Abstract
The movement of Canadian nurses to the United States increased over the past decade and is an ongoing concern of health policy analysts. This study examines why Canadian nurses emigrate to the United States and whether there is interest in returning to work in Canada. A survey of Canadian-educated nurses in North Carolina showed that lack of full-time work opportunities played a key role in emigration. Focus groups of respondents revealed deep dissatisfaction with many aspects of nursing practice in Canada, particularly undervaluing of the profession. There is an urgent need for healthcare policy makers to explore what should be done to reduce the loss of this critical human resource.
Abstract
Le nombre d'infirmières et d'infirmiers canadiens qui s'installent aux États-Unis a augmenté au cours de la dernière décennie et constitue une préoccupation pour les analystes des politiques de santé. La présente étude se penche sur les raisons qui poussent le personnel infirmier à émigrer aux États-Unis et tente de voir si ces professionnels ont l'intention de revenir travailler au Canada. Un sondage effectué auprès du personnel infirmier qui a reçu sa formation au Canada et qui travaille en Caroline du Nord montre que le manque de possibilités de travail à temps plein joue un rôle important dans l'émigration. Les groupes de discussion révèlent une profonde insatisfaction envers plusieurs aspects de la pratique infirmière au Canada, particulièrement en ce qui a trait à la sous-évaluation de la profession. Les responsables de politiques de santé devraient sérieusement examiner les mesures à prendre afin de réduire les pertes touchant cette importante ressource humaine.
International mobility is known to characterize some healthcare professions (Buchan 2001), particularly nursing, which has been described as a “carousel” (Kingma 2006). Global nursing shortages create opportunities that give nurses the ability to move more easily between countries. Nurses have taken advantage of these opportunities to seek improved wages and working conditions abroad (Gamble 2002).
Increased mobility of the nursing workforce has generated concerns: one Canadian report stated that Ontario nurses were leaving to go to other jurisdictions or to jobs outside healthcare (Nursing Task Force 1999). The United States has been actively recruiting and employing foreign nurses for more than 50 years (Brush et al. 2004). Recent literature indicates that many hospitals across the United States are recruiting foreign nurses for the first time to address their staffing challenges (Brush 2008). Brush (2008) reports that 20.2% of foreign nurses entering the United States to work emigrate from Canada. Some authors have suggested that US hospitals, which employ the majority of expatriate Canadian nurses, favour Canadians because they do not experience language barriers or significant culture shock, and their education and training is comparable to that of US nurses (Elabdi 1996).
The US Health Resources and Services Administration (2004) has estimated that the United States will face a shortage of almost a million nurses by the year 2020. These numbers are staggering and affirm the urgency with which the United States is recruiting foreign-educated nurses to cope with its nursing shortage. At the same time, US immigration policy and individual state efforts to eliminate the Commission on Graduates of Foreign Nursing Schools (CGFNS) entrance examinations have facilitated foreign nurse migration (Brush and Sochalski 2007). As the rates of international nurse migration increase (Buchan et al. 2003) and, specifically, as Canadian nurses continue to migrate to the United States, the need for Canadian healthcare policy makers to act on the loss of nurses becomes more urgent to confront Canada's own nursing shortage. Although there is descriptive literature on global nurse migration, little primary research has been done to determine factors that contribute to emigration. There is also limited research on nurses' migration to specific areas of the United States. This study was aimed at addressing these research gaps by examining why Canadian nurses emigrate to the United States, specifically to North Carolina, and whether they would be interested in returning to work in Canada in the future.
Method
This study was conducted over a four-month period – from February 1 to May 31, 2006 – using a mixed-method approach. First, a cross-sectional survey research design using a sample of all RN registrants from Canada working in North Carolina was obtained from the North Carolina Board of Nursing (NCBON), the registration body for the state's registered nurses (RNs) and licensed practical nurses (LPNs). Next, four focus groups were held with a random sample of 17 Canadian nurses employed in North Carolina to verify the survey findings.
