Abstract
Objective:
This study tested the effectiveness of brief primary care provider interventions delivered in a college student health center to a sample of college students who screened positive for high-risk drinking.
Method:
Between November 2005 and August 2006, 8,753 students who presented as new patients to the health service at a large public university were screened for high-risk drinking, and 2,484 students (28%) screened positive on the 5/4 gender-specific high-risk drinking question (i.e., five or more drinks per occasion for men and four or more for women). Students who screened positive for high-risk drinking and consented to participate (N = 363; 52% female) were randomly assigned either to a control group (n = 182) or to an experimental group (n = 181). Participants in the experimental group received two brief intervention sessions that were founded in motivational interviewing techniques and delivered by four specially trained providers within the student health center. Data on alcohol use and related harms were obtained from a Web-based Healthy Lifestyle Questionnaire, 30-day Timeline Followback alcohol-use diaries, the Rutgers Alcohol Problem Index (RAPI), and eight items from the Drinker Inventory of Consequences-2L.
Results:
Repeated measures analysis showed that, compared with the control group (C), the intervention group (I) had significant reductions in typical estimated blood alcohol concentration (BAC) (C = .071 vs I = .057 at 3 months; C = .073 vs I = .057 at 6 months), peak BAC (C = .142 vs I = .112 at 3 months; C = .145 vs I = .108 at 6 months), peak number of drinks per sitting (C = 8.03 vs I = 6.87 at 3 months; C = 7.98 vs I = 6.52 at 6 months), average number of drinks per week (C = 9.47 vs I = 7.33 at 3 months; C = 8.90 vs I = 6.16 at 6 months), number of drunk episodes in a typical week (C = 1.24 vs I = 0.85 at 3 months; C = 1.10 vs I = 0.71 at 6 months), number of times taken foolish risks (C = 2.24 vs I = 1.12 at 3 months), and RAPI sum scores (C = 6.55 vs I = 4.96 at 6 months; C = 6.17 vs I = 4.58 at 9 months).
Conclusions:
Brief interventions delivered by primary care providers in a student health center to high-risk-drinking students may result in significantly decreased alcohol consumption, high-risk drinking, and alcohol-related harms.
Alcohol misuse among college students is prevalent and is associated with substantial harms (Task Force of the National Advisory Council on Alcohol Abuse and Alcoholism, 2002). Four out of five college students drink alcohol (Wechsler et al., 2002). Approximately half that number report heavy episodic drinking on at least one occasion in the last 2 weeks (Wechsler et al., 2002), typically defined as consuming five or more drinks in a row for men and four or more drinks in a row for women (Wechsler et al., 1994). The National Institute on Alcohol Abuse and Alcoholism (NIAAA) National Advisory Council defines heavy episodic drinking as a pattern of drinking that brings the blood alcohol concentration (BAC) to .08% or above. For a typical adult, this concentration corresponds to consuming five or more drinks for men or four or more drinks for women in about 2 hours.
Each year, 2.8 million college students drive while intoxicated, more than 1,700 college students die from alcohol-related unintentional injury, and more than 500,000 are unintentionally injured as a result of alcohol use (Hingson et al., 2005). Other harms include decreased academic performance (Wechsler et al., 2002), property damage (Wechsler et al., 1995), interpersonal violence (Perkins et al., 2002), unintended or unprotected sexual activity (Perkins et al., 2002; Hingson et al., 2005), and sexual victimization (Abbey et al., 2002; Hingson et al., 2005).
Presley and Pimental (2006) categorized students by the amount and frequency of alcohol consumption and grouped drinkers into three risk categories: “nonheavy,” “heavy” (five or more drinks at least once in the past 2 weeks), and “heavy and frequent” (five or more drinks at least once in the past 2 weeks and drinking 3 or more days per week). The heavy and frequent drinkers were the highest risk group, as they were three times more likely to experience alcohol-related harms than heavy drinkers.
Despite campus and legislative policy changes, there has not been any significant change in the amounts of alcohol consumed or patterns of high-risk drinking over the last 20 years (Wechsler et al., 2002). A variety of prevention strategies have been implemented to reduce high-risk drinking and its consequences on college campuses, including programs that target freshmen, athletes, fraternity/sorority society members, and students that violate college alcohol policies (Larimer and Cronce, 2002, 2007). Group and individualized interventions delivered by counselors, peers, and resident advisors and Web-based programs have been adapted for college settings.
Brief motivational interventions (BMIs) that combine cognitive-behavioral skills with personalized feedback, norms clarification, risk-reduction strategies, and motivational enhancement have been effective (Larimer and Cronce, 2002, 2007). The NIAAA Task Force on College Drinking (Fleming, 2002) lists BMI as a Tier 1 preventive strategy with demonstrated effectiveness among college students. Previous trials conducted in nonmedical settings have shown that interventions combining cognitive-behavioral skills and motivational interviewing (MI) lead to reduced alcohol consumption by college students (Baer et al., 2001; Borsari and Carey, 2000; D'Amico and Fromme, 2000; Larimer et al., 2001; Marlatt et al., 1998). A review of BMI studies with college students by Fager and Melnyk (2004) suggested continued use of a personalized approach addressing expectancies and normative use employing a motivational interview style. These authors stated an urgent need for health care professionals to deliver evidence-based interventions in college health settings.
Problem drinking is prevalent, harmful, preventable, and treatable in the setting of outpatient primary care (Gordon, 2006). Multicontact BMIs delivered by primary health care providers have been shown to reduce alcohol consumption by three to nine drinks per week in adult patients (Whitlock et al., 2004). Within the timeframe of a standard primary care visit, multiple studies demonstrated that BMIs consistently produced reductions in alcohol consumption (Bertholet et al., 2005; Fleming et al., 1997; Grossberg et al., 2004; Kaner et al., 2007). Screening and brief counseling for alcohol misuse in primary care also are cost effective (Solberg et al., 2008). Despite potential barriers related to the implementation of BMIs by health care providers (e.g., practitioner attitudes, lack of training) or to preventive services in general (e.g., time constraints, lack of resources) (Miller et al., 2006; Saitz et al., 2003), the United States Preventive Services Task Force (2004) recommends routine screening and behavioral counseling interventions to reduce alcohol misuse by adults in primary care settings. The NIAAA stresses the primary care provider's role in identifying heavy drinkers and intervening to help reduce risky drinking behaviors.
