Abstract
A significant number of burn and other traumatic injuries are reported to occur under the influence of alcohol (EtOH) intoxication. Despite this overwhelming association between EtOH intoxication and injury, relatively little attention has been paid to determining the role of EtOH in post-injury pathogenesis. This article reviews studies which have evaluated the impact of EtOH on post-burn intestinal immunity and barrier functions. The findings from these studies suggest that while a smaller burn injury by itself may not have an adverse effect on host defense, when combined with prior EtOH intoxication it may become detrimental. Experimental data from our laboratory further supports the notion that EtOH intoxication before burn injury suppresses intestinal immune defense, impairs gut barrier functions, and increases bacterial growth. This results in increased bacterial translocation which may contribute to post injury pathogenesis. Altogether, the studies reviewed in this article suggest that EtOH intoxication at the time of injury is a risk factor, and therefore blood EtOH should be checked in burn/trauma patients at the time of hospital admission.
Keywords: Inflammation, tissue damage, trauma
Trauma remains the leading cause of death among people between 1–44 years of age. Burn injury, which is one type of major trauma, is very common at all ages. Nearly one million burn injuries are reported every year in the United States.[1] Burns and trauma are also a major cause of morbidity and mortality in other parts of the world. However, the extent of the problem is poorly documented, particularly in the developing and underdeveloped countries, including in India. Studies have shown that many of these injuries are sustained under the influence of alcohol (EtOH). An analysis of the data indicates that in the United States, nearly half of the burn patients are found positive for blood EtOH at the time of hospital admission.[2–14] A more or less similar proportion of other trauma are also reported to occur in patients under the influence of EtOH.[2,3,11,12,15,16] A few studies have examined the effect of EtOH intoxication on the management of trauma patients. Findings from these studies indicated that intoxicated patients require frequent intubations. Furthermore, they, experience delayed wound healing, and longer hospital stay.[2–16] These findings further suggest that intoxicated patients are more susceptible to infection, and the overall mortality is also relatively higher in intoxicated patients compared to burn patients who have not consumed EtOH prior to injury.[2,3,5–7,9–13] Since the focus of this article is on the intestine, we attempted to review the findings on the effect of EtOH on post-burn intestinal immune and epithelial barrier function.
EtOH INTOXICATION AND POST-BURN HOST DEFENSE
Both experimental and clinical findings indicate that EtOH intoxication has adverse effects on many organs[2,3,11,17–19]; however, the effect of EtOH abuse on morbidity and mortality following burn injury and other trauma remains largely unknown. Studies have shown that in the absence of EtOH intoxication burn injury induces an inflammatory response characterized by uncontrolled production of inflammatory mediators, including cytokines and chemokines, and leukocyte infiltration. However, the adaptive arm of the immune defense, such as antigen presentation, T-cell proliferation, and IL-2 production, is severely suppressed.[20–22] This results in a decrease in host resistance and increase in susceptibility to infection. Similar alterations in immune responses are also reported following EtOH intoxication.[2,11,17–19] In recent years, experimental models were developed to study the impact of EtOH on host defense and other organ functions following burn injury. Results from these studies, as summarized in Figure 1, suggest that acute EtOH intoxication prior to burn injury exacerbates the suppression of host defense and enhances susceptibility to bacterial infection.[2,3,11,17–19] Although, the initial release of cytokines or other inflammatory mediators is a normal host response to injury, if it remains unchecked it can lead to multiorgan dysfunction and failure, which is a major cause of death in injured patients. A common factor in many of these complications is suggested to be the bacteria or their products originating from the intestine. The intestine has therefore become the focus of many studies in the recent past.[23–26]
Figure 1.
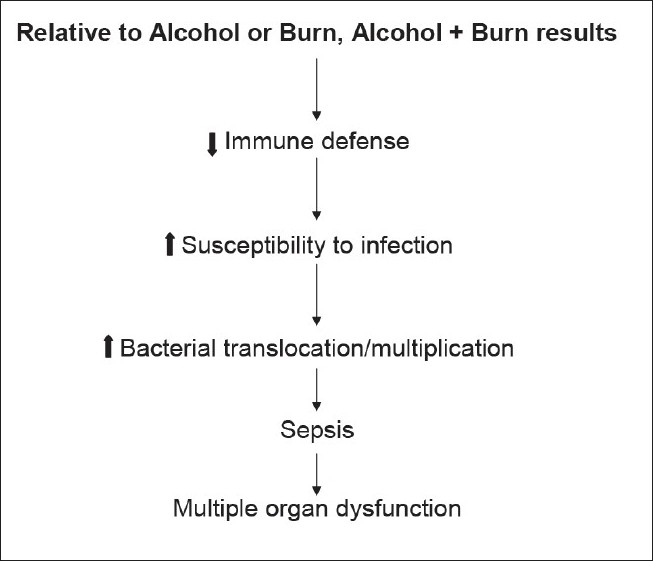
Acute alcohol intoxication exacerbates the suppression in immunity and host defense leading to organ dysfunction that is seen following burn injury
EtOH AND POST-BURN INTESTINAL IMMUNITY
The intestine maintains a mucosal and immunological barrier that is normally effective in keeping bacteria within the intestinal lumen. However, these defense mechanisms are impaired in individuals with a history of EtOH abuse and in some disease conditions. The intestinal immune system, also known as the gut-associated lymphoid tissue (GALT), consists of Peyer's patches (PP), mesenteric lymph nodes (MLN), and a large number of immune cells distributed throughout the lamina propria (LP) and epithelium of the intestine.[2] Only few studies could be found in the literature that have examined the effects of EtOH on intestinal immune defense.[2,27,28] The findings from these studies suggested that EtOH consumption is associated with increased intestinal immune cell apoptosis and suppression of immune cell effector response.[2,27,28] Our laboratory has been studying the mechanism by which EtOH intoxication combined with burn injury impairs intestinal immunity. We used a rat model of acute EtOH intoxication and burn injury.[2,29,30] Rats in this model received a single dose of EtOH by gavage feeding of 5 ml of 20% EtOH 4 h prior to burn injury. The results obtained using this model suggest that on day 1 after injury, the suppression in MLN T-cell proliferation and IL-2 production was evident only in the group that had the combined insult of EtOH intoxication and burn injury, while no significant suppression in MLN T-cells was observed in rats receiving either EtOH intoxication or burn injury alone. In contrast, on day 2 after injury, there was a decrease in MLN T-cell function following burn injury alone in the absence of EtOH intoxication, but the suppression was greater in the group receiving combined insult of EtOH intoxication and burn injury than in the rats receiving burn injury alone.[2,29,31–34] These findings collectively suggest that a single dose of acute EtOH may not be sufficient to suppress the T-cell responses; however, in combination with burn injury, EtOH can exacerbate the suppression of T-cell response following the injury. Another study[35] examined the effect of chronic EtOH on post-burn complications; it also compared the effects of enteral (oral) and intravenous administration of EtOH. Rats received 20% EtOH daily for 14 days by gavage (oral) or superior vena cava (intravenous) infusion. Four hours after the final dose of EtOH on day 14, the rats underwent a 30% total body surface area (TBSA) full-thickness burn injury. On day 4 after the burn injury, the rats were killed and various immune and gastrointestinal function parameters were determined. The findings suggest that oral, but not intravenous, administration of EtOH induced significant immunologic and gastrointestinal dysfunction. Furthermore, chronic EtOH abuse with or without burn injury results in a significantly greater suppression of lymphocyte proliferation, damage to intestinal mucosa, and increase in bacterial translocation.[35] These results suggest that both acute and chronic EtOH ingestion prior to burn injury may result in a synergistic alteration of intestinal immunity and barrier function.