This state was selected for several reasons. First, North Carolina has reciprocal licensure with Canadian nurses, a practice that facilitates the process for Canadian nurses to acquire licenses and obtain employment in the state. Second, North Carolina is one of five states that employ a large number of Canadian nurses, third only to Texas and Florida (CGFNS 2002). Third, North Carolina hospitals reported that Canada ranked third among countries from which they were actively recruiting the greatest number of RNs, behind India and the Philippines (NCCN 2004). Fourth, the NCBON biennial registration for the state's RNs includes extensive personal data and the state/country of basic nursing education; thus, the NCBON database is of high quality and current. Finally, the team of researchers assembled for this study has extensive knowledge of the United States and Canadian nursing workforces. Specifically, at the time of this study, three of the five researchers had studied the Canadian nursing workforce for many years, four had lived and worked in North Carolina and two had extensive experience studying the US nursing workforce.
Following institutional ethics review board approval, the NCBON provided mailing labels to the researchers for all registrants who obtained their nursing education in Canada, were licensed and were currently working in North Carolina. A total of 1,412 Canadian nurse registrants were surveyed; 678 nurses (48%) responded, of which 651 (46%) questionnaires were usable. The survey, developed by the study team of researchers following a systematic review of the literature on issues related to nurse migration, was pilot-tested for face and content validity with a group of eight Canadian nurses working in the United States to ensure the relevance of the data items. The survey comprised 28 items, with some forced-choice items requiring a “yes” or “no” answer (e.g., “Do you have any plans to return to work in Canada?”) and other, open-ended items providing the opportunity for respondents to select more than one item (e.g., “Why did you come to North Carolina to work as a nurse? Please check [√] as many responses as apply”).
Survey items were grouped into four sections: (1) emigrating to work in the United States: five items capturing the timing and reasons for the study nurses' migration to North Carolina, and the types of incentives that attracted them to the United States to work; (2) current work characteristics: nine items, including work setting, position, reasons for staying in the United States to work, work environment characteristics such as nurse-to-patient ratio, and supports in place for career development and ongoing education; (3) returning to work in Canada: six items, including plans to return to work in Canada, possible incentives for returning to work in Canada and the disincentives of returning to Canada to work; and (4) demographic characteristics: eight items.
All nurses who participated in the survey were asked to indicate their interest in participating in a focus group to be held at a later point in the study. Over 80 nurses indicated interest in participating in the focus groups, from which 20 were randomly selected by the research team. A total of 17 nurses, ranging in age from 22 to 58 years (similar to the age range of the sample from the study survey reported below), attended the one-hour focus group. To improve accessibility, enable a broad range of Canadian nurses to attend and minimize excluding nurses for reasons of geography, the focus groups were held in different areas of North Carolina. The majority of focus group participants were diploma-prepared, while a few held baccalaureate degrees. The participants were asked to describe their perceptions and elaborate on the preliminary study findings regarding the migration of Canadian nurses to North Carolina. Focus groups were taped, field notes were taken and transcripts were produced. The transcripts were reviewed using a set of codes to ensure consistent interpretation and reporting. Analysis of the data resulted in the identification of various themes.
Descriptive statistics were used to analyze the survey responses. The number of responses and the percentages are reported for the open-ended items. Analysis of variance (ANOVA) was conducted to determine any significant differences in responses between the nurses who indicated interest in returning to work in Canada and those indicating no interest. The results of the thematic analysis of the focus group data were simultaneously triangulated with the survey data. The process of simultaneous triangulation was well suited to this study because it permits the complementary use of qualitative and quantitative methods. The findings were integrated at the end of the study (Morse 1991).
