Abstract
This is a report of a middle-aged male with blepharochalasis, who was successfully treated with oral acetazolamide. To our knowledge, this is the first case in the literature reporting the benefits of the use of acetazolamide in the treatment of blepharochalasis.
Keywords: blepharochalasis, acetazolamide, eyelid edema
Introduction
Blepharochalasis is a rare condition that usually affects younger individuals and is characterized by lax, thin and wrinkled eyelid skin (Held and Schneiderman 1990; Piffaretti and Haefliger 2004). The methods described to manage the cosmetic appearance of the skin involves the use of steroids and surgery for blepharoplasty, with or without aponeurotic repair for persistent ptosis. These methods have met with only limited success. We report a case of a middle-aged patient with blepharochalasis, who was successfully treated with oral acetazolamide.
Case report
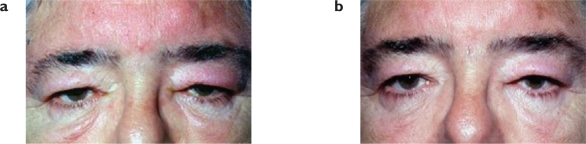
A 57-year old man was referred to the Eye Department in November 2003 because of a history of persisting periorbital swelling over a 4-year period, that tended to improve towards the end of the day. At the eye clinic, he presented with bilateral painless periorbital edema and some degree of erythema (Figure 1a). The patient was a controlled hypertensive on bendrofluazide and enalapril; he also suffered from sleep apnea and renal calculi. He had been previously investigated at the Dermatology and lymphedema clinics but no significant underlying abnormalities were identified.
Figure 1.
(a) Initial presentation: Bilateral eyelid oedema. Corneal reflexes can not be visualised on primary position. (b) Nine months later: improvement of periorbital oedema. Both corneal reflexes are visible on primary position.
From the clinical examination and the long history of regular swelling, the diagnosis of bilateral blepharochalasis was made. Management was conservative with no treatment at the beginning.
Three months later the appearances had not changed and he was then started on medical treatment. Surgical correction was not indicated because of the risk of recurrent edema in the immediate post operative period. The patient was initially started on low dose of systemic steroids but with no improvement and, after consultation with the urologists, the patient was then changed to oral acetazolamide 250 mg SR daily.
After 4-months, oral acetazolamide proved to be effective in reducing the periorbital edema and improving the symptoms of discomfort in the periorbital region. Due to the side effects of acetazolamide (paraesthesiae), the treatment was tapered off over the following month (250 mg acetazolamide SR on alternate days). Nine months from presentation, the periorbital swelling had clearly reduced and the patient remained asymptomatic and was happier with his appearance (Figure 1b). He still refused to consider blepharoplasty surgery, which was offered at this stage to debulk the remaining skin tissue. At his last follow up appointment, now 3-years since presentation, he remains asymptomatic and is still not willing to consider surgical intervention.
Comment
To our knowledge, this is the first case in the literature reporting the benefits of the use of acetazolamide in the treatment of blepharochalasis.
Blepharochalasis comes from the Greek words blepharo (= eyelid) and chalasis (= slackening) (Albert and Jakobiec 1999, p 112). It describes recurrent attacks of idiopathic transient painless edema of the upper eyelids, that may produce permanent tissue changes. Because of recurrences, the eyelid skin of patients becomes thin and wrinkled, simulating the appearances of dermatochalasis (Held and Schneiderman 1990). In this case, the presence of prior chronic recurrent eyelid edema was an important differentiating feature. Similarly, in a review of 30 cases of blepharochalasis, the histopathology (reported as variable picture of epithelial atrophy, vasculitis and loss of elastic fibers) did not aid in differentiating the condition from angioedema, lymphedema or dermatochalasis (Collin 1991). The diagnosis again was based on clinical features of intermittent attacks of localized swelling affecting one or more eyelids, associated with thinning of the eyelid skin (Bergin et al 1988).
A pathophysiological explanation which considers blepharochalasis as a localized angioedema has been proposed (Jordan 1992; Piest 1999). Furthermore, it has been reported that eye diseases have been associated with sleep apnea syndrome, upper lid ptosis and blepharochalasis (Mojon 2001). In our patient, sleep apnea could have also played a role in his blepharochalasis.
Standard practice has been to address the joint problem of recurrent inflammation and redundant skin. Various authors have reported effective use of systemic steroids and the need for blepharoplasty, which may require to be repeated (Collin et al 1979; Bergin et al 1988; Collin 1991). Our attempt to treat with steroids was ineffective and potential problems with fragile control of his hypertension prompted us to discontinue this form of management. Surgery was not employed, as this patient has persistently declined any surgical intervention. However, surgical repair of blepharochalasis, an option usually kept for the quiescent stage, may be complicated by repeated episodes of inflammation and edema, causing recurrence of ptosis and other eyelid changes (Collin et al 1979; Collin 1991).
There is, therefore, no well defined, established treatment protocol for the management of blepharochalasis. Treatment with steroids has been described as effective, on the basis of their powerful anti-inflammatory properties (Habal 1985). The treatment, which we have given using oral acetazolamide, promoted the resolution of the edema, but the exact mechanism is not fully understood: it seems that the improvement was likely to be based on its diuretic properties (BNF 2005).
Here we presented a patient with blepharochalasis with significant improvement after treatment with oral acetazolamide. We suggest that acetazolamide, not having the side effects of steroids, is a non-invasive alternative approach for treating patients with blepharochalasis, seeking cosmetic improvement but not keen on surgery. This could be considered at a later stage in development, when all signs of inflammation have resolved.
References
- Albert DM, Jakobiec FA. Blepharochalasis. Principles and Practice of Ophthalmology. 1999;1:112. [Google Scholar]
- Bergin DJ, McCord CD, Berger T, et al. Blepharochalasis. Br J Ophthalmol. 1988;72:863–7. doi: 10.1136/bjo.72.11.863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BNF . British national formulary. 50th edn. 2005. Carbonic anhydrase inhibitors; p. 71. [Google Scholar]
- Collin JR. Blepharochalasis. A review of 30 cases. Ophthal Plast Reconstr Surg. 1991;7:153–7. doi: 10.1097/00002341-199109000-00001. [DOI] [PubMed] [Google Scholar]
- Collin JR, Beard C, Stern WH, et al. Blepharochalasis. Br J Ophthalmol. 1979;63:542–6. doi: 10.1136/bjo.63.8.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habal MB. Prevention of postoperative facial edema with steroids after facial surgery. Aesthetic Plast Surg. 1985;9:69–71. doi: 10.1007/BF01570331. [DOI] [PubMed] [Google Scholar]
- Held JL, Schneiderman P. A review of blepharochalasis and other causes of the lax, wrinkled eyelid. Cutis. 1990;45:91–4. [PubMed] [Google Scholar]
- Jordan DR. Blepharochalasis syndrome: a proposed pