Abstract
Investigations into complementary and alternative medicine (CAM) approaches to address stress, depression, and anxiety of those experiencing chronic pain are rare. The objective of this pilot study was to assess the value of a structured massage therapy program, with a focus on myofascial trigger points, on psychological measures associated with tension-type headache. Participants were enrolled in an open-label trial using a baseline control with four 3-week phases: baseline, massage (two 3-week periods) and a follow-up phase. Eighteen subjects with episodic or chronic tension-type headache were enrolled and evaluated at 3-week intervals using the State-Trait Anxiety Inventory, Beck Depression Inventory, and the Perceived Stress Scale. The Daily Stress Inventory was administered over 7-day periods during baseline and the final week of massage. Twice weekly, 45-minute massage therapy sessions commenced following the baseline phase and continued for 6 weeks. A significant improvement in all psychological measures was detected over the timeframe of the study. Post hoc evaluation indicated improvement over baseline for depression and trait anxiety following 6 weeks of massage, but not 3 weeks. A reduction in the number of events deemed stressful as well as their respective impact was detected. This pilot study provides evidence for reduction of affective distress in a chronic pain population, suggesting the need for more rigorously controlled studies using massage therapy to address psychological measures associated with TTH.
KEYWORDS: Beck Depression Inventory, Complementary and Alternative Medicine, Daily Stress Inventory, Myofascial Pain, State-Trait Anxiety Inventory
Tension-type headache (TTH) is a 15 days per month and the chronic form dull aching headache that affects a 15 or more days per month1. The epilarge percentage of the population sodic form of TTH affects between 20to varying degrees; it frequently resolves 42% of the population while the chronic with time or over-the-counter analgesics. form affects 2.5-3%2,3. The authors of a however, for some individuals, the regu-recent review article concluded that larity of headache persists to a clinical worldwide disability attributable to condition that is recognized as either epi-headache is greater for TTH than other sodic or chronic, the difference based classifications including migraine head-primarily on the frequency of attack with ache4. The personal burden associated the episodic form occurring fewer than with these clinical forms of TTH can be substantial as it encompasses physical suffering alongside the personal economic effect from lost work days, which in turn perpetuate psychological symptoms such as stress, anxiety, and depression. Yet while TTH is the most prevalent form of headache and has a considerable impact on quality of life, treatment avenues have been under-investigated5. Moreover, due to the pervasive nature of TTH, pain measures alone that are typically used in the current literature provide incomplete information about the impact of headache on these associated psychological aspects.
On average, perceived stress is higher in individuals who report chronic daily headache than in a healthy population6. Although recurrent TTH sufferers have similar physiological responses to laboratory stressors, they report a greater number of everyday stresses or daily “hassles” than do matched non-headache control subjects7,8. Furthermore, stressful events are appraised as more stressful for recurrent TTH sufferers than for headache-free subjects7. Stress is also the most frequent headache trigger with 88% of patients from the general population in urban and rural areas reporting this variable as a cause for ensuing headache9. Finally, stress has been noted to exacerbate headache symptoms; and minor everyday stressors, rather than major life events, have been tagged as a contributor to maintaining or prolonging existing headache10. Thus, stress, particularly as a result of minor everyday frustrations, is an important area of investigation in relation to headache.
In addition to stress, elevated anxiety and depression are commonly reported among those with headache11. Again, the prevalence of anxiety and depression is greater in those with TTH than in a non-headache population11, with chronicity of headache associated with increased affective distress12. In adult patients with chronic TTH, major depression has been reported in 59%, with 25% experiencing an anxiety disorder13. The effect is not limited to adults; a study involving children and young adults with TTH reported that 50% suffer from one or more psychiatric disorders, with anxiety and depression the two most commonly cited14. In a study examining stress, depression, and anxiety in primary headache patients, depression and anxiety were found to frequently co-exist in the same subject15. Affective distress, in addition to pain, has been described as an important component to address in the treatment of TTH patients9.
Complementary and alternative therapies have been used as corrective treatments for ailments including chronic pain and psychopathological conditions16. Of patients visiting a headache clinic, 40% use one or more complementary and alternative medicine modalities to reduce pain associated with chronic TTH17, with 26.7% using massage as a coping strategy for the pain18. Additional reference to the use of massage has been noted in several studies involving TTH patients. Scalp massage is cited as a primary self-treatment used by TTH sufferers19, and self-massage of cranial musculature is regularly employed by 25% of TTH patients as a quick means to reduce pain although the immediate benefit was found to wane within 5 minutes of stopping the maneuver20. Although only a few pilot studies have directly investigated the effect of massage therapy on TTH, the findings have been positive for reducing headache frequency and intensity21,22.
In addition to its use for reducing headache pain, massage therapy has also been suggested as a means for reducing psychological distress. Reductions in measures of stress, anxiety, and depression have been noted in healthy populations23–25 as well as those experiencing chronic pain26,27. healthcare professionals also rank massage therapy as effective for stress and anxiety reduction28. The effect of massage therapy on psychological affect in a TTH population has not been specifically studied. Subsequently, the objective of this study was to evaluate a replicable massage therapy treatment directed at cervical and cranial musculature on psychological measures including stress, anxiety, and depression in subjects with TTH.