Results
Table 1 shows the characteristics of the Canadian nurse sample responding to the survey and compares the study nurses to other nurses working in North Carolina and the United States at this time. All study respondents were registered nurses; most were relatively young, with half the sample younger than 40 years of age. Participants were also younger than the average nurse working in North Carolina and in the United States overall. A higher proportion of study participants were male compared to nurses working in North Carolina and elsewhere in the United States. Over half the sample held diploma certification, while close to one-third were baccalaureate-prepared. The proportion of baccalaureate respondents was similar to state and US averages, although a far greater number of Canadian than US diploma-prepared nurses was apparent in this survey. Although few respondents were enrolled in educational programs at the time of the survey, more Canadian-educated nurses were enrolled in ongoing education than their counterparts working in North Carolina and the United States overall. Over three-quarters of the sample were employed full time, with a few employed part time or in casual or contract positions. This number is slightly higher than North Carolina and US averages. Few of the respondents held more than one nursing position, similar to other nurses in North Carolina and the United States overall. Over three-quarters of the participants were employed in direct patient care roles; approximately two-thirds of North Carolina and US nurses overall held direct care roles.
TABLE 1.
Characteristics of the study sample compared to US and NC nurses
| Canadian nurses in North Carolina | Working United States nurses | Working North Carolina nurses | |||||
|---|---|---|---|---|---|---|---|
| Number | Percentage | Number | Percentage | Number | Percentage | ||
| Sex | Male | 65 | 10 | 1,792 | 6.3 | 39 | 6.4 |
| Female | 586 | 90 | 26,640 | 93.7 | 573 | 93.6 | |
| Not stated | 0 | 0 | 3 | <1 | 0 | 0 | |
| Age | <30 | 74 | 11 | 2,475 | 8.7 | 63 | 10.3 |
| 30–39 | 255 | 39 | 5,664 | 19.9 | 150 | 24.5 | |
| 40–49 | 186 | 28 | 9,665 | 34.0 | 201 | 32.8 | |
| 50–59 | 102 | 16 | 8,116 | 28.5 | 150 | 24.5 | |
| >60 | 24 | 4 | 2,387 | 8.4 | 48 | 7.8 | |
| Not stated | 10 | 2 | 157 | <1 | 0 | 0 | |
| Highest educational preparation | Diploma | 348 | 55 | 4,122 | 14.5 | 74 | 12.1 |
| Baccalaureate | 201 | 31 | 9,948 | 35.0 | 198 | 32.4 | |
| Master's | 46 | 8 | 3,556 | 12.5 | 83 | 13.6 | |
| Associate degree | 35 | 5 | 10,481 | 36.9 | 248 | 40.5 | |
| Doctorate | 4 | 1 | 244 | 0.9 | 7 | 1.1 | |
| Not stated | 0 | 0 | 126 | <1 | 2 | <1 | |
| Enrolment in educational programs | No | 551 | 85 | 26,088 | 91.8 | 579 | 94.6 |
| Yes | 87 | 14 | 2,341 | 8.2 | 32 | 5.2 | |
| Not stated | 13 | 1 | 6 | <1 | 1 | <1 | |
| Work status | Full-time | 516 | 79 | 19,802 | 69.6 | 470 | 76.8 |
| Part-time | 67 | 10 | 8,596 | 30.2 | 142 | 23.2 | |
| Casual/contract | 56 | 9 | N/A | N/A | N/A | N/A | |
| Not stated | 12 | 2 | 37 | <1 | 0 | 0 | |
| Number of employers | One | 553 | 85 | 24,062 | 84.6 | 530 | 86.6 |
| More than one | 89 | 14 | 4,373 | 15.4 | 820 | 13.4 | |
| Not stated | 9 | 1 | 0 | 0 | 0 | 0 | |
| Involvement in direct patient care | Yes | 505 | 78 | 18,815 | 66.2 | 424 | 69.3 |
| No | 146 | 22 | 9,267 | 32.5 | 180 | 29.4 | |
| Not stated | 0 | 0 | 353 | 1.3 | 8 | 1.3 | |
2004 National Sample Survey of Registered Nurses, US Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions, Division of Nursing.
When did Canadian nurses migrate to North Carolina?
