Abstract
Objective
To assess whether equipping resident pediatricians and community pediatricians with both training and practical tools improves their perceived confidence, ease, and frequency of obesity-related counseling to patients.
Methods
In 2005-2006, resident pediatricians (n = 49) and community pediatricians (n=18) received training regarding three evidence-based obesity prevention/treatment tools and responded to pre-and post-intervention questionnaires. We analyzed changes in reported mean confidence, ease, and frequency of dietary, physical activity, and weight status counseling.
Results
Baseline scores of confidence, ease, and frequency of counseling were higher in community pediatricians than residents. Mean scores increased significantly in the combined group, among residents only, and trended towards improvement in the community pediatricians following the intervention. Means for “control” questions were unchanged.
Conclusion
Training and tools for residents and community pediatricians improved their confidence, ease, and frequency of obesity-related counseling.
Practice Implications
This study demonstrates that when feasible and appropriate tools and training were provided through a simple intervention, physicians gained confidence and ease and increased their counseling frequency. The results here suggest that widespread implementation of such educational interventions for community practitioners and practitioners in training could change the way physicians counsel patients to prevent the often frustrating problem of childhood obesity.
Keywords: Childhood overweight, Counseling, Residency, Nutrition, Physical activity
1. Introduction
The epidemic of childhood overweight and its current and forecasted medical, social, and economic toll has resulted in national recommendations that primary care physicians institute measures to prevent and treat obesity [1, 2]. As we await development and testing of effective and practical interventions, the Committee on Nutrition of the American Academy of Pediatrics (AAP) and other experts advise physicians to encourage families to adopt behaviors that promote healthy weight by increasing physical activity, limiting television viewing, and promoting healthy eating patterns, such as limiting sugar-sweetened drinks [2-4]. The 2001 Surgeon General's report [1], the Institute of Medicine (IOM) [5], and the AAP Committee on Nutrition [2] have also called for regular Body Mass Index (BMI) screening in children over 2 years of age.
Despite this call to action and that pediatricians generally believe childhood overweight needs treatment and is unlikely to be outgrown [6], only 50% of pediatricians routinely counsel to maintain a healthy weight [7]. Pediatricians may feel ill-equipped to deal with this challenge. Three recent surveys found pediatricians report low confidence in their obesity-related counseling skills [6, 8, 9]. This may be the combination of the difficulties in treating and preventing obesity relative to other common problems as well as the incredible burgeoning of recommendations for anticipatory guidance presented to pediatricians [9, 10]. Social cognitive theory suggests that improvements in self-efficacy (or the belief in one's capabilities which many studies, like ours, interchange with the concept of confidence [11-13]) may result in increased counseling by physicians. For purposes of this article, the terms “self efficacy” and “confidence” will be used interchangeably. Self-efficacy is associated with the extent of physicians' counseling about a variety of lifestyle-related topics, including physical activity [14], smoking [12, 15], and growth and nutrition in general [13]. While awareness of recommendations [8], training [16], and experience [17] improve self-efficacy, more seasoned pediatricians may actually have “inertia of prior practice” as a result of experiences with failure may actually have lower levels of self-efficacy [17] and may be less likely to follow appropriate standards of care and may be in greater need of quality improvement interventions [18].
Because of the desire to improve training and experience while at the same time overcome clinical inertia [19], we targeted pediatricians in training and in established community settings with an intervention to improve self-efficacy in obesity management and counseling. Training in counseling has improved confidence, knowledge, and counseling skills for pediatric resident physicians (RPs) in areas as diverse as smoking cessation [20] and breastfeeding counseling knowledge and behaviors [21]. However, there are few studies on training in counseling skills for obesity prevention such as dietary or physical activity counseling for residents [22] or community pediatricians (CPs) [23].
This intervention intended to teach RPs and CPs to: 1) detect unhealthy weight trajectories; 2) sensitively communicate weight status to parent and child; 3) provide all families with evidence-based, brief, targeted counseling to improve diet and activity; 4) follow-up at risk and overweight children to reinforce counseling; and, thus, provide tools and experience to, 5) improve physician confidence, ease, and frequency of counseling about these issues.
This intervention was designed to meet the needs of both RPs and CPs and to improve patient-physician communication. The intervention is compatible with pediatric residency educational goals because residency programs are now being asked to prepare pediatricians to integrate technical skills into practice and become competent in information management [24]. Further, the Accreditation Council for Graduate Medical Education (ACGME) recommends that residents “[p]rovide child health supervision with an emphasis on age and developmentally appropriate anticipatory guidance and screening [and] provide anticipatory guidance regarding …preventive health care.” [25] Recent interviews with pediatric residency program directors found that obesity prevention and management training is often lacking and that numerous barriers exist to develop curriculum in these areas [26], so we designed the intervention to meet that need. In addition, we designed the training to meet needs identified by practitioners in two prior survey studies, including content and tools identified previously as lacking, such as better counseling tools to guide patients toward lifestyle modification and better tools to communicate weight problems to patients [6, 9]. We hypothesized that equipping pediatricians with training and counseling tools would improve their perceived confidence, ease, and frequency of counseling about healthy weight, nutrition, and physical activity.