Methods
Study Design
Subjects with TTH received twelve 45-minute massage sessions over 6 weeks. Massage was directed toward soft tissues of the cervical and cranial regions with an emphasis on reducing myofascial trigger point (MTrP) activity. MTrPs have recently become of interest in the TTH population due to their increased presence in TTH populations and their ability to produce a referred pain phenomenon that directly mimics the patient's pain complaint29–31. A 3-week baseline period preceded 6 weeks of massage, and a final evaluation was conducted 3 weeks following the massage phase. Subject stress, depression, and anxiety were measured using standardized tests at study start and at 3-week intervals throughout the study. Primary and secondary headache measures from subjects in this study have been previously reported32. The Institutional Review Board at the Boulder College of Massage Therapy approved this study; all subjects signed an informed consent prior to study enrollment.
Subjects
Selection criteria conformed to the 2004 International headache Society guidelines for episodic or chronic TTH and included regular headache occurring for at least the prior six months, each headache bout ≥4 hours; 21-65 years of age; and ≤1 migraine headaches per month1. Subjects taking anti-psychotic or antidepressant medications were excluded from the study. headache parameters were verified through a 3-week headache diary during the baseline phase. Subjects were recruited from fliers placed in local medical doctor's offices and advertisements in a local newspaper. Enrollment criteria were verified by interview, review of headache diary, and confirming diagnosis by the subject's medical doctor. A total of 18 subjects met selection criteria and agreed to participate. Two subjects were subsequently removed from the study for involvement in a motor vehicle accident and an insufficiently maintained headache diary. Thus, 16 subjects completed all massage sessions and evaluations and are included in this report.
Massage Therapists
Subjects were randomly assigned to one of six massage therapists for the duration of the massage treatment phase. The continuity of therapist was adopted because clients typically receive treatment from the same practitioner and familiarity with the practitioner would likely reduce any anxiety associated with treatment. Massage therapists employed in this study had an average of 6 years of professional massage experience and all therapists underwent at least 6 hours of training specific to the protocol prior to study onset. To isolate the effect of the massage procedure from therapist-subject camaraderie, conversation between therapists and subjects was limited to the current treatment (e.g., depth of massage pressure, presence of referred pain); subject headache history was not discussed.
Massage Protocol
Two 45-minute massage sessions were conducted each week over a 6-week period. Each massage session was separated by at least 48 hours. Details of the massage procedure have been described previously32 and are briefly summarized in Table 1.
TABLE 1.
Outline of the Massage Procedure
| Duration (min) | Techniques Used | Tissues Addressed | Intent of Treatment |
|---|---|---|---|
| 15 | Palmar glide | Back, shoulders, chest, and neck | Tissue warm-up, increase local circulation |
| 15 | Ischemic compression, cross-fber friction | Upper trapezius, suboccipitals, sternocleidomastoid, and splenius capitis muscles | Reduce MTrP activity |
| 5 | Post-isometric relaxation | Right and lef lateral cervical fexion | Reduce MTrP activity |
| 5 | Circular or cross-fber friction | Masseter, temporalis, and occipital-frontalis muscles | Reduce muscle tension in MTrP referral zone |
| 5 | Efeurage and petrissage | Neck and shoulders | Tissue fushing and recovery |
MTrP = Myofascial trigger point; Min = minutes
Test Administration
The standardized tests described below were administered a total of 5 times occurring at 3-week intervals by a study author trained in their application (AM). Evaluation occurred twice during the baseline period, after the 6th and 12th massage, and 3 weeks after massage ended (follow-up). The tests were administered either prior to or on a day separate from massage treatment to avoid measuring an immediate effect of massage.
State-Trait Anxiety Inventory (STAI)
The STAI is a widely used self-report assessment of anxiety with use in over 8000 clinical or research studies33. It contains two 20-item scales: one scale instructs subjects to complete the measure based on how they are feeling at the present time (state anxiety) while the other scale instructs subjects to complete the measure based on how they generally feel (trait anxiety)34,35. Sample items for assessing state anxiety include “I feel at ease” and “I feel upset.” Sample items for assessing trait anxiety include “I am a steady person” and “I lack self-confidence.” Each question is scored on a point scale (1 to 4) with a higher score indicating greater anxiety. The STAI has shown good internal consistency with an alpha coefficient ranging from 0.83 to 0.9234,35.
Beck Depression Inventory (BDI-II)
The BDI-II is an instrument for measuring somatic, emotional, cognitive, and motivational symptoms observed in depression. It has been used in over 1000 research studies and has been found to detect depression as effectively as structured interviews33,36. The test consists of 21 symptom-related questions and is used to identify the degree of depression in adolescents and adults37. Each question is scored from 0-3 with a higher score indicating higher levels of depressive symptoms. The BDI-II has shown good internal consistency with an alpha coefficient of 0.8638.