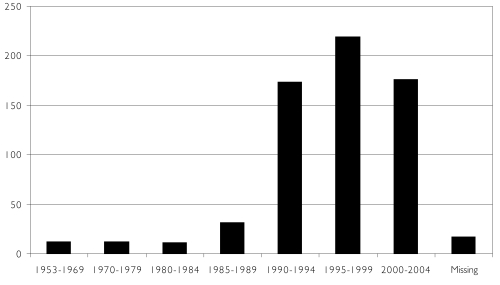
Data from the participants in this study indicate that nurse migration from Canada to North Carolina escalated in the 1990s, peaked in the latter half of that decade and remained high early into the 21st century. Figure 1 demonstrates that 27% (n=173) of nurse respondents migrated to the United States between 1990 and 1994, followed by 34% (n=219) between 1995 and 1999 and 27% (n=176) between 2002 and 2004.
FIGURE 1.
Timing of migration to North Carolina
Why do Canadian nurses move to North Carolina?
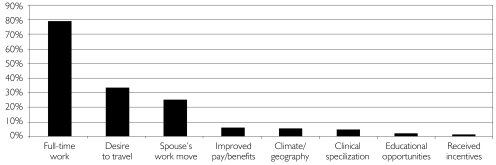
When the participants were asked to indicate their rationale for moving to the United States, over three-quarters of respondents said they left Canada to obtain full-time RN employment (see Figure 2). One-third reported leaving Canada because of a desire to travel, while one-quarter migrated with a spouse or partner who moved to the North Carolina area. Fewer respondents identified improved pay and benefits, climate or geographical location, the opportunity to specialize in a specific field, educational opportunities or targeted incentives as reasons for leaving Canada. These findings are similar to those of a study of new nursing graduates from Atlantic Canada who identified greater job availability, full-time work, appropriate orientation, packages for job benefits and career development opportunities as the key factors that influenced their decision to migrate to the United States (Gillis et al. 2004).
FIGURE 2.
Reasons for move to North Carolina
These findings were substantiated by focus group participants, who provided detailed examples of the challenges they faced seeking employment as a nurse in Canada. Focus group attendees overwhelmingly verified that their main reason for emigration to the United States was the lack of employment opportunities in Canada, in particular full-time nursing jobs.
The hospital I was working in was a very small hospital and it was basically someone had to retire or die for you to get a job because there weren't any openings. It didn't seem like there was ever going to be any openings, so we moved down here to gain full-time employment.
By the time I finished school there wasn't a job to be had, not one. The valedictorian of my class was offered a part-time position in Toronto and [for] the rest of us, there wasn't a job anywhere.
I went into nursing school knowing I was going to have to move to the States for a full-time job. My [relative] had done it ahead of me and when I finally decided I was going to nursing school, I mean, I went into it knowing I was moving, highly doubting I was going to get a job in Canada. Then by the time I finished nursing school and figured out what area I wanted to work in, I knew I wasn't getting a job in Canada in that area. There had been people that had been working in the hospital at home for seven, eight years trying to get into that department and still hadn't been able to get in, so I packed up and left.
What are the incentives for working in North Carolina?
Close to two-thirds of study participants indicated that the opportunity for full-time employment was the key incentive that North Carolina hospitals used to recruit Canadian nurses. Other important incentives included relocation assistance, salary incentives, career advancement opportunities, innovative scheduling strategies, signing bonuses, educational subsidies and organizational reputation for good physician–nurse relationships. Many of the participants indicated that more than one incentive played a role in their decision to immigrate to the United States.
Focus group participants also discussed the incentives provided to Canadian nurses. For the most part, nurse participants capitalized on the main incentive offered by North Carolina healthcare organizations that was pushing Canada's nurses to the United States: the search for full-time employment. At the same time, North Carolina's interest in Canada's nurses contrasted starkly with the situation in Canada. While some nurses in the focus groups identified salary as an incentive for migrating, the majority described North Carolina's strong interest in and valuation of Canadian nurses as a human resource.
The fact that they offered you a full-time job, I mean, that makes you feel valued other than you're just this disposable person that they're going to call when they need you.
I didn't feel very valued as a nurse in Canada, it was just kind of like you're not even just a cog in the wheel, it was like you were really low man on the totem pole, so you didn't have a lot of respect as a nurse. But coming to the States, they really wanted you and they were very happy to have you here and you were valued and respected even if, you know, I didn't get my bachelor's or my master's until much later. Just the fact that you were a Canadian-educated nurse.