College students who experience the greatest burden of alcohol-related harms and who have the greatest need for alcohol interventions may be the least likely to participate (Presley and Pimentel, 2006). The college student health center provides a unique opportunity to increase student participation in interventions, given the high patient volume and participation that student health centers have on campuses. The primary care provider at a student health center can address this important public health problem in the context of other health issues, often at the time when harms and consequences are present. Students who present to the student health center for routine medical care but are not actively seeking help for alcohol misuse may willingly discuss their drinking with a provider during this “teachable moment.”
The majority of student health centers do not provide routine alcohol screening, and many fail to provide appropriate treatment and referral, as a result of barriers of inadequate provider training, limited time, and limited resources (Foote et al., 2004). Students with high-risk drinking often are referred to alcohol-treatment programs that address alcohol abuse and dependence and often promote abstinence rather than harm reduction (Foote et al., 2004).
The student health center has been shown to be a feasible location to conduct screening and brief intervention for alcohol misuse, and previous research has suggested a need for an effectiveness trial based in a student health center (Ehrlich et al., 2006). This article presents the results of the first large randomized controlled trial to test the effectiveness of BMIs administered by primary care providers in a student health center to a sample of college students who screened positive for high-risk drinking.
Method
Study participants
The trial was conducted at the university health services of a large public southeastern university. The university's institutional review board approved the study. The university health services is centrally located on the campus. Health care providers encounter a variety of acute and chronic health care problems during 50,000 visits annually, and approximately half of the student population uses the university health services annually.
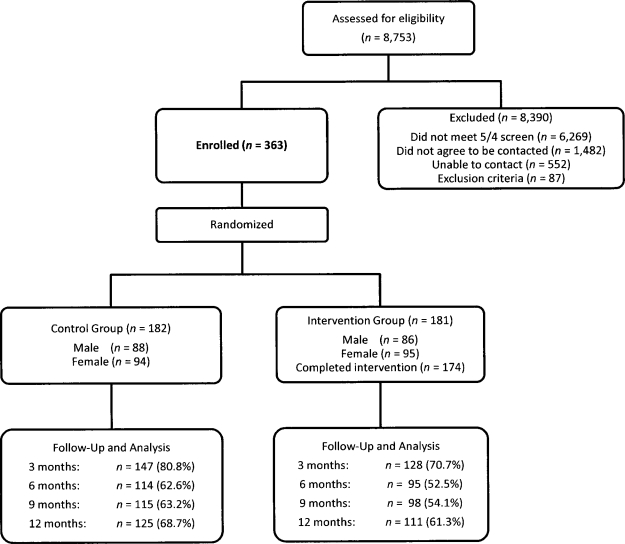
College students who sought care at the university health services completed an 11-item personal information form as a health history and screening tool. Figure 1 shows the flowchart of the enrollment of participants and the completion of data collection throughout the study period. Students were considered for inclusion in the study if they (1) answered “yes” to the personal information form 5/4 alcohol screening question (“Men, during the past 2 weeks have you had 5 or more drinks containing alcohol in a row on at least one occasion?” or “Women, during the past 2 weeks have you had 4 or more drinks containing alcohol in a row on at least one occasion?”) and (2) answered “yes” for permission to contact them to participate in research studies. The 5/4 definition was used as the screening question, because it meets the NIAAA (Task Force of the National Advisory Council on Alcohol Abuse and Alcoholism, 2002) recommendation for an efficient single question screen, and it has been extensively used in large-scale studies to identify high-risk drinkers (Wechsler et al., 2002).
Figure 1.
Enrollment and participation flowchart
Students were excluded from the study if they were younger than age 18, were pregnant, planned to leave the university within 12 months, were enrolled in an alcohol- or drug-treatment program, consumed more than 200 drinks in the past 30 days, or had a BAC greater than .35 on any day within the past 30 days. Students who exceeded these alcohol-consumption limits were thought to be at more immediate risk and were referred to the University Alcohol and Other Drug Prevention Office for evaluation and treatment. Students who met eligibility criteria were contacted via telephone and met with the project coordinator or a graduate research assistant during the enrollment period, November 2005 to November 2006.
The study was originally designed to have at least 200 participants (100 men and 100 women) for the duration of the 1-year period. To answer the primary research questions, account for an estimated 33% attrition, and achieve the necessary statistical power (.80 for an effect size of .20 with α at .05), the targeted sample size was 400 participants. Although more women than men seek care at the university health services, a decision was made to use stratified random sampling to enroll equal numbers of men and women. The sample consisted of 363 participants (189 females; 52%). The mean (SD) age was 20.6 (2.7) years. Participant race/ethnicity was 78% white, 11% Hispanic, 5% black, 2% Asian, and 4% other. Participants were 26% first-year, 21% second-year, 28% third-year, and 17% fourth-year college students, and 7% had graduated college.
Procedures
Subjects were block randomized using SPSS Version 15.0 (SPSS Inc., Chicago, IL) to either the control or the intervention group, where the order of the interventions varied randomly within each block. Randomization also was stratified by gender. The group assignment was placed into a sealed envelope by the data manager and was not available to those recruiting subjects until after informed consent was obtained. After consent, participants received instructions from the project coordinator or a research assistant on standard drink sizes and the method of completion of the Timeline Followback (TLFB) drinking calendar. They completed the online Healthy Lifestyle Questionnaire and TLFB baseline measures at a dedicated computer in a research office at the university health services. The baseline TLFB was reviewed by the project coordinator or a research assistant to ensure that the person continued to meet inclusion criteria. Participants were then assigned to the control or the intervention group based on preassignment.
Both control and intervention participants were provided an alcohol-prevention educational brochure, “Drinking: What's Normal, What's Not” (ETR Associates, 2004). Control group participants were assigned to university health services providers who received no training in the BMI protocol for their health care for the duration of the study. Intervention group participants were scheduled for two 20-minute BMI sessions, 2 weeks apart, with one of four providers trained in the BMI protocol. All future health care visits for those in the intervention group were scheduled with one of these providers for the duration of the study. At 3, 6, 9, and 12 months following enrollment, participants were contacted via email by the project coordinator or a research assistant with a reminder to complete their online follow-up Healthy Lifestyle Questionnaire and TLFB. Phone calls and reminder emails were sent weekly until follow-up data were received. After 60 days, data were considered incomplete. Participants were paid cash incentives up to $100 for completing study instruments ($30 at baseline; $10 each at 3, 6, and 9 months; $40 at 12 months).