2. Methods
2.1 Study design and participants
A pre-test / post-test study was conducted between April 2005 and July 2006 at the University of North Carolina at Chapel Hill Pediatrics Continuity Clinic and between April 2005 and January 2006 in four rural community practice sites that are all part of AccessCare, Inc., a network of approximately 300 primary care practices that seek to provide coordinated, high quality medical services to those insured by Medicaid and the uninsured in the state of North Carolina (NC). All RPs or CPs who staffed the sites during the study period were eligible to participate. To be included in the study, physician participants had to consent to participate, be trained in the use of the intervention tools, complete physician data collection instruments, which had undergone pilot testing in our formative phase, and implement the patient/parent-focused intervention in their clinic using what we called the “Promoting Healthy Weight” tools [27]. RPs were excluded from participation if they were to complete their residency during the summer of 2005 or if in the Medicine-Pediatrics combined residency program because this latter group rotated to different primary care sites during the intervention. This study was approved by the University of North Carolina at Chapel Hill School of Medicine Institutional Review Board (Childhood Obesity Prevention Instrument Development, IRB # 04-1574, formerly 04-HPDP-771).
2.2 Residency setting recruitment and training
Investigators sent email invitations to eligible RPs asking them to attend a “Promoting Healthy Weight” noon conference training session. The one-hour physician training session, initially held in April 2005, included a review of childhood overweight, as well as instruction on how to improve physician-parent communication using the “Promoting Healthy Weight” tools, including “Starting the Conversation (STC),” parental assessment of readiness to change, and the BMI color-coded charts [27]. As part of this training session, physicians were taught how to interpret BMI in children, use the color-coded BMI charts to facilitate communication of weight status with parents, and how to counsel about healthy eating and activity patterns by scanning the parent's responses to questions on STC form, reinforce areas where child is doing well, identify areas needing improvement, ask the parent and child to identify 2-3 areas needing improvement that they are willing to work on before next visit, and review specific tips offered for each area needing change on the STC form. The physicians were taught to use a collaborative, non-confrontational approach using specific communication techniques that drew from theories such as the Transtheoretical Model [28] and Motivational Interviewing [29]. They were given sample scripts (that they were able to tailor) of how to communicate sensitively about body mass indices, how to use the “Starting the Conversation” questionnaires both in video clip and in written sample cases vignettes, and how to assess and advance readiness to change.
2.3 Community settings recruitment and training
A convenience sample of four rural community practices was identified to test the intervention in a variety of geographic, patient population, and practice infrastructure (such as electronic medical records systems) environments. Once each practice agreed to participate, a one-hour lunchtime training was arranged at a date convenient for the practice, and a co-investigator and study team member conducted consent procedures, the Physician Survey described above, and the training. All relevant clinic staff members such as nurses, case managers, and all available physicians were encouraged to attend the training to facilitate intervention implementation, but only physicians were enrolled in the study. Trainings were held at the four sites between April and September 2005. At two clinics not all physicians attended the training, and the primary contact physician at each site made the slides, handouts, and videos demonstrating use of the counseling tools available for review by the absent physician with the lead physician available for questions as needed.
2.4 Intervention tools
Following training and enrollment, physicians began using the “Promoting Healthy Weight” tools to counsel parents and patients insured by Medicaid during well-child checks and visits to clinic for minor illness. These tools are described elsewhere [27] but comprise color-coded BMI charts and STC assessment and counseling tools. The BMI color-coded charts are used to plot the child's BMI (for children at least 2 years of age) according to a stop light motif (red, yellow, and green) based on the child's level of risk for overweight. This tool is based on the Centers for Disease Control (CDC) recommended chart [30], enhanced by our group with color-coding to facilitate risk identification by the pediatrician and communication of BMI status with parents. The STCs are rapid assessment tools and tailored counseling guides designed by our group for use by primary care physicians and completed by parents in either the waiting or exam rooms. Assessment questions are derived from evidence-based determinants of obesity in children such as lack of outdoor play, screen time, and consumption of sugar-sweetened beverages. Physicians use these tools to identify nutrition and physical activity behaviors and barriers that may put the child at risk for overweight. One section of the STC measures parental readiness to change to help the physicians tailor their counseling approach. Copies of the STC and BMI chart are included in the medical record so that the physician can monitor patient behavior changes from one visit to another. The STC tools are age-specific: 2 years to less than 4 years of age and 4 to 12 years of age. The RPs completed the intervention over nine months. CPs had originally been asked to pilot the tools in their practices for three months, but the actual duration varied at each community site from two to four months. The resident intervention was longer because the resident physicians are in clinic fewer hours per week and therefore needed a longer period of time to gain experience using the tools.
2.5 Study Measures
Prior to the one-hour training, RPs were recruited and asked to complete informed consent and physician questionnaires that included basic demographic information such as physician birth year, gender, degrees completed, year in residency program, ethnicity and race. They also answered questions with 4-point Likert response options regarding their perceived confidence, ease, and frequency of counseling in the areas of nutrition, physical activity, patient weight status, and “control” counseling behaviors not expected to change as a result of the intervention. A four-point response option was chosen because research suggests that such an option offers adequate reliability with the simplicity respondents prefer [31-33].
The seven questions about confidence in one's abilities were adapted from a prior survey whose results were previously published [9]. Based on the fact that detailed and reliable pre-post intervention questions were necessary here, a new questionnaire was created for this study and pilot tested. The final questionnaire demonstrated clarity, reliability, and usability.
At the completion of the intervention, participants were asked to complete a follow-up physician questionnaire. For both groups this questionnaire repeated questions measuring perceived confidence, ease and frequency of counseling, and for the RP group an additional 4 questions were asked to solicit feedback on the main study instruments. Both the helpfulness (from 1=not helpful to 4 = very helpful) of the BMI color-coded charts to interpret body mass index and of the STC in terms of counseling about diet and activity and the effect on time spent during well-child checks for each of these instruments (STCs and BMI color-coded charts) were queried.
2.6 Data Management and Analysis
Teleform™ (Verity) software was used to facilitate three aspects of data management: collection, entry, and export. TELEform software was used to create optically scanned data collection instruments which go through a verification process before data are written to Structured Query Language data tables. This approach eliminates the need for double data entry and greatly reduces data editing tasks since range checks are built into all choice option fields and data verification is done on-screen. In addition to a high accuracy rate, this method of data entry can make data available for analysis virtually in real time, allowing for early and frequent consistency checks. Electronic copies (“tiff” images) are archived of all scanned data and serves as a back-up of the paper files. After data were verified, Teleform® automatically exported data to a database in a specified format to be easily converted to SAS for further data editing, coding, and analysis. The Data Capture Services Unit of the UNC Center for Health Promotion and Disease Prevention oversaw data entry for this study.
2.7 Statistical Analysis
Changes between pre-intervention and post-intervention scores were computed for each physician respondent for each of the questions using a 4-point Likert scale. Pre-post mean score changes were tested using the Signed Rank Test because this non-parametric analogue to the paired t-test allows for analysis when data are ordinal rather than continuous and the distribution of differences between pairs is non-normally distributed. Comparisons were made pre- and post-intervention for the RP and CP groups individually and for both intervention groups combined. To determine whether there was a shift in scores to the highest level of confidence, ease, and frequency, pre-post comparisons were made between those physicians responding with scores = 4 in each of these domains represented by 7 separate questions versus all other responses (scores of 1-3) using the McNemar's test, a non-parametric test for dichotomous data. The data were analyzed again using categorical responses but with similar results, so dichotomized results are presented here for simplicity and ease of understanding. These analyses were performed to determine whether physician confidence, ease, and frequency of counseling improved to the highest levels after the training and experience working with the tools. Questions about frequency in discussing topics such as school behavior problems, school issues, and sleep issues, as well as BMI calculation (done at the resident site automatically by the computer system and not a learning objective of this intervention) were not expected to change, and were used as “control” questions so that we could examine whether reported attitude/behavior changes were specific to the intervention.
3. Results
3.1 Study sample, resident physician characteristics, patient characteristics, and number of encounters
Of 52 potentially eligible pediatric resident physicians, 49 (94%) enrolled in the study, participated in patient enrollment and/or follow-up, and completed the post-test survey. Of 27 potential community physicians, 20 chose to participate and complete this optional intervention, and 18 (90%) completed surveys from the four sites (4 providers at each of three sites and 6 providers at the fourth). Forty-nine RPs and 18 CPs enrolled in the study and completed all components (N=67). Approximately 80% of the RPs were female, and 88% were white (Table 1). The residents used the tools with an average of 5 patients each. Their patients were diverse: 49% female, 8% Hispanic, 66% African American, 21% white. While CPs completed surveys on confidence, difficulty, and frequency of counseling, we did not collect their demographic information in order to not over-generalize from a small number of providers, minimize respondent burden, and maintain anonymity given the small numbers of providers at each practice. Their patients' information was also not collected in order to minimize human subjects' consents at a busy community practice. The community physicians used the tools with an average of 23 patients each.
Table 1. Characteristics of RPs (n=49).
| Characteristic | Frequency |
|---|---|
| Age in Years | |
| 26 – 27 | 7 (14.3%) |
| 28 – 29 | 23 (46.9%) |
| 30 – 31 | 17 (34.7%) |
| 32 – 34 | 2 (4.1%) |
| Female | 39 (79.6%) |
| Year in Residency | |
| 1st | 28 (57.1%) |
| 2nd | 14 (28.6%) |
| 3rd | 7 (14.3%) |
| Educational Background (MD +) | |
| Masters in Public Health (MPH) | 4 (8.2%) |
| Masters of Science in Public Health (MSPH) | 1 (2.0%) |
| Pharm D | 1 (2.0%) |
| Ethnicity | |
| Not Hispanic/Latino | 49 (100%) |
| Race | |
| Asian | 4 (8.2%) |
| Black or African American | 2 (4.1%) |
| White | 43 (87.8%) |
3.2 Psychometric validity of measures
The Cronbach's alpha for the confidence questions was 0.86 providing high internal consistency reliability. The Cronbach's alpha for the difficulty questions was also 0.86.
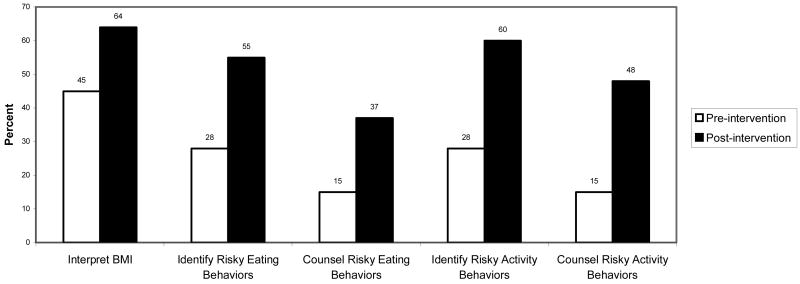
3.3 Physicians' confidence
Pre-intervention CPs' self-reported confidence in their ability to assess and counsel parents and children on all measures was significantly higher than for RPs. Post-intervention, rating improved significantly in all intervention areas for all participants combined and for the RPs group alone and trended towards improvement for the CPs. Post-intervention, there was no longer a significant difference between the RPs' and CPs' confidence. Mean scores of confidence in all intervention (“non-control”) areas assessed increased following the intervention: interpreting BMI, identifying eating behaviors, counseling about eating behaviors, identifying physical activity behaviors, and counseling about physical activity behaviors (p<0.003 for all pre-post-comparisons for the combined and RP groups) (Table 2). Significant increases also occurred in the proportion of physicians reporting the highest level of confidence, ease, and frequency with the greatest improvement in perceived physician confidence for the ability to counsel about physical activity behaviors that increase children's risk for overweight (from 15% to 49%, p<0.0003; Figure 1). Confidence about calculating BMI was not expected to change for residents because their clinic's computer system calculates BMI and, calculation of BMI was not a learning objective of our intervention. Thus, the fact that it did not change demonstrates the specificity of the intervention.
Table 2. Reported Confidence, Ease, and Frequency of Counseling.
| Resident Pediatricians (n=49) | Community Pediatricians (n=18) | All Participants Combined (N=67) | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Post | Baseline | Post | Baseline | Post | p-value | ||
| Confidence in… | Interpreting BMI | 3.2 | 3.6 | 3.7 | 3.7 | 3.2 | 3.6 | 0.003 |
| Identifying risky eating behaviors | 3.1 | 3.5 | 3.4 | 3.6 | 3.1 | 3.5 | 0.002 | |
| Counseling about risky eating behaviors | 2.7 | 3.2 | 3.2 | 3.4 | 2.7 | 3.2 | <0.0001 | |
| Identifying risky physical activity behaviors | 3.1 | 3.5 | 3.4 | 3.7 | 3.1 | 3.5 | 0.002 | |
| Counseling about risky physical activity behaviors | 2.8 | 3.2 | 3.3 | 3.6 | 2.8 | 3.3 | <0.0001 | |
| Ease in counseling about… | Healthy eating | 2.8 | 3.2 | 2.9 | 3.4 | 2.8 | 3.2 | 0.002 |
| Physical activity | 2.7 | 3.2 | 2.9 | 3.4 | 2.8 | 3.2 | 0.004 | |
| Healthy weight | 2.7 | 3.2 | 2.8 | 3.4 | 2.7 | 3.2 | <0.001 | |
| Frequency of discussing… | Dietary habits | 3.2 | 3.5 | 3.6 | 3.6 | 3.2 | 3.6 | 0.007 |
| Physical activity | 3.0 | 3.4 | 3.4 | 3.5 | 3.0 | 3.3 | 0.01 | |
Means are based on a 4-point scale, with 1 = not at all confident to 4 = very confident.
Figure 1.
% of Participating Physicians (N=67) Reporting They Are “Very Confident” Performing These Behaviors at Well-Child Visits of 4-12 Year-olds. Physicians more frequently reported the highest level of confidence in all measured areas post intervention than they did pre-intervention.
*Significant, p<0.005 by McNemar's Test, comparing the proportion of “very confident” responses to all other responses.
† Significant, p<0.02 by McNemar's Test, comparing the proportion of “very confident” responses to all other responses
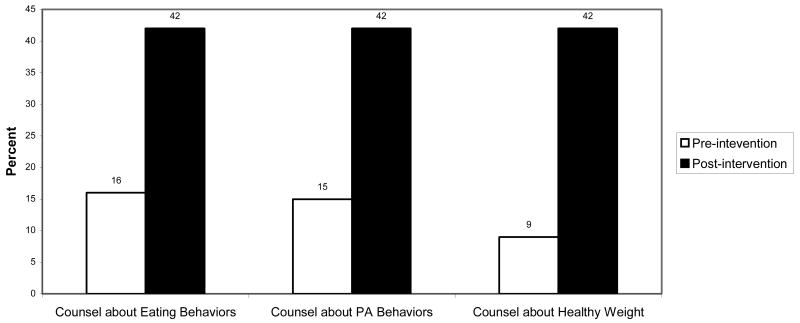
3.4 Physicians' ease in counseling about healthy weight behaviors
Prior to implementing the intervention, most participants, including the CPs, reported some degree of difficulty with counseling about healthy eating, physical activity, and healthy weight. Post-intervention reported ease of counseling increased significantly for each area of counseling for the combined group and the RPs. The proportion of physicians indicating that counseling on these topics is “not difficult at all” ranged from as low as 9% to 16% at baseline. Post-intervention measurements demonstrated significant improvements to 42% (p<0.005 for all pre- post- comparisons; Figure 2).
Figure 2.
% Participating Physicians (N=67) Reporting “Not at All Difficult” To Do During Well-Child Visits of 4-12 Year-Olds. Following the intervention, a much higher percentage of physicians reported lack of difficulty in counseling about healthy eating, physical activity, and healthy weight during school age primary care visits.
*Significant, p<0.005 by McNemar's Test, comparing the proportion of “not at all difficult” responses to all other responses.
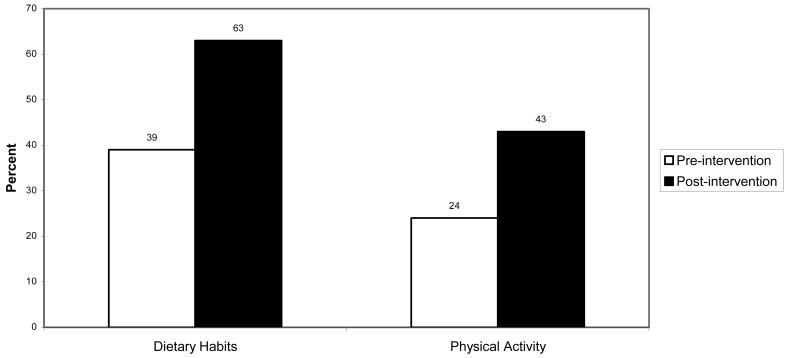
3.5 Frequency in discussing weight-related and other topics with families
Physician surveys asked participants to estimate the frequency with which they discussed diet, physical activity, and topics unrelated to the intervention (for control questions) during well child checks of 4 to 12 year old children. The proportion of physicians who reported “always” discussing diet increased from 39% to 63%, p = 0.0094. Self-assessed frequency of “always” discussing physical activity during routine counseling increased from 24% to 43%, p = 0.01, Figure 3. Pre-post intervention changes for residents in discussing two control topics (behavior problems and sleep issues) did not increase significantly.
Figure 3.
% Participating Physicians (N=67) Reporting “Always Discussing” During Well-Child Visits of 4-12 Year-Olds. Following the intervention a much higher percentage of physicians reported that they always discussed dietary habits and physical activity habits during well child visits with school-age children.
*Significant, p<0.02 by McNemar's Test, comparing the proportion of “always” responses to all other responses.
3.6 Resident physician assessment of intervention tools
The feedback provided by resident physicians on the utility of the STC and colored BMI graph was favorable. The colored BMI graph was reported to be helpful or very helpful in interpreting BMI by 98% of participating residents. Most RPs (73.4%) believed the colored BMI graph decreased or did not change the amount of time spent during well-child checks. The STC tools were considered helpful or very helpful in counseling about diet and activity by 88% of RPs. However, more than half (59%) of RPs indicated that the STC increased the amount of time spent during well child visits.
4. Discussion and Conclusion
4.1 Discussion
4.1.1. Summary of main findings
Following our intervention to equip them with practical, office-based tools, the pediatric residents and practicing pediatricians in our study reported increased confidence, ease, and frequency of counseling with respect to healthy eating, activity, and weight status. Because their confidence did not increase significantly in areas not targeted (control questions), the intervention was specific to the targeted topics. Specifically for residents still in training, the intervention appeared to provide an additive component to their natural development as learners and equip them to enter practice more confident of their abilities to counsel about nutrition and physical behavior. For the community pediatricians, even though their baseline self-assessment showed relatively high confidence, they still showed improvement for all areas, and demonstrated significant improvement in perceived ease of counseling in these important areas. Post-intervention, there was no longer a significant difference between the resident and experienced physicians, suggesting that the “Promoting Healthy Weight” tools helped bridge the skills gap to practice. While one recent study found that second-year residents who participated in an “Obesity Prevention in Pediatrics” curriculum improved their knowledge and comfort level [22], our study is the first to show that at least short-term confidence can increase for both residents and practitioners using the same practical office-based tools.
4.1.2. Limitations
This study has some limitations that need to be considered. The lack of a control group calls into question the results, though the results of control questions help demonstrate the specificity of the intervention. Also, the number of encounters and the duration of the intervention varied between types of sites (resident versus community physician) as well as varying from community physician to community physician site. We sustained the intervention with residents longer (9 months versus 2-4 months) to partially account for their limited time each week with primary care patients. Thus we are not able to make conclusions about differential exposure times or number of encounters needed to effect change. In addition, this study involved trainees at just one practice and a small convenience sample of community pediatricians motivated to improve their practice regarding childhood overweight, calling generalizability into question. Because physicians were aware they were being asked about behaviors they knew were expected of them, responses could reflect some social desirability bias, but one would expect that both pre-and post-intervention responses would be equally affected in this regard. Because participants were not “blinded” to the subject under investigation, the magnitude of the pre-post changes might be inflated, though one would expect that one of our “control” questions regarding calculation of BMI (which was not a learning objective of the teaching intervention but did concern the same topic) would have been similarly affected. Though highly internally reliable, we have no standardized validity measures for the physician survey other than face validity. Also the increased time that resident physicians stated was spent on the STC tool suggests the need for continued work to refine our intervention tools for efficiency. While the intervention did appear to influence change on many measures, a large percentage of residents still did not achieve the highest levels of confidence, ease, or frequency post-intervention. The significant pre-post changes in confidence may be seen as minor, and statistical significance may not translate into clinical significance. However, we used an outcome of highest levels of confidence, ease, and frequency because we believe it is at these superlatives when any barriers are effectively eliminated and social cognitive theory would predict that the extent of counseling would increase. Also, given the fact that the problem of childhood obesity is so prevalent and counseling's efficacy is so unpredictable, “universal” (or highest frequency) compliance with recommendations is very important. Of course, in this study, as in so many, we do not know whether increased counseling frequency leads to improved self-efficacy or vice-versa. Still, the cycle is one that will likely benefit patient care regardless of which comes first. Finally, we only can assess short-term confidence change and cannot address the sustainability of such changes or their effects from this study. Patient-specific outcomes were measured by our investigation at the resident site, and we plan to report these separately.
4. 2 Conclusion
While the limitations of this study need to be considered, the results suggest some important conclusions: training and tools for residents and community pediatricians improved their confidence, ease, and frequency of obesity-related counseling. There are at least two promising reasons to design and test obesity management interventions like this one in resident and practicing physicians. First, today's physicians are confronted with the need to enhance their counseling skills to combat a variety of psychosocial problems that define the new morbidities [34], and this has become an increased focus of pediatric residency training. Obesity is the epitome of a multi-factorial, chronic illness requiring improved counseling. Second, educating and equipping emerging physicians avoids the “inertia of prior practice” phenomenon that may plague physicians further along in their career [17]. Since counseling behaviors also increased for our community physician group, combining training with practice tools may also stimulate behavior change in experienced physicians. Our study demonstrates that both groups of learners may benefit from the same intervention, and we hope future research of our group and others will allow this study to be one step in the ultimate goal of patient behavioral change and healthy outcomes.
4.3 Practice implications
Incorporating evidence-based intervention for childhood obesity in primary care has been difficult due to lack of physician self-efficacy and simple practice tools. Increasing confidence in and ease of counseling with feasible tools will enhance likelihood that such counseling can be routinely incorporated into practice. Through a simple intervention, this study demonstrates that when appropriate tools and training are provided, practice habits can change for the frequent and often frustrating problem of childhood obesity. While further research is needed to determine whether improved self-efficacy in this arena translates into improved care and clinically relevant outcomes, social cognitive theory combined with these results suggests that efforts to improve the self-efficacy of practicing and future pediatricians via brief training and tools to facilitate their practice may prove critically important in combating the childhood obesity epidemic. Interventions like this one which simultaneously and using the same strategies boost the confidence of experienced practitioners and emerging doctors will help the greatest number of patients receive recommended counseling and improve doctor-patient communication on important health topics.
Acknowledgments
This project was supported by Dr. Perrin's NIH K23 career development award (1K23 HD051817-01A1) and Dr. Ammerman's R01 (5 R01 HD050981-02). The authors would like to thank Gina Chung, Dr. Lisa Pullen-Davis, and especially Dr. Karah Daniels and Joanne Propst Finkle for their research help and support throughout the project. We would also like to thank Dr. Michael Steiner and Dr. Andrew Perrin for their careful reading of the paper in draft form and Dr. Ziya Gizlice and Dr. Asheley Skinner for help with statistical analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Eliana M. Perrin, Assistant Professor, Department of Pediatrics, UNC at Chapel Hill
Julie C. Jacobson Vann, Clinical Assistant Professor, School of Nursing, UNC at Chapel Hill
Suzanne Lazorick, Assistant Professor, Department of Pediatrics, Brody School of Medicine, East Carolina University.
Alice Ammerman, Director, Center for Health Promotion and Disease Prevention and Professor, Department of Nutrition, UNC at Chapel Hill.
Sari Teplin, Consultant to the North Carolina Foundation for Advanced Health Programs, Inc
Kori Flower, Charles Drew Community Health Center, Piedmont Health Services.
Steven E. Wegner, Community Care of North Carolina, and Adjunct Assistant Professor, Department of Pediatrics, UNC Chapel Hill
John T. Benjamin, Professor, Department of Pediatrics, UNC at Chapel Hill
References
- 1.U.S. Department of Health and Human Services. The Surgeon General's Call to Action to Prevent and Decrease Overweight and Obesity. Rockville MD: Office of the Surgeon General; 2001. [PubMed] [Google Scholar]
- 2.American Academy of Pediatrics. Committee on Nutrition. Policy Statement: Prevention of Pediatric Overweight and Obesity. Pediatrics. 2003;112:424–30. doi: 10.1542/peds.112.2.424. [DOI] [PubMed] [Google Scholar]
- 3.Whitaker RC. Obesity prevention in pediatric primary care: four behaviors to target. Arch Pediatr Adolesc Med. 2003;157:725–7. doi: 10.1001/archpedi.157.8.725. [DOI] [PubMed] [Google Scholar]
- 4.Dietz WH, Robinson TN. Clinical practice. Overweight children and adolescents. N Engl J Med. 2005;352:2100–9. doi: 10.1056/NEJMcp043052. [DOI] [PubMed] [Google Scholar]
- 5.Institute of Medicine. Committee on Prevention of Obesity in Children and Youth Preventing Childhood Obesity: Health in the Balance. Washington, D.C.: National Academies Press; 2004. [Google Scholar]
- 6.Story MT, Neumark-Stzainer DR, Sherwood NE, et al. Management of child and adolescent obesity: attitudes, barriers, skills, and training needs among health care professionals. Pediatrics. 2002;110:210–4. [PubMed] [Google Scholar]
- 7.Rattay KT, Fulton JE, Galuska DA. Weight counseling patterns of U. S. Pediatricians Obes Res. 2004;12:161–9. doi: 10.1038/oby.2004.21. [DOI] [PubMed] [Google Scholar]
- 8.Kolagotla L, Adams W. Ambulatory management of childhood obesity. Obes Res. 2004;12:275–83. doi: 10.1038/oby.2004.35. [DOI] [PubMed] [Google Scholar]
- 9.Perrin EM, Flower KB, Garrett J, Ammerman AS. Preventing and treating obesity: pediatricians' self-efficacy, barriers, resources, and advocacy. Ambul Pediatr. 2005;5:150–6. doi: 10.1367/A04-104R.1. [DOI] [PubMed] [Google Scholar]
- 10.Belamarich PF, Gandica R, Stein RE, Racine AD. Drowning in a sea of advice: pediatricians and American Academy of Pediatrics policy statements. Pediatrics. 2006;118:e964–78. doi: 10.1542/peds.2006-0652. [DOI] [PubMed] [Google Scholar]
- 11.Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 12.Cabana MD, Rand C, Slish K, Nan B, Davis MM, Clark N. Pediatrician self-efficacy for counseling parents of asthmatic children to quit smoking. Pediatrics. 2004;113:78–81. doi: 10.1542/peds.113.1.78. [DOI] [PubMed] [Google Scholar]
- 13.Cheng TL, DeWitt TG, Savageau JA, O'Connor KG. Determinants of counseling in primary care pediatric practice: physician attitudes about time, money, and health issues. Arch Pediatr Adolesc Med. 1999;153:629–35. doi: 10.1001/archpedi.153.6.629. [DOI] [PubMed] [Google Scholar]
- 14.Eckstrom E, Hickam DH, Lessler DS, Buchner DM. Changing physician practice of physical activity counseling. J Gen Intern Med. 1999;14:376–8. doi: 10.1046/j.1525-1497.1999.00356.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kviz FJ, Clark MA, Slezak JA, Davis AM. Providers' smoking cessation attitudes and practices for older patients. Behav Med. 1999;25:53–61. doi: 10.1080/08964289909595737. [DOI] [PubMed] [Google Scholar]
- 16.Cabana MD, Rand CS, Becher OJ, Rubin HR. Reasons for pediatrician non-adherence to asthma guidelines. Arch Pediatr Adolesc Med. 2001;155:1057–62. doi: 10.1001/archpedi.155.9.1057. [DOI] [PubMed] [Google Scholar]
- 17.Cabana MD, Ebel BE, Cooper-Patrick L, Powe NR, Rubin HR, Rand CS. Barriers pediatricians face when using asthma practice guidelines. Arch Pediatr Adolesc Med. 2000;154:685–93. doi: 10.1001/archpedi.154.7.685. [DOI] [PubMed] [Google Scholar]
- 18.Choudhry NK, Fletcher RH, Soumerai SB. Systematic review: the relationship between clinical experience and quality of health care. Ann Intern Med. 2005;142:260–73. doi: 10.7326/0003-4819-142-4-200502150-00008. [DOI] [PubMed] [Google Scholar]
- 19.Phillips LS, Branch WT, Cook CB, et al. Clinical inertia. Ann Intern Med. 2001;135:825–34. doi: 10.7326/0003-4819-135-9-200111060-00012. [DOI] [PubMed] [Google Scholar]
- 20.Lee MT, Hishinuma ES, Derauf C, Guerrero AP, Iwaishi LK, Kasuya RT. Smoking cessation counseling training for pediatric residents in the continuity clinic setting. Ambul Pediatr. 2004;4:289–94. doi: 10.1367/A03-180.1. [DOI] [PubMed] [Google Scholar]
- 21.Hillenbrand KM, Larsen PG. Effect of an educational intervention about breastfeeding on the knowledge, confidence, and behaviors of pediatric resident physicians. Pediatrics. 2002;110:e59. doi: 10.1542/peds.110.5.e59. [DOI] [PubMed] [Google Scholar]
- 22.Gonzalez JL, Gilmer L. Obesity prevention in pediatrics: A pilot pediatric resident curriculum intervention on nutrition and obesity education and counseling. J Nat'l Med Assoc. 2006;98:1483–8. [PMC free article] [PubMed] [Google Scholar]
- 23.Patrick K, Sallis JF, Prochaska JJ, et al. A multicomponent program for nutrition and physical activity change in primary care: PACE+ for adolescents. Arch Pediatr Adolesc Med. 2001;155:940–6. doi: 10.1001/archpedi.155.8.940. [DOI] [PubMed] [Google Scholar]
- 24.Epstein RM, Hundert EM. Defining and assessing professional competence. J Amer Med Assoc. 2002;287:226–35. doi: 10.1001/jama.287.2.226. [DOI] [PubMed] [Google Scholar]
- 25.Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Pediatrics. [June 6, 2008]; July 1, 2007. Available at: http://www.acgme.org/acWebsite/downloads/RRC_progReq/320pediatrics07012007.pdf.
- 26.Goff SL, Holmboe ES, Curry L. Barriers to obesity training for pediatric residents: a qualitative exploration of residency director perspectives. Teach Learn Med. 2006;18:348–55. doi: 10.1207/s15328015tlm1804_13. [DOI] [PubMed] [Google Scholar]
- 27.Perrin EM, Finkle JP, Benjamin JT. Obesity prevention and the primary care pediatrician's office. Curr Opin Pediatr. 2007;19:354–61. doi: 10.1097/MOP.0b013e328151c3e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 29.Miller WR, Rollnick S. Motivational Interviewing: Preparing People to Change. New York: Guilford Press; 2002. [Google Scholar]
- 30.National Center for Health Statistics and National Center for Chronic Disease Prevention and Health Promotion. Clinical Growth Charts. [June 6, 2008]; October 16, 2000. Available at: www.cdc.gov/nchs/about/major/nhanes/growthcharts/clinical_charts.htm.
- 31.Masters J. The relationship between number of response categories and reliability of Likert-type questionnaires. Journal of Educational Management. 1974;11:49–53. [Google Scholar]
- 32.Alwin DF, Krosnick JA. The reliability of survey attitude measurement: The influence of question and respondent attributes. Sociological Methods and Research August. 1991;20:139–81. [Google Scholar]
- 33.McDonald JL. The optimal number of categories for numerical rating scales (Doctoral dissertation, University of Denver) Dissertation Abstracts International. 2004;65:1664. [Google Scholar]
- 34.Committee on Psychosocial Aspects of Child and Family Health. American Academy of Pediatrics. The new morbidity revisited: a renewed commitment to the psychosocial aspects of pediatric care. Pediatrics. 2001;108:1227–30. doi: 10.1542/peds.108.5.1227. [DOI] [PubMed] [Google Scholar]