Well, they paid for a luxury apartment. I mean, they paid for everything. All I had to pay was my long-distance phone bill. So they paid the heating, they paid, you know, the basic phone bill.
Why have Canadian nurses stayed in North Carolina?
One-third of the respondents identified salary as a factor influencing them to continue to work in North Carolina, while close to one-third identified benefits as a factor. As well, attempts by management to accommodate nurse schedules, good relationships between physicians and nurses, mentorship and colleagueship among nurses, opportunities for continuing education, adequate staffing levels, management that listens to nurse concerns, opportunities for career advancement, and control over nursing practice were also cited as important retention factors.
Focus group participants provided a number of reasons for staying in the United States to work as a nurse. Again, while some nurses acknowledged salary as an important factor, most described respect for nurses and good relationships between management and staff nurses as influential factors keeping them in the United States. Several described opportunities provided by management for their professional development.
Part of it is the pay, but at the same time I need to know their [hospital] reputation in the way they treat nurses, how they handle conflicts … with nurses, and I make decisions based on that. I look at the way they treat their nurses.
I have been encouraged to participate in our professional association locally and nationally. … That makes you feel valued … .
Other subtle things, like being given the opportunity or being encouraged to present at a national level, to publish in a national journal, to do a poster presentation at a national level, just to be sort of pushed off a cliff to do that and then, you know, having the feeling of being published and … just being proud of that.
One of the big things I noticed when I came down here is back home there was a big separation between management and the employees. I would never back home have dreamed of going and knocking on my manager's door to discuss x, y, z either from a departmental standpoint or a personal issue. Now two, three times a week I'm knocking on my manager's door: “You'll never believe what just happened…” And it's an open-door policy; she wants to know, she's there, she reacts to it, she supports us. Everything that we had to do back home had to go through the union, had to be funnelled through the union. Management was scared to talk to us because of what it would do, you know, were they violating the collective agreement.
What are the disincentives for returning to work in Canada?
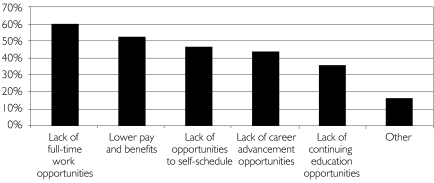
Figure 3 identifies five primary disincentives for Canadian nurses to return to Canada to work. Almost two-thirds of respondents identified the lack of full-time work opportunities, and over half indicated lower pay and benefits. Lack of opportunity to self-schedule work hours and lack of career advancement opportunities were identified by just under half the participants, while two-thirds indicated lack of continuing education opportunities as a deterrent. These five disincentives clearly stand apart from the “other” category, which included climate, specific issues in the work environment and cost of living, all of which are more commonly held beliefs about Canadian nursing workforce migration behaviours.
FIGURE 3.
Disincentives to return to work in Canada
Focus group participants expressed frustration with Canadian health human resources strategies related to the employment of nurses. Much of the discussion focused on the gap between management and staff in the Canadian healthcare environment.
Even though there's a nursing shortage … administrators are being hired; nurses are being laid off. People are scrambling because they're always working two and three people short. They don't get breaks, don't get lunches, there's not enough staffing. They have laid off part-time people and they've hired casual retired people, and so people are still being laid off and can't get hours but they're hiring retired people to come back. So I don't understand why there's such a shortage when nurses are available to work.
I think when we were in Canada it was like they were doing us a favour by giving you a job, by hiring us. It was a big deal that we got the job, but here in the United States they wanted you, I mean, it was really a sense that they really wanted you. They needed you.
In Canada everyone has to work two weekends a month. What is that about? Some people want to work weekends. You know, that whole shift idea is just obsolete here. You can do whatever you want, and that's a huge issue. People who want to work strictly weekends that have young kids and don't want to put them in daycare get to do that.