Perceived Stress Scale (PSS)
The PSS is a 10-item questionnaire designed to assess the degree to which situations in one's life are appraised as stressful over a defined period of time. Targeted areas of the measure relate to aspects in life that are unpredictable, uncontrollable, and overloading39. Study participants were asked to complete the scale in regard to the previous three weeks. Each question is rated from 0 (never) to 4 (very often). Cronbach's alpha coefficient has been reported to be between 0.84 and 0.8639.
Daily Stress Inventory (DSI)
The Daily Stress Inventory (DSI) addresses the relationship between stressful life events and stress-related disorders such as chronic headache40,41. The DSI is a 58-item questionnaire designed to assess the sources and magnitude of minor stressful events over a 24-hour period. Subjects score each item on a 7-point Likert scale ranging from 1 (occurred but was not stressful) to 7 (caused me to panic); if an event did not occur, a score of 0 is given. Both the number of events identified as stressful and their impact is determined. Internal consistency has been established from a community sample of adults with Cronbach's alpha coefficient for event scores of 0.83 and for impact scores of 0.8740. To examine stress at the level of daily experiences, subjects completed the DSI at the end of each day for 7 consecutive days; a daily average was subsequently determined per published methodology42. The DSI was administered during the week prior to onset of massage treatment and the final week of massage treatment.
Smallest Real Difference (SRD) Calculation
The SRD indicates the smallest score change to denote a clinically relevant change and was calculated using published methodology43. Measurement of the STAI, BDI-II, and PSS twice prior to treatment provides a stable assessment for these variables in a TTH population. The standard deviation of the difference (SDdiff) in the two baseline measurements can then be calculated to determine the score range that would be expected due to normal fluctuation rather than a treatment effect. To evaluate whether the observed change in patient score is greater than would be expected from normal fluctuation, the SDdiff is multiplied by 1.96; observed change of at least this value implies an SRD with 95% confidence43.
Statistics
Statistical analysis was conducted using StatView for Windows (SAS Institute) with statistical significance accepted at p<0.05. The study was divided into four distinct 3-week phases: a baseline phase, at the middle of the massage phase (6 sessions), the end of the massage phase (12 sessions), and at a 3-week follow-up. The PSS, BDI-II, and STAI were administered at the beginning and end of the baseline phase; no statistical difference was detected between the two baseline assessments for any of the measures (p>0.05), and data for these two time points were subsequently averaged. Data for the STAI, BDI-II, and PSS are presented as the mean ± 95% confidence interval (CI), and statistical differences were assessed by repeated measures analysis of variance (RMANOVA). Post hoc analysis was conducted using paired t-tests with Bonferroni correction. Given the pilot nature of the study, data from each test evaluation is only compared to the baseline value; thus, the corrected p-value is 0.017. The DSI was analyzed using a paired t-test.
Results
Twelve females and four males completed the study. The mean (±SD) subject age was 43.8±9.3 (range 28-56) with subjects experiencing TTH for a median of 7.5 years (range 0.5-40). In the six months prior to study enrollment, 4 subjects reported receiving no massage and 12 reported at least 1 massage from a professional massage therapist; no subject received massage to specifically address headache pain. All subjects were white; 13 subjects met IHS criteria for chronic and 3 for episodic TTH.
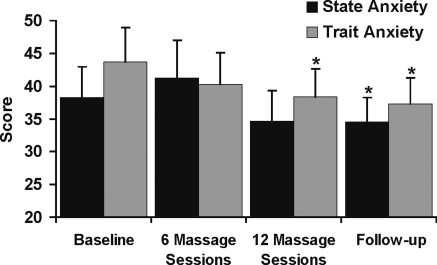
Results for the state and trait scales of the STAI are presented in Figure 1. State anxiety, which assesses perceived anxiety at the present time, changed significantly over the course of the study (p<0.01). The baseline state anxiety score was 38.3±4.7. A non-significant increase in state anxiety was noted at the midpoint of the massage phase (p=0.12; 41.2±5.8), but by the end of massage treatment, the mean score approached a significant decrease compared to baseline (p=0.02; 34.7±4.6).
FIGURE 1.
Scores for the state and trait subscales of the State-Trait Anxiety Inventory (STAI) are presented as the mean ±95% CI. A significant change in state and trait anxiety was detected across the study timeframe (p<0.01).
∗Denotes p< 0.01 compared to respective baseline.
Trait anxiety decreased over the course of the study (F(3,45)=9.0, p<0.001) with the highest score occurring during the baseline period (43.7±5.3). Post hoc analysis revealed a non-statistically significant decrease from baseline after the 6th massage (p=0.02), but statistical significance was found after the 12th massage treatment (p<0.01). The lowest score for trait anxiety took place at the follow-up measurement (p<0.01, 37.2±4.0).
