurable.7–15 Previous stigma reduction interventions for service providers have shown improvement in knowledge about HIV/AIDS, practice of infection control, and willingness to treat PLWHA.16–20
With the increase in its estimated HIV/AIDS cases to approximately 650,000 in recent years,21 China has implemented many national programs to fight the problem of HIV/AIDS including interventions aimed at reducing HIV-related stigma among providers. Many of these interventions follow a traditional training style using passive didactic formats with large groups of service providers attending a lecture, and do not involve any active participation by the trainees.22 In contrast, small group behavioral interventions emphasize learning through active participation in role-plays, group discussions, and other interactive activities.23 In the United States, this strategy has been proven effective in promoting desired behaviors with various populations.23–25
The present study was conducted as part of a multiyear project and involved a brief behavioral intervention pilot intended to reduce stigma and increase level of comfort working with PLWHA for service providers in China. The intervention incorporated role-plays, group discussions, games, HIV advocate testimony, and presentation from a physician specialized in AIDS care. Intervention facilitators came from various backgrounds including local government health educators, nongovernment organization (NGO) intervention specialists, and project staff. The intervention pilot is unique in China because of its participatory format and its focus on stigma reduction in the health care setting.
Methods
Participants and recruitment
The original study was conducted in Yunnan province, which has the highest number of reported HIV infections among all the provinces of China.26,27 The study phases consisted of a qualitative formative study, quantitative assessment study, and an intervention pilot study aimed at reducing HIV-related stigma among service providers. This paper will focus on findings from the intervention pilot.
From December 2005 to June 2006, the intervention pilot was conducted with a two-arm design whereby participants were randomized into an intervention arm and a control arm. Attitude and behavioral assessment data were collected at baseline, and 3- and 6-month follow-ups. Study participants were service providers, consisting of doctors, nurses, and lab technicians from four county hospitals. Employment at the selected hospitals and willingness to participate were the only inclusion criteria. Two of the county hospitals were randomly assigned to the intervention condition, and the other two to the control condition. Providers in the control condition completed the same study assessments at the same time as the intervention participants. In addition, some of the control participants received HIV/AIDS trainings conducted by their hospitals during the course of the study, but none received the brief intervention under the study.
Project staff approached potential participants at each of the hospitals, explained the project, and distributed informational materials. Contrasting from the traditional “training,” this study was framed as a “round table discussion” in order to reduce resistance to conventional training and emphasize the participatory style of this small group intervention. Informed consent was secured by a research staff in a private office, and participants were compensated with a gift equivalent to 40 Yuan (about $5 dollars) for completion of each assessment. Study participation was completely voluntary. All materials and procedures that were used had been approved by IRB at both UCLA and China CDC. To gain administrative support, such as approval of time away to participate in the intervention, hospital administrators were contacted by research staff with information about the study.
Data collection and measures
Data were collected using paper-and-pencil self-administered assessments at baseline and at 3 and 6 months after the completion of the intervention. Baseline response rate was 86%. Follow-up rates at 3 and 6 months were high at 98% and 97%, respectively. In these surveys, data were gathered on demographics, HIV-related training, contact with PLWHA, and attitude and behavior toward PLWHA. To assess attitude and behavior, participants indicated their agreement/disagreement with a series of statements using the response categories of “agree”, “not sure,” and “disagree.” There were three primary statements assessing provider's attitudes toward confidentiality protection, patients' right to HIV testing, provider's discriminatory attitude, and knowledge about universal precautions. The statements were: “It is okay if the provider discloses the HIV status of a patient to his/her family members”; “If a patient refuses to provide informed consent for HIV testing, the doctor should have the right to make the final decision about whether to give the patient an HIV test”; and “You feel afraid of PLWHA.” The survey also assessed providers' understanding and practice of universal precautions by asking the following question, adapted from the USAID HIV/AIDS-related stigma and discrimination indicators development workshop (2004): “When measuring the blood pressure of a PLWHA, should a health care professional wear gloves to protect his or her self from being infected with HIV?” (with response categories “yes” or “no”). This indirect evaluation has shown greater validity in assessing participants' knowledge of universal precautions.28
Brief intervention
A Community Advisory Board (CAB) was formed to provide consultation on cultural appropriateness and applicability of the intervention design for this population. The CAB was composed of officials from the provincial Health Bureau, health providers and administrators from county hospitals, administrators from local Centers for Disease Prevention and Control (CDC), intervention specialists from a local NGO, and persons living with HIV/AIDS. Before assessments and interventions were conducted, revisions were made according to suggestions provided by the CAB. Initially the intervention comprised four sessions. After consulting with the CAB, the intervention was redesigned into one 4-hour session with a 15-minute break.