In Canada it was strictly a job because I never actually chose anywhere I could work – it was wherever anything is open, you jump in there. It doesn't matter if you like it or not, you need a paycheque, so you just work wherever.
Hospitals down here aren't prone to shutting down beds, you know, because that's their business.
Interest in returning to work in Canada
The vast majority of nurses responding to the survey who had migrated to North Carolina (72%, n=468) expressed no interest in returning to work in Canada. This finding was substantiated by participants in the focus groups.
I'm so angry with the Canadian government, I don't think I would go back from the way I was treated when I left. They didn't want me, well fine, somebody else did.
For me there [are] just no opportunities because last year about this time I looked into going back, and [for] the job offers that I did receive I would have to go back to rotating days, nights.
I feel like I've worked my way to where I am, worked very hard to have the reputation that I do and have a lot of people that I'm mentoring to blossom into other things in the department or in their professional careers. I enjoy something like that versus, let's say, going to a part-time position [in Canada].
I'm towards the end of my nursing career, so I wouldn't think about going back because I can call whenever I want to work, and if I want to work even less than that, I can.
On the other hand, close to one-quarter of respondents (23%, n=149) reported an interest in returning to work in Canada. Further analysis revealed statistically significant differences between nurses who indicated that they would be interested in returning to work in Canada and those who said they were not interested (F=13.342; df=627, 2; p=0.000). Specifically, nurses who indicated an interest in returning to Canada to work were more likely to have migrated to the United States more recently. This finding is similar to that of a study of 51 new graduate nurses from Atlantic Canada, which reported that 35.2% returned to Canada to work (Gillis et al. 2004). Nurses participating in the focus groups provided further context regarding repatriation, discussing the logistical problems as well as the political or policy issues.
Canada needs to recruit us. They need to gear their marketing towards their Canadian nurses. I get offers on my computer every day: “We'll hire you for $120,000 in southern California to do this.” Every single day I get them. I don't even open them because I know I'll just get more.
It is a nightmare, I'm telling you. Everyone says to me, “How come you didn't go back?” People don't understand; in Canada, when you leave a job you don't have a job to go back [to]. I had nothing to go back to, so I had to stay.
I would go back if I could have a full-time job and the security that I have in my job right now. I would go back very easily.
Discussion and Policy Implications
This study provides evidence of both the timing and reasons for recent Canadian nurse migration to North Carolina, but it may also provide broader explanations of why Canadian-educated nurses work in the United States, in general.
First and foremost, Canadian-educated nurses moved to the United States, and specifically to North Carolina, in search of full-time employment. Although other factors were evident in the decision to move, they were not as important as full-time employment. Given that Canadian-educated nurses, like other professionals, invest years to acquire an education and absorb some of the associated training costs, it is only reasonable to expect that they would desire to practise professionally and seek full-time employment. When these opportunities are not available to them in Canada, many nurses may have no choice other than to search for employment in the United States.
Nurses in this study reported that a number of financial incentives – including relocation assistance, higher salaries and signing bonuses – helped to recruit them from Canada. As well, opportunities for career advancement and subsidies for continuing education were important recruitment incentives. Finally, participants identified specific organizational characteristics, including flexible and innovative scheduling systems such as self-scheduling, and the reputation of the organization for good physician–nurse relationships, as important recruitment factors.
Although financial incentives are a common recruitment and retention strategy, this study also highlights the importance of a hospital administration that supports and values its nurses. This finding is evidenced by flexible schedules that accommodate nurses' needs, career advancement and continuing education opportunities, adequate staffing levels, control over practice and managers who listen to nurses' concerns. An organizational climate that fosters good relationships with medical staff and colleagueship and mentorship with peers are reasons for many of Canada's nurses to remain in the United States.
Most of the incentives to remain in the United States were also identified as disincentives to return to work in Canada. Of greatest importance was the perception that full-time work is not available. There is clearly a perception, founded or unfounded, that there may not be full-time employment available for nurses in Canada.
They think they're saving money, but what they're doing is they're devaluing a workforce and they continue to do that. How can you go back to Canada when there's no guaranteed security, even as a professional nurse?
