Abstract
Background
There is a tenfold variation across U.S. states in the prevalence of feeding tube use among elderly nursing home residents (NHR) with advanced cognitive impairment. The goal of this study was to examine whether regions with higher rates of health care transitions at the end of life are more likely to use feeding tubes in patients with severe cognitive impairment.
Methods
A retrospective cohort study of U.S. nursing home residents with advanced cognitive impairment. The incidence of feeding tube insertion was determined by Medicare Part A and B billing data. A count of the number of health care transition in the last 6 months of life was determined for nursing home residents. A multivariate model examined the association of residing in a geographic region with a higher rates of health care transition and the insertion of a feeding tube in nusing home resident with advance cognitive impairment.
Results
Hospital Referral Region (HRR) health care transitions varied from 192 (Salem, Oregon) to 509 per 100 decedents (Monroe, Louisiana) within the last 6 months of life. HRRs with higher transition rates had a higher incidence of feeding tube insertion (Spearman correlation = 0.58). Subjects residing in regions with the highest quintile of transitions rates were 2.5 times (95% confidence interval [CI] 1.9–3.2) more likely to have a feeding tube inserted compared to those that resided in the lowest quintile.
Conclusions
Regions with higher rates of care transitions among nursing home residents are also much more likely to have higher rates of feeding tube placement for patients with severe cognitive impairment, a population in whom benefit is unlikely.
Introduction
Dementia is a chronic, progressive illness, and a leading cause of death among older Americans.1 Dysphagia is a hallmark of end-stage dementia that often leads to weight loss, aspiration, and recurrent pneumonias. Therefore, decisions regarding to hospitalize severely demented nursing home residents with acute infections commonly occur in conjunction with treatment decisions for feeding problems (i.e., tube feeding versus hand feeding). No previous research has considered the potential relationship between health care transitions, such as hospitalizations, and feeding tube insertion in end-stage dementia.
Multiple reviews of the literature have questioned the benefits of tube-feeding persons with advanced dementia.2–4 Feeding tubes have not been found to improve survival, prevent aspiration pneumonias, heal decubitus ulcers, or other important health outcomes. Previous research has revealed striking variation in the prevalence of feeding tubes among persons with advanced dementia.1,5,6 Important limitations of existing research is studying the prevalence of feeding tube use rather than incident tube insertions and the lack of information about the point in an illness episode a feeding tube is inserted. For example, if feeding tubes are predominately inserted during a hospitalization, efforts to reduce their use would need to focus on advance care planning for preferences regarding artificial nutrition occurs in the nursing home setting and ensuring that those wishes are communicated from the nursing home to the acute care hospital.
Two cost containment strategies were implemented a time when there was increase in the rate of transfer of elderly persons from hospitals to nursing homes. Both the Medicare prospective payment system using diagnostic-related groups (DRGs) for hospital reimbursements and the growth of managed care reduced hospital length of stay, leading to more transfers to nursing homes for rehabilitation, and transfers of patients with higher intensity medical needs.7–10 Such transitions have been associated with medical errors,11 functional decline,12 and bereaved family members' perceptions that health care providers did not have the correct information to provide the best possible care.13 Using the Medicare Beneficiary Survey, Coleman and colleagues14 examined the rate and pattern of transitions occurring after acute care hospitalizations in 1997–1998. Approximately one third of persons experienced multiple transitions within 30 days posthospitalization. The authors estimated that one in four of these transitions were complicated (e.g., going from a hospital to a nursing home and then returning to a hospital). Saliba and colleagues15 estimate that 40% of hospitalizations of nursing home residents are inappropriate, and that nursing home residents could have been safely cared for in the nursing home. This research provides preliminary evidence that many transitions are inappropriate, resulting in increased health care costs and potentially, increased morbidity and mortality to frail, older persons. In this study, we specifically wanted to examine the association of whether geographic regions with a higher rate of health care transitions for nursing home residents had a higher rate of feeding tubes insertions for people with advanced cognitive impairment.
Methods
Sample
Two samples are utilized in this research. Both samples were created by linking Medicare claims data with the National Repository of the Resident Assessment Instrument Minimum Data Set (MDS) from 2000. The MDS is a standardized instrument that collects demographic, health status and care needs information for persons residing in all Medicare/Medicaid certified U.S. nursing homes. For the first sample, subjects had to be present in a randomly drawn 20% sample of Part B claims, 100% Part A claims and reside in a nursing home based on MDS assessment within 60 days of April 1. Subjects resided in the continental United States. Additionally, subjects were aged 65 and older, had advanced cognitive impairment, and did not have a feeding tube at the time of the baseline assessment (N = 97,239). Advanced cognitive impairment was defined as having a Cognitive Performance Score (CPS)16 ranging from 4 (moderately severe impairment) to 6 (very severe impairment with eating problems). The second sample includes person-level counts of the number of transitions among all Medicare beneficiaries who died in 2000 and had at least one nursing home stay in the last 6 months of life. Death date was based on the Medicare denominator file.
Measures
Feeding tube insertion
The cohort of nursing home residents with advanced cognitive impairment were followed to determine whether or not they had a feeding tube insertion during the year following their baseline MDS assessment. Feeding tube insertion was determined from both Part A and Part B Medicare Claims Files and defined by the occurrence of any of the following physician billing or CPT codes: ICD-9 procedure codes; 43.1, 43.11, 43.19, or 44.32; or CPT-4 codes; 43246, 43653, 43750, 43830, 43832, 44372, 44373, or 74350.
Health care transitions
The rate of health care transitions were determined by linking Medicare Claims Files with MDS data. The unit of analysis is a Hospital Referral Region (HRR) (N = 306 across the United States). Within each HRR, the number of decedents in 2000 who had a nursing home admission (based on MDS data) were identified. Transitions were defined as transfer to or from any of the following settings; hospital, inpatient rehabilitation, nursing home, inpatient hospice, and home with or without home health services as determined from both Medicare Claims and MDS data. The mean number of health care transitions per 100 decedents within the last six months of life was calculated for each HRR.
Statistical Analyses
The average rate of transitions in the last 6 months of life per 100 decedents was depicted in a U.S. map grouping HRRs into quintiles. Incidence of tube-feeding placement was calculated per 1000 persons. To examine the association between the transition rate and the incident rate of feeding tube insertion, a Spearman's correlation coefficient was used. A multivariate model using a Huber White adjustment examined the association of the individual 1-year risk of feeding tube insertion with geographic variation in health care transitions adjusting for age, gender, race, education, functional status,17 whether functioning is improving or declining, medical diagnoses, cognitive performance score (i.e., 4, 5, or 6), difficulty swallowing, the presence of a do-not-resuscitate order, an order to forego artificial hydration and nutrition, the MDS-CHESS scale,18 and whether the resident had a recent pneumonia.
Results
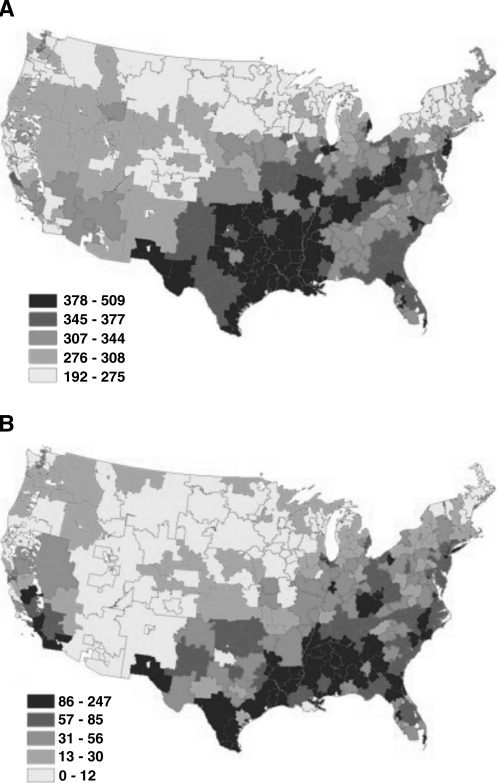
Overall, among the cohort of 97,241 nursing home residents (mean age, 84.7 ± 7.6 years 74.3% female, 87.4% white) the 12-month incidence of feeding tube insertion was 53.9 per 1000 persons. Nearly two thirds (48.3%) of the cohort died within 1 year after feeding tube insertion. Across the 306 HRRs, the 12-month incident rate of feeding tube insertion ranged between 0 to 217 per 1000 nursing home residents (Fig. 1A). Nationwide, the 348,276 decedents (mean age, 84.0, female, 64.0%) with a nursing home stay in 2000 had 328.4 transitions per 100 decedents in the last 6 months of life. The transition rate ranged from 192 transitions (Salem, Oregon), to 509 per 100 decedents (Monroe, Louisiana; Fig. 1B).
FIG. 1.
(A) One-year incidence of feeding tube insertion by hospital referral region. (B) Rates of health care transitions for 100 decedents with a nursing home stay in 2000 by hospital referral region.
HRRs with higher end-of-life health care transition rates had a higher rate of feeding tube insertion (Spearman correlation = 0.58), compared to the region with the lowest quintile of health care transitions, nursing home residents residing in the highest quintile had 2.5 times increased likelihood of 1-year insertion of feeding tubes after adjusting for other covariates (95% confidence interval [CI] of the adjusted odds ratio is 1.9–3.3). Table 1 provides the adjusted odds ratio of having a feeding tube inserted in persons with advanced cognitive impairment residing in regions that vary in the rate of health care transitions for decedents who had a stay in a nursing home.
Table 1.
Adjusted Odds of Feeding Tube Insertion Among Nursing Home Residents with Advanced Cognitive Impairment Residing in Regions Varying on Rate of Health Care Transitionsa
| Quintile of health care transition | Mean rate of health care transitions per 100 decedents | Adjusted odds ratio | 95% confidence interval |
|---|---|---|---|
| 1st Quintile | 264.6 | Reference | |
| 2nd Quintile | 302.7 | 1.3 | 0.97–1.7 |
| 3rd Quintile | 330.0 | 2.3 | 1.7–3.0 |
| 4th Quintile | 359.6 | 1.9 | 1.5–2.4 |
| 5th Quintile | 401.5 | 2.5 | 2.0–3.2 |
Adjusted for ethnicity, gender, order to forego resuscitation, restrictions on the use of artificial hydration and nutrition, medical diagnoses, difficulty swallowing, activities of daily living, weight loss, education, whether there was recent pneumonia, where their functioning is improving or declining, and the MDS-CHESS Scale.
Discussion
Previous research has highlighted quality of care concerns associated with poorly executed health care transitions and the striking variation in the use of feeding tubes among persons with advanced cognitive impairment. We found that persons with advanced dementia residing in a nursing home were more likely to have a feeding tube inserted if they lived in region of the continental United States that had higher rates of health care transitions. While this observation does not necessarily imply a causal relationship, it raises serious concerns about the quality and efficiency of end-of-life care in the United States. Future research is needed to understand whether a poorly executed transition played a role in the insertion of a feeding tube, or that this strong association is a reflection of a medical culture towards overall aggressive medical care.
Poorly executed health care transitions are associated with medical errors, functional decline, and the perception by bereaved family members that health care providers do not have adequate information to provide the best possible care. On average, we found that decedents experienced 3.2 transitions in the last 6 months of life. This varied threefold across the country. Beyond describing the rate and geographic variation of health care transitions among decedents with a nursing home stay in 2000, we examined whether persons with advanced cognitive impairment living in geographic regions with a higher rate of health care transitions among decedents had a higher risk of feeding tube insertion. Persons residing in regions with the highest quintile of health care transitions had more than 2 times the incidence insertion rate of feeding tubes compared to those residing in the lowest quintile of health care transitions among decedents with a nursing home stay.
While our research utilized the merger of two national databases, an important limitation is that information is not available to confirm or refute potential mechanisms that would explain the association of health care transitions with feeding tube insertion. For example, it is possible that persons are hospitalized without information about their wishes regarding artificial hydration and nutrition. This information discontinuity results in inappropriate use of feeding tubes. An alternate potential explanation is that both of these findings are markers of local medical culture that tends toward aggressive interventions such as feeding tubes and hospitalizations among dying persons. Our analysis did adjust for available information on nursing home residents' preferences, including whether the nursing home resident had an order to forgo hydration and nutrition. Future research is needed to understand the mechanisms of this variation especially in light of recent research that suggests that such variation is not associated with improved patient outcomes.19–21
An important question for this century is how to provide competent, coordinated, and cost effective care for a growing population of elderly persons with chronic progressive illnesses. Our results demonstrate striking variation in care transitions for decedents with a nursing home stay. A nursing home resident residing in a geographic region with a higher transition rate for decedents had a higher risk of feeding tube insertion, despite growing evidence that feeding tube insertion does not lead to improved patient outcomes. Instead of saving health care resources as assumed to occur with prospective payment, transitions could increase health care costs when poorly executed.22,23 Future research is needed to understand this variation, the role of state policies resulting in more frequent transitions, and interventions to improve care coordination.
Acknowledgments
The authors thank Mrs. Cindy Williams for assistance in manuscript preparation and Mr. Christopher Brostrup-Jensen for preparation of the data base.
The funder was the National Institute of Aging (R01AG24365 and P01AG19783). The funder had no role in design, methods, recruitment, analysis, and preparation of the manuscript.
Funding for this research was provided by the National Institute of Aging (R01AG24265 and P01AG19783). The funder had no role in design, methods, recruitment, analysis, and preparation of the manuscript.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Mitchell SL. Teno JM. Roy J. Kabumoto G. Mor V. Clinical and organizational factors associated with feeding tube use among nursing home residents with advanced cognitive impairment. JAMA. 2003;290:73–80. doi: 10.1001/jama.290.1.73. [DOI] [PubMed] [Google Scholar]
- 2.Finucane TE. Christmas C. Travis K. Tube feeding in patients with advanced dementia: A review of the evidence. JAMA. 1999;282:1365–1370. doi: 10.1001/jama.282.14.1365. [DOI] [PubMed] [Google Scholar]
- 3.Gillick MR. Rethinking the role of tube feeding in patients with advanced dementia. N Engl J Med. 2000;342:206–210. doi: 10.1056/NEJM200001203420312. [DOI] [PubMed] [Google Scholar]
- 4.Finucane TE. Christmas C. Leff BA. Tube feeding in dementia: How incentives undermine health care quality and patient safety. J Am Med Dir Assoc. 2007;8:205–208. doi: 10.1016/j.jamda.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 5.Teno JM. Mor V. DeSilva D. Kabumoto G. Roy J. Wetle T. Use of feeding tubes in nursing home residents with severe cognitive impairment. JAMA. 2002;287:3211–3212. doi: 10.1001/jama.287.24.3211. [DOI] [PubMed] [Google Scholar]
- 6.Gessert CE. State practice variation in the use of tube feeding for nursing home residents with severe cognitive impairment. J Am Geriatr Soc. 2001;49:1399. doi: 10.1046/j.1532-5415.2001.49278.x. [DOI] [PubMed] [Google Scholar]
- 7.Liu K. Taghavi L. Cornelius ES. Changes in Medicaid nursing home beds and residents. Health Care Financ Rev Annu Suppl. 1992:303–310. [PubMed] [Google Scholar]
- 8.Cornelius E. Feldman J. Marsteller JA. Liu K. Creating a MEDPAR (Medicare provider analysis and review) analog to the RUG-III (Resource Utilization Groups, Version III) classification system. Health Care Financ Rev. 1994;16:101–126. [PMC free article] [PubMed] [Google Scholar]
- 9.Haas JS. Phillips KA. Sonneborn D. McCulloch CE. Liang SY. Effect of managed care insurance on the use of preventive care for specific ethnic groups in the United States. Med Care. 2002;40:743–751. doi: 10.1097/00005650-200209000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Kane RL. Flood S. Bershadsky B. Keckhafer G. Effect of an innovative medicare managed care program on the quality of care for nursing home residents. Gerontologist. 2004;44:95–103. doi: 10.1093/geront/44.1.95. [DOI] [PubMed] [Google Scholar]
- 11.Boockvar K. Fishman E. Kyriacou CK. Monias A. Gavi S. Cortes T. Adverse events due to discontinuations in drug use and dose changes in patients transferred between acute and long-term care facilities. Arch Intern Med. 2004;164:545–550. doi: 10.1001/archinte.164.5.545. [DOI] [PubMed] [Google Scholar]
- 12.Gillick MR. Serrell NA. Gillick LS. Adverse consequences of hospitalization in the elderly. Soc Sci Med. 1982;16:1033–1038. doi: 10.1016/0277-9536(82)90175-7. [DOI] [PubMed] [Google Scholar]
- 13.Bourbonniere M. Teno JM. Roy J. Mor V. Transitions at the end of life: Quality of care and information continuity [abstract] J Am Geriatr Soc. 2003;51:S40–41. [Google Scholar]
- 14.Coleman EA. Min SJ. Chomiak A. Kramer AM. Posthospital care transitions: patterns, complications, and risk identification. Health Serv Res. 2004;39:1449–1465. doi: 10.1111/j.1475-6773.2004.00298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saliba D. Kington R. Buchanan J. Bell R. Wang M. Lee M. Herbst M. Lee D. Sur D. Rubenstein L. Appropriateness of the decision to transfer nursing facility residents to the hospital. J Am Geriatr Soc. 2000;48:154–163. doi: 10.1111/j.1532-5415.2000.tb03906.x. [DOI] [PubMed] [Google Scholar]
- 16.Morris JN. Fries BE. Mehr DR. Hawes C. Phillips C. Mor V. Lipsitz LA. MDS Cognitive Performance Scale. J Gerontol. 1994;49:M174–182. doi: 10.1093/geronj/49.4.m174. [DOI] [PubMed] [Google Scholar]
- 17.Morris JN. Fries BE. Morris SA. Scaling ADLs within the MDS. J Gerontol A Biol Sci Med Sci. 1999;54:M546–553. doi: 10.1093/gerona/54.11.m546. [DOI] [PubMed] [Google Scholar]
- 18.Hirdes JP. Frijters DH. Teare GF. The MDS-CHESS scale: A new measure to predict mortality in institutionalized older people. J Am Geriatr Soc. 2003;51:96–100. doi: 10.1034/j.1601-5215.2002.51017.x. [DOI] [PubMed] [Google Scholar]
- 19.Fisher ES. Wennberg DE. Stukel TA. Gottlieb DJ. Lucas FL. Pinder EL. The implications of regional variations in Medicare spending. Part 2: Health outcomes and satisfaction with care. Ann Intern Med. 2003;138:288–298. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- 20.Fisher ES. Wennberg DE. Stukel TA. Gottlieb DJ. Lucas FL. Pinder EL. The implications of regional variations in Medicare spending. Part 1: The content, quality, and accessibility of care. Ann Intern Med. 2003;138:273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 21.Teno JM. Fisher ES. Mor V. Roy J. Clarridge B. Wennberg JE. Dying in HSA with higher ICU utilization: Is more better [abstract]? J Am Geriatr Soc. 2003;51:S39–40. [Google Scholar]
- 22.Weissman JS. Ayanian JZ. Chasan-Taber S. Sherwood MJ. Roth C. Epstein AM. Hospital readmissions and quality of care. Med Care. 1999;37:490–501. doi: 10.1097/00005650-199905000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Corrigan JM. Martin JB. Identification of factors associated with hospital readmission and development of a predictive model. Health Serv Res. 1992;27:81–101. [PMC free article] [PubMed] [Google Scholar]