The contents of the intervention were identified and developed based on findings from earlier phases of qualitative and quantitative studies. We had learned that HIV-related stigma in health care was related to a number of sociocultural, structural, and personal factors. To be effective, an intervention to combat stigma must address issues on awareness of HIV policies and procedures, ensure access to universal precautions and postexposure prophylaxis, improve knowledge of HIV transmission, and increase level of comfort working with PLWHA. At the same time, the intervention must be culturally appropriate for the population and logistically feasible to be carried out and sustained.
The intervention session includes 15 service provider participants who sat in a large circle facing the facilitators. The session was designed to be highly interactive. After a brief introduction of the project by a facilitator, participants join a game called “Rescue Mission” that focuses on equal medical treatment to everyone regardless of their social status, type of disease, or infection routes. A testimony by 2 HIV advocates follows the game. Participants are then separated into smaller groups of 5 persons each to discuss commonly heard or seen language, attitudes, and behaviors in a medical setting that can be discriminatory and to explore ways to change them. After the small group discussion, participants engage in two rounds of a role-play session called “Discrimination among us,” which emphasizes the prevalence of discrimination in society and how it can make everyone a potential victim. Facilitators and provider participants take turns and play the roles of a PLWHA, family members, and providers to show how provider discrimination can harm personal feelings and family relations. Then, one of the facilitators, who is a physician specializing in AIDS care, talks about first-hand experiences of overcoming difficult situations in their daily medical practice. To conclude the intervention, facilitators disseminate informative HIV/AIDS materials developed for the project while HIV advocates distribute gifts hand-made by PLWHA.
All facilitators participated in trainings prior to the intervention. Postintervention evaluation data were collected immediately after each intervention session to gather participants' feedback about the intervention.
Statistical analysis
Descriptive statistics for the demographic and HIV-related variables (e.g., HIV-related training and contact with PLWHA at baseline) are presented in Table 1. We compared differences in the demographic and HIV-related descriptive variables between the intervention and control groups using χ2 test for dichotomized or categorical variables and t test for continuous variables.
Table 1.
Baseline Demographic for the Intervention and Control Groups (N = 138)
| |
Group |
|
|
|---|---|---|---|
| Control | Intervention | Total | |
| N (%) | 68 (49.3) | 70 (50.7) | 138 |
| Agea (mean [SD]) | 35.0 (7.53) | 35.9 (8.41) | 35.4 (7.97) |
| Female | 55 (80.9) | 52 (74.3) | 107 (77.5) |
| Han ethnicity | 60 (84.5) | 61 (92.4) | 121 (87.7) |
| Occupation | |||
| Doctor | 28 (41.2) | 33 (47.1) | 61 (44.2) |
| Nurse | 32 (47.1) | 31 (44.3) | 63 (45.7) |
| Lab technician | 8 (11.8) | 6 (8.6) | 14 (10.1) |
| Medical education | |||
| Associate medical degree or higher | 45 (66.2) | 45 (64.3) | 90 (65.2) |
| Have contact/interact with PLWHA | 50 (73.5) | 42 (60.0) | 92 (66.7) |
| Have received HIV-related training | 67 (98.6) | 64 (91.4) | 131 (94.9) |
Two subjects did not report age.