EtOH AND POST-BURN INTESTINAL BARRIER FUNCTION
EtOH is known to cause toxic effects in the liver, pancreas, and gastrointestinal tract.[36–41] Absorption of EtOH occurs throughout the entire intestinal mucosa, but studies indicate that absorption is faster in the duodenum and jejunum.[36,41–44] There is evidence that both acute and chronic EtOH consumption affects the structure and function of the entire gastrointestinal tract.[36,41–43] Acute administration of EtOH results in the loss of epithelium at the tips of the villi, hemorrhagic erosions, hemorrhage in the lamina propria, and inflammatory cell infiltration.[45] However, the degree of mucosal damage is dependent on the dose of EtOH and the manner in which EtOH is administered.
Similarly, chronic EtOH ingestion has been found to cause damage in the mucosa of the small intestine. Studies have shown that rats gavaged daily with 3 ml of 20% EtOH for 4 and 8 weeks exhibited flattening and blunting of villi in the jejunal mucosa.[41] These changes in intestinal morphology were accompanied with an increase in intestinal permeability. In an another study, Keshavarzian et al.[46] showed that chronic EtOH consumption reversibly affects the integrity of small intestinal villi in men. In yet another study, Rossi et al.[47] have shown that alcoholic animals exhibited conspicuous alterations in their mitochondria and endoplasmic reticulum. Altogether, these findings suggest that EtOH abuse impairs the intestinal barrier function.
The intestine is continuously exposed to the outside environment. It is a major reservoir of nutrients, proteolytic enzymes, bacteria, and bacterial toxins. Under healthy conditions, the intestine maintains a mucosal barrier, which permits selective absorption of nutrients into the circulation. This barrier also functions as a local defense, preventing bacteria and endotoxin contained within the intestinal lumen from translocating to extraintestinal sites. However, this mucosal barrier is impaired in various pathologic conditions, including in burns and trauma.[48–54] Increased bacterial translocation is the most common marker of intestine tissue injury.
Many studies have indicated that burn injury causes gut mucosal atrophy, alters mucosal integrity, and deteriorates intestinal mucosal barrier function.[2,50,55–59] It was found that a small burn injury (< 20% TBSA) did not induce bacterial translocation.[53] In contrast, a relatively larger burn area (40% TBSA) caused a significant increase in viable bacterial translocation. Similarly, Fazal et al.[50] have indicated that there is enhanced translocation of viable bacteria into the mucosal tissue, PP, and MLN at day 1 after injury in rats receiving 30% TBSA burn injury. Thus, the severity of the injury may be a factor in post-burn pathogenesis.
Only few studies in the literature have examined the effect of EtOH intoxication on the intestine barrier following burn injury. In one study,[35] rats were fed on EtOH by gavage for 14 days prior to receiving a 30% TBSA burn injury. The translocation of bacteria was determined 4 days after burn injury. The results show a significant increase in bacterial translocation in rats receiving a combined insult of EtOH intoxication and burn injury compared with rats receiving either EtOH intoxication or burn injury alone. Studies in our laboratory have evaluated the effect of a single dose of EtOH (5 ml of 20% EtOH) on post-burn intestinal barrier function.[29,31,33,60] We found that as compared to control, rats receiving a single dose of EtOH exhibited an increase in intestinal permeability on day 1 but not on day 2.[29,31,33] In contrast, burn injury (12.5% TBSA) alone did not influence the intestine permeability on day 1 after injury. However, a tendency for an increase in intestinal permeability was observed in rats receiving burn injury alone on day 2 after injury as compared to sham controls. The combined insult of EtOH and burn injury resulted in a significant increase in intestinal permeability on both days.[29,31,33,60] This was accompanied by an increase in the number of bacteria in the MLN. Thus, it appears that EtOH intoxication before injury acts synergistically with the injury to adversely affect intestinal barrier functions and thus increase bacterial translocation.