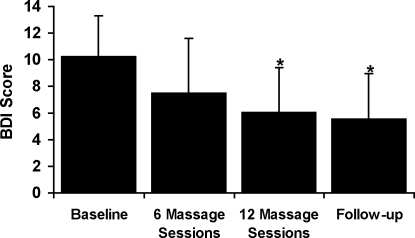
A statistically significant decrease in BDI-II score was measured across the study timeframe (Figure 2) (F(3,45) = 5.61, p<0.01). Post hoc analysis revealed a significant reduction from a score of 10.3±3.0 during baseline to 6.1±3.4 at the 6-week (12th massage) measurement and a study low of 5.6±3.4 at follow-up (p<0.01), but not after six massage sessions (7.5±4.1, p=0.12). One subject, included in the analysis, reported scores of 0 at all measurement time points.
FIGURE 2.
Scores for the Beck Depression Inventory (BDI-II) are presented as the mean ±95% CI. A significant change in the BDI-II was detected across the study timeframe (p<0.01).
∗Denotes p< 0.01 compared to baseline.
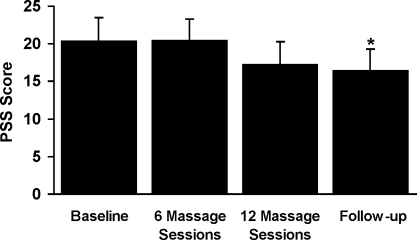
Figure 3 presents perceived stress over the course of the study as measured by the PSS (F(3,45)= 5.39, p<0.01). Post hoc analysis indicated that a statistically significant reduction in perceived stress compared to baseline (20.4±3.0) did not occur until the follow-up visit at 3 weeks following massage (p<0.01; 16.4±2.9), although a trend was apparent immediately following the massage treatment phase (p=0.059; 17.2±3.0).
FIGURE 3.
Scores for the Perceived Stress Scale (PSS) are presented as the mean±95% CI. A significant change in the PSS was detected across the study timeframe (p<0.01).
∗Denotes p< 0.01 compared to baseline.
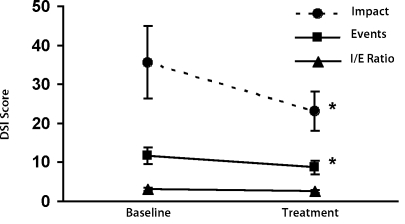
The DSI evaluated subjective stress during two 7-day periods: the last week of the baseline period and the 6th (final) week of massage treatment (Figure 4). A significant decrease in the daily number of events considered stressful was detected, with an average of 11.7 ±2.1 events during baseline decreasing to 8.7 ±1.7 events during the last week of massage (p=0.02). Similarly, the daily impact score decreased from 35.6 (±9.3) during the baseline measurement to 23.1 (±5.1) during the final week of massage (p=0.02). There was a trend for a decrease in the Impact:Event ratio (3.1±.0.5 to 2.6±0.4, p=0.09). Two subjects did not complete the diary for both 7-day periods and are not included in the analysis. Event and impact scores decreased for 11 of the 14 subjects completing both questionnaires. For two subjects where scores increased, both the number of events and their impact changed proportionately, thus resulting in no change in the Impact:Event ratio.
FIGURE 4.
Scores for the Daily Stress Inventory (DSI) are presented. The number of events considered stressful, their respective impact, and the Impact:Event ratio was determined over 7-day periods during baseline and the end of the treatment phase.
∗Denotes p< 0.02 compared to respective baseline.
Table 2 presents the percent of subjects meeting at least the smallest real difference (SRD) for each psychological measure. Based on this calculated assessment, scores for fewer than one-third of the subjects attained a clinically relevant improvement on any of the evaluations. An SDdiff calculated for STAI-state anxiety was the largest, thus requiring a greater change in score for this variable than the other assessments, and correspondingly, fewer subjects (18.8%) reached this threshold. For the STAI-trait, BDI-II, and PSS assessments, 31.3% of the subjects reached the SRD at some point during the study. Baseline scores for some subjects were sufficiently low, indicating that attainment of an SRD would not be possible. Of the 16 study subjects, five subject baseline scores on the STAI-state and BDI-II, and one subject each on the STAI-trait and PSS were too low to be able to change the SRD amount. Calculation of the percent of subjects changing the SRD with those described above held out of consideration yields a high of 27.3% for STAI-state, 45.5% for BDI-II, and 33.3% for STAI-trait and PSS.
TABLE 2.