Chi-square tests were used for all baseline variables except for age, and the t-test was used for the age variable. No significances were found. PLWHA, people living with HIV/AIDS.
To evaluate the effect of the intervention for each of the outcome measures, we used a logistic regression mixed-effects model via a generalized linear mixed-effects model, allowing for fixed and participant-level random effects, specifications of a binomial error distribution, and covariance structure. Covariates included time (measured in months), assigned intervention group, and a two-way linear and quadratic time-by-intervention interaction. The model also included participant-level random effects to account for correlation between repeated measures at baseline, and 3- and 6-month follow-up assessments. Table 2 presents the estimated odds ratios with 95% confidence intervals from the final logistic regression mixed-effects model. All analyses were performed using SAS version 9.1 (SAS Institute Inc., Cary, NC). A value of 0.05 (2-sided) was used for test of significance.
Table 2.
Comparison of Intervention vs. Control from Logistic Regression Mixed-Effects Model
| Odds ratio (95% CI) | p value | |
|---|---|---|
| Keep patients' HIV status confidential | ||
| Baseline | 2.5 (0.9, 7.4) | 0.0943 |
| 3-Month | 3.9 (1.5, 10.4) | 0.0062 |
| 6-Month | 4.5 (1.8, 11.3) | 0.0018 |
| Respect patients' rights for HIV testing | ||
| Baseline | 2.7 (0.9, 8.4) | 0.0804 |
| 3-Month | 2.2 (0.5, 5.5) | 0.1037 |
| 6-Month | 7.5 (2.9, 19.6) | <0.0001 |
| Reduce negative feelings toward PLWHA | ||
| Baseline | 1.0 (0.5, 2.1) | 0.9526 |
| 3-Month | 2.2 (1.0, 4.9) | 0.0446 |
| 6-Month | 2.4 (1.0, 5.5) | 0.0395 |
| Correctly practice universal precautions | ||
| Baseline | 1.5 (0.6, 3.8) | 0.3853 |
| 3-Month | 2.6 (1.0, 6.4) | 0.0457 |
| 6-Month | 4.9 (1.9, 12.7) | 0.0013 |
PLWHA, people living with HIV/AIDS.
Results
Table 1 summarizes demographic characteristics of the 138 service providers in the study. The average age of the sample was 35 years. Most participants were female (77.5%) and Han ethnicity (87.7%). Approximately 65% had received an associate degree or higher in medicine. Lab technicians represent 10% of the sample, and there are about equal proportions of doctor (44.2%) and nurse participants (45.7%). Close to 95% of all participants had received HIV-related training, and about two thirds reported having contact with PLWHA prior to baseline assessment.
There were no statistical differences between the intervention and control participants in terms of their age, gender, education, or previous HIV-related training. Outcome variable comparison at baseline was made using the mixed-effects model that compared the intervention group with the control group, and we found that the groups did not differ significantly on all of the variables at baseline.
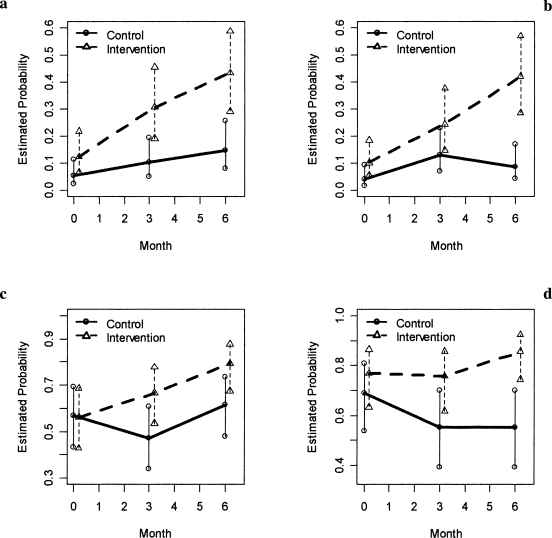
Keeping patients' HIV status confidential
The odds for agreeing with keeping patients' HIV-status confidential to family members was almost four times higher among the intervention group than among the control group at the 3-month follow-up (95% CI: 1.5–10.4; p = 0.0062); the odds were more than four times higher at the 6-month follow-up (95% CI: 1.8–11.3; p = 0.0018). The final model showed that the linear and quadratic time by intervention terms were not statistically significant. Positive time trends were observed for both groups as shown in Fig. 1a; however, service providers who received the intervention sessions were more likely to keep the patients' HIV status confidential.
FIG. 1.
Estimated probabilities over time for (a) keeping patients' HIV status confidential, (b) respecting patients' rights for HIV testing, (c) reducing negative feelings toward people living with HIV/AIDS, and (d) correctly practicing universal precautions. In each plot, the circle and solid line represent the control group and the triangular and dashed line represent the intervention group; 95% confidence intervals are also plotted.
Respecting patients' rights for HIV testing
After the intervention was implemented, the estimated probability of providers respecting patients' right for HIV testing increased over time for the intervention group, as shown in Fig. 1b, whereas that for the control group slightly increased before the 3-month follow-up and then decreased after the 3-month follow-up. The odds of respecting patient's right for HIV testing at 6-month follow-up was 7.5 times higher among the intervention group than among the control group (95% CI: 2.9–19.6; p < 0.0001). As seen in Fig. 1b, the 95% CI for the two groups did not overlap at the 6-month follow-up.
Reducing negative feelings toward PLWHA
In comparison of intervention and control groups in terms of negative feelings toward PLWHA, we found that the odds for not having negative feelings toward PLWHA was 2.2 times higher among the intervention group than among the control group at 3-month follow-up (p = 0.0446); the rate was still significantly higher at the 6-month follow-up (OR = 2.4; 95% CI: 1.0–5.5; p = 0.0395).
Correctly practicing universal precautions
At the 3-month follow-up, the estimated odds for correctly practicing universal precautions was 2.6 times higher among the intervention group compared to the control group (95% CI: 1.0–6.4; p = 0.0457); the rate was almost five times higher for the intervention group at the 6-month follow-up (95% CI: 1.9, 12.7; p = 0.0013). As shown in Fig. 1d, the estimated probability of correctly practicing universal precautions among the intervention group stayed the same until the 3-month follow-up, and then started to increase after the 3-month follow-up, whereas the estimated probability decreased for the control group. Also, the 95% confidence intervals became less overlapped on and after the 3-month follow-up assessment.
Discussion
The brief intervention was designed based on findings and lessons from previous qualitative and quantitative studies. The intervention was not only implemented successfully in the health care settings in China, but also showed positive intervention outcomes. Providers in the intervention group reported stronger belief in patient confidentiality protection and patients' right to HIV testing, reduced level of fear of PLWHA, and better knowledge and practice of universal precautions. The results are significant, especially given its cultural background and the fact that China is in the era of facing a significant increase of HIV/AIDS cases.29 This poses a special challenge to providers working in the field of HIV/AIDS in China.
Unlike providers in Western culture, Chinese providers often consider disclosing a patient's condition to his/her family member(s) as their first option for test result notification, especially when the condition is of serious diagnoses or fatal prognoses, such as HIV/AIDS.30 There are clear benefits to getting the family involved including daily care of the PLWHA, sharing medical costs and psychological support; however, there are also significant negative consequences. Notifying family members first places the additional responsibilities of disclosure and counseling on the shoulders of family members, who are not equipped with sufficient knowledge to counsel on medical treatment and care. In addition to breach of patient confidentiality, studies have also shown that providers overwhelmingly endorsed mandatory HIV testing without patient consent.13,31,32 This social acceptance of breach of confidentiality and disregard of informed consent makes it particularly important to educate providers on issues pertaining to patients' rights.
Our brief intervention addressed these topics through games and role plays utilizing experiences from existing stigma reduction interventions33 as well as local examples that we learned during the study. The outcome analyses showed significantly greater respect for patients' rights to confidentiality and informed consent in the intervention group, as compared to the control condition.
Service providers in China also displayed a general attitude of fear of PLWHA. In our previous study of the 1101 service providers, more than 28% of the participants admitted that they felt afraid of PLWHA.14 Studies have found that multiple levels of factors are significantly related to this general fear and stigma, such as providers' knowledge and practice of universal precautions34–36 and providers' attitudes and opinions toward PLWHA. Among these studies, one of our previous studies also included assessment of providers working in similar county health care facilities in China.36 To address the underlying factors influencing the fear of PLWHA, this intervention incorporated components on knowledge of universal precautions and access to postexposure prophylaxis. Intervention methods involving face-to-face interactive experience with PLWHA have been shown to be effective in changing providers' negative HIV attitude and opinions.37 In applying this method, this brief intervention also invited HIV advocates to give a testimony and provided a face-to-face contact opportunity with PLWHA for the provider participants, for many of whom this a first-time experience. Compared to the control group, intervention participants showed significantly reduced level of fear of PLWHA and better understanding of universal precautions at both 3-and 6-month follow-up assessments.
Although the study's results are promising, a number of limitations must be acknowledged. First, the study sample size is small, consisting of only 138 total participants across both the control and intervention groups. Second, the study sample was recruited from county hospitals of Yunnan province, which has the highest reported HIV/AIDS cases in China, and is therefore not representative of or generalizable to all providers in China. Third, we only collected 3- and 6-month follow-up data for the outcome evaluation. An intervention trial with sufficient sample size and long-term follow-up is needed to assess the efficacy of the intervention. Finally, Chinese society is experiencing fast-paced changes everyday, and there are many other social factors that could have influenced the participants but were not measured in this study, such as mass media HIV reports and social marketing campaigns at national and local levels.
Human Participant Protection
Protocols and consent forms were approved by the institutional review boards of the University of California, Los Angeles and the China Centers for Disease Control and Prevention. Service providers participating in this study were provided with a clear description of the study protocol and signed an informed consent form.
References
- 1.Joint United Nations Programme on HIV/AIDS. Stigma and discrimination fact sheet. 2003. http://data.unaids.org/Publications/Fact-Sheets03/fs_stigma_discrimination_en.pdf?preview=true. [Jun 10;2007 ]. http://data.unaids.org/Publications/Fact-Sheets03/fs_stigma_discrimination_en.pdf?preview=true
- 2.Foreman M. Lyra P. Breinbauer C. Washington, DC: Pan American Health Organization; 2003. Understanding and Responding to HIV/AIDS-Related Stigma and Discrimination in the Health Sector. [Google Scholar]
- 3.Malcolm A. Aggleton P. Bronfman M. Galvao J. Mane P. Verrall J. HIV-related stigmatization and discrimination: Its forms and contexts. Crit Public Health. 1998;8:347–370. [Google Scholar]
- 4.Surlis S. Hyde A. HIV-positive patients' experiences of stigma during hospitalization. JANAC: J Assoc Nurses AIDS Care. 2001;12:68–77. doi: 10.1016/S1055-3290(06)60185-4. [DOI] [PubMed] [Google Scholar]
- 5.Khakha DC. Discrimination in health care to patients living with HIV/AIDS. Nurs J India. 2003;94:273–275. [PubMed] [Google Scholar]