Brief intervention protocol
As already stated, study participants assigned to the experimental group received two 20-minute BMI sessions administered by four trained providers (two physicians, one physician's assistant, and one nurse practitioner) within the university health services. The intervention combined patient-centered MI techniques (Miller and Rollnick, 2002) and cognitive-behavioral skills training based on the NIAAA curriculum “Clinical Protocols to Reduce High Risk Drinking in College Students” (Fleming, 2002) and the Brief Alcohol Screening and Intervention for College Students (BASICS; Dimeff et al., 1999). The MI framework included clinician empathizing, reflecting, reframing negative talk into change talk, rolling with resistance, avoiding argumentation, developing discrepancy between negative or ambivalent feelings toward alcohol, supporting self-efficacy through contemplation of past success, and acknowledging reluctance to change.
A “participant feedback” document was compiled by research staff based on each participant's responses to the Healthy Lifestyle Questionnaire and TLFB, and this document was used by the providers as the source of individual normative feedback information. The participant feedback document summarized the participant's Healthy Lifestyle Questionnaire responses regarding overall healthy lifestyle behaviors (nutrition, exercise, mental health, safety, tobacco, drugs, sleep); alcohol-related harms, especially drinking and driving; alcohol expectancies; tolerance; use of protective behaviors, including choosing not to drink, counting drinks and setting limits, eating before drinking, selecting a designated driver, and avoiding drinking games and distilled spirits; and readiness-to-change. The participant feedback document also summarized the TLFB data on quantity and frequency of alcohol consumption, including number of drinking days, average and peak number of drinks per drinking day, typical and peak BAC with instructions on estimation of BAC using a BAC card, and norms clarification by comparing personal alcohol consumption with peer alcohol consumption.
The focus of the first BMI session was to establish rapport between the participant and the provider. By initially focusing on the student's expressed healthy lifestyle concern, the provider was able to gain the interest and trust of the student, allowing for a facilitated introduction of the alcohol discussion and the start of cognitive-behavioral skills training. The second session maintained the student-centered focus of MI and stressed the alcohol skills training components of the BASICS program. At completion of the second BMI session, participants received the participant feedback document for future reference.
Before initiation of the trial, the four university health services providers conducting the brief interventions received 8 hours of education and training in MI techniques, the NIAAA curriculum “Clinical Protocols to Reduce High Risk Drinking in College Students,” and the BASICS curriculum. During the training the providers practiced the techniques through supervised role playing with mock patients. Fidelity to the MI model and the BMI protocol was achieved by monthly competency assessment sessions between each provider and a mental health counselor trained in MI, who reviewed session audiotapes. Participants completed a “participant comment” form after each BMI session, which rated the provider's level of empathy and statements that represented an MI approach. After each BMI session, the providers completed a “provider comment” form, which included a checklist of the MI skills and the BASICS components discussed. These forms were used by the trainer to give ongoing provider feedback throughout the intervention period.
Measures
Data were collected at enrollment (baseline) and 3, 6, 9, and 12 months thereafter. The following tools were used to gather data.
Healthy Lifestyle Questionnaire.
The Healthy Lifestyle Questionnaire is a 280-question, Web-based survey related to healthy behaviors, which the students completed in a range of 20 to 40 minutes. Fifty-five of the items related to alcohol-consumption behaviors, alcohol-related harms, and protective factors related to drinking. Other items included demographic data, alcohol expectancies, tobacco and drug use, and readiness-to-change behaviors. The entire tool was administered at baseline and at 12 months. A shortened version of the tool (120 items) was administered at the 3-, 6-, and 9-month follow-up periods; this version excluded the items related to expectancies and drug use.
Rutgers Alcohol Problem Index (RAPI).
The 23-item RAPI (White and Labouvie, 1989) was imbedded into the Healthy Lifestyle Questionnaire to measure frequency of alcohol-related harms. At baseline and at 12 months, participants were asked to report the frequency of harms in the past year. At 3, 6, and 9 months, participants were asked to report the frequency of harms in the previous 3 months. Counts were grouped into five categories: (0) 0 times, (1) 1-2 times, (2) 3-5 times, (3) 6-10 times, and (4) more than 10 times. Internal consistency was adequate at baseline and follow-up (Cronbach's α = .89-.92). A RAPI sum score was computed by adding the score for each of the 23 items.
Other harms.
Eight items from the Drinker Inventory of Consequences-2L (DrInC-2L; Miller et al., 1995) were imbedded into the Healthy Lifestyle Questionnaire. These items included driving under the influence of alcohol, riding with someone under the influence, risk taking, regrets, legal consequences, and physical injury. At baseline and at 12 months, frequencies from the past 12 months were reported. At 3, 6, and 9 months, participants reported frequencies for the prior 3-month period.
Readiness-to-change.
Readiness-to-change was assessed by the 12-item Readiness to Change Questionnaire (Rollnick et al., 1992). Based on responses, subjects were classified into one of three categories: precontemplation, contemplation, or action. Students also rated their readiness-to-change on a scale of 0 (not ready) to 10 (ready); this was called the readiness-to-change ruler.
Timeline Followback drinking measure.
Alcohol-consumption behaviors for the previous 30 days were recorded using the TLFB procedure. Participants recorded their drinking on an electronic calendar with self-identified historical reference points to enhance recall. The TLFB is a well-established tool that provides reliable self-reported drinking data (Sobell and Sobell, 1992). Typical and peak BACs were calculated from the TLFB data, which included gender and weight (Turner et al., 2004).
Data analysis
Chi-square or Fisher's exact tests for categorical variables and t-tests or Wilcoxon rank-sum tests for continuous variables were used to test for differences at baseline. Repeated measures analysis of covariance (RM ANCOVA) was used to test for differences between groups by modeling postbaseline outcomes, adjusting for baseline measure and the correlation of the repeated measures over time. Several covariance pattern models were fit in these analyses, where the structure with best fit was determined using Akaike information criteria (Fitzmaurice et al., 2004). These models were fit using the method of Maximum Likelihood and used all available data (Schafer and Graham, 2002).
Further modeling for secondary subgroup analyses for gender and baseline drinking category as covariates or effect modifiers was considered. If the overall trend test from RM ANCOVA was not significant, tests for significant group differences at each time point were adjusted using a Bonferroni correction. Individual harms from the DrInC-2L were modeled using longitudinal Negative Binomial count regression to account for skewness (Neal and Simons, 2007).