Smallest real diference (SRD)
| Percent of subjects exceeding the SRD |
|||||
|---|---|---|---|---|---|
| Assessment | SDdiff | SRD | Treatment Phase I | Treatment Phase II | Follow-up |
| STAI-State | 7.7 | 15.0 | 0.0 | 6.25 | 18.8 |
| STAI-Trait | 4.4 | 8.7 | 12.5 | 5.0 | 31.3 |
| BDI-II | 4.7 | 9.1 | 18.8 | 18.8 | 31.3 |
| PSS | 3.3 | 6.5 | 6.25 | 31.3 | 31.3 |
STAI = State-Trait Anxiety Inventory; BDI-II = Beck Depression Inventory; PSS = Perceived Stress Scale; SDdiff = Standard deviation of the difference
Discussion
Psychological distress is frequently acknowledged in patients with TTH. From this pilot study, significant reductions across the study time frame were observed in stress, anxiety, and depression for subjects with TTH who received massage therapy. While psychological distress is more common among headache sufferers than the normal population8, few treatment-based studies specifically address this aspect. In one study involving TTH, stress management therapy was used separate from and in combination with tricyclic antidepressant medication; equal improvement in headache parameters was provided by both treatments, yet measures of stress, depression, or anxiety were not reported9,44. No studies on TTH and massage therapy have reported psychological measures. In a study on migraine headache, Lawler and Cameron45 did report a reduction in state anxiety pre/ post a massage session. Assessment was taken immediately before and after a massage session; thus, the finding may represent an acute effect of massage treatment rather than the impact of massage on state anxiety associated with migraine. That study also measured stress using the PSS, but it did not detect a change across the six-week program of once weekly massage. When matched with the same number of treatment sessions (6), the present study also did not note a change in the PSS, although across the entire study a reduction in stress was detected. The single massage a week and use of student therapists to administer treatment used in the Lawler and Cameron study contrasts with the twice-a-week treatment frequency and therapist experience level in the present study. Published research has found that student therapists may not have sufficient technical skills to bring about optimal outcomes in massage-based studies46, which may further explain why that study did not detect a change in this measure of stress.
Consistent with previous research, subjects in the present study reported pre-treatment (baseline) scores on the BDI-II and STAI of similar values to TTH patients from clinical or university research settings7,9,47. Those reports also assessed a control population and noted significantly higher scores for TTH patients on all psychological measures. Collectively, subjects in the present study reported levels of psychological distress similar to those that would be expected for a tension headache population. however, it should be noted that baseline scores on the BDI-II evaluation placed subjects at a level of “no or minimal depression,”33 which suggests that although reduced following massage treatments, depression was not a major psychological issue for the population studied. An assessment for the responsiveness of outcome measures was conducted to provide an objective evaluation of clinical improvement. This analysis identified that depending on the test instrument, 18.8-31.3% of subjects made a clinically relevant improvement over baseline. This finding may highlight that the reported statistical gains were influenced by a fewer number of individuals who responded more strongly and that massage may be more effective for a subset of the tension headache population. It should also be noted that the percent of subjects showing responsiveness might underestimate the actual effect because baseline scores for some subjects could not change by the SRD magnitude due to a basement effect; and with only 16 subjects in the study, the standard deviation on which the SRD is based could be inflated.
Two tests to evaluate stress were conducted in an effort to evaluate the impact of massage therapy on daily stressors akin to hassles (Daily Stress Inventory) and on a more general perception of stress (Perceived Stress Scale). With regard to the DSI, both the number of stressful events and their perceived impact were lessened at the end of massage treatment compared to baseline values. Because both of those measures were reduced, it is not surprising that the Impact:Events ratio did not change statistically. While a change in the PSS was detected over the course of the study, it was not until the follow-up visit, three weeks following massage, when a significant post hoc difference from baseline was detected. Questions on the DSI focus on specific daily events and are scored as to the degree of stress that each event evoked, whereas the PSS requires a 3-week recall of events and is more general in the line of questioning. The general line of questioning and the risk of recall bias inherent with the PSS may explain some of the difference in statistical findings of these two measures48. Yet it appears that a reduction in lesser (daily) stressors were more impacted by the treatment, which is in agreement with the findings from other researchers10.
Significant changes in psychological measures were detected following 6 weeks of massage (12 sessions), but not 3 weeks (6 sessions). This observation suggests that physiological or psychological manifestations from massage are not rapid changes and do not manifest until after the 6th massage session for those who are in chronic pain. Massage therapy encompasses varied techniques to lessen pain in soft tissues or to increase relaxation, both of which are important areas to address in TTH patients. A primary intent of the massage treatment in the present study was to reduce activity of MTrPs, which can be a source of local and referred pain and have been shown to be of increased incidence in headache patients30,31,49. A reduction in headache pain could subsequently result in an improvement in psychological measures. Since significant improvements in both pain32 and psychological affect were first detected at the same measurement time point (week 6), it is unclear whether the improvement in headache pain had a subsequent effect on the psychological measures.
Chronicity of headache has been associated with higher levels of perceived stress; thus, a reduction in headache frequency could result in a reduction in stress6. Massage therapy is thought to stimulate the parasympathetic branch of the autonomic nervous system, which may facilitate relaxation, thus reducing stress perception. Reduction in psychological distress has been reported for many groups who receive relaxation-oriented massage therapy24,50,51. Alongside the physical aspect, massage has also been likened to psychotherapy due to the personalized therapist-client relationship; thus, it is also possible that personal attention, independent of massage, may have an impact on psychological measures. Those arguments for the observed changes in the present study are unsatisfying. While some massage techniques used in the present study may be considered relaxing, the inclusion was to support the treatment-oriented techniques (MTrP therapy) by tissue warm-up or to facilitate tissue recovery rather than to promote relaxation. The possibility of a psychotherapy effect was intentionally minimized in this study by administering a standardized massage protocol and limiting communication to the present treatment in which personal events or even headache progression were not discussed. Therefore, it is unlikely that any relaxing massage techniques or a psychotherapy effect were major contributors to the observed reductions in psychological distress. While massage strokes that are designed to promote relaxation are thought to be more effective at reducing stress than treatment-oriented techniques, one study using MTrP therapy reported an increase in heart rate variability immediately after massage therapy, which indicated an increase in parasympathetic activity suggestive of an increased relaxation response52. Thus, reductions in stress and pain may both be achieved through MTrP therapy.