EtOH AND POST-BURN INTESTINAL BACTERIAL GROWTH
Under healthy conditions, a few indigenous bacteria continuously translocate to the MLN, but because of the intact immune defense these bacteria do not survive. Thus, the MLN from normal animals remains relatively sterile. However, EtOH ingestion, with or without burn injury, disrupts the effective mucosal defense, leading to the passage of viable bacteria across the luminal barrier to the MLN and distant organs. The definitive pathways by which bacteria reach the MLN and systemic organs following EtOH and burn injury are uncertain and remain to be established. ‘M cells’ which are the specialized epithelial cells in the PP may serve as a carrier for translocating bacteria.[61] The pathogens, once they cross the gut epithelial barrier through M cells, come in contact with the immune cells of the PP and are cleared if the immune cells are functioning normally. However, when PP immune cell functions are not intact, these bacteria are not cleared; rather, the immune cells (e.g., macrophages or dendritic cells) may become the carrier and transport the bacteria from the PP to the MLN and from the MLN to the systemic circulation. As reviewed in a previous article,[2] studies have shown spontaneous gut bacterial translocation to the MLN, spleen, and liver in athymic (nu/nu) mice, whereas no translocation was noticed in heterozygous (nu/+) or nude (+/+) mice grafted with thymus. To determine whether T-cell-dependent immunity is critical for defense against enteric bacteria, we performed an experiment using rats in which T-cells were depleted prior to EtOH intoxication and burn injury. The data obtained from this experiment suggest that the depletion of CD3+ cells in healthy rats caused an increase in the bacterial accumulation in the MLN. Furthermore, CD3+ cells depletion in EtOH plus burn-injured rats appeared to promote the spread of bacteria to the spleen and the systemic circulation.[29]
EtOH AND POST-BURN INTESTINAL BACTERIAL GROWTH
Under physiological conditions, nearly 1012-1015 bacteria are present in the intestine.[62,63] Of these nearly 109are potentially pathogenic gram-negative enteric bacteria. Under healthy conditions, these bacteria normally reside in the lower part of the gastrointestinal tract. Studies have shown that individuals with a history of heavy EtOH use had an increase in intestinal bacterial growth, and in many cases these bacteria started colonizing the upper part of the gastrointestinal tract.[2,64,65] In one study, 89 patients with alcoholic cirrhosis and 40 healthy subjects were enrolled to assess the prevalence of intestinal bacterial overgrowth and its relationship with the severity of liver dysfunction.[66] The findings from this study suggested intestinal bacterial overgrowth in nearly 30% (27 out of 89) of the patients with alcoholic cirrhosis. Furthermore, the study concluded that intestinal bacterial overgrowth occurs in patients with advanced liver dysfunction. Although the mechanism by which EtOH influences bacterial growth remains unclear, there are reports suggesting that neurochemicals can directly influence the growth and virulence of bacteria.[67] Since both EtOH intoxication and burn injury influence hormonal levels, it is likely that these changes in hormone levels may affect bacterial growth. However, studies are needed to confirm such a role for hormones in the increase in bacterial growth or virulence. Another possibility is that individuals with a history of EtOH abuse have impaired intestinal peristalsis, which increases the likelihood of bacterial growth. In one study we examined the effect of acute EtOH intoxication on post-burn intestinal bacterial growth [Figure 2]. The finding from this study indicates that although administration of a single dose of EtOH did not influence the intestine bacterial number, it significantly enhanced the bacterial growth following burn injury.[31]
Figure 2.
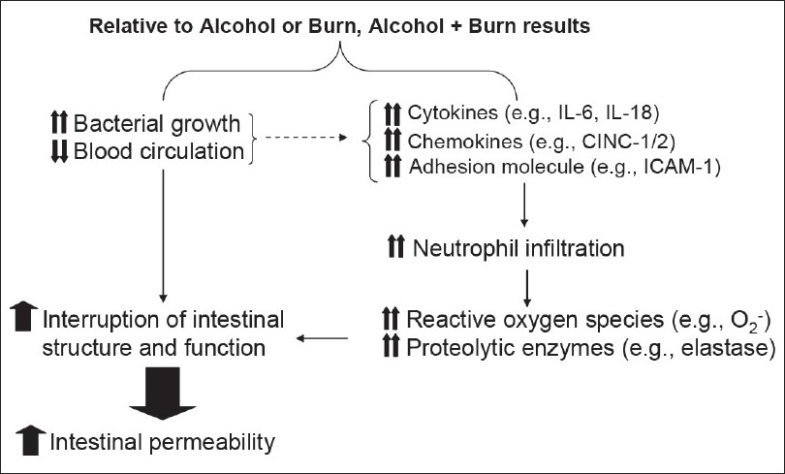
Diagrammatic representation of the events leading to increased intestine permeability following a combined insult of alcohol and burn injury
The question whether increased bacterial growth causes increase in bacterial translocation following EtOH, either alone or in combination with burn injury, remains to be answered. A few studies have suggested that anaerobic intestinal bacteria are 100- to 1000-fold more numerous than the gram-negative enteric bacteria and are closely associated with the intestinal epithelial lining.[62,63] The presence of this large number of anaerobic bacteria prevents gram-negative enteric bacteria from gaining attachment to the intestinal epithelial lining. Furthermore, studies have also shown that this ratio of anaerobic bacteria to gram-negative bacteria changes following ingestion of broad-spectrum antibiotics, to which the anaerobes are more sensitive.[62,63] Such a decrease in anaerobic bacterial numbers increases the possibility of the attachment of gram-negative pathogens to intestinal epithelial lining and their subsequent translocation to extra-intestinal sites. Although it is not clear whether EtOH influences this ratio, findings from the studies suggest an increase in gram-negative bacteria following EtOH abuse.[64,68] Thus, any change in intestinal bacterial growth, as is observed following EtOH intoxication plus burn injury, may result in bacterial translocation [Figure 2]. However, more studies are needed to confirm this paradigm.
EtOH AND POST-BURN INTESTINE INFLAMMATORY RESPONSE
Several lines of evidence indicate that EtOH intoxication, as well as injury such as burn and trauma, results in an increase in the inflammatory mediators. As summarized in Figure 2 these include, for example, the infiltration of leukocytes, such as neutrophils; the production of cytokines, such as IL-6 and IL-10; and chemokines IL-8, MIP, MCP-1 cytokine-induced neutrophil chemoattractant (CINC), and adhesion molecules (e.g., ICAM). Furthermore, the increase in these inflammatory mediators has been proposed to contribute to tissue damage under those conditions.[50,56,57,68–80] Previous findings from our laboratory have shown that acute EtOH intoxication combined with burn injury enhances IL-18 production in various lymphoid organs and in the intestine.[33,81] There was also an increase in intestinal tissue neutrophil infiltration, neutrophil chemokines, edema, and permeability.[33,60] Moreover, we found that animals treated with anti-IL-18 antibody did not exhibit an increase in intestine neutrophil infiltration, tissue edema, or increase in intestinal permeability following a combined insult of EtOH and burn injury. Similarly, other cytokines/chemokines such as IL-6, MIP, and MCP1 may also help in neutrophil recruitment. The depletion of neutrophils prior to injury prevented the increase in intestinal MPO activity, edema, and permeability after EtOH and burn injury but it did not influence IL-18 levels.[33,81] Similarly, neutrophil presence was found to be critical for the increase in intestinal permeability following burn injury.[58,59] Thus, the increase in cytokines or chemokines following major injury helps in the recruitment of neutrophils, which in turn may play a predominant role in tissue injury following major trauma and burn injury, as well as following EtOH intoxication. Neutrophil-mediated oxidant injury is demonstrated in other pathologic conditions, such as rheumatoid arthritis, acute respiratory distress syndrome, and tissue ischemia. Although an exact mechanism by which neutrophils may cause tissue damage following major injury remains to be established, studies have shown that under normal conditions neutrophils release oxygen radical species and proteolytic enzymes to kill pathogens. In various inflammatory conditions, such as burn, trauma, and acute and chronic EtOH ingestion, neutrophils are hyperactive, resulting in the excessive release of oxygen radical species and proteolytic enzymes.[33,58,82–85] Such excessive release of neutrophil reactive oxygen species and proteases has been implicated in organ tissue damage [Figure 2].
