Abstract
Peliosis hepatis is a rare benign vascular disorder of the liver that may be associated with malignancy, infection and drugs. The imaging manifestation of this disorder is often variable and nonspecific making its diagnosis difficult. We describe a rare case of peliosis hepatis and gummatous syphilis of the liver with emphasis on CT findings. Image characteristics of our patient included pseudotumoral appearance of peliosis hepatis, isodensity to the adjacent liver parenchyma on unenhanced and dual-phase scanning. To our knowledge, peliosis hepatis associated with syphilis and unique enhancement pattern has not been reported. Considering the imaging features of peliosis hepatis, it should be considered in the differential diagnosis of atypical focal hepatic lesion.
Keywords: Focal liver lesion, Peliosis hepatis, Syphilis, Computed tomography
INTRODUCTION
Peliosis hepatis is a rare kind of benign vascular disorder characterized by widespread blood-filled cystic cavities in the liver[1]. Occasionally, the lesion mimics tumor. The imaging manifest of this disorder is variable and nonspecific, making its diagnosis and differential diagnosis difficult. To our knowledge, no study is yet available on peliosis hepatis associated with syphilis. We report a rare case of focal peliosis hepatis and gummatous syphilis, their computed tomography (CT) and ultrasonography (US) findings along with the features of histopathology.
CASE REPORT
A 44-year-old woman had upper right abdominal pain for 4 months with no hemorrhagic tendency. Physical examination revealed no icteric skin and sclera, no abdominal mass, hepatosplenomegaly and superficial lymph nodes. On admission, treponema pallidum antibody test was positive, α-fetoprotein (AFP) was normal (1.74 ng/mL, normal range 0-8), routine blood chemistry and serum transaminase values were within the normal limits.
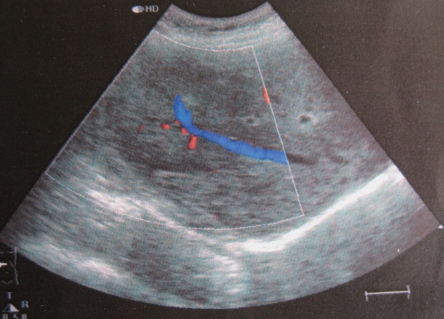
Abdominal ultrasonography showed a heterogeneous hypoechoic mass in the right lobe of the liver and the right hepatic vein was observed crossing the lesion with a normal shape (Figure 1). The hepatic veins, portal veins and other abdominal organs did not show any abnormalities. Unenhanced and contrast-enhanced dual-phase CT examination of the upper abdomen was performed with a 16 channel spiral CT scanner. There was an ill-defined isodensity area measuring 70 mm × 65 mm with punctate calcification in segments V and VI (Figure 2A). The attenuation of contrast in the mass was identical to that in the adjacent liver parenchyma during arterial and portal-venous phase. The center of this area was not enhanced. The right hepatic vein crossed the lesion with a normal shape (Figure 2B and C). Meanwhile, there was a hypo-attenuated lesion (10 mm in diameter) in segment VIII without enhancement at arterial and portal-venous phases (Figure 3). The spleen was normal and no lymphadenopathy was observed in the upper abdominal cavity and retroperitoneal space.
Figure 1.
Doppler sonographic image showing a slightly heterogeneous hyperechoic lesion in the right lobe of liver without mass effect on the right hepatic vein.
Figure 2.