- 6.Green G. Platt S. Fear and loathing in health care settings reported by people with HIV. Sociol Health Illn. 1997;19:70–92. [Google Scholar]
- 7.Daniel H. Parker R. Sexuality, Politics and AIDS in Brazil. London: Falmer Press; 1993. [Google Scholar]
- 8.Herek GM. Capitanio GP. Public reactions to AIDS in the United States, a second decade of stigma. Am J Public Health. 1993;83:574–577. doi: 10.2105/ajph.83.4.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herek G. Workshop report: AIDS & stigma. A conceptual framework and research agenda. AIDS Public Policy J. 1998;13:36–47. [PubMed] [Google Scholar]
- 10.Blendon RJ. Donelan K. Discrimination against people with AIDS. Am J Public Health. 1988;319:1022–1026. doi: 10.1056/NEJM198810133191522. [DOI] [PubMed] [Google Scholar]
- 11.Tesch BJ. Simpson DE. Kirby BD. Medical and nursing students' attitudes about AIDS issues. Acad Med. 1990;65:467–469. doi: 10.1097/00001888-199007000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Cole BL. Zhang Z. Chen CZ. HIV-related knowledge and attitudes among medical students in China. AIDS Care. 1993;5:305–312. doi: 10.1080/09540129308258613. [DOI] [PubMed] [Google Scholar]
- 13.Li L. Wu ZY. Wu S, et al. Mandatory HIV testing in China: The perception of health care providers. Int J STD AIDS. 2007;18:476–481. doi: 10.1258/095646207781147355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li L. Wu ZY. Zhao Y. Lin CQ. Detels R. Wu S. Use case vignettes to measure HIV-related stigma among health professionals. Int J STD AIDS. 2007b;36:178–184. doi: 10.1093/ije/dyl256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Joint United Nations Programme on HIV/AIDS. India: HIV and AIDS-related discrimination, stigmatization and denial. 2001. http://data.unaids.org/Publications/IRC-pub02/JC587-India_en.pdf. [Aug 24;2007 ]. http://data.unaids.org/Publications/IRC-pub02/JC587-India_en.pdf
- 16.Brown L. Macintyre K. Trujillo L. Interventions to reduce HIV/AIDS stigma: What have we learned? AIDS Educ Prev. 2003;15:49–69. doi: 10.1521/aeap.15.1.49.23844. [DOI] [PubMed] [Google Scholar]
- 17.Rutstein RM. Kershaw DL. Harwell TS. Rudy BJ. Ricksecker MA. Spence MR. Pediatric primary care provider's knowledge of HIV/AIDS care. AIDS Patient Care STDs. 1998;12:217–225. doi: 10.1089/apc.1998.12.217. [DOI] [PubMed] [Google Scholar]
- 18.Sowell R. Seals G. Wilson B. Robinson C. Evaluation of an HIV/AIDS continuing education program. J Contin Educ Nurs. 1998;29:85–93. doi: 10.3928/0022-0124-19980301-11. [DOI] [PubMed] [Google Scholar]
- 19.Buskin SE. Li L. Yin H. Yu T. McGough JP. HIV/AIDS knowledge and attitudes in Chinese medical professionals and students before and after an informational lecture on HIV/AIDS. J Public Health Manag Pract. 2002;8:38–43. doi: 10.1097/00124784-200211000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Lalonde B. Uldall KK. Huba G.J et al. Impact of HIV/AIDS education on health care provider practice: Results from nine grantees of the Special Projects of National Significance Program. Eval Health Prof. 2002;25:302–320. doi: 10.1177/0163278702025003004. [DOI] [PubMed] [Google Scholar]
- 21.China Ministry of Health, Joint United Nations Program on HIV/AIDS, World Health Organization. update on the HIV/AIDS epidemic and response in China. 2005. http://casy.org/engdocs/2005-China%20HIV-AIDS%20Estimation-English.pdf. [Aug 24;2007 ]. http://casy.org/engdocs/2005-China%20HIV-AIDS%20Estimation-English.pdf
- 22.Wu Z. Detels R. Ji G, et al. Diffusion of HIV/AIDS knowledge, positive attitudes, and behaviors through training of health professionals in China. AIDS Educ Prev. 2002;14:379–390. doi: 10.1521/aeap.14.6.379.24074. [DOI] [PubMed] [Google Scholar]