EtOH AND POST-BURN INTESTINE BLOOD FLOW
In addition to increased inflammatory mediators, changes in blood circulation to the intestine may produce alterations in intestine immune and epithelial barrier functions following EtOH and burn injury [Figure 2]. Such changes in blood circulation to the intestine could result from redistribution of the blood supply to some organs versus others. Many studies have shown that following major trauma or injury, blood supply to some organs is markedly reduced in order to maintain the functioning of the vital organs. Studies have shown that blood flow to the intestinal bed is significantly decreased following major burn injury.[52,86–90] There are two phases of cardiovascular response to burn injury.[71,72] The initial phase, referred to as the ‘hypovolemic phase,’ is characterized by decreased blood flow to tissues and organs. This is followed by a hyper-metabolic phase that is characterized by increased blood flow to the tissues and organs. Studies have also indicated that the hemodynamic response to burn injury is dependent on the size of the burn area.[86,87] Carter et al.[73] did not observe differences in intestinal and hepatic blood flow after 20% TBSA burn injury. Similarly, the studies of Ferguson et al.[76] did not show significant differences in liver and intestinal blood flow following burn injury. We examined the effect of EtOH intoxication on post-burn intestinal blood flow.[91] We did not observe a significant effect of 12.5% TBSA burn injury on hemodynamic responses. In contrast, hemodynamic responses were significantly altered when the 12.5% TBSA burn injury was combined with prior EtOH intoxication. Our findings suggest that the cardiac output and blood flow in the liver and small intestine was significantly decreased in rats receiving a combined insult of EtOH and burn injury compared to rats receiving either sham or burn injury alone.
The oxygen delivery to the liver and small intestine was also significantly decreased following EtOH plus burn injury compared to either EtOH or burn injury alone. The oxygen extraction and consumption, on the other hand, was significantly enhanced in both the organs. This difference in oxygen delivery and oxygen consumption may cause hypoxic insult to the liver and intestine. Thus, following EtOH and burn injury, such ischemic conditions may create an inflammatory environment which, in turn, may cause tissue damage in the intestine and other organs.[74,79,84–86]
CONCLUSIONS AND FUTURE RECOMMENDATIONS
The studies reviewed in this article indicate a significant association between EtOH intoxication and traumatic injuries, including burns. However, a clear picture of the role of EtOH in post-injury complications remains to be established. Findings obtained using experimental models of EtOH and burn injury indicate that a small burn injury may not produce significant alterations in immune and other organ functions; however, when it combines with prior EtOH intoxication, it becomes detrimental. Studies have also indicated that acute EtOH intoxication prior to burn injury exacerbates the suppression of intestinal immunity and deteriorates gut permeability following burn injury. There was a significant decrease in the intestine blood flow following a combined insult of EtOH intoxication and burn injury. A significant increase in bacterial growth was also observed in the intestine of rats receiving a combined insult of EtOH intoxication and burn injury. Such alterations in intestinal immunity and barrier functions may cause an increase in bacterial translocation, which in turn may contribute to organ dysfunction and pathogenesis in the injured host. Thus, studies are needed to delineate the mechanism by which alcohol intoxication combined with burn injury produces alterations not only in intestinal immunity and barrier functions but other organs also. Studies are also needed to determine whether age and gender has any role to play in the pathogenesis following alcohol and burn injury. The results from these studies will help in designing therapeutic approaches specific for the treatment of burn and trauma patients with EtOH history.
Acknowledgments
This work is supported by National Institutes of Health through grants R01AA015731 and R21AA015979 (MAC) and R01GM37127 (IHC).