Statistical reductions in measurements of psychological distress were not evident until after 12 massage sessions. Typically, MTrPs develop over a period of time as a result of ongoing habits such as poor posture or repetitive movements. Once active, the tenacious nature of an MTrP makes resolving it a challenging task that is difficult to accomplish in patients with chronic pain unless multiple treatments are applied. In conjunction with eliminating or decreasing MTrP activity, individual habits that initially contributed to establishing the MTrP must also be addressed. Collectively, this may explain the need for multiple treatments before significant change is witnessed. It remains to be determined whether pain and psychological distress would be eliminated if the activity of pertinent MTrPs was eradicated. Although therapists in the present study reported greater difficulty locating MTrPs as the treatment phase progressed, which suggest reduced MTrP activity, it should be noted that specific measures of pain or sensitivity at MTrPs were not conducted.
One clear limitation with this study is the lack of an adequate comparison group, which reduces the ability to determine causality of the massage treatment. however, this pilot study suggests evidence for a role of massage on reducing psychological distress in a TTH population and presents an intriguing possibility for future investigations of massage for patients in chronic pain. It should also be noted that this study employed therapists with distinguished skills in massage therapy who had undergone additional training specific to the procedures and may not be representative of most massage therapists. While the techniques used are common to an educated therapist, proficiency in their application is needed to provide an optimal probability for improvement.
Conclusion
Primary (frequency) and secondary (intensity and duration) headache measures were improved for the subjects in this study32. The present report indicates that a reduction in psychological distress occurred in this population, as well. Few studies that have investigated a treatment effect for TTH have reported a full panel of psychological measures to address stress, anxiety, and depression even though these elements are frequently elevated in TTH patients. While the lack of a non-treatment comparison group limits our ability to infer causality of the massage treatment, this pilot study provides evidence that psychological distress can be reduced in TTH patients who receive a replicable massage procedure from highly trained massage therapists and is encouraging for future placebo-controlled studies in this research area.
Acknowledgements
The authors would like to thank Nathan Butryn, Maria hassett, Marjorie Johnson, Rob Killam, and Lynn St. Denis for their role as massage therapists and Alison Low Choy for technical assistance.
Footnotes
Financial support for this study was provided by the National Headache Foundation, Chicago, IL
REFERENCES
- 1.The International Classification of Headache Disorders. 2nd ed. Cephalalgia. 2004;24(Suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 2.Schwartz BS, Stewart WF, Simon D, Lipton RB. Epidemiology of tension-type headache. JAMA. 1998;279:381–383. doi: 10.1001/jama.279.5.381. [DOI] [PubMed] [Google Scholar]
- 3.Pascual J, Colas R, Castillo J. Epidemiology of chronic daily headache. Curr Pain Headache Rep. 2001;5:529–536. doi: 10.1007/s11916-001-0070-6. [DOI] [PubMed] [Google Scholar]
- 4.Stovner L, Hagen K, Jensen R, et al. The global burden of headache: A documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27:193–210. doi: 10.1111/j.1468-2982.2007.01288.x. [DOI] [PubMed] [Google Scholar]
- 5.Jensen R. Diagnosis, epidemiology, and impact of tension-type headache. Curr Pain Headache Rep. 2003;7:455–459. doi: 10.1007/s11916-003-0061-x. [DOI] [PubMed] [Google Scholar]
- 6.Martin PR, Soon K. The relationship between perceived stress, social support and chronic headaches. Headache. 1993;33:307–314. doi: 10.1111/j.1526-4610.1993.hed3306307.x. [DOI] [PubMed] [Google Scholar]
- 7.Ficek SK, Wittrock DA. Subjective stress and coping in recurrent tension-type headache. Headache. 1995;35:455–460. doi: 10.1111/j.1526-4610.1995.hed3508455.x. [DOI] [PubMed] [Google Scholar]
- 8.Holm JE, Holroyd KA, Hursey KG, Penzien DB. The role of stress in recurrent tension headache. Headache. 1986;26:160–167. doi: 10.1111/j.1526-4610.1986.hed2604160.x. [DOI] [PubMed] [Google Scholar]
- 9.Holroyd KA, Stensland M, Lipchik GL, Hill KR, O'Donnell FS, Cordingley G. Psychosocial correlates and impact of chronic tension-type headaches. Headache. 2000;40:3–16. doi: 10.1046/j.1526-4610.2000.00001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fernandez E, Sheffield J. Relative contributions of life events versus daily hassles to the frequency and intensity of headaches. Headache. 1996;36:595–602. doi: 10.1046/j.1526-4610.1996.3610595.x. [DOI] [PubMed] [Google Scholar]
- 11.Mongini F, Rota E, Deregibus A, et al. Accompanying symptoms and psychiatric comorbidity in migraine and tension-type headache patients. J Psychosom Res. 2006;61:447–451. doi: 10.1016/j.jpsychores.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 12.Heckman BD, Holroyd KA. Tension-type headache and psychiatric comorbidity. Curr Pain Headache Rep. 2006;10:439–447. doi: 10.1007/s11916-006-0075-2. [DOI] [PubMed] [Google Scholar]
- 13.Juang KD, Wang SJ, Fuh JL, Lu SR, Su TP. Comorbidity of depressive and anxiety disorders in chronic daily headache and its subtypes. Headache. 2000;40:818–823. doi: 10.1046/j.1526-4610.2000.00148.x. [DOI] [PubMed] [Google Scholar]
- 14.Guidetti V, Galli F, Fabrizi P, et al. Headache and psychiatric comorbidity: Clinical aspects and outcome in an 8-year follow-up study. Cephalalgia. 1998;18:455–462. doi: 10.1046/j.1468-2982.1998.1807455.x. [DOI] [PubMed] [Google Scholar]
- 15.Puca F, Genco S, Savarese M. Stress, depression, and anxiety in primary headache sufferers: Evaluation by means of the SCL90-R. Headache Quarterly. 1992;3:187–192. [Google Scholar]
- 16.Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997: Results of a follow-up national survey. JAMA. 1998;280:1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 17.Rossi P, Di Lorenzo G, Faroni J, Malpezzi MG, Cesarino F, Nappi G. Use of complementary and alternative medicine by patients with chronic tension-type headache: Results of a headache clinic survey. Headache. 2006;46:622–631. doi: 10.1111/j.1526-4610.2006.00412.x. [DOI] [PubMed] [Google Scholar]
- 18.Kaynak Key FN, Donmez S, Tuzun U. Epidemiological and clinical characteristics with psychosocial aspects of tension-type headache in Turkish college students. Cephalalgia. 2004;24:669–674. doi: 10.1111/j.1468-2982.2004.00736.x. [DOI] [PubMed] [Google Scholar]
- 19.Bag B, Karabulut N. Pain-relieving factors in migraine and tension-type headache. Int J Clin Pract. 2005;59:760–763. doi: 10.1111/j.1368-5031.2005.00535.x. [DOI] [PubMed] [Google Scholar]
- 20.Zanchin G, Maggioni F, Granella F, Rossi P, Falco L, Manzoni GC. Self-administered pain-relieving manoeuvres in primary headaches. Cephalalgia. 2001;21:718–726. doi: 10.1046/j.1468-2982.2001.00199.x. [DOI] [PubMed] [Google Scholar]
- 21.Puustjarvi K, Airaksinen O, Pontinen PJ. The effects of massage in patients with chronic tension headache. Acupunct Electrother Res. 1990;15:159–162. doi: 10.3727/036012990816358234. [DOI] [PubMed] [Google Scholar]
- 22.Quinn C, Chandler C, Moraska A. Massage therapy and frequency of chronic tension headaches. Am J Public Health. 2002;92:1657–1661. doi: 10.2105/ajph.92.10.1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brennan MK, De Bate RD. The effect of chair massage on stress perception of hospital bedside nurses. J Bodywork Movement Ther. 2006;10:335–342. [Google Scholar]
- 24.Cowen VS, Burkett L, Bredimus J, et al. A comparative study of Thai massage and Swedish massage relative to physiological and psychological measures. J Bodywork Movement Ther. 2006;10:266–275. [Google Scholar]
- 25.Shulman KR, Jones GE. The effectiveness of massage therapy intervention on reducing anxiety in the workplace. J Applied Behavioral Sci. 1996;32:160–173. [Google Scholar]
- 26.Field T, Peck M, Krugman S, et al. Burn injuries benefit from massage therapy. J Burn Care Rehabil. 1998;19:241–244. doi: 10.1097/00004630-199805000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Preyde M. Effectiveness of massage therapy for subacute low-back pain: A randomized controlled trial. Canadian Med Assoc J. 2000;162:1815–1820. [PMC free article] [PubMed] [Google Scholar]
- 28.Long L, Huntley A, Ernst E. Which complementary and alternative therapies benefit which conditions? A survey of the opinions of 223 professional organizations. Complement Ther Med. 2001;9:178–185. doi: 10.1054/ctim.2001.0453. [DOI] [PubMed] [Google Scholar]
- 29.Fernandez-de-Las-Penas C, Alonso-Blanco C, Cuadrado ML, Gerwin RD, Pareja JA. Myofascial trigger points and their relationship to headache clinical parameters in chronic tension-type headache. Headache. 2006;46:1264–1272. doi: 10.1111/j.1526-4610.2006.00440.x. [DOI] [PubMed] [Google Scholar]
- 30.Fernandez-de-Las-Penas C, Ge HY, Arendt-Nielsen L, Cuadrado ML, Pareja JA. Referred pain from trapezius muscle trigger points shares similar characteristics with chronic tension type headache. Eur J Pain. 2007;11:475–482. doi: 10.1016/j.ejpain.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 31.Fernandez-de-Las-Penas C, Alonso-Blanco C, Cuadrado ML, Pareja JA. Myofascial trigger points in the suboccipital muscles in episodic tension-type headache. Man Ther. 2006;11:225–230. doi: 10.1016/j.math.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 32.Moraska A, Chandler C. Changes in clinical parameters in patients with tension-type headache following massage therapy: A pilot study. J Man Manip Ther. 2008;16:106–112. doi: 10.1179/106698108790818468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Groth-Marnat G. Handbook of Psychological Assessment. 4th ed. Hoboken, NJ: John Wiley; 2003. [Google Scholar]
- 34.Spielberger C, Gorsuch R, Lushene R. The State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- 35.Spielberger C, Gorsuch R, Lushene R, Vagg P, Jacobs G. State-Trait Anxiety Inventory. Redwood City, CA: Mind Garden; 1983. [Google Scholar]
- 36.Stukenburg K. Depression scale validation screening. Psych Assess. 1990;2:134–138. [Google Scholar]
- 37.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 38.Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 39.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 40.Brantley PJ, Waggoner CD, Jones GN, Rappaport NB. A Daily Stress Inventory: Development, reliability, and validity. J Behav Med. 1987;10:61–74. doi: 10.1007/BF00845128. [DOI] [PubMed] [Google Scholar]
- 41.Zalaquett CP, Wood RJ. Evaluating Stress: A Book of Resources. Lanham, MD: Scarecrow Press; 1998. [Google Scholar]
- 42.Brantley PJ, Dietz LS, McKnight GT, Jones GN, Tulley R. Convergence between the Daily Stress Inventory and endocrine measures of stress. J Consult Clin Psychol. 1988;56:549–551. doi: 10.1037//0022-006x.56.4.549. [DOI] [PubMed] [Google Scholar]
- 43.de Vet HC, Bouter LM, Bezemer PD, Beurskens AJ. Reproducibility and responsiveness of evaluative outcome measures: Theoretical considerations illustrated by an empirical example. Int J Technol Assess Health Care. 2001;17:479–487. [PubMed] [Google Scholar]
- 44.Holroyd KA, O'Donnell FJ, Stensland M, Lipchik GL, Cordingley GE, Carlson BW. Management of chronic tension-type headache with tricyclic antidepressant medication, stress management therapy, and their combination: A randomized controlled trial. JAMA. 2001;285:2208–2215. doi: 10.1001/jama.285.17.2208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lawler SP, Cameron LD. A randomized, controlled trial of massage therapy as a treatment for migraine. Ann Behav Med. 2006;32:50–59. doi: 10.1207/s15324796abm3201_6. [DOI] [PubMed] [Google Scholar]
- 46.Moraska A. Therapist education impacts the massage effect on post-race muscle recovery. Med Sci Sports Exerc. 2007;39:34–37. doi: 10.1249/01.mss.0000240320.16029.d2. [DOI] [PubMed] [Google Scholar]
- 47.Andrasik F, Blanchard EB, Arena JG, Teders SJ, Teevan RC, Rodichok LD. Psychological functioning in headache sufferers. Psychosom Med. 1982;44:171–182. doi: 10.1097/00006842-198205000-00003. [DOI] [PubMed] [Google Scholar]
- 48.Wittrock DA, Foraker SL. Tension-type headache and stressful events: The role of selective memory in the reporting of stressors. Headache. 2001;41:482–493. doi: 10.1046/j.1526-4610.2001.01086.x. [DOI] [PubMed] [Google Scholar]
- 49.Fernandez-de-Las-Penas C, Ge HY, Arendt-Nielsen L, Cuadrado ML, Pareja JA. The local and referred pain from myofascial trigger points in the temporalis muscle contributes to pain profile in chronic tension-type headache. Clin J Pain. 2007;23:786–792. doi: 10.1097/AJP.0b013e318153496a. [DOI] [PubMed] [Google Scholar]
- 50.Cassileth BR, Vickers AJ. Massage therapy for symptom control: Outcome study at a major cancer center. J Pain Symptom Manage. 2004;28:244–249. doi: 10.1016/j.jpainsymman.2003.12.016. [DOI] [PubMed] [Google Scholar]
- 51.Bost N, Wallis M. The effectiveness of a 15-minute weekly massage in reducing physical and psychological stress in nurses. Aust J Advanc Nurs. 2006;23:28–33. [PubMed] [Google Scholar]
- 52.Delaney J, Leong KS, Watkins A, Brodie D. The short-term effects of myofascial trigger point massage therapy on cardiac autonomic tone in healthy subjects. J Advanc Nurs. 2002;37:364–371. doi: 10.1046/j.1365-2648.2002.02103.x. [DOI] [PubMed] [Google Scholar]