- 23.Lightfoot M. Rotheram-Borus MJ. Tevendale H. An HIV-preventive intervention for youth living with HIV. Behav Modif. 2007;31:345–363. doi: 10.1177/0145445506293787. [DOI] [PubMed] [Google Scholar]
- 24.Latkin CA. Sherman S. Knowlton A. HIV prevention among drug users: Outcome of a network-oriented peer outreach intervention. Health Psychol. 2003;22:332–339. doi: 10.1037/0278-6133.22.4.332. [DOI] [PubMed] [Google Scholar]
- 25.Purcell DW. Garfein RS. Latka MH, et al. Development, description, and acceptability of a small-group, behavioral intervention to prevent HIV and hepatitis C virus infections among young adult injection drug users. Drug Alcohol Depend. 2007;91(Suppl 1):573–580. doi: 10.1016/j.drugalcdep.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 26.State Council AIDS Working Committee Office UN Theme Group on HIV/AIDS in China. A joint assessment of HIV/AIDS prevention, treatment and care in China. Beijing, China: UN Theme Group on HIV/AIDS in China; 2004. [Aug 24;2007 ]. [Google Scholar]
- 27.U.S. Embassy. AIDS In China: Yunnan Province Confronts HIV. http://usembassy-china.org.cn/sandt/yunnanbarth.html. [Jul 12;2007 ]. http://usembassy-china.org.cn/sandt/yunnanbarth.html
- 28.United State Agency for International Development. HIV/AIDS-related stigma and discrimination indicators development workshop report. http://m-mc.org/topics/hiv_stigma/ICRW06_CanWeMeasure-HIVstigmaReport.pdf. [Jul 12;2007 ]. http://m-mc.org/topics/hiv_stigma/ICRW06_CanWeMeasure-HIVstigmaReport.pdf
- 29.Wu Z. Sullivan S. Wang Y. Rotheram-Bonus MJ. Detels R. Evolution of China's response to HIV/AIDS. Lancet. 2007;369:679–690. doi: 10.1016/S0140-6736(07)60315-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu X. Informing HIV status by service providers. China Medical Tribune – Online. http://cmt.com.cn/article/060629/a0606291804.htm. [Jul 24;2007 ]. http://cmt.com.cn/article/060629/a0606291804.htm
- 31.Chan R. Khoo L. Goh CL. A knowledge, attitudes, beliefs and practices (KABP) survey on HIV infection and AIDS among doctors and dental surgeons in Singapore. Ann Acad Med Singapore. 1997;26:581–587. [PubMed] [Google Scholar]
- 32.Grove DI. Mulligan JB. Consent, compulsion and confidentiality in relation to testing for HIV infection: The views of WA doctors. Med J Australia. 1990;152:174–178. doi: 10.5694/j.1326-5377.1990.tb125141.x. [DOI] [PubMed] [Google Scholar]
- 33.The CHANGE Project & International Center for Research on Women. Understanding and Challenging HIV Stigma: Toolkit for Action. http://changeproject.org/technical/hivaids/stigma.html. [Jul 24;2007 ]. http://changeproject.org/technical/hivaids/stigma.html
- 34.Lin CQ. Li L. Wu ZY. Wu S. Jia MH. Occupational exposure of human immunodeficiency virus (HIV) among health care providers: A qualitative study in Yunnan, China. J Int Assoc Physicians AIDS Care. 2008;7:35–41. doi: 10.1177/1545109707302089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wu S. Li L. Wu ZY, et al. Universal Precautions in the era of HIV/AIDS: Perception of health service providers in Yunnan, China. AIDS Behav. (In press). [DOI] [PMC free article] [PubMed]
- 36.Li L. Wu ZY. Wu S. Zhao Y. Jia MH. Yan ZH. HIV-related stigma in health care setting: A survey of service providers in China. AIDS Patient Care STDs. 2007;21:753–762. doi: 10.1089/apc.2006.0219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sangiwa G. FHI's contribution to HIV counseling and testing scale-up. Paper presented at: Panel discussion on expanding and diversifying HIV testing and counseling: Findings from the field sponsored by the Horizons Program; Mar 14;2007 ; Washington, D.C. [Google Scholar]