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.American Burn Association. Burn incidence and treatment in the US: 2000 fact sheet. 2000 [Google Scholar]
- 2.Choudhry MA, Rana SN, Kavanaugh MJ, Kovacs EJ, Gamelli RL, Sayeed MM. Impaired intestinal immunity and barrier function: A cause for enhanced bacterial translocation in alcohol intoxication and burn injury. Alcohol. 2004;33:199–208. doi: 10.1016/j.alcohol.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 3.Choudhry MA, Gamelli RL, Chaudry IH. Alcohol abuse: A major contributing factor to post-burn/trauma immune complications. In: Vincent JL, editor. Yearbook of Intensive Care and Emergency Medicine. New York: Springer; 2004. pp. 15–26. [Google Scholar]
- 4.Grobmyer SR, Maniscalco SP, Purdue GF, Hunt JL. Alcohol, drug intoxication, or both at the time of burn injury as a predictor of complications and mortality in hospitalized patients with burns. J Burn Care Rehabil. 1996;17:532–9. doi: 10.1097/00004630-199611000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Haum A, Perbix W, Hack HJ, Stark GB, Spilker G, Doehn M. Alcohol and drug abuse in burn injuries. Burns. 1995;21:194–9. doi: 10.1016/0305-4179(95)80008-c. [DOI] [PubMed] [Google Scholar]
- 6.Jones JD, Barber B, Engrav L, Heimbach D. Alcohol use and burn injury. J Burn Care Rehabil. 1991;12:148–52. doi: 10.1097/00004630-199103000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Kelley D, Lynch JB. Burns in alcohol and drug users result in longer treatment times with more complications. J Burn Care Rehabil. 1992;13:218–20. doi: 10.1097/00004630-199203000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Marshall SW, Runyan CW, Bangdiwala SI, Linzer MA, Sacks JJ, Butts JD. Fatal residential fires: Who dies and who survives? JAMA. 1998;279:1633–7. doi: 10.1001/jama.279.20.1633. [DOI] [PubMed] [Google Scholar]
- 9.McGill V, Kowal-Vern A, Fisher SG, Kahn S, Gamelli RL. The impact of substance use on mortality and morbidity from thermal injury. J Trauma. 1995;38:931–4. doi: 10.1097/00005373-199506000-00019. [DOI] [PubMed] [Google Scholar]
- 10.McGwin G, Jr, Chapman V, Rousculp M, Robison J, Fine P. The epidemiology of fire-related deaths in Alabama, 1992-1997. J Burn Care Rehabil. 2000;21:75–83. doi: 10.1097/00004630-200021010-00016. [DOI] [PubMed] [Google Scholar]
- 11.Messingham KA, Faunce DE, Kovacs EJ. Alcohol, injury, and cellular immunity. Alcohol. 2002;28:137–49. doi: 10.1016/s0741-8329(02)00278-1. [DOI] [PubMed] [Google Scholar]
- 12.Pories SE, Gamelli RL, Vacek P, Goodwin G, Shinozaki T, Harris F. Intoxication and injury. J Trauma. 1992;32:60–4. doi: 10.1097/00005373-199201000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Powers PS, Stevens B, Arias F, Cruse CW, Krizek T, Daniels S. Alcohol disorders among patients with burns: Crisis and opportunity. J Burn Care Rehabil. 1994;15:386–91. doi: 10.1097/00004630-199407000-00017. [DOI] [PubMed] [Google Scholar]
- 14.Swenson JR, Dimsdale JE, Rockwell E, Carroll W, Hansbrough J. Drug and alcohol abuse in patients with acute burn injuries. Psychosomatics. 1991;32:287–93. doi: 10.1016/S0033-3182(91)72067-7. [DOI] [PubMed] [Google Scholar]
- 15.Maier RV. Ethanol abuse and the trauma patient. Surg Infect (Larchmt) 2001;2:133–41. doi: 10.1089/109629601750469456. [DOI] [PubMed] [Google Scholar]
- 16.Molina PE, McClain C, Valla D, Guidot D, Diehl AM, Lang CH, et al. Molecular pathology and clinical aspects of alcohol-induced tissue injury. Alcohol Clin Exp Res. 2002;26:120–8. [PubMed] [Google Scholar]
- 17.Brown LA, Cook RT, Jerrells TR, Kolls JK, Nagy LE, Szabo G, et al. Acute and chronic alcohol abuse modulate immunity. Alcohol Clin Exp Res. 2006;30:1624–31. doi: 10.1111/j.1530-0277.2006.00195.x. [DOI] [PubMed] [Google Scholar]
- 18.Hoek J, Thiele GM, Klassen LW, Mandrekar P, Zakhari S, Cook RT, et al. RSA 2004: Combined basic research satellite symposium-mechanisms of alcohol-mediated organ and tissue damage: Inflammation and immunity and alcohol and mitochondrial metabolism: at the crossroads of life and death session one: alcohol, cellular and organ damage. Alcohol Clin Exp Res. 2005;29:1735–43. doi: 10.1097/01.alc.0000179313.64522.56. [DOI] [PubMed] [Google Scholar]
- 19.Waldschmidt TJ, Cook RT, Kovacs EJ. Alcohol and inflammation and immune responses: Summary of the 2005 Alcohol and Immunology Research Interest Group (AIRIG) meeting. Alcohol. 2006;38:121–5. doi: 10.1016/j.alcohol.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 20.Lederer JA, Rodrick ML, Mannick JA. The effects of injury on the adaptive immune response. Shock. 1999;11:153–9. doi: 10.1097/00024382-199903000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Murphy TJ, Paterson HM, Mannick JA, Lederer JA. Injury, sepsis, and the regulation of Toll-like receptor responses. J Leukoc Biol. 2004;75:400–7. doi: 10.1189/jlb.0503233. [DOI] [PubMed] [Google Scholar]
- 22.Schwacha MG, Chaudry IH. The cellular basis of post-burn immunosuppression: macrophages and mediators. Int J Mol Med. 2002;10:239–43. [PubMed] [Google Scholar]
- 23.Enomoto N, Ikejima K, Bradford BU, Rivera CA, Kono H, Goto M, et al. Role of Kupffer cells and gut-derived endotoxins in alcoholic liver injury. J Gastroenterol Hepatol. 2000;15:D20–5. doi: 10.1046/j.1440-1746.2000.02179.x. [DOI] [PubMed] [Google Scholar]
- 24.Keshavarzian A, Holmes EW, Patel M, Iber F, Fields JZ, Pethkar S. Leaky gut in alcoholic cirrhosis: A possible mechanism for alcohol-induced liver damage. Am J Gastroenterol. 1999;94:200–7. doi: 10.1111/j.1572-0241.1999.00797.x. [DOI] [PubMed] [Google Scholar]
- 25.Rao RK, Seth A, Sheth P. Recent advances in alcoholic liver disease I: Role of intestinal permeability and endotoxemia in alcoholic liver disease. Am J Physiol Gastrointest Liver Physiol. 2004;286:G881–4. doi: 10.1152/ajpgi.00006.2004. [DOI] [PubMed] [Google Scholar]
- 26.Purohit V, Russo D. Cellular and molecular mechanisms of alcoholic hepatitis: Introduction and summary of the symposium. Alcohol. 2002;27:3–6. doi: 10.1016/s0741-8329(02)00211-2. [DOI] [PubMed] [Google Scholar]
- 27.Lopez MC, Watzl B, Colombo LL, Watson RR. Alterations in mouse Peyer's patch lymphocyte phenotype after ethanol consumption. Alcohol. 1997;14:107–10. doi: 10.1016/s0741-8329(96)00104-8. [DOI] [PubMed] [Google Scholar]
- 28.Sibley DA, Fuseler J, Slukvin I, Jerrells TR. Ethanol-induced depletion of lymphocytes from the mesenteric lymph nodes of C57B1/6 mice is associated with RNA but not DNA degradation. Alcohol Clin Exp Res. 1995;19:324–31. doi: 10.1111/j.1530-0277.1995.tb01510.x. [DOI] [PubMed] [Google Scholar]
- 29.Choudhry MA, Fazal N, Goto M, Gamelli RL, Sayeed MM. Gut-associated lymphoid T cell suppression enhances bacterial translocation in alcohol and burn injury. Am J Physiol Gastrointest Liver Physiol. 2002;282:G937–47. doi: 10.1152/ajpgi.00235.2001. [DOI] [PubMed] [Google Scholar]
- 30.Kawakami M, Switzer BR, Herzog SR, Meyer AA. Immune suppression after acute ethanol ingestion and thermal injury. J Surg Res. 1991;51:210–5. doi: 10.1016/0022-4804(91)90096-5. [DOI] [PubMed] [Google Scholar]
- 31.Kavanaugh MJ, Clark C, Goto M, Kovacs EJ, Gamelli RL, Sayeed MM, et al. Effect of acute alcohol ingestion prior to burn injury on intestinal bacterial growth and barrier function. Burns. 2005;31:290–6. doi: 10.1016/j.burns.2004.09.021. [DOI] [PubMed] [Google Scholar]
- 32.Li X, Rana SN, Kovacs EJ, Gamelli RL, Chaudry IH, Choudhry MA. Corticosterone suppresses mesenteric lymph node T cells by inhibiting p38/ERK pathway and promotes bacterial translocation after alcohol and burn injury. Am J Physiol Regul Integr Comp Physiol. 2005;289:R37–44. doi: 10.1152/ajpregu.00782.2004. [DOI] [PubMed] [Google Scholar]
- 33.Li X, Rana SN, Schwacha MG, Chaudry IH, Choudhry MA. A novel role for IL-18 in corticosterone-mediated intestinal damage in a two-hit rodent model of alcohol intoxication and injury. J Leukoc Biol. 2006;80:367–75. doi: 10.1189/jlb.1205745. [DOI] [PubMed] [Google Scholar]
- 34.Li X, Schwacha MG, Chaudry IH, Choudhry MA. A role of PP1/PP2A in mesenteric lymph node T cell suppression in a two-hit rodent model of alcohol intoxication and injury. J Leukoc Biol. 2006;79:453–62. doi: 10.1189/jlb.0705369. [DOI] [PubMed] [Google Scholar]
- 35.Napolitano LM, Koruda MJ, Zimmerman K, McCowan K, Chang J, Meyer AA. Chronic ethanol intake and burn injury: Evidence for synergistic alteration in gut and immune integrity. J Trauma. 1995;38:198–207. doi: 10.1097/00005373-199502000-00008. [DOI] [PubMed] [Google Scholar]
- 36.Gottfried EB, Korsten MA, Lieber CS. Alcohol-induced gastric and duodenal lesions in man. Am J Gastroenterol. 1978;70:587–92. [PubMed] [Google Scholar]
- 37.Parlesak A, Schafer C, Schutz T, Bode JC, Bode C. Increased intestinal permeability to macromolecules and endotoxemia in patients with chronic alcohol abuse in different stages of alcohol-induced liver disease. J Hepatol. 2000;32:742–7. doi: 10.1016/s0168-8278(00)80242-1. [DOI] [PubMed] [Google Scholar]
- 38.Parlesak A, Billinger MH, Bode C, Bode JC. Gastric alcohol dehydrogenase activity in man: influence of gender, age, alcohol consumption and smoking in a caucasian population. Alcohol Alcohol. 2002;37:388–93. doi: 10.1093/alcalc/37.4.388. [DOI] [PubMed] [Google Scholar]
- 39.Ramstedt M. Alcohol and pancreatitis mortality at the population level: Experiences from 14 western countries. Addiction. 2004;99:1255–61. doi: 10.1111/j.1360-0443.2004.00798.x. [DOI] [PubMed] [Google Scholar]
- 40.Sand J, Lankisch PG, Nordback I. Alcohol consumption in patients with acute or chronic pancreatitis. Pancreatology. 2007;7:147–56. doi: 10.1159/000104251. [DOI] [PubMed] [Google Scholar]
- 41.Worthington BS, Meserole L, Syrotuck JA. Effect of daily ethanol ingestion on intestinal permeability to macromolecules. Am J Dig Dis. 1978;23:23–32. doi: 10.1007/BF01072571. [DOI] [PubMed] [Google Scholar]
- 42.Krasner N, Cochran KM, Russell RI, Carmichael HA, Thompson GG. Alcohol and absorption from the small intestine, 1: Impairment of absorption from the small intestine in alcoholics. Gut. 1976;17:245–8. doi: 10.1136/gut.17.4.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Millan MS, Morris GP, Beck IT, Henson JT. Villous damage induced by suction biopsy and by acute ethanol intake in normal human small intestine. Dig Dis Sci. 1980;25:513–25. doi: 10.1007/BF01315213. [DOI] [PubMed] [Google Scholar]
- 44.Rajendram R, Preedy VR. Effect of alcohol consumption on the gut. Dig Dis. 2005;23:214–21. doi: 10.1159/000090168. [DOI] [PubMed] [Google Scholar]
- 45.Beck IT, Dinda PK. Acute exposure of small intestine to ethanol: Effects on morphology and function. Dig Dis Sci. 1981;26:817–38. doi: 10.1007/BF01309614. [DOI] [PubMed] [Google Scholar]