At the same time, among a minority of respondents, specifically nurses who had migrated recently, there was some interest in returning to Canada to work. For this to occur, healthcare administrators and policy makers would need to create an environment that supports nurses' repatriation. The importance of healthcare leaders' focusing on creating healthy work environments in efforts to recruit and retain Canadian nurses has been highlighted in recent literature (Keatings 2006). A need has also been identified for policy makers in nursing to consider capacity-building mechanisms, including improvements in nursing work conditions, educational capacity, salaries, professional career development and enhanced roles in health policy and practice (Brush 2008).
Nurses must be reassured that they will have full-time employment, otherwise they will search elsewhere. Clearly, different signals need to be sent. A campaign needs to be mounted to send a strong message to Canadian nurses that they are wanted and needed in Canada's healthcare system, and that there are jobs available for them. Such an approach would require greater attention to long-term planning of human resources needs for nursing. In the past, approaches have lacked consistency and follow-through. Healthcare delivery organizations need to have some level of guarantee of ongoing funding so that their employees can be assured of predictable employment. In other words, there is a need to eliminate the boom-and-bust cycles of RN hiring and find a healthcare financing strategy that reduces the perpetual instability of RN employment cycles.
Nurse migration has been described as unchecked, uncoordinated and individualized, to the point where some countries benefit while others suffer (Brush et al. 2004). One health economist has suggested that the nursing shortages being experienced in many Western countries reflects a failure by planners to recognize the increased intensity of nursing work and the associated stress and burnout (Armstrong 2003). If this is truly the case, then there is a great opportunity to undertake the challenge of changing the work environment for nurses and to assume a more global approach to nursing workforce planning. Are there aspects of professional practice in the United States that Canada could emulate? Are there opportunities for career advancement (e.g., clinical ladders, enhanced scope-of-practice models) that should be considered? Clearly, these questions must be explored and, if certain strategies are identified and adopted, the effectiveness of these approaches must be examined.
Limitations
This study utilized a purposive sample because it allowed the researchers to survey the population of interest – Canadian-educated nurses working in North Carolina. Because the findings do not represent all Canadian nurses working in the United States, they may not be generalizable beyond the specific population studied.
Conclusion
This study provides evidence about the reasons nurses chose to leave Canada to pursue nursing careers in the United States and their interest in returning to work in Canada. Although the survey provided the “hardest” evidence, some of the most poignant findings were obtained from the focus groups. The level of dissatisfaction and occasional anger expressed by focus group participants at the way they had been treated by hospitals, physicians, managers, unions and governments in Canada were striking. Although concrete issues, such as the lack of full-time work opportunities, were the most frequent topics of discussion, they were often accompanied by anecdotes, comments and asides indicating a lack of respect and an undervaluing of their work in Canada. These stories typically included examples of how the situation in the United States differs.
The exodus of Canadian nurses to the United States is long-standing and shows little inclination to slow. There is an urgent need for healthcare policy makers to be cognizant of the career interests of these nurses and to develop more effective strategies for enhancing recruitment and retention in the nursing profession.
Acknowledgements
This research was funded by the Ontario Ministry of Health and Long-Term Care.
Contributor Information
Linda McGillis Hall, Associate Professor, Associate Dean of Research and External Relations, Lawrence S. Bloomberg Faculty of Nursing, University of Toronto, Toronto, ON.
George H. Pink, Associate Professor, Department of Health Policy and Administration; Senior Research Fellow, Cecil G. Sheps Center for Health Services Research, University of North Carolina at Chapel Hill, Chapel Hill, NC.
Cheryl Jones, Associate Professor, Department of Health Policy and Administration; Research Fellow, Cecil G. Sheps Center for Health Services Research, University of North Carolina at Chapel Hill, Chapel Hill, NC.
Peggy Leatt, Professor, Department of Health Policy and Administration; Associate Dean of Academic Affairs, School of Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC.
Michael Gates, Assistant Professor, School of Nursing, San Diego State University, San Diego, CA.