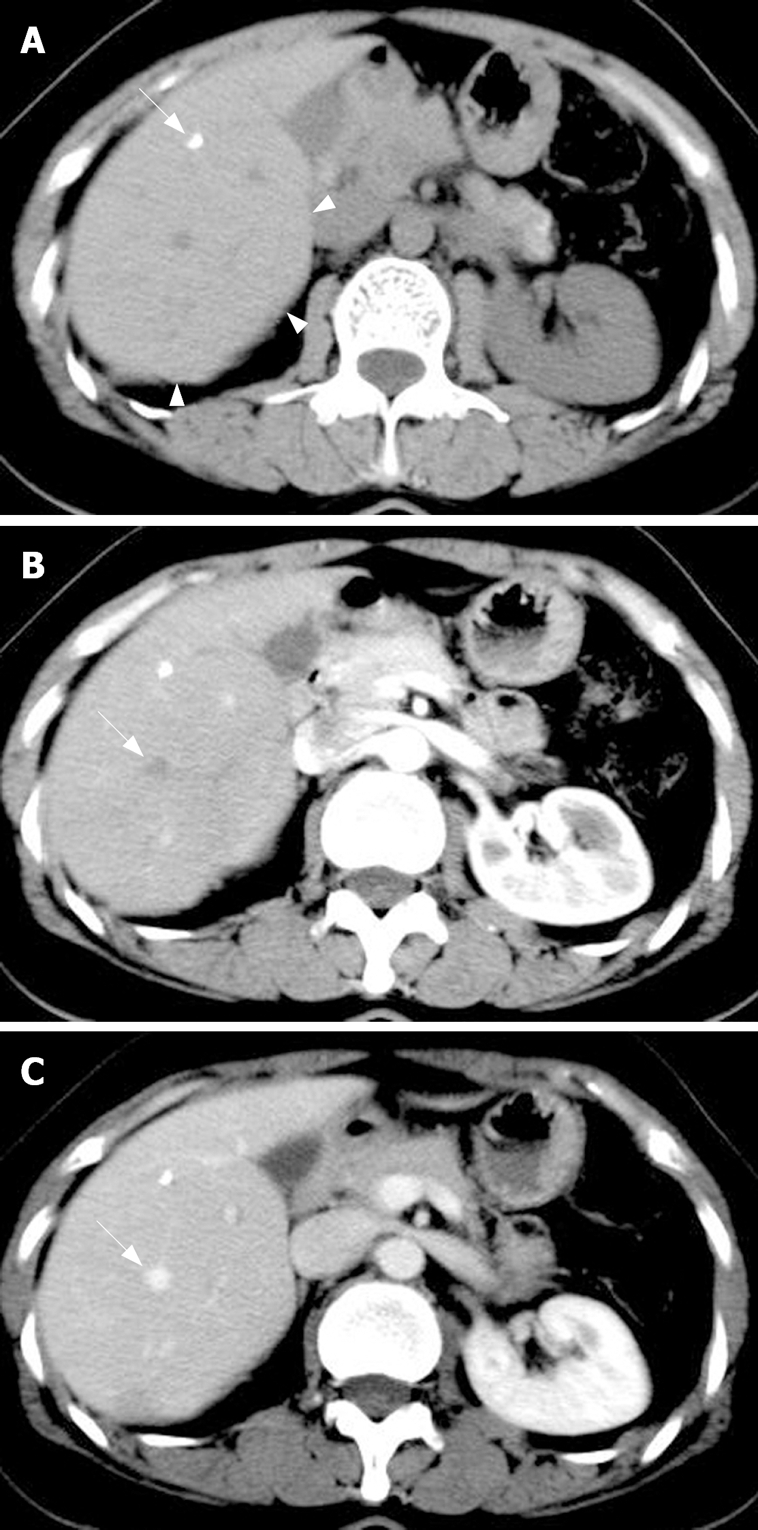
Transverse unenhanced CT image showing the protrudent visceral surface which hints a local iso-attenuated lesion (arrowheads) with punctate calcification (arrow) (A), identical density of the lesion to the adjacent liver parenchyma at arterial phase (B) and portal phase (C). The right hepatic vein with a normal shape and location crosses the lesion (arrow).
Figure 3.

Portal phase image showing a hypo-attenuated lesion (10 mm in diameter) within segment VIII (arrow). Histopathology proved it to be a gumma.
After lobectomy of the right lobe of liver was performed and the resected hepatic specimen was split, a dark violet mass was located in segments V and VI.Histopathology showed a mass with multifocal and irregular blood-filled cystic spaces and ectatic adjacent sinusoids. The histopathological diagnosis was peliosis hepatis (Figure 4), while the hypodensity lesion within segment VIII was a gumma (Figure 5).
Figure 4.
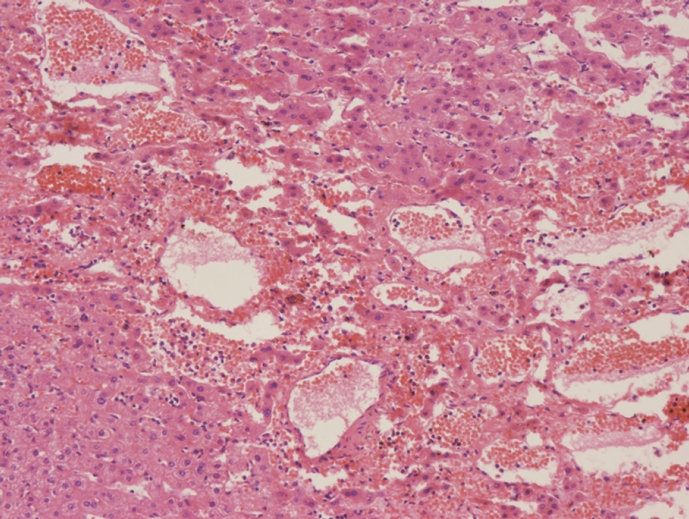
Histology of specimens (HE, × 50). Microscopy reveals multiple blood-filled cystic spaces and ectatic sinusoids.
Figure 5.
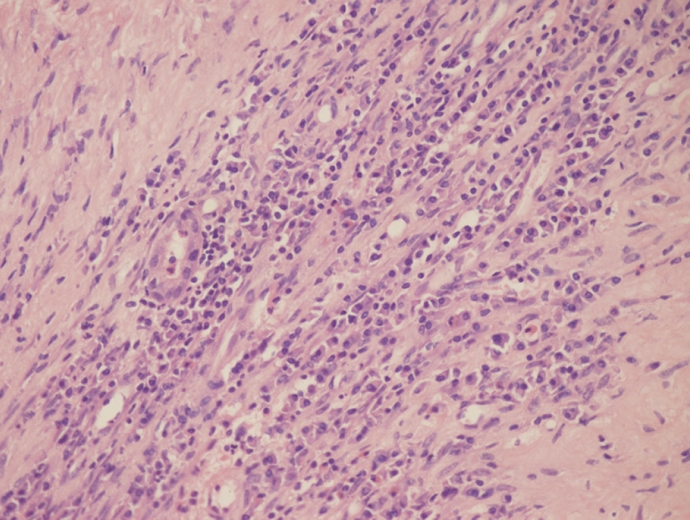
Gumma on segment VIII characterized by multifocal coagulation necrosis and significant infiltration of plasma cells mixed with lymph cells (HE, × 100).
DISCUSSION
Peliosis hepatic, first described by Wagner and named by Schoenlank, is a rare benign vascular disorder. The lesion varies from 1 mm to several centimeters with multiple blood-filled cavities[2,3]. The lesions typically involve the whole liver, but local peliosis hepatis (also called peliosis hepatis pseudotumor) has also been reported[4], like our case. Yanoff and Rawson[5] have reported two types of the disease: parenchymal and phlebectatic. The irregularly-shaped blood spaces of the parenchymal type, usually associated with hemorrhagic parenchymal necrosis, are not lined with endothelium. The blood spaces of the phlebectatic type, based on aneurismal dilatation of the central vein, are covered with endothelium and have no hemorrhagic parenchymal necrosis.
The causes for peliosis hepatis are unknown. However, peliosis hepatis is associated with drugs (anabolic steroids, oral contraceptives, etc), malignant tumor (particularly hepatocellular carcinoma), and chronic infections (pulmonary tuberculosis, leprosy and HIV infections)[2–4]. Peliosis hepatis accompanying syphilis infection has not, to our knowledge, previously been reported. Syphilis infection may be one of the causes for peliosis hepatis, but their relationship needs to be further investigated.
The clinical manifestations and laboratory examinations of peliosis hepatis are not specific and the imaging features of US, CT and MRI may be helpful for its diagnosis. The imaging findings of peliosis hepatis are variable depending on the pathologic patterns, lesion size, extent of communication with sinusoids, and complications such as thrombosis or haemorrhage within the lesion and concomitant hepatic steatosis[2–4]. Conventional gray-scale sonography shows hyperechoic lesions in patients with a healthy liver, homogeneous hypoechoic lesions in patients with hepatic steatosis and heterogeneous hypoechoic lesions if complicated by hemorrhage. Absence of a mass effect on peripheral blood vessels is considered characteristic of a peliosis hepatis pseudotumor[3,4]. On unenhanced CT, peliotic lesions usually have multiple areas of low attenuation, calcifications and hemorrhage within the lesions have also been described[2]. On MR imaging, the signal intensities of the lesions largely depend on the stage and status of the blood component. On T1-weighted sequence, the lesions are hypo-intense or heterogeneous hypo-intense if complicated by hemorrhage. On T2-weighted sequence, peliotic lesions are usually hyper-intense compared to liver parenchyma. On contrast-enhanced imaging, the lesions show a predominantly central enhancement at the arterial phase and slow centrifugal progression at the portal-venous and delayed phases (the so-called target sign) or an unusual centripetal enhancement pattern similar to hemangioma, from the periphery to the centre. Hemorrhagic parenchymal necrosis and thrombosed cavities manifest as a non-enhancing area. In some instances, small (< 2 cm) peliotic lesions also show hyper-attenuation on both arterial and portal venous phase images[2]. As imaging appearances and laboratory examinations are not specific, biopsy is the only way to make its diagnosis. The lesion of our case showed isodensity and was ill-defined on unenhanced scanning and synchronous enhancement with the liver parenchyma on enhanced CT. The enhancement pattern was different from previous reports. It may be due to the difference in the severity of sinusoids dilatation.
In conclusion, our case is unusual in several respects: (1) peliosis hepatis with syphilitic gumma of the liver, (2) isodensity to the adjacent liver parenchyma on unenhanced and dual-phase scanning, (3) pseudotumoral appearance. Awareness of the imaging features of peliosis hepatis is important to make its diagnosis. Peliosis hepatis should be considered in the differential diagnosis of atypical local hepatic lesion.
Acknowledgments
The authors thank Dr. Zhu HB for her valuable advice regarding the pathology of peliosis and gummatous syphilis of the liver and Dr. Song QL for help in the preparation of this manuscript.
Peer reviewer: James M Millis, Professor, University of Chicago, Section of Transplantation, MC 5027, 5841 S. Maryland Avenue, Chicago, IL 60637, United States
S- Editor Zhu WL L- Editor Wang XL E- Editor Lu W
References
- 1.Gouya H, Vignaux O, Legmann P, de Pigneux G, Bonnin A. Peliosis hepatis: triphasic helical CT and dynamic MRI findings. Abdom Imaging. 2001;26:507–509. doi: 10.1007/s00261-001-0023-x. [DOI] [PubMed] [Google Scholar]
- 2.Iannaccone R, Federle MP, Brancatelli G, Matsui O, Fishman EK, Narra VR, Grazioli L, McCarthy SM, Piacentini F, Maruzzelli L, et al. Peliosis hepatis: spectrum of imaging findings. AJR Am J Roentgenol. 2006;187:W43–W52. doi: 10.2214/AJR.05.0167. [DOI] [PubMed] [Google Scholar]
- 3.Verswijvel G, Janssens F, Colla P, Mampaey S, Verhelst H, Van Eycken P, Erven W. Peliosis hepatis presenting as a multifocal hepatic pseudotumor: MR findings in two cases. Eur Radiol. 2003;13 Suppl 4:L40–L44. doi: 10.1007/s00330-003-1852-5. [DOI] [PubMed] [Google Scholar]
- 4.Savastano S, San Bortolo O, Velo E, Rettore C, Altavilla G. Pseudotumoral appearance of peliosis hepatis. AJR Am J Roentgenol. 2005;185:558–559. doi: 10.2214/ajr.185.2.01850558. [DOI] [PubMed] [Google Scholar]
- 5.Yanoff M, Rawson AJ. Peliosis hepatis. An anatomic study with demonstration of two varieties. Arch Pathol. 1964;77:159–165. [PubMed] [Google Scholar]