- 46.Keshavarzian A, Fields JZ, Vaeth J, Holmes EW. The differing effects of acute and chronic alcohol on gastric and intestinal permeability. Am J Gastroenterol. 1994;89:2205–11. [PubMed] [Google Scholar]
- 47.Rossi MA, Zucoloto S. Effect of chronic ethanol ingestion on the small intestinal ultrastructure in rats. Beitr Pathol. 1977;161:50–61. doi: 10.1016/s0005-8165(77)80109-1. [DOI] [PubMed] [Google Scholar]
- 48.Baker JW, Deitch EA, Li M, Berg RD, Specian RD. Hemorrhagic shock induces bacterial translocation from the gut. J Trauma. 1988;28:896–906. doi: 10.1097/00005373-198807000-00002. [DOI] [PubMed] [Google Scholar]
- 49.Faries PL, Simon RJ, Martella AT, Lee MJ, Machiedo GW. Intestinal permeability correlates with severity of injury in trauma patients. J Trauma. 1998;44:1031–5. doi: 10.1097/00005373-199806000-00016. [DOI] [PubMed] [Google Scholar]
- 50.Fazal N, Shamim M, Zagorski J, Choudhry MA, Ravindranath T, Sayeed MM. CINC blockade prevents neutrophil Ca(2+) signaling upregulation and gut bacterial translocation in thermal injury. Biochim Biophys Acta. 2000;1535:50–9. doi: 10.1016/s0925-4439(00)00082-x. [DOI] [PubMed] [Google Scholar]
- 51.Herndon DN, Zeigler ST. Bacterial translocation after thermal injury. Crit Care Med. 1993;21:S50–4. doi: 10.1097/00003246-199302001-00010. [DOI] [PubMed] [Google Scholar]
- 52.Horton JW. Bacterial translocation after burn injury: The contribution of ischemia and permeability changes. Shock. 1994;1:286–90. [PubMed] [Google Scholar]
- 53.Maejima K, Deitch EA, Berg RD. Bacterial translocation from the gastrointestinal tracts of rats receiving thermal injury. Infect Immun. 1984;43:6–10. doi: 10.1128/iai.43.1.6-10.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Russell DH, Barreto JC, Klemm K, Miller TA. Hemorrhagic shock increases gut macromolecular permeability in the rat. Shock. 1995;4:50–5. doi: 10.1097/00024382-199507000-00008. [DOI] [PubMed] [Google Scholar]
- 55.Magnotti LJ, Deitch EA. Burns, bacterial translocation, gut barrier function and failure. J Burn Care Rehabil. 2005;6:383–91. doi: 10.1097/01.bcr.0000176878.79267.e8. [DOI] [PubMed] [Google Scholar]
- 56.Deitch EA. Role of the gut lymphatic system in multiple organ failure. Curr Opin Crit Care. 2001;7:92–8. doi: 10.1097/00075198-200104000-00007. [DOI] [PubMed] [Google Scholar]
- 57.Deitch EA, Lu Q, Feketeova E, Hauser CJ, Xu DZ. Intestinal bacterial overgrowth induces the production of biologically active intestinal lymph. J Trauma. 2004;56:105–10. doi: 10.1097/01.TA.0000054650.15837.1B. [DOI] [PubMed] [Google Scholar]
- 58.Sir O, Fazal N, Choudhry MA, Gamelli RL, Sayeed MM. Neutrophil depletion prevents intestinal mucosal permeability alterations in burn-injured rats. Am J Physiol Regul Integr Comp Physiol. 2000;278:R1224–31. doi: 10.1152/ajpregu.2000.278.5.R1224. [DOI] [PubMed] [Google Scholar]
- 59.Sir O, Fazal N, Choudhry MA, Goris RJ, Gamelli RL, Sayeed MM. Role of neutrophils in burn-induced microvascular injury in the intestine. Shock. 2000;14:113–7. doi: 10.1097/00024382-200014020-00006. [DOI] [PubMed] [Google Scholar]
- 60.Rana SN, Li X, Chaudry IH, Bland KI, Choudhry MA. Inhibition of IL-18 reduces myeloperoxidase activity and prevents edema in intestine following alcohol and burn injury. J Leukoc Biol. 2005;77:719–28. doi: 10.1189/jlb.0704396. [DOI] [PubMed] [Google Scholar]
- 61.Rescigno M, Urbano M, Valzasina B, Francolini M, Rotta G, Bonasio R, et al. Dendritic cells express tight junction proteins and penetrate gut epithelial monolayers to sample bacteria. Nat Immunol. 2001;2:361–7. doi: 10.1038/86373. [DOI] [PubMed] [Google Scholar]
- 62.Husebye E. The pathogenesis of gastrointestinal bacterial overgrowth. Chemotherapy. 2005;51:1–22. doi: 10.1159/000081988. [DOI] [PubMed] [Google Scholar]
- 63.Swank GM, Deitch EA. Role of the gut in multiple organ failure: Bacterial translocation and permeability changes. World J Surg. 1996;20:411–7. doi: 10.1007/s002689900065. [DOI] [PubMed] [Google Scholar]
- 64.Bode C, Bode JC. Effect of alcohol consumption on the gut. Best Pract Res Clin Gastroenterol. 2003;17:575–92. doi: 10.1016/s1521-6918(03)00034-9. [DOI] [PubMed] [Google Scholar]
- 65.Hauge T, Persson J, Danielsson D. Mucosal bacterial growth in the upper gastrointestinal tract in alcoholics (heavy drinkers) Digestion. 1997;58:591–5. doi: 10.1159/000201507. [DOI] [PubMed] [Google Scholar]
- 66.Casafont MF, las Heras CG, Martin RL, Lopez Arias MJ, Ledesma F, Pons RF. Small bowel bacterial overgrowth in patients with alcoholic cirrhosis. Dig Dis Sci. 1996;41:552–6. doi: 10.1007/BF02282340. [DOI] [PubMed] [Google Scholar]
- 67.Freestone PP, Williams PH, Haigh RD, Maggs AF, Neal CP, Lyte M. Growth stimulation of intestinal commensal Escherichia coli by catecholamines: A possible contributory factor in trauma-induced sepsis. Shock. 2002;18:465–70. doi: 10.1097/00024382-200211000-00014. [DOI] [PubMed] [Google Scholar]
- 68.Bode C, Bode JC. Activation of the innate immune system and alcoholic liver disease: Effects of ethanol per se or enhanced intestinal translocation of bacterial toxins induced by ethanol? Alcohol Clin Exp Res. 2005;29:166S–71S. doi: 10.1097/01.alc.0000189280.19073.28. [DOI] [PubMed] [Google Scholar]
- 69.Bahrami S, Redl H, Yao YM, Schlag G. Involvement of bacteria/endotoxin translocation in the development of multiple organ failure. Curr Top Microbiol Immunol. 1996;216:239–58. doi: 10.1007/978-3-642-80186-0_11. [DOI] [PubMed] [Google Scholar]