Two analyses to assess the impact of study attrition were performed: Differences in attrition rates between groups were assessed using a chi-square test, and pattern-mixture modeling was used to assess the impact of dropout (Hedeker and Gibbons, 1997; Najavits et al., 2007). In the pattern-mixture modeling, missing data patterns were considered in two ways: (1) a binary indicator variable that was 0 = had a response at baseline and at 12-month follow-up (completed) or 1 = did not have a response at 12-month follow-up (dropped out); and (2) patterns were grouped into four categories: all missing (no data), monotone (missed at least one follow-up and never returned), intermittent (missed at least one follow-up but provided data elsewhere), and complete case (no missing data). These two pattern groupings were considered in modeling as predictors as main effects and interaction effects with treatment group (Pattern × Treatment group). All analyses were performed on an intent-to-treat basis using SAS Version 9.1.3 (SAS Institute, Cary, NC) and Stata Version 10 (StataCorp LP, College Station, TX). A two-sided p value < .05 was considered to be statistically significant.
Results
Baseline comparability
Baseline demographic data, drinking behaviors, alcohol-related harms, and readiness-to-change assessment are given in Table 1. No significant differences between the intervention and control groups were noted at baseline on demographics, alcohol-consumption measures, and alcohol-related harms (p > .05), except for the harm “number of times drove after ≥3 drinks.” The control group reported significantly more occasions of this harm at baseline, compared with the intervention group (p < .01). An average of 8.6 (5.6) days drinking in the past 30 days was reported, with 5.2 (4.7) days of 5/4 heavy episodic drinking. The mean typical BAC was .08 (.05), and the mean peak BAC was .15 (.08). The participants at baseline were in the following risk categories (Presley and Pimentel, 2006): 19% nonheavy, 61% heavy, and 20% heavy and frequent.
Table 1.
Baseline demographics and outcomes of student participants (N = 363)
| Characteristic | Control (n = 182) n (%) or mean (SD) | Intervention (n = 181) n (%) or mean (SD) | p a |
| Demographics | |||
| Gender | .873 | ||
| Female | 94 (52%) | 95 (52%) | |
| Male | 88 (48%) | 86 (48%) | |
| Age | 20.6 (2.7) | 20.5 (2.8) | .74 |
| Academic class year | .71 | ||
| Freshman | 44 (24%) | 51 (28%) | |
| Sophomore | 35 (19%) | 41 (23%) | |
| Junior | 54 (30%) | 49 (27%) | |
| Senior | 34 (19%) | 28 (15%) | |
| Graduate/postbaccalaureate | 15 (8%) | 12 (7%) | |
| Race/ethnicity | .97 | ||
| White | 140 (77%) | 141 (78%) | |
| Black | 8 (4%) | 9 (5%) | |
| Hispanic | 23 (13%) | 18 (10%) | |
| American Indian/Alaskan Native | 0 | 1 (<1%) | |
| Asian | 3 (2%) | 5 (3%) | |
| Native Hawaiian/Pacific Islander | 1 (<1%) | 1 (<1%) | |
| Other | 6 (3%) | 5 (3%) | |
| Prefer not to respond | 1 (<1%) | 1 (<1%) | |
| Brief motivational intervention | 23.3 (3.5) | 23.9 (4.5) | .41 |
| Drinking behaviors | |||
| Typical BAC | .080 (.048) | .076 (.047) | .47 |
| Peak BAC | .158 (.086) | .144 (.082) | .21 |
| No. of drinks/sitting | 4.90 (2.38) | 4.69 (2.24) | .40 |
| No. days met 5/4 HED in month | 5.42 (4.93) | 5.04 (4.53) | .46 |
| Peak no. drinks in a sitting | 8.68 (4.36) | 8.15 (4.41) | .26 |
| Average no. drinks/week | 9.59 (8.36) | 8.38 (7.43) | .23 |
| No. times drunk in a typical week | 1.11 (1.20) | 1.14 (1.14) | .61 |
| Drinking category | .49 | ||
| Nonheavy drinker | 32(18%) | 36 (20%) | |
| Heavy drinker | 109 (60%) | 113 (62%) | |
| Heavy and frequent drinker | 41 (23%) | 32(18%) | |
| Alcohol-related harms | |||
| 23-item RAPI sum score | 16.1 (12.9) | 14.1 (12.9) | .09 |
| No. times drove after ≥3 drinks | 7.8 (16.9) | 4.7 (9.8) | <.01 |
| No. times taken foolish risks | 6.58 (11.9) | 5.43 (10.0) | .184 |
| Readiness-to-change | |||
| Readiness-to-change category | .27 | ||
| Pre-contemplative | 83 (46%) | 86 (48%) | |
| Contemplative | 41 (23%) | 48 (27%) | |
| Action | 54 (30%) | 40 (22%) | |
| Not available | 4 (2%) | 7 (4%) | |
| Readiness-to-change ruler | 4.93 (2.79) | 4.50 (2.49) | .14 |
Notes: BAC = blood alcohol concentration; HED = heavy episodic drinking; RAPI = Rutgers Alcohol Problem Index.
p value from t test or Wilcoxon rank-sum for continuous variables or chi-square or Fisher's exact test for categorical variables.
The average 23-item RAPI score at baseline was 15.1 (12.9) (median = 12). In terms of readiness-to-change drinking categories, 47% of the students were in precontemplation, 25% were in contemplation, and 26% were in action. The readiness-to-change ruler had excellent agreement with the readiness-to-change category assessment, and the mean was 4.7 (2.7).
Treatment effects over follow-up
Table 2 gives the comparison of the intervention and control groups on outcomes over the study follow-up. All outcome responses were moderately correlated across follow-ups, with ranges from r = .30 to .71. Compared with the control group, the intervention group had statistically significant reductions over time in drinking behavior outcomes: typical BAC (trend p = .018), peak BAC (trend p = .006), peak number of drinks in a sitting (trend p = .046), average number of drinks per week (trend p = .032), and number of times drunk in a typical week (trend p < .001). For the average number of drinks per sitting, there were statistically significant reductions in the intervention group only at 6 months (p = .027). For the number of days reporting 5/4 heavy episodic drinking in the past month, there were statistically significant reductions in the intervention group only at 6 months (p = .031).
Table 2.
Study outcomes over 12-month follow-upa
| Variable | Baseline | 3 months | 6 months | 9 months | 12 months | Trend p b |
| Drinking behaviors | ||||||
| Typical BAC | (.47) | (.003) | (.002) | (.603) | (.937) | .018 |
| Intervention | .076 [.003] | 057 [.004] | .057 [.004] | .059 [.005] | 060 [.004] | |
| Control | .080 [.004] | .071 [.004] | .073 [.005] | .062 [.004] | .060 [.004] | |
| Peak BAC | (.21) | (.003) | (<0.001) | (.309) | (.646) | .006 |
| Intervention | .144 [.006] | .112 [.007] | .108 [.007] | .110 [.008] | .113 [.007] | |
| Control | .158 [.006] | .142 [.007] | .145 [.008] | .122 [.007] | .118 [.007] | |
| Average no. drinks/sitting | (.40) | (.147) | (.027) | (.928) | (.757) | .064 |
| Intervention | 4.69 [0.168] | 4.029 [0.239] | 3.818 [0.244] | 3.982 [0.289] | 3.969 [0.224] | |
| Control | 4.90 [0.176] | 4.497 [0.228] | 4.559 [0.254] | 4.009 [0.214] | 4.043 [0.224] | |
| No. days met 5/4 HED in month | (.46) | (.322) | (.031) | (.534) | (.942) | .102 |
| Intervention | 5.04 [0.339] | 4.55 [0.464] | 3.92 [0.399] | 3.94 [0.414] | 4.34 [0.439] | |
| Control | 5.42 [0.366] | 5.37 [0.484] | 5.33 [0.570] | 4.79 [0.554] | 4.37 [0.554] | |
| Peak no. drinks in a sitting | (.26) | (.029) | (.005) | (.626) | (.700) | .046 |
| Intervention | 8.15 [0.330] | 6.87 [0.400] | 6.52 [0.392] | 6.71 [0.411] | 6.71 [0.392] | |
| Control | 8.68 [0.323] | 8.03 [0.382] | 7.98 [0.394] | 6.92 [0.333] | 6.92 [0.340] | |
| Average no. drinks/week | (.23) | (.033) | (.007) | (.134) | (.700) | .032 |
| Intervention | 8.38 [0.549] | 7.33 [0.627] | 6.16 [0.558] | 6.12 [0.534] | 6.45 [0.555] | |
| Control | 9.59 [0.619] | 9.47 [0.715] | 8.90 [0.733] | 7.47 [0.635] | 7.26 [0.620] | |
| No. times drunk in a typical week | (.61) | (<.001) | (.003) | (.078) | (.727) | <.001 |
| Intervention | 1.14 [0.086] | 0.854 [0.069] | 0.713 [0.070] | 0.936 [0.099] | 1.31 [0.157] | |
| Control | 1.11 [0.089] | 1.24 [0.085] | 1.10 [0.081] | 1.33 [0.113] | 1.70 [0.152] | |
| Alcohol-related harmsc | ||||||
| 23-item RAPIsum score | (.09) | (.447) | (.028) | (.041) | (.556) | .030 |
| Intervention | 14.1 [0.977] | 6.22 [0.537] | 4.96 [0.490] | 4.58 [0.495] | 5.80 [0.457] | |
| Control | 16.1 [0.987] | 7.80 [0.617] | 6.55 [0.605] | 6.17 [0.644] | 7.36 [0.581] | |
| No. times drove after ≥3 drinks | (<.01) | (.005) | (.549) | (.998) | (.542) | .136 |
| Intervention | 4.69 [0.735] | 0.929 [0.180] | 0.890 [0.175] | 1.03 [0.154] | 2.24 [0.268] | |
| Control | 7.84 [1.28] | 2.02 [0.334] | 1.23 [0.257] | 1.40 [0.242] | 3.60 [0.882] | |
| No. times taken foolish risks | (.184) | (.004) | (.685) | (.485) | (.261) | .036 |
| Intervention | 5.43 [0.753] | 1.12 [0.227] | 1.54 [0.353] | 1.39 [0.301] | 3.14 [0.780] | |
| Control | 6.58 [0.896] | 2.24 [0.347] | 1.72 [0.321] | 2.23 [1.10] | 4.80 [1.26] | |
| Readiness-to-change | ||||||
| Readiness-to-change ruler | (.14) | (.644) | (.984) | (.312) | (.539) | .981 |
| Intervention | 4.50 [0.192] | 4.58 [0.198] | 4.59 [0.207] | 4.34 [0.210] | 4.44 [0.209] | |
| Control | 4.93 [0.211] | 4.59 [0.189] | 4.60 [0.196] | 4.35 [0.202] | 4.44 [0.199] | |
Notes: BAC = blood alcohol concentration; HED = heavy episodic drinking; RAPI = Rutgers Alcohol Problem Index.
Values in each postbaseline column represent: (p value) adjusted mean [SE]; (p value) in parentheses represents significance for treatment group differences uncorrected for multiple comparisons if overall trend p value is significant; if overall trend p value is not significant, (p value) represents significance for group differences with Bonferroni correction;
trend p value is from repeated measures analysis of covariance model adjusting for baseline measure and correlation of repeated measures over time; trend p value < .05 indicates a significant difference between treatment groups over time;
baseline and 12 months represent average frequencies reported in past 12 months.
Alcohol-related harms as measured by the 23-item RAPI scores were reduced for the intervention group, compared with the control group at 6 months (p = .028) and 9 months (p = 0.041), and the overall trend after baseline was significant (trend p = .030). There were statistically significant reductions in the intervention group, compared with the control group, only at 3 months in number of times drove after three or more drinks (p = .005). There were statistically significant reductions in the intervention group only at 3 months in number of times taken foolish risks (p = .004), and the overall trend after baseline was significant (trend p = .036).
In subgroup analyses, the interaction effects of the treatment group and the baseline drinking category were marginally significant (p = .09). The adjusted means from the trend model for the heavy and frequent group were 7.6 for the intervention group and 12.3 for the control group. Although the marginally significant effect could be the result of the small sample size of this subgroup (n = 73), this observed difference may be of clinical importance. There were no significant differences between groups in the readiness-to-change measures after baseline.
Longitudinal attrition
Study follow-up rates were n = 275 (76%) at 3 months, n = 209 (58%) at 6 months, n = 213 (59%) at 9 months, and n = 236 (65%) at 12 months. There were no significant differences in follow-up rates by treatment group (χ2 = 1.45, 4 df, p = .84). In terms of patterns of missing data on outcomes, the range (depending on TLFB or Healthy Lifestyle Questionnaire data) of participants with all missing data was 0%-1%, monotone = 30%-34%, intermittent = 21%-36%, and complete case = 33%-45%. No outcomes had intervention differences moderated by a missing data pattern (p > .10), except number of times drunk for only one of the two pattern operationalizations (Pattern × Group interaction p = .043).
Discussion
Our findings replicate previous studies showing the effectiveness of BMIs with college students. We have demonstrated that BMI delivered by providers within a student health center is effective in reducing negative alcohol behaviors and associated harms among college students screened for high-risk drinking. We addressed a few limitations in some of the previous BMI studies with college students, including small sample size, short-term follow-up, and intervention strategies that were impractical for use by primary care providers. Our study achieved a sample size of 363, follow-up outcomes at 3-month intervals up to 12 months, and a BMI protocol that was feasible and acceptable for use in a student health center.
There have been more than 70 reported studies testing the effectiveness of BMIs in medical settings. However, there has been only one other randomized controlled trial conducted specifically with college students and delivered in a health care setting (Dimeff and McNeely, 2000), but that study was limited by a small sample size of 41. Monti et al. (1999) tested a single-session BMI delivered by a research therapist in the emergency department with patients ages 18 and 19 and showed a 3-month reduction in alcohol-related injuries but no difference in alcohol use. Martens et al. (2007) examined BMIs at a university-based health and mental health care setting and showed reductions in alcohol use, but that study was limited by a brief 6-week follow-up and the lack of a control group.
In addition to short-term intervention effects, the intent of delivering BMIs is to achieve long-term effects with sustained behavior change and reduction of alcohol-related harms. Testing the duration of the intervention effect has been limited in other BMI studies with college students, and only one study has reported outcomes beyond 6 months. The longest term study (Marlatt et al., 1998) reported a 4-year follow-up (Baer et al., 2001), showing that the BMI group had significant decreases in alcohol-related problems but not sustained decreases in alcohol consumption. Our short-term drinking behavior outcomes showed significant reductions in the intervention group, compared with the control group, in five of the seven outcomes at the 3-month and 6-month follow-up intervals. There was a loss of a long-term intervention effect for these outcomes because the intervention group failed to show statistically significant reductions, compared with the control group, at the 9- and 12-month intervals. The alcohol-related harms outcome data showed slightly longer duration intervention effects, with reductions in RAPI sum scores at 6 and 9 months but not at 12 months. Improved long-term effectiveness could possibly be achieved by a “booster effect” at the 6-month interval and might include scheduling brief follow-up provider appointments or implementing a reminder in the health record to discuss alcohol use at future appointments.
The subgroup analysis did not rule out that the BMI was equally effective with all three Presley and Pimentel (2006) baseline risk groups. Although risk group subanalysis did not reach statistical significance for the 73 students in the heavy and frequent group, there was a trend toward an intervention effect. This highest risk group could be the focus of a resource-limited BMI protocol or referral to a more intense intervention outside of the student health center.
One of the goals of the intervention was to move students along the readiness-to-change continuum by motivating them to begin to contemplate their drinking behavior and to consider change. Readiness-to-change self-assessment did not change over the 1-year period, but, the participants in the BMI intervention group achieved positive behavior change as measured in decreased alcohol use and harms outcome data.
The student health center has high use rates and offers an opportunity to identify and treat a large number of high-risk drinking students that come from all academic class years and race and ethnic groups. The 2007 National College Health Assessment (American College Health Association, 2008) found that students surveyed identified student health center medical staff and health educators as the most believable source of information about health issues. College students may be more open to discuss sensitive issues, such as alcohol misuse, at a confidential health care visit and in the context of routine medical care, at a time when they are focused on health and more likely to consider health behavior change.
We witnessed a wide spectrum of alcohol use and misuse and encountered extremely high-risk students and those with alcohol-use disorders, including three students enrolled who were involuntarily withdrawn from the study and referred for more intense treatment of possible alcohol abuse or dependence (according to Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, criteria; American Psychiatric Association, 1994). A recent survey showed that 31% of college students met the criteria for alcohol abuse, and 6% met the criteria for dependence (Knight at al., 2002). These extremely high-risk students might be identified only by means of routine screening and intervention at the student health center.
There was a 28% positive response rate to the 5/4 definition screening question among the group of students presenting to the university health services for initial registration. This rate is lower than the 40%-44% overall college population 5/4 definition prevalence rate observed in the College Alcohol Study conducted in 1993, 1997, 1999, and 2001 (Wechsler et al., 2002). Female students typically have a lower rate of high-risk drinking, and 67% of the students that present to the university health services are female. The relatively low 28% prevalence rate is a possible limitation of this study as a result of possible selection bias and the possible reluctance by certain students to accurately report a positive response to the 5/4 screen at the time of enrollment to the university health services.
Another possible limitation of this study is the questionable reliability of self-reported alcohol use, as there were no independent confirmations of alcohol use. However, research supports the validity and reliability of self-reported alcohol use (Sobell and Sobell, 1992; Wechsler et al., 1994). Despite assurances of confidentiality, it is possible that those who received the BMI may have wanted to “please” their provider by reporting falsely lower drinking rates and harms. This limitation was likely moderated by collecting data over 12 months. The university IRB required the control group to receive a brochure on alcohol prevention, and this alcohol information may have influenced the control group outcomes.
Although anticipated, the attrition rate was another possible limitation. The analysis of attrition data found no differences, with the exception of “number of times drunk past 30 days.” The primary reasons for attrition were leaving the university and the time required to complete data collection every 3 months.
The BMI protocol was developed to be brief and efficient sessions that focused on behavior change and harm reduction. As previous research has shown (Ehrlich et al., 2006), our participants and providers found the BMI protocol feasible and acceptable for use at a student health center. A review of the Provider Comment forms indicated that the MI approach facilitated discussion of student alcohol use. A review of the Participant Feedback forms indicated that 90% of the students rated their providers as mostly or highly empathic. Providers intended to deliver the intervention consistent with the principles of MI, yet the need to provide alcohol skills information necessitated at times a more directive and informational approach. Further research is needed to determine how to optimally deliver the most effective components of the alcohol skills curriculum while maintaining MI techniques in a brief clinical setting.
The “healthy lifestyle” context of this study, approaching the topic of alcohol misuse by way of other preventive health topics, allowed for a more accepted and effective introduction and discussion of the topic of alcohol use and misuse. The BMI in this study was delivered within the context of a dedicated holistic preventive health visit, but the staff of a student health center might choose to deliver the BMI at the teachable moment when the student presents with an acute alcohol-related problem or is identified as high risk through routine screening. Investigation of the effectiveness of BMI delivered outside of the dedicated prevention visit at a student health center is warranted.
There is currently poor compliance with alcohol screening and BMI by providers at student health centers, partly because of a lack of effective MI skills and alcohol-counseling knowledge necessary to administer an effective BMI (Foote et al., 2004). Given the success of our study at a student health center and BMI studies with college students in other settings, methods to improve compliance at student health centers should be considered, such as improved provider training and streamlining the BMI for use in a busy clinical setting. There is a need for a more efficient distribution of feedback. The student's alcohol information could be entered in a computer-based format at the student health center or at another confidential setting, and a personalized normative feedback summary would be immediately available for a BMI in the student health center. Considering the extensive amount of alcohol-related morbidity encountered by college students presenting to student health centers, it is incumbent on the college health care system to adopt routine, efficacious, and sustainable alcohol screening and BMI protocols.
Acknowledgment
The authors thank Michael E. Dunn, Ph.D., for his invaluable assistance in conducting this study.
Footnotes
This research was supported by National Institute on Alcohol Abuse and Alcoholism grants 1 U18 AA015673-01 and U01 AA14741
References
- Abbey A. Alcohol-related sexual assault: A common problem among college students. J. Stud. Alcohol. 2002;(Supplement No. 14):118–128. doi: 10.15288/jsas.2002.s14.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American College Health Association. American College Health Association-National College Health Assesssment Spring 2007 Reference Group Data Report (Abridged) J. Amer. Coll. Hlth. 2008;56:469–479. doi: 10.3200/JACH.56.5.469-480. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) Washington, DC: 1994. [Google Scholar]
- Baer JS, Kivlahan DR, Blume AW, McKnight P, Marlatt AG. Brief intervention for heavy-drinking college students: 4-year follow-up and natural history. Amer. J. Publ. Hlth. 2001;91:1310–1316. doi: 10.2105/ajph.91.8.1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: Systematic review and meta-analysis. Arch. Intern. Med. 2005;165:986–995. doi: 10.1001/archinte.165.9.986. [DOI] [PubMed] [Google Scholar]
- Borsari B, Carey KB. Effects of a brief motivational intervention with college student drinkers. J. Cons. Clin. Psychol. 2000;68:728–733. [PubMed] [Google Scholar]
- D'Amico EJ, Fromme K. Implementation of the risk skills training program: A brief intervention targeting adolescent participation in risk behaviors. Cog. Behav. Pract. 2000;7:101–117. [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA. Brief Alcohol Screening and Intervention for College Students: A Harm Reduction Approach. New York: Guilford Press; 1999. [Google Scholar]
- Dimeff LA, McNeely M. Computer-enhanced primary care practitioner advice for high-risk college drinkers in a student primary health-care setting. Cog. Behav. Pract. 2000;7:82–100. [Google Scholar]
- Ehrlich PF, Haque A, Swisher-McClure S, Helmkamp J. Screening and brief intervention for alcohol problems in a university student health clinic. J. Amer. Coll. Hlth. 2006;54:279–287. doi: 10.3200/JACH.54.5.279-288. [DOI] [PubMed] [Google Scholar]
- ETR Associates. Drinking: What's Normal, What's Not. Title No. R041. Scotts Valley, CA: ETR Associates; 2004. [Google Scholar]
- Fager JH, Melnyk BM. The effectiveness of intervention studies to decrease alcohol use in college undergraduate students: An integrative analysis. Worldviews on evidence-based nursing. 2004;1:102–119. doi: 10.1111/j.1741-6787.2004.04028.x. [DOI] [PubMed] [Google Scholar]
- Fitzmaurice GM, Laird NM, Ware JH. Applied Longitudinal Analysis. Hoboken, NJ: John Wiley & Sons; 2004. [Google Scholar]
- Fleming M. (Developed for the NIAAA Task Force on College Drinking). Clinical Protocols to Reduce High Risk Drinking in College Students: The College Drinking Prevention Curriculum for Health Care Providers. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2002. [Google Scholar]
- Fleming MF, Barry KL, Manwell LB, Johnson K, London R. Brief physician advice for problem alcohol drinkers: A randomized controlled trial in community-based primary care practices. JAMA. 1997;277:1039–1045. [PubMed] [Google Scholar]
- Foote J, Wilkens C, Vavagiakis P. A national survey of alcohol screening and referral in college health centers. J. Amer. Coll. Hlth. 2004;52:149–157. [PubMed] [Google Scholar]
- Gordon A. Screening the drinking: Identifying problem alcohol consumption in primary care settings. Johns Hopkins Adv. Stud. Med. 2006;6:137–147. [Google Scholar]
- Grossberg PM, Brown DD, Fleming MF. Brief physician advice for high-risk drinking among young adults. Ann. Fam. Med. 2004;2:474–480. doi: 10.1370/afm.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedeker D, Gibbons RD. Application of random-effects pattern-mixture models for missing data in longitudinal studies. Psychol. Meth. 1997;2:64–78. [Google Scholar]
- Hingson R, Heeren T, Winter M, Wechsler H. Magnitude of alcohol-related mortality and morbidity among U.S. college students ages 18-24: Changes from 1998 to 2001. Annual Rev. Publ. Hlth. 2005;26:259–279. doi: 10.1146/annurev.publhealth.26.021304.144652. [DOI] [PubMed] [Google Scholar]
- Kaner EFS, Dickinson HO, Beyer FR, Campbell F, Schlesinger C, Heather N, Saunders JB, Burnand B, Pienaar ED. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database of System. Rev. 2007;2:CD004148. doi: 10.1002/14651858.CD004148.pub3. [DOI] [PubMed] [Google Scholar]
- Knight JR, Wechsler H, Kuo M, SeibrIng M, Weitzman ER, Schuckit MA. Alcohol abuse and dependence among U.S. college students. J. Stud. Alcohol. 2002;63:263–271. doi: 10.15288/jsa.2002.63.263. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Cronce JM. Identification, prevention and treatment: A review of individual-focused strategies to reduce problematic alcohol consumption by college students. J. Stud. Alcohol. 2002;(Supplement No. 14):148–163. doi: 10.15288/jsas.2002.s14.148. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Cronce JM. Identification, prevention, and treatment revisited: Individual-focused college drinking prevention strategies 1999-2006. Addict. Behav. 2007;32:2439–2468. doi: 10.1016/j.addbeh.2007.05.006. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Turner AP, Anderson BK, Fader JS, Kilmer JR, Palmer RS, Cronce JM. Evaluating a brief alcohol intervention with fraternities. J. Stud. Alcohol. 2001;62:370–380. doi: 10.15288/jsa.2001.62.370. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Baer JS, Kivlahan DR, Dimeff LA, Larimer ME, Quigley LA, Somers JM, Williams E. Screening and brief intervention for high-risk drinking college student drinkers: Results from a two-year follow-up assessment. J. Cons. Clin. Psychol. 1998;66:604–615. doi: 10.1037//0022-006x.66.4.604. [DOI] [PubMed] [Google Scholar]
- Martens MP, Cimini MD, Barr AR, Rivero EM, Vellis PA, Desemone GA, Horner KJ. Implementing a screening and brief intervention for high-risk drinking in university-based health and mental health care settings: Reductions in alcohol use and correlates of success. Addict. Behav. 2007;32:2563–2572. doi: 10.1016/j.addbeh.2007.05.005. [DOI] [PubMed] [Google Scholar]
- Miller WR, Baca C, Compton WM, Ernst D, Manuel JK, Pringle B, Schermer CR, Weiss RD, Willenbring ML, Zweben A. Addressing substance abuse in health care settings. Alcsm Clin. Exp. Res. 2006;30:292–302. doi: 10.1111/j.1530-0277.2006.00027.x. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd Edition. New York: Guilford Press; 2002. [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. The Drinker Inventory of Consequences (DrInC): An Instrument for Accessing Adverse Consequences of Alcohol Abuse (Test Manual). NIAAA Project MATCH Monograph Series, Vol. 4, NIH Publication No. 95-3911. [Google Scholar]
- Monti PM, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, Myers M, Woolard R, Lewander W. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. J. Cons. Clin. Psychol. 1999;67:989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Harned MS, Gallop RJ, Butler SF, Barber JP, Thase ME, Crits-Christoph P. Six-month treatment outcomes of cocaine-dependent patients with and without PTSD in a multisite national trial. J. Stud. Alcohol Drugs. 2007;68:353–361. doi: 10.15288/jsad.2007.68.353. [DOI] [PubMed] [Google Scholar]
- Neal DJ, Simons JS. Inference in regression models of heavily skewed alcohol use data: A comparison of ordinary least squares, generalized linear models, and bootstrap resampling. Psychol. Addict. Behav. 2007;21:441–452. doi: 10.1037/0893-164X.21.4.441. [DOI] [PubMed] [Google Scholar]
- Perkins HW. Surveying the damage: A review of research on consequences of alcohol misuse in college populations. J. Stud. Alcohol. 2002;(Supplement No. 14):91–100. doi: 10.15288/jsas.2002.s14.91. [DOI] [PubMed] [Google Scholar]
- Presley CA, Pimentel ER. The introduction of the heavy and frequent drinkers: A proposed classification to increase accuracy of alcohol assessment in postsecondary educational settings. J. Stud. Alcohol. 2006;67:324–331. doi: 10.15288/jsa.2006.67.324. [DOI] [PubMed] [Google Scholar]
- Rollnick S, Heather N, Gold R, Hall W. Development of a short ‘readiness to change’ questionnaire for use in brief, opportunistic interventions among excessive drinkers. Brit. J. Addict. 1992;87:743–754. doi: 10.1111/j.1360-0443.1992.tb02720.x. [DOI] [PubMed] [Google Scholar]
- Saitz R, Horton NJ, Sullivan LM, Moskowitz MA, Samet JH. Addressing alcohol problems in primary care: A cluster randomized, controlled trial of a systems intervention. The screening and intervention in primary care (SIP) study. Ann. Intern. Med. 2003;138:372–382. doi: 10.7326/0003-4819-138-5-200303040-00006. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychol. Meth. 2002;7:147–177. [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-report alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring Alcohol Consumption: Psychology and Biochemical Methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Solberg LI, Maciosek MV, Edwards NM. Primary care intervention to reduce alcohol misuse: Ranking its health impact and cost effectiveness. Amer. J. Prev. Med. 2008;34:143–152. doi: 10.1016/j.amepre.2007.09.035. [DOI] [PubMed] [Google Scholar]
- Task Force of the National Advisory Council on Alcohol Abuse and Alcoholism. A Call to Action: Changing the Culture of Drinking at U.S. Colleges, NIH Pub. No. 02-5010. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2002. [Google Scholar]
- Turner JC, Bauerle J, Shu J. Estimated blood alcohol concentration correlation with self-reported negative consequences among college students using alcohol. J. Stud. Alcohol. 2004;65:741–749. doi: 10.15288/jsa.2004.65.741. [DOI] [PubMed] [Google Scholar]
- United States Preventive Services Task Force. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: Recommendation statement. Ann. Intern. Med. 2004;140:554–556. doi: 10.7326/0003-4819-140-7-200404060-00016. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Davenport A, Dowell G, Moeykens B, Castillo S. Health and behavioral consequences of binge drinking in college: A national survey of students at 140 campuses. JAMA. 1994;272:1672–1677. [PubMed] [Google Scholar]
- Wechsler H, Lee JE, Kuo M, Seibring M, Nelson TF, Lee H. Trends in college binge drinking during a period of increased prevention efforts: Findings from 4 Harvard School of Public Health College Alcohol Study surveys: 1993-2001. J. Amer. Coll. Hlth. 2002;50:203–217. doi: 10.1080/07448480209595713. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Moeykens B, Davenport A, Castillo S, Hansen J. The adverse impact of heavy episodic drinkers on other college students. J. Stud. Alcohol. 1995;56:628–634. doi: 10.15288/jsa.1995.56.628. [DOI] [PubMed] [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. J. Stud. Alcohol. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- Whitlock EP, Polen MR, Green CA, Orleans T, Klein J. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: A summary of the evidence for the U.S. Preventive Services Task Force. Ann. Intern. Med. 2004;140:557–568. doi: 10.7326/0003-4819-140-7-200404060-00017. [DOI] [PubMed] [Google Scholar]