Leah Pink, Lawrence S. Bloomberg Faculty of Nursing, University of Toronto, Toronto, ON.
Jessica Peterson, Lawrence S. Bloomberg Faculty of Nursing, University of Toronto, Toronto, ON.
Lisa Seto, Lawrence S. Bloomberg Faculty of Nursing, University of Toronto, Toronto, ON.
References
- Armstrong F. Migration of Nurses: Finding a Sustainable Solution. Australian Nursing Journal. 2003;11(3):24–26. [Google Scholar]
- Brush B.L. Global Nurse Migration Today. Image: Journal of Nursing Scholarship. 2008;40(1):20–25. doi: 10.1111/j.1547-5069.2007.00201.x. [DOI] [PubMed] [Google Scholar]
- Brush B.L., Sochalski J. International Nurse Migration: Lessons from the Philippines. Policy, Politics and Nursing Practice. 2007;8(1):37–46. doi: 10.1177/1527154407301393. [DOI] [PubMed] [Google Scholar]
- Brush B.L., Sochalski J., Berger A.M. Imported Care: Recruiting Foreign Nurses to United States Health Care Facilities. Health Affairs. 2004;23(3):78–88. doi: 10.1377/hlthaff.23.3.78. [DOI] [PubMed] [Google Scholar]
- Buchan J. Nurse Migration and International Recruitment. Nursing Inquiry. 2001;8(4):203–4. doi: 10.1046/j.1440-1800.2001.00112.x. [DOI] [PubMed] [Google Scholar]
- Buchan J., Parkin T., Sochalski J. International Nurse Mobility: Trends and Policy Implications. Geneva: World Health Organization, International Council of Nurses and Royal College of Nursing; 2003. [Google Scholar]
- Commission on Graduates of Foreign Nursing Schools (CGFNS) Characteristics of Foreign Nurse Graduates in the United States Workforce 2000–2001. Philadelphia: Author; 2002. [Google Scholar]
- Elabdi M. US Still Land of Opportunity for Canadian Nurses – Recruiters Report Strong Demand for Alberta RNs. AARN News Letter. 1996;52(6):6–7. [PubMed] [Google Scholar]
- Gamble D.A. Filipino Nurse Recruitment as a Staffing Strategy. Journal of Nursing Administration. 2002;32(4):175–77. doi: 10.1097/00005110-200204000-00002. [DOI] [PubMed] [Google Scholar]
- Gillis A., Jackson W., Beiswanger D. University Nurse Graduates: Perspectives on Factors of Retention and Mobility. Canadian Journal of Nursing Leadership. 2004;17:97–110. doi: 10.12927/cjnl.2004.16246. [DOI] [PubMed] [Google Scholar]
- Health Resources and Services Administration (HRSA) What Is Behind HRSA's Projected Supply, Demand, and Shortage of Registered Nurses? 2004 Retrieved March 24, 2009. < ftp://ftp.hrsa.gov/bhpr/workforce/behindshortage.pdf>.
- Keatings M. Health Services Delivery: Reframing Policies for Global Nurse Migration in North America: A Canadian Perspective. Policy, Politics and Nursing Practice. 2006;7(3):62S–65S. doi: 10.1177/1527154406293488. [DOI] [PubMed] [Google Scholar]
- Kingma M. Nurses on the Move: Migration and the Global Health Care Economy. Ithaca, NY: Cornell University Press; 2006. [Google Scholar]
- Morse J. Approaches to Qualitative–Quantitative Methodological Triangulation. Nursing Research. 1991;40(1):120. [PubMed] [Google Scholar]
- North Carolina Center for Nursing (NCCN) Quick Facts: Use of Contract Personnel and Foreign Recruitment by Nurse Employers in North Carolina. Part of 2004 Survey of Nurse Employers. 2004 Retrieved December 28, 2006. < http://www.nccenterfornursing.org/research/empsurv2004/study%20methods.pdf>.
- Nursing Task Force. Good Nursing, Good Health: An Investment for the 21st Century. Toronto: Ontario Ministry of Health and Long-Term Care; 1999. [Google Scholar]