- 70.Frink M, Lu A, Thobe BM, Hsieh YC, Choudhry MA, Schwacha MG, et al. Monocyte chemoattractant protein-1 influences trauma-hemorrhage-induced distal organ damage via regulation of keratinocyte-derived chemokine production. Am J Physiol Regul Integr Comp Physiol. 2007;292:R1110–6. doi: 10.1152/ajpregu.00650.2006. [DOI] [PubMed] [Google Scholar]
- 71.Hildebrand F, Hubbard WJ, Choudhry MA, Frink M, Pape HC, Kunkel SL, et al. Kupffer cells and their mediators: The culprits in producing distant organ damage after trauma-hemorrhage. Am J Pathol. 2006;169:784–94. doi: 10.2353/ajpath.2006.060010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sayeed MM. Exuberant Ca(2+) signaling in neutrophils: A cause for concern. News Physiol Sci. 2000;15:130–6. [PubMed] [Google Scholar]
- 73.Wang W, Smail N, Wang P, Chaudry IH. Increased gut permeability after hemorrhage is associated with upregulation of local and systemic IL-6. J Surg Res. 1998;79:39–46. doi: 10.1006/jsre.1998.5385. [DOI] [PubMed] [Google Scholar]
- 74.Yu HP, Hsieh YC, Suzuki T, Choudhry MA, Schwacha MG, Bland KI, et al. Mechanism of the nongenomic effects of estrogen on intestinal myeloperoxidase activity following trauma-hemorrhage: Up-regulation of the PI-3K/Akt pathway. J Leukoc Biol. 2007;82:774–80. doi: 10.1189/jlb.0307182. [DOI] [PubMed] [Google Scholar]
- 75.Zallen G, Moore EE, Johnson JL, Tamura DY, Ciesla DJ, Silliman CC. Posthemorrhagic shock mesenteric lymph primes circulating neutrophils and provokes lung injury. J Surg Res. 1999;83:83–8. doi: 10.1006/jsre.1999.5569. [DOI] [PubMed] [Google Scholar]
- 76.Bode C, Bode JC. Alcohol's role in gastrointestinal tract disorders. Alcohol Health Res World. 1997;21:76–83. [PMC free article] [PubMed] [Google Scholar]
- 77.Bode JC, Bode C, Heidelbach R, Durr HK, Martini GA. Jejunal microflora in patients with chronic alcohol abuse. Hepatogastroenterology. 1984;31:30–4. [PubMed] [Google Scholar]
- 78.Deitch EA, Berg R. Bacterial translocation from the gut: A mechanism of infection. J Burn Care Rehabil. 1987;8:475–482. [PubMed] [Google Scholar]
- 79.Guo W, Ding J, Huang Q, Jerrells T, Deitch EA. Alterations in intestinal bacterial flora modulate the systemic cytokine response to hemorrhagic shock. Am J Physiol. 1995;269:G827–32. doi: 10.1152/ajpgi.1995.269.6.G827. [DOI] [PubMed] [Google Scholar]
- 80.Guo W, Magnotti LJ, Ding J, Huang Q, Xu D, Deitch EA. Influence of gut microflora on mesenteric lymph cytokine production in rats with hemorrhagic shock. J Trauma. 2002;52:1178–85. doi: 10.1097/00005373-200206000-00026. [DOI] [PubMed] [Google Scholar]
- 81.Li X, Schwacha MG, Chaudry IH, Choudhry MA. Acute Alcohol intoxication potentiates neutrophil-mediated intestine tissue damage following burn injury. Shock. 2007;29:377–83. doi: 10.1097/shk.0b013e31815abe80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Botha AJ, Moore FA, Moore EE, Kim FJ, Banerjee A, Peterson VM. Postinjury neutrophil priming and activation: An early vulnerable window. Surgery. 1995;118:358–64. doi: 10.1016/s0039-6060(05)80345-9. [DOI] [PubMed] [Google Scholar]
- 83.Deitch EA, Bridges W, Berg R, Specian RD, Granger DN. Hemorrhagic shock-induced bacterial translocation: The role of neutrophils and hydroxyl radicals. J Trauma. 1990;30:942–51. doi: 10.1097/00005373-199008000-00002. [DOI] [PubMed] [Google Scholar]
- 84.Fazal N, Al Ghoul WM, Schmidt MJ, Choudhry MA, Sayeed MM. Lyn- and ERK-mediated vs Ca+ -mediated neutrophil O responses with thermal injury. Am J Physiol Cell Physiol. 2002;283:C1469–79. doi: 10.1152/ajpcell.00114.2002. [DOI] [PubMed] [Google Scholar]
- 85.Dobke MK, Deitch EA, Harnar TJ, Baxter CR. Oxidative activity of polymorphonuclear leukocytes after thermal injury. Arch Surg. 1989;124:856–9. doi: 10.1001/archsurg.1989.01410070116023. [DOI] [PubMed] [Google Scholar]
- 86.Carter EA, Tompkins RG and Burke JF. Hepatic and intestinal blood flow following thermal injury. J Burn Care Rehabil. 1988;9:347–350. doi: 10.1097/00004630-198807000-00006. [DOI] [PubMed] [Google Scholar]
- 87.Ferguson JL, Merrill GF, Miller HI, Spitzer JJ. Regional blood flow redistribution during early burn shock in the guinea pig. Circ Shock. 1977;4:317–26. [PubMed] [Google Scholar]
- 88.Jones WG, Minei JP, Barber AE, Fahey TJ, 3rd, Shires GT, 3rd, Shires GT. Splanchnic vasoconstriction and bacterial translocation after thermal injury. Am J Physiol Heart Circ Physiol. 1991;261:H1190–6. doi: 10.1152/ajpheart.1991.261.4.H1190. [DOI] [PubMed] [Google Scholar]
- 89.Lorente JA, Ezpeleta A, Esteban A, Gordo F, de la Cal MA, Diaz C, et al. Systemic hemodynamics, gastric intramucosal PCO2 changes, and outcome in critically ill burn patients. Crit Care Med. 2000;28:1728–35. doi: 10.1097/00003246-200006000-00005. [DOI] [PubMed] [Google Scholar]
- 90.Sakurai H, Traber LD, Traber DL. Altered systemic organ blood flow after combined injury with burn and smoke inhalation. Shock. 1998;9:369–74. doi: 10.1097/00024382-199805000-00010. [DOI] [PubMed] [Google Scholar]
- 91.Choudhry MA, Ba ZF, Rana SN, Bland KI, Chaudry IH. Alcohol ingestion before burn injury decreases splanchnic blood flow and oxygen delivery. Am J Physiol Heart Circ Physiol. 2005;288:H716–21. doi: 10.1152/ajpheart.00797.2004. [DOI] [PubMed] [Google Scholar]


