Abstract
Purpose
To develop a generic instrument for measuring short-term health status in the recovery period among patients undergoing abdominal and pelvic surgery.
Methods
Instrument content was based on qualitative data ascertained from focus groups of patients and input from an expert panel of clinicians and psychometricians. A draft questionnaire was then piloted and revised, leading to the 27-item Convalescence And Recovery Evaluation (CARE). CARE consists of 4 individually-scored domains, which were identified using factor analysis. Test-retest reliability, internal consistency, and convergent validity were assessed.
Results
Test-retest reliability was high, ranging from 0.78 for the activity domain to > 0.88 for all others. Internal consistency varied over time postoperatively, but was moderate to high for all domains throughout. Correlations between the 4 domains of CARE were low (each r ≤ 0.57). Moderate agreement was evident between CARE domains and the appropriate components of validated instruments, providing convergent validity.
Conclusions
CARE is a robust, multi-dimensional measure of convalescence after abdominal and pelvic surgery. CARE can be used to better understand the phenomenon of recovery and to measure the impact of new processes of care (e.g., surgical technology adoption) on short-term patient outcomes.
Keywords: Quality-of-life, surgery, validation, reliability
Introduction
Novel health care technologies are often introduced into clinical practice without empirical support for their use.[1] In the context of surgery, such variation from the routine can manifest as a change in technique or the use of a new device; indeed, `there is no FDA for the surgeon'.[2] New procedures often come with a hefty price tag and highly variable results, at least during their initial adoption.[3] Although innovation may offer the promise of improved quality and efficiency,[4] the implications for the patient are potentially unknown.[5] While the effectiveness of these surgical technologies is being established, the measurement of secondary endpoints, including patient-reported quality-of life,[6] would be helpful to inform both patients and clinicians as to the short-term benefits and tradeoffs of their adoption.
Many surveys can provide significant insight into issues germane to specific populations or surgical procedures (i.e., the procedure-specific approach); however, their focus tends to be appropriately directed toward themes limited to the procedure of interest. For example, the Expanded Prostate Cancer Index Composite[7]focuses on disease-specific constructs (urinary, sexual, and hormonal function and impairment) among patients treated for prostate cancer, which may not be applicable to those undergoing surgery for other indications. In contrast, generic measures of patient health have been largely insensitive to changes during surgical recovery.[8-10] Such relative equipoise among treatments, as evident in some high profile clinical trials,[8, 11, 12] may be mistakenly interpreted as a lack of differences in convalescence. As these questionnaires were not designed explicitly for measuring postoperative recovery, they may fail to capture important constructs that ultimately result in considerable ascertainment bias. Finally, the heterogeneity of indications for abdominal and pelvic surgery has limited the development of generic measures of postoperative recovery,[13-16] all of which lack construct validity and have seen little use. However, the procedure-specific approach is impractical, and the common issues facing patients undergoing abdominal surgery[17] suggest that a generic approach is possible.
For these reasons, we sought to develop a multidimensional health-related quality-of-life instrument for ascertaining health status following abdominal and pelvic surgery. The instrument is intended to be a generic measure of health status for use in the postoperative period, and is designed to supplement information garnered from pertinent procedure-specific surveys. Recognizing that technology diffusion in surgery is inevitable and has, at times, unforeseen consequences,[18] the overarching purpose behind this work is to better understand the relationship between adoption of novel processes of care and patient convalescence following abdominal and pelvic surgery.
Methods
Conceptual Framework
The initial design of our questionnaire was based on a conceptual framework that incorporated a review of the social science and clinical literature. We believe that recovery is grounded as a patient's perception of his or her own health prior to surgery, which establishes an internal standard. A variety of factors then mediate this standard, including prior illness, surgery, expectations, amelioration of symptoms and/or disease, and exposures to various external stimuli (e.g., a newspaper article regarding a specific medical condition).[19-21] Divergence between the internal standard and a subject's postoperative experiences leads to the conscious development of symptoms[22, 23] that persist until recovery is complete.[24] Multiple symptoms (e.g., pain, nausea, physical impairment) of recovery are common to a broad range of surgical procedures across disciplines.[17] Although the severity and duration of these health states are highly variable depending on the procedure, they collectively contribute to a patient's perception of health. For the purpose of this study, we defined recovery as the period of time during which the patient has measurable and dynamic changes in health status attributable to the intervention.
Instrument Design
Initial content for CARE was developed based on a thorough review of the medical and social sciences literature, and our conceptual framework of postoperative recovery. Validated instruments measuring constructs thought to be pertinent to recovery were reviewed, and the investigative team adapted questions to create new items.[25] To ensure content validity, the initial items were reviewed by 10 expert panelists, 9 whom had a clinical understanding of the recovery process (surgeons) and 6 of whom had expertise in psychometrics. The questionnaire was revised to include questions measuring mental health and more explicit descriptors of the various types of functional activity assessment.
The 51-item draft was next reviewed as a component of our in-depth focus groups to provide face validity. Focus groups consisted of 7 patients derived from one of three surgical disciplines (including urology, general surgery and gynecology) as a convenience sample. Focus groups were conducted by an experienced facilitator who was responsible for creating a psychological climate that encouraged a frank discussion of the issues,[26] and who ensured that these were covered systematically and completely.[27] The groups addressed 5 key topics, including defining the concept of recovery, characterizing the symptoms of recovery, identifying barriers to recovery, outlining the effect of recovery on other aspects of life, and timing of recovery. At the end of each session, participants reviewed a draft survey and commented on appropriateness (face and content validity), readability, and ambiguity of each item.
Next, the questionnaire was piloted in 50 patients who were recruited as a convenience sample from the urology, surgery and gynecology clinics. Responses from this pilot group were used to assess item interpretability, endorsement frequency, internal consistency, and initial factor loading. The preliminary psychometric properties were used to eliminate items, including those measuring emotional themes, vitality, sleep-related issues, constipating symptoms, and activity-related impairment. The revised questionnaire was then piloted in a separate group of 50 patients, recruited from the same clinics. Preliminary reliability checks and factor analyses were again conducted prior to the validation study.
Patients in both focus groups and pilot phases were provided a small monetary compensation for their time. To afford insight into the recovery process, all patients recruited to the focus and pilot groups were at least 90, and more than 365, days removed from their prior abdominal and pelvic surgery. Following the pilot phase, the 27-item Convalescence And Recovery Evaluation (CARE) instrument with 4 domains (pain, gastrointestinal, cognitive, and activity) was finalized for validation studies. The instrument and scoring instructions are available in appendices 1 and 2, respectively.
Validation of CARE
In the validation phase, patients scheduled to undergo abdominal or pelvic surgery were recruited as a convenience sample from the urology (n=35), general surgery (n=29) and gynecology (n=32) clinics at the University of Michigan. Patients were recruited within each clinic to be representative of general practice of that specialty and to reflect the breadth of complexity of procedures within the discipline (based on the judgment of the specialists within each discipline). All patients provided written informed consent and agreed to complete a battery of questionnaires, including CARE, preoperatively and at regular intervals postoperatively (weeks 1, 2, 4, 6 and 12). To avoid placing an excessive burden on patients, validated instruments used to ascertain concurrent and divergent validity were completed at discrete intervals rather than at all possible intervals. These measures included: the SF-12,[28] an abbreviated version of the SF-36[29] that measures general physical and mental health (administered preoperatively, and postoperatively at weeks 4 and 12); the Post-discharge Surgical Recovery Scale (PRS),[15] a uni-dimensional questionnaire designed to measure health status among surgery patients (administered preoperatively, and postoperatively at weeks 1, 2, 4, 6 and 12); and, the Symptom Distress Scale (SDS),[30] a wide-ranging questionnaire comprised of items that address issues commonly facing surgical patients, including nausea, appetite, pain, bowel patterns, mobility, and appearance (administered preoperatively, and postoperatively at weeks 2 and 6). All questionnaires were self-administered and returned by mail, with the exception of the preoperative questionnaire that was completed at the time of the preoperative surgery visit. Participants were compensated for their time.
Study staff provided phone reminders to assist patients in returning questionnaires at the appropriate intervals.
Statistical Analyses
Exploratory factor analysis was performed using varimax rotation to identify discrete domains in CARE—pain, gastrointestinal, cognition, and activity. Response options for each item form a Likert scale and the multi-item domain scores were transformed linearly into a 0 to 100 scale, which is then used to develop the composite score. In all cases, higher scores represented a better health state. Test-retest correlation coefficients were measured for a sample of patients (n=18) who were administered CARE between 12 and 14 weeks postoperatively when symptomatic improvement is thought to be complete (based on the clinical judgment of the investigative team). This group was chosen using a stratified randomization method to ensure the patients within each discipline had equal representation. The internal consistency overall and for each domain was estimated using Cronbach's alpha. Pearson correlation coefficients were calculated between each domain of CARE to assess redundancy and independence. The concurrent and divergent validity of CARE were examined by calculating correlation coefficients between the domain and composite scores of CARE and those of the appropriate validated questionnaire.
All analyses were performed using computerized software (SAS, v9.1.2, Cary, NC). All statistical testing was two-sided and p < 0.05 was considered statistically significant. The study was approved by the Institutional Review Board at the University of Michigan.
Results
Patient Characteristics
Table 1 demonstrates patient characteristics in the validation cohort (n=96) stratified by the clinic from which they were recruited. Among patients recruited from the urology clinics, the most common procedures included radical prostatectomy for prostate cancer (n=11), radical cystectomy and urinary diversion for bladder cancer (n=9), and partial or radical nephrectomy for variety of indications (n=9). Among patients recruited from the general surgery clinics, the most common procedures included bowel resections for a variety of indications (n=14), various hernia repairs (n=5), and adrenalectomy (n=3). Finally, among patients recruited from the gynecology clinics the most common procedures included hysterectomy (n=9), laparoscopy +/- ablation/excision/lysis (n=9), myomectomy for fibroids (n=6), and incontinence-related surgery (n=5).
Table 1.
Clinical Characteristics of the Validation Cohort
| Characteristic | Stratum | Surgical Discipline | ||
|---|---|---|---|---|
| Urology (n=35) | General Surgery (n=29) | Gynecology (n=32) | ||
| Mean Age, years | 63.5 | 53.1 | 23.7 | |
| No. of Comorbidities (%) | 0 | 8.6 | 31.0 | 21.9 |
| 1 | 34.3 | 27.3 | 37.5 | |
| 2 | 37.1 | 20.7 | 25.0 | |
| 3 or more | 20.0 | 20.7 | 15.6 | |
| Race (%) | White | 90.9 | 92.8 | 83.9 |
| Black | 6.1 | 3.6 | 16.1 | |
| Other | 3.0 | 3.6 | 0 | |
| Marital Status (%) | Married / Living with a Partner | 76.5 | 82.1 | 62.5 |
| Widowed | 8.8 | 3.6 | 3.1 | |
| Divorced / Separated | 11.8 | 7.1 | 12.5 | |
| Never Married | 2.9 | 7.1 | 21.9 | |
| Household Income (%) | < 20,000 | 15.2 | 7.4 | 25.8 |
| 20,000-50,000 | 24.2 | 14.8 | 35.5 | |
| 50,001-75,000 | 15.2 | 29.6 | 16.1 | |
| 75,001-150,000 | 33.3 | 29.6 | 19.4 | |
| > 150,000 | 12.1 | 18.6 | 3.2 | |
| Support Structure (%) | Extensive | 61.8 | 71.4 | 70.0 |
| Good | 29.4 | 17.9 | 20.0 | |
| Modest | 0 | 0 | 6.7 | |
| Poor | 8.8 | 10.7 | 3.3 | |
All patients completed the CARE questionnaire preoperatively and at 1, 2, 4, 6, and 12 weeks postoperatively. Among the 96 patients, 74 (77.1%) completed all 6 packets, 84 (87.5%) completed at least 5 packets, and 89 (90.6%) completed at least 3 packets of questionnaires.
Reliability
Table 2 summarizes the internal consistency of the 4 domains and the composite score for the 96 patients in the validation cohort. For the composite, gastrointestinal, cognition and activity scores, internal consistency was high with Cronbach's alpha > 0.70 for all of the assessment periods. In contrast, the internal consistency of the pain domain ranged from moderate (Cronbach's Alpha = 0.66) at postoperative week 1 to high (Cronbach's Alpha = 0.84) at postoperative week 12. Ceiling and floor effects within each domain and test-retest reliability are also illustrated in Table 2. For all domains and the composite score, test-retest reliability was excellent with intraclass correlation coefficients all above 0.70.
Table 2.
Characteristics of CARE's Composite and Domain Scores for the Validation Cohort
| Preoperative | |||||
|---|---|---|---|---|---|
| No. of Items | Mean Score (SD) | Scoring Minimum N (%) | Scoring Maximum N (%) | Cronbach's Alpha | |
| Composite | 27 | 80.0 (17.7) | - | 5 (5.9) | 0.92 |
| Domain Scores | |||||
| Pain | 9 | 83.8 (16.8) | - | 17 (18.5) | 0.78 |
| Gastrointestinal | 10 | 82.9 (19.4) | - | 26 (27.4) | 0.90 |
| Cognitive | 4 | 75.8 (28.5) | 2 (2.2) | 38 (41.3) | 0.95 |
| Activity | 4 | 74.9 (28.4) | 3 (3.2) | 31 (33.3) | 0.87 |
| Postoperative Week 1 | |||||
|---|---|---|---|---|---|
| No. of Items | Mean Score (SD) | Scoring Minimum N (%) | Scoring Maximum N (%) | Cronbach's Alpha | |
| Composite | 27 | 58.6 (15.8) | - | - | 0.87 |
| Domain Scores | |||||
| Pain | 9 | 71.3 (15.0) | - | - | 0.66 |
| Gastrointestinal | 10 | 62.9 (22.9) | 2 (2.2) | 3 (3.3) | 0.87 |
| Cognitive | 4 | 72.1 (21.8) | - | 28 (31.8) | 0.92 |
| Activity | 4 | 28.5 (21.8) | 10 (11.4) | - | 0.72 |
| Postoperative Week 2 | |||||
|---|---|---|---|---|---|
| No. of Items | Mean Score (SD) | Scoring Minimum N (%) | Scoring Maximum N (%) | Cronbach's Alpha | |
| Composite | 27 | 71.4 (15.7) | - | - | 0.90 |
| Domain Scores | |||||
| Pain | 9 | 80.8 (14.3) | - | - | 0.68 |
| Gastrointestinal | 10 | 78.5 (20.6) | - | - | 0.87 |
| Cognitive | 4 | 81.1 (24.8) | 1 (1.2) | 37 (44.6) | 0.93 |
| Activity | 4 | 43.3 (25.4) | 3 (3.7) | 3 (3.7) | 0.76 |
| Postoperative Week 4 | |||||
|---|---|---|---|---|---|
| No. of Items | Mean Score (SD) | Scoring Minimum N (%) | Scoring Maximum N (%) | Cronbach's Alpha | |
| Composite | 27 | 80.5 (15.1) | - | 2 (2.6) | 0.89 |
| Domain Scores | |||||
| Pain | 9 | 87.4 (13.2) | - | 15 (17.4) | 0.75 |
| Gastrointestinal | 10 | 87.1 (17.2) | - | 34 (39.1) | 0.86 |
| Cognitive | 4 | 83.4 (24.1) | - | 48 (60.0) | 0.95 |
| Activity | 4 | 63.6 (27.4) | 4 (4.8) | 11 (13.2) | 0.80 |
| Postoperative Week 6 | |||||
|---|---|---|---|---|---|
| No. of Items | Mean Score (SD) | Scoring Minimum N (%) | Scoring Maximum N (%) | Cronbach's Alpha | |
| Composite | 27 | 83.8 (15.4) | - | 5 (6.9) | 0.93 |
| Domain Scores | |||||
| Pain | 9 | 88.8 (13.9) | - | 19 (23.4) | 0.80 |
| Gastrointestinal | 10 | 88.4 (16.5) | - | 33 (40.2) | 0.90 |
| Cognitive | 4 | 83.8 (24.8) | 2 (2.6) | 44 (57.9) | 0.96 |
| Activity | 4 | 72.1 (23.6) | 1 (1.3) | 15 (19.0) | 0.77 |
| Postoperative Week 12 | ||||||
|---|---|---|---|---|---|---|
| No. of Items | Mean Score (SD) | Scoring Minimum N (%) | Scoring Maximum N (%) | Cronbach's Alpha | Test-Retest* | |
| Composite | 27 | 84.8 (16.5) | - | 8 (11.1) | 0.94 | 0.94 |
| Domain Scores | ||||||
| Pain | 9 | 89.7 (14.9) | - | 28 (36.8) | 0.84 | 0.95 |
| Gastrointestinal | 10 | 89.8 (15.0) | - | 38 (49.4) | 0.85 | 0.88 |
| Cognitive | 4 | 80.8 (27.0) | 2 (2.7) | 36 (49.3) | 0.96 | 0.96 |
| Activity | 4 | 81.3 (22.4) | - | 31 (40.3) | 0.82 | 0.78 |
Between 12 and 14 weeks postoperatively
Validity
Face and content validity were assessed by our expert panel and patient focus groups. The final 27-items comprising CARE represented the most highly endorsed questions measuring the constructs delineated by these groups. For example, several items were added to the questionnaire to measure cognitive ability, a construct which is measured by 4 items in the final instrument. A common and unexpected theme among focus group participants was the presence of a “brain fog” that hampered their ability to concentrate during the postoperative period. Another common complaint of the recovery process related to its adverse effects on sleeping patterns.[17] Several items were initially added to address this construct; however, during pilot testing, it became apparent that these items loaded (based on preliminary factor analysis) onto both the pain and gastrointestinal domains, suggesting that sleep issues were more reflective of these themes rather than being a unique construct.
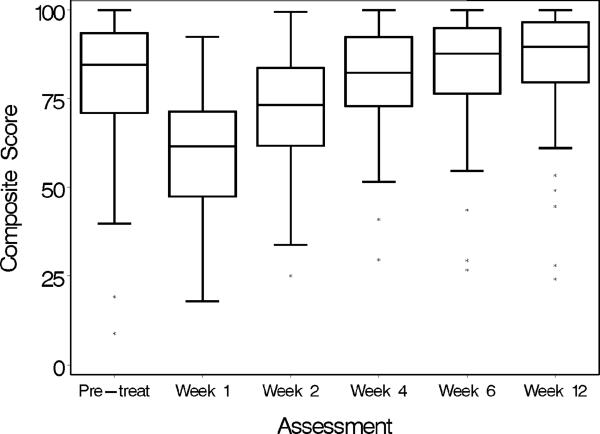
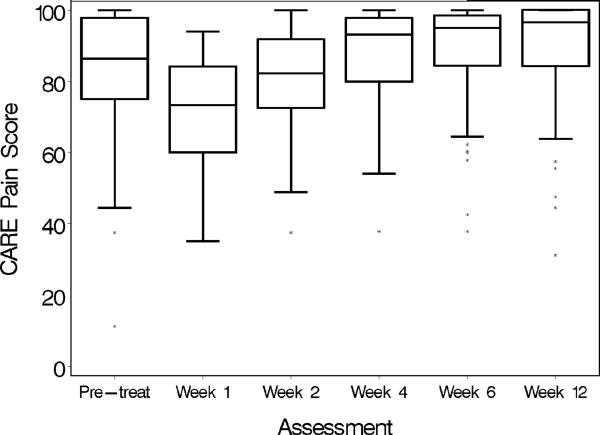
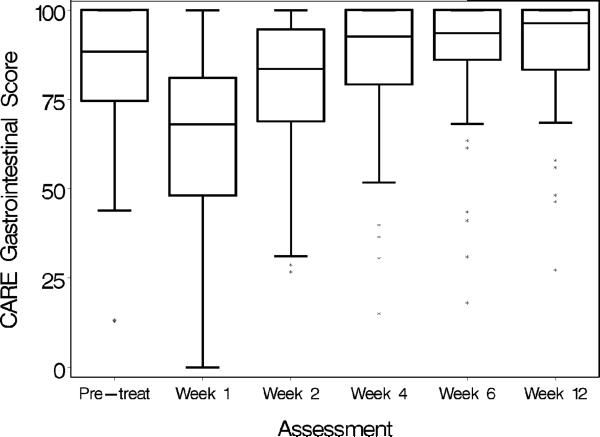
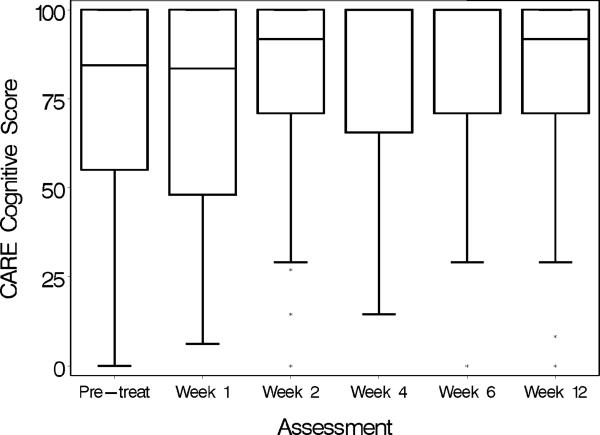
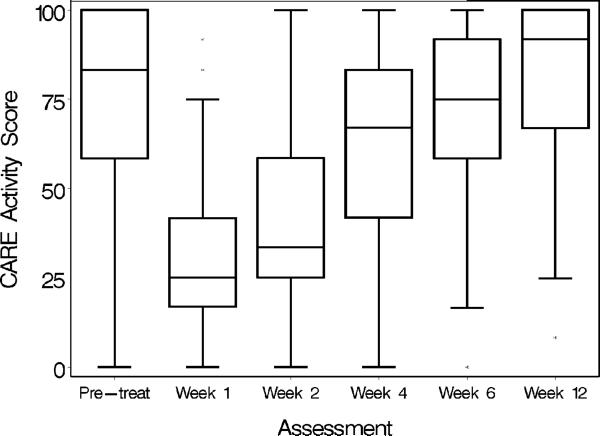
Despite the heterogeneity of the patient population comprising the validation cohort, CARE was responsive to changes in health status over time (Figure 1a-e). Table 3 illustrates the intrascale correlations between CARE domains and the composite score. Through the initial phases of postoperative recovery, intrascale correlations were low with r ≤ 0.60 through postoperative week 4 suggesting that the domains are measuring unique constructs. As recovery continues and nears completion, intrascale correlations are somewhat higher.
Figure 1.
Responsiveness of CARE (a) and its domains (b-e) to changes in health status over the 12-week period following abdominal and pelvic surgery.
Table 3.
Intrascale Correlations between CARE Composite and Domain Scores
| Quality of Life Measure | |||||
|---|---|---|---|---|---|
| Preoperative | |||||
| Composite | Pain | Gastrointestinal | Cognition | Activity | |
| Composite | 1.00 | ||||
| Pain | 0.78 | 1.00 | |||
| Gastrointestinal | 0.81 | 0.63 | 1.00 | ||
| Cognition | 0.78 | 0.58 | 0.64 | 1.00 | |
| Activity | 0.74 | 0.43 | 0.42 | 0.27 | 1.00 |
| Postoperative Week 1 | |||||
|---|---|---|---|---|---|
| Composite | Pain | Gastrointestinal | Cognition | Activity | |
| Composite | 1.00 | ||||
| Pain | 0.62 | 1.00 | |||
| Gastrointestinal | 0.76 | 0.26 | 1.00 | ||
| Cognition | 0.81 | 0.35 | 0.49 | 1.00 | |
| Activity | 0.64 | 0.30 | 0.31 | 0.26 | 1.00 |
| Postoperative Week 2 | |||||
|---|---|---|---|---|---|
| Composite | Pain | Gastrointestinal | Cognition | Activity | |
| Composite | 1.00 | ||||
| Pain | 0.73 | 1.00 | |||
| Gastrointestinal | 0.79 | 0.56 | 1.00 | ||
| Cognition | 0.77 | 0.55 | 0.50 | 1.00 | |
| Activity | 0.70 | 0.33 | 0.35 | 0.22 | 1.00 |
| Postoperative Week 4 | |||||
|---|---|---|---|---|---|
| Composite | Pain | Gastrointestinal | Cognition | Activity | |
| Composite | 1.00 | ||||
| Pain | 0.80 | 1.00 | |||
| Gastrointestinal | 0.77 | 0.42 | 1.00 | ||
| Cognition | 0.78 | 0.60 | 0.58 | 1.00 | |
| Activity | 0.76 | 0.41 | 0.46 | 0.28 | 1.00 |
| Postoperative Week 6 | |||||
|---|---|---|---|---|---|
| Composite | Pain | Gastrointestinal | Cognition | Activity | |
| Composite | 1.00 | ||||
| Pain | 0.81 | 1.00 | |||
| Gastrointestinal | 0.82 | 0.63 | 1.00 | ||
| Cognition | 0.86 | 0.69 | 0.72 | 1.00 | |
| Activity | 0.69 | 0.38 | 0.32 | 0.31 | 1.00 |
| Postoperative Week 12 | |||||
|---|---|---|---|---|---|
| Composite | Pain | Gastrointestinal | Cognition | Activity | |
| Composite | 1.00 | ||||
| Pain | 0.84 | 1.00 | |||
| Gastrointestinal | 0.83 | 0.65 | 1.00 | ||
| Cognition | 0.86 | 0.74 | 0.62 | 1.00 | |
| Activity | 0.76 | 0.48 | 0.58 | 0.42 | 1.00 |
Table 4 illustrates the relationship between the CARE composite and domain scores and those of other HRQOL measures. In the midst of recovery (postoperative week 4), the mental and physical components of the SF-12 were most highly correlated with cognition and activity domains of CARE with r = 0.67 and r = 0.73, respectively. The PRS was highly correlated with the CARE composite score throughout the recovery period with all r ≥ 0.70. Further divergent validity is provided by the high inverse correlation of CARE with the SDS.
Table 4.
Interscale Correlations between CARE Domains and HRQOL Measures
| CARE Component | Criterion Measures | ||||
|---|---|---|---|---|---|
| Preoperative | |||||
| SF-12 Mental | SF-12 Physical | Symptom Distress Scale | Post-discharge Recovery Scale | Satisfaction | |
| Composite | 0.47 | 0.60 | -0.79 | 0.64 | 0.71 |
| Pain | 0.43 | 0.65 | -0.76 | 0.70 | 0.74 |
| Gastrointestinal | 0.53 | 0.45 | -0.80 | 0.55 | 0.58 |
| Cognition | 0.65 | 0.38 | -0.71 | 0.46 | 0.68 |
| Activity | 0.09 | 0.53 | -0.38 | 0.44 | 0.34 |
| Postoperative Week 1 | |||||
|---|---|---|---|---|---|
| SF-12 Mental | SF-12 Physical | Symptom Distress Scale | Post-discharge Recovery Scale | Satisfaction | |
| Composite | - | - | - | 0.70 | 0.79 |
| Pain | - | - | - | 0.48 | 0.50 |
| Gastrointestinal | - | - | - | 0.51 | 0.59 |
| Cognition | - | - | - | 0.37 | 0.60 |
| Activity | - | - | - | 0.63 | 0.47 |
| Postoperative Week 2 | |||||
|---|---|---|---|---|---|
| SF-12 Mental | SF-12 Physical | Symptom Distress Scale | Post-discharge Recovery Scale | Satisfaction | |
| Composite | - | - | -0.79 | 0.79 | 0.77 |
| Pain | - | - | -0.66 | 0.60 | 0.60 |
| Gastrointestinal | - | - | -0.67 | 0.58 | 0.65 |
| Cognition | - | - | -0.68 | 0.46 | 0.60 |
| Activity | - | - | -0.37 | 0.56 | 0.44 |
| Postoperative Week 4 | |||||
|---|---|---|---|---|---|
| SF-12 Mental | SF-12 Physical | Symptom Distress Scale | Post-discharge Recovery Scale | Satisfaction | |
| Composite | 0.49 | 0.72 | - | 0.71 | 0.80 |
| Pain | 0.42 | 0.62 | - | 0.58 | 0.69 |
| Gastrointestinal | 0.36 | 0.44 | - | 0.46 | 0.59 |
| Cognition | 0.67 | 0.29 | - | 0.43 | 0.74 |
| Activity | 0.10 | 0.73 | - | 0.67 | 0.45 |
| Postoperative Week 6 | |||||
|---|---|---|---|---|---|
| SF-12 Mental | SF-12 Physical | Symptom Distress Scale | Post-discharge Recovery Scale | Satisfaction | |
| Composite | - | - | -0.88 | 0.82 | 0.81 |
| Pain | - | - | -0.80 | 0.72 | 0.71 |
| Gastrointestinal | - | - | -0.77 | 0.70 | 0.66 |
| Cognition | - | - | -0.83 | 0.66 | 0.49 |
| Activity | - | - | -0.45 | 0.53 | 0.49 |
| Postoperative Week 12 | |||||
|---|---|---|---|---|---|
| SF-12 Mental | SF-12 Physical | Symptom Distress Scale | Post-discharge Recovery Scale | Satisfaction | |
| Composite | 0.63 | 0.70 | - | 0.71 | 0.69 |
| Pain | 0.62 | 0.62 | - | 0.66 | 0.70 |
| Gastrointestinal | 0.58 | 0.54 | - | 0.57 | 0.59 |
| Cognition | 0.56 | 0.49 | - | 0.55 | 0.60 |
| Activity | 0.42 | 0.68 | - | 0.63 | 0.49 |
Discussion
We have developed a questionnaire for measuring postoperative convalescence that measures themes common to patients recovering from abdominal and pelvic surgery. The instrument, CARE, was prospectively validated in a diverse patient population derived from surgical disciplines that perform a variety of procedures, ranging from laparoscopy to open surgery, and is therefore applicable to a significant proportion of patients undergoing surgery. CARE assesses convalescence in four domains that are common to the wide spectrum of indications for abdominal and pelvic surgery, including pain-related issues, activity, gastrointestinal issues, and cognition. The instrument is intended to be a generic survey of surgical recovery, and is designed to supplement procedure-specific instruments for ascertaining health status after surgery. Further, the benefits or tradeoffs in recovery that are associated with perturbations in perioperative processes must be weighed against the ultimate success of the procedure based on its indications. In these contexts, CARE can be used to inform clinicians and patients about recovery following abdominal and pelvic surgery.
The robust psychometrics observed in the validation phase, particularly in predictive validity, support its role for measuring health status following abdominal and pelvic surgery. First, test-retest reliability was outstanding with an intraclass correlation coefficient of 0.94 for the composite score. Second, despite the heterogeneity of the patient population, internal consistency was generally high for all of the time periods studied. Third, the review of questionnaire content by experts and patient focus groups demonstrate CARE's content and face validity, respectively. Further, correlations of appropriate CARE domains with other validated measures illustrate their concurrent and divergent validity. For example, at 4 weeks postoperatively, correlations of the activity component of the SF-12 were considerably higher with the activity domain of CARE than for its cognitive domain (0.73 vs. 0.29).
The importance of patient-reported health status is well recognized as a facet of health care quality,[6] and is a valuable means for quantitatively measuring the implications of technology adoption for the patient, who typically judge the effectiveness of a surgical procedure by whether it improves their quality-of-life, in many cases.[31] Unfortunately, their has been little work in this realm and few validated questionnaires exist.[13-16] Some lack potentially relevant content (e.g., items pertaining to cognition).[15, 16] Others use a relatively short frame of reference (at the current time[15] to within the past 24 hours[14]) that may be too sensitive to within-patient variation thereby limiting test-retest reliability. Finally, uni-dimensional questionnaires[13, 15, 16] do not adequately account for the inherent heterogeneity of patients undergoing surgery. As garnered from our focus group interviews and other qualitative work,[17] convalescence is multifaceted and perceived as a series of milestones, which varies by procedure and perhaps with modifications of surgical technique. Thus, uni-dimensional questionnaires may average out changes in health status across conceptual domains thereby masking true differences in recovery. For these reasons, available measures of convalescence have not been widely adopted and thus have not established construct validity.
However, there is a clear need for short-term health assessment after abdominal and pelvic surgery. A recent high profile study comparing quality-of-life outcomes for laparoscopic and conventional colectomy reported minimal differences.[8] While true differences may indeed not exist, a plausible alternative is that the survey measure, in this case the SDS,[30] was insensitive to the actual changes in health status. This has led some to favor more disease-specific measures; however, for practical reasons, a generic measure of postoperative health status would be more efficient and have broader appeal. While some generic quality-of-life questionnaires (e.g., the SF-36) have demonstrated responsiveness to changes in health status after some surgical procedures,[32] the lack of similar sensitivity for other procedures[8-10] limits their widespread use. Thus, CARE, which was designed to measure constructs common to all patients after abdominal and pelvic surgery, has the potential to fill the present void in assessing health status after abdominal and pelvic procedures.
Surgery represents a considerable component of the total financial outlay for health care in the U.S.[33] The implementation of new and unproven devices and techniques accounts for a portion of this investment.[34] In some circumstances, disease-specific benefits (e.g., better potency rates after robotic prostatectomy compared to retropubic prostatectomy) are not widely evident, and the promises of the new technology are ill-defined or of unclear value (e.g., a device that makes a procedure technically easier for the surgeon). The roll-out of new devices and techniques typically comes at both a financial and opportunity cost to the patient, with the severity of the latter dictated by the consequences of the `learning curve'.[18] For example, the rapid diffusion of laparoscopic cholecystectomy in the early 1990s[35] offered dramatic convalescence benefits for many, yet ultimately resulted in nearly a three-fold increase in biliary tract injuries,[1] an unanticipated consequence.
CARE provides a reliable and valid means of quantitatively measuring these effects and also allows the investigator to assess the relative value (or cost) of perioperative processes of care to patient health status postoperatively. Further, CARE can provide quantitative feedback for the impact of complications on convalescence. For example, do complications after a procedure using a new technology abrogate all or part of its promised health benefits? Clearly, this information may temper the enthusiasm for a particular surgical innovation, and, more importantly, would provide patients and physicians with highly relevant information for decision-making.
Though we have demonstrated that CARE's robust psychometrics, these data should be interpreted with a few limitations in mind. First, our prospective validation cohort was comprised of 96 patients derived from a single institution. Although patients were recruited from 3 different surgical disciplines, future work should continue to evaluate the responsiveness of CARE to additional abdominal / pelvic surgeries, technique (e.g., laparoscopic vs. conventional), and other processes (e.g., continent vs. incontinent urinary diversion after radical cystectomy, concurrent prolapse treatment at the time of incontinence surgery) thereby establishing construct validity. Second, as with other generic measures of health status, CARE is not designed to replace the disease-specific instrument entirely. For a variety of surgical conditions, there are important health states that are very specific to that procedure (e.g., erectile dysfunction after radical prostatectomy), where disease-specific questionnaires afford valuable information. In contrast, CARE has been developed to address more global themes common to all abdominal and pelvic surgery and is intended to complement procedure-and disease- specific instruments. Lastly, CARE was not validated among children, among whom many surgical procedures are also performed.
We have developed a robust, multi-dimensional questionnaire of convalescence after abdominal and pelvic surgery. CARE was intentionally developed in a diverse patient population arising from three surgical disciplines and thus the sample sizes of those undergoing individual procedures are small. While the psychometrics of CARE are promising and suggestive of its usefulness as a means to assess recovery after surgery, further work in larger cohorts is necessary to better understand its construct validity. Our questionnaire addresses gastrointestinal-, pain-, activity-, and cognitive- related symptoms that are common to a wide spectrum of surgeries. CARE is potentially useful for quantitatively measuring the benefits and tradeoffs of adopting new surgical technologies and techniques to patient-reported convalescence.
Acknowledgments
Funding: This work was supported by a developmental grant to BKH by the George M. O'Brien Urology Research Center (1 P50 DK065313-01).
Appendices
PAIN DOMAIN
1. Over the past seven days, how much pain have you experienced in your bladder, pelvic and/or genital areas? None//Very Mild//Mild//Moderate//Severe//Very Severe
2. Over the past seven days, how much pain have you experienced in your abdominal or belly areas? None//Very Mild//Mild//Moderate//Severe//Very Severe
3. Over the past seven days, how much pain have you experienced in your flank or side areas? None//Very Mild// Mild//Moderate//Severe//Very Severe
4. Over the past seven days, how much pain have you experienced in your lung, heart and/or chest areas? None//Very Mild// Mild//Moderate//Severe//Very Severe
5. Over the past seven days, how much pain have you experienced in your arms? None//Very Mild// Mild//Moderate//Severe//Very Severe
6. Over the past seven days, how much pain have you experienced in your legs? None//Very Mild// Mild//Moderate//Severe//Very Severe
7. Over the past seven days, how much pain have you experienced in your head or neck areas? None//Very Mild// Mild//Moderate//Severe//Very Severe
8. During the last seven days, how many days have you taken non-prescription pain pills like acetaminophen (Tylenol®) or ibuprofen (Motrin® or Advil®) (0-7)?
9. During the last seven days, how many days have you taken prescription pain pills like codeine (Tylenol#3®), hydrocodone (Vicodin®), Percocet®, Darvocet®, Celebrex®, or Bextra® (0-7)?
GASTROINTESTINAL DOMAIN
10. I have had nausea over the past seven days. Strongly Disagree//Disagree//Agree//Strongly Agree; How much of a problem has nausea been for you during the past seven days? No problem//Very small problem//Small problem//Moderate problem//Big problem
11. I have had a poor appetite over the past seven days. Strongly Disagree//Disagree//Agree//Strongly Agree; How much of a problem has a poor appetite been for you during the past seven days? No problem//Very small problem//Small problem//Moderate problem//Big problem
12. I have been unable to eat over the past seven days. Strongly disagree// Disagree//Agree//Strongly Agree; How much of a problem has being unable to eat been for you during the past seven days? No problem//Very small problem//Small problem//Moderate problem//Big problem
13. I have had diarrhea over the past seven days. Strongly Disagree// Disagree//Agree//Strongly Agree; How much of a problem has diarrhea been for you during the past seven days? No problem//Very small problem//Small problem//Moderate problem//Big problem
14. I have been bloated and gassy over the past seven days. Strongly Disagree//Disagree//Agree//Strongly Agree; How much of a problem has being bloated and gassy been for you during the past seven days? No problem//Very small problem//Small problem//Moderate problem//Big problem
COGNITIVE DOMAIN
15. I have had trouble concentrating over the past seven days. Strongly Disagree//Disagree//Agree//Strongly Agree; How much of a problem has having trouble concentrating been for you during the past seven days? No problem//Very small problem//Small problem//Moderate problem//Big problem
16. I have been forgetful over the past seven days. Strongly Disagree//Disagree//Agree//Strongly Agree; How much of a problem has being forgetful been for you during the past seven days? No problem//Very small problem//Small problem//Moderate problem//Big problem
ACTIVITY DOMAIN
17. During the last seven days, I have been able to drive whenever I wanted. Strongly Disagree//Disagree//Agree//Strongly Agree//I don't drive
18. During the last seven days, I have been able to participate in light activities such as dressing myself, walking a block or climbing up a flight stairs. Strongly Disagree// Disagree//Agree//Strongly Agree
19. During the last seven days I have been able to participate in moderate activities such as moving a small table or pushing a vacuum cleaner. Strongly Disagree//Disagree// Agree//Strongly Agree//I don't participate in moderate activities
20. During the last seven days I have been able to participate in vigorous activities such as running or lifting heavy objects (25 lbs.). Strongly Disagree//Disagree//Agree//Strongly Agree//I don't participate in vigorous activities
References
- 1.Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. Journal of the American College of Surgeons. 1995;180(1) [PubMed] [Google Scholar]
- 2.Spodick DH. Numerators without denominators. There is no FDA for the surgeon. JAMA. 1975;232(1) doi: 10.1001/jama.232.1.35. [DOI] [PubMed] [Google Scholar]
- 3.Pearson SD, Rawlins MD. Quality, innovation, and value for money: NICE and the British National Health Service.[see comment] JAMA. 2005;294(20) doi: 10.1001/jama.294.20.2618. [DOI] [PubMed] [Google Scholar]
- 4.Wall LL. Innovation in surgery: caveat emptor. International Urogynecology Journal. 2001;12(6) doi: 10.1007/s001920170010. [DOI] [PubMed] [Google Scholar]
- 5.Mastroianni AC. Liability, regulation and policy in surgical innovation: the cutting edge of research and therapy. Health Matrix. 2006;16(2) [PubMed] [Google Scholar]
- 6.The National Roundtable on Health Care Quality . Measuring the Quality of Health Care. National Academy Press; Washington D.C.: 1999. [PubMed] [Google Scholar]
- 7.Wei JT, Dunn RL, Litwin MS, Sandler HM, Sanda MG. Development and validation of the expanded prostate cancer index composite (EPIC) for comprehensive assessment of health-related quality of life in men with prostate cancer. Urology. 2000;56:899–905. doi: 10.1016/s0090-4295(00)00858-x. [DOI] [PubMed] [Google Scholar]
- 8.Weeks JC, Nelson H, Gelber S, Sargent D, Schroeder G, Clinical Outcomes of Surgical Therapy (COST) Study Group Short-term quality-of-life outcomes following laparoscopic-assisted colectomy vs open colectomy for colon cancer: a randomized trial. JAMA. 2002;287:321–328. doi: 10.1001/jama.287.3.321. [DOI] [PubMed] [Google Scholar]
- 9.Litwin MS, Hays RD, Ganz PA, Leake B, Leach GE, Brook RH. Quality-of-life outcomes in men treated for localized prostate cancer.[comment] JAMA. 1995;273:129–135. doi: 10.1001/jama.273.2.129. [DOI] [PubMed] [Google Scholar]
- 10.Barkun JS, Keyser EJ, Wexler MJ, Fried GM, Hinchey EJ, Fernandez M, Meakins JL. Short-term outcomes in open vs. laparoscopic herniorrhaphy: confounding impact of worker's compensation on convalescence. Journal of Gastrointestinal Surgery. 1999;3(6) doi: 10.1016/s1091-255x(99)80078-x. [DOI] [PubMed] [Google Scholar]
- 11.Neumayer L, Giobbie-Hurder A, Jonasson O, Dunlop D, Gibbs J, Reda D, Henderson W, Veterans Affairs Cooperative Studies Program Open mesh versus laparoscopic mesh repair of inguinal hernia. New England Journal of Medicine. 2004;350(18) doi: 10.1056/NEJMoa040093. [DOI] [PubMed] [Google Scholar]
- 12.Squirrell DM, Majeed AW, Troy G, Peacock JE, Nicholl JP, Johnson AG. A randomized, prospective, blinded comparison of postoperative pain, metabolic response, and perceived health after laparoscopic and small incision cholecystectomy. Surgery. 1998;123(5) doi: 10.1067/msy.1998.87552. [DOI] [PubMed] [Google Scholar]
- 13.McKenna SP, Doward LC, Whalley D. The development and testing of the well-being index for surgical patients (WISP) Quality of Life Research. 1998;7(2) doi: 10.1023/a:1008861627541. [DOI] [PubMed] [Google Scholar]
- 14.Urbach DR, Harnish JL, McIlroy JH, Streiner DL. A measure of quality of life after abdominal surgery. Quality of Life Research. 2006;15(6) doi: 10.1007/s11136-006-0047-3. [DOI] [PubMed] [Google Scholar]
- 15.Kleinbeck SV. Self-reported at-home postoperative recovery. Research in Nursing & Health. 2000;23:461–472. doi: 10.1002/1098-240X(200012)23:6<461::AID-NUR5>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 16.Wolfer JA, Davis CA. Assessment of surgical patients' preoperative emotional condition and postoperative welfare. Nursing Research. 1970;19:402–414. [PubMed] [Google Scholar]
- 17.Urbach DR, Harnish JL, Long G. Short-term health-related quality of life after abdominal surgery: a conceptual framework. Surgical Innovation. 2005;12(3) doi: 10.1177/155335060501200310. [DOI] [PubMed] [Google Scholar]
- 18.Strasberg SM, Ludbrook PA. Who oversees innovative practice? Is there a structure that meets the monitoring needs of new techniques? Journal of the American College of Surgeons. 2003:938–948. doi: 10.1016/S1072-7515(03)00112-1. [DOI] [PubMed] [Google Scholar]
- 19.Leventhal H, Meyer D, Nerenz D. The common sense representation of illness danger. In: Rachman S, editor. Contributions to medical psychology. Pergamon Press; New York; 1980. pp. 7–30. [Google Scholar]
- 20.Leventhal H. Behavioral medicine: Psychology in health care. In: Mechanic D, editor. Handbook of health, health care, and the health professions. Free Press; New York: 1983. pp. 709–743. [Google Scholar]
- 21.Lutz GK, Butzlaff ME, Atlas SJ, Keller RB, Singer DE, Deyo RA. The relation between expectations and outcomes in surgery for sciatica. Journal of General Internal Medicine. 1999;14(12) doi: 10.1046/j.1525-1497.1999.10417.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leventhal H, Johnson JE. Laboratory and field experimentation: Development of a theory of self-regulation. In: Woolridge PJ, Schmitt MH, Skipper JK, Leonard RC, editors. Behavior science and nursing theory. Mosby; St. Louis: 1983. pp. 189–262. [Google Scholar]
- 23.Leventhal H, Nerenz DR, Steele DJ. Illness representations and coping with health threats. In: Baum A, Singer J, editors. Handbook of psychology and health. Erlbaum; Hillsdale, NJ: 1983. pp. 219–252. [Google Scholar]
- 24.Andreoli KG. Key aspects of recovery. Springer; New York: 1990. [Google Scholar]
- 25.McDowell I, Newell C. Measuring Health: A guide to rating scales and questionnaires. Oxford University Press; New York: 1996. [Google Scholar]
- 26.Anderson RM, Barr PA, Edwards GJ, Funnell MM, Fitzgerald JT, Wisdom K. Using focus groups to identify psychosocial issues of urban black individuals with diabetes. Diabetes Educator. 1996;22(1) doi: 10.1177/014572179602200104. [DOI] [PubMed] [Google Scholar]
- 27.Stewart D. Fcous Groups: Theory and Practice. Sage Publications: 1990. [Google Scholar]
- 28.Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, Bullinger M, Kaasa S, Leplege A, Prieto L, Sullivan M. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. Journal of Clinical Epidemiology. 1998;51(11) doi: 10.1016/s0895-4356(98)00109-7. [DOI] [PubMed] [Google Scholar]
- 29.Ware JE, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36). I. Conceptual framework and item selection. Medical Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 30.McCorkle R, Quint-Benoliel J. Symptom distress, current concerns and mood disturbance after diagnosis of life-threatening disease. Social Science & Medicine. 1983;17:431–438. doi: 10.1016/0277-9536(83)90348-9. [DOI] [PubMed] [Google Scholar]
- 31.Urbach DR. Measuring quality of life after surgery. Surgical Innovation. 2005;12(2) doi: 10.1177/155335060501200216. [DOI] [PubMed] [Google Scholar]
- 32.Mangione CM, Goldman L, Orav EJ, Marcantonio ER, Pedan A, Ludwig LE, Donaldson MC, Sugarbaker DJ, Poss R, Lee TH. Health-related quality of life after elective surgery: measurement of longitudinal changes. Journal of General Internal Medicine. 1997;12(11) doi: 10.1046/j.1525-1497.1997.07142.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chernew ME, Hirth RA, Cutler DM. Increased spending on health care: how much can the United States afford? Health Affairs. 2003;22:15–25. doi: 10.1377/hlthaff.22.4.15. [DOI] [PubMed] [Google Scholar]
- 34.Macario A, Vitez TS, Dunn B, McDonald T, Brown B. Hospital costs and severity of illness in three types of elective surgery. Anesthesiology. 1997;86:92–100. doi: 10.1097/00000542-199701000-00013. [DOI] [PubMed] [Google Scholar]
- 35.Miller DC, Wei JT, Dunn RL, Hollenbeck BK. Trends in the diffusion of laparoscopic nephrectomy. JAMA. 2006;295(21) doi: 10.1001/jama.295.21.2480. [DOI] [PubMed] [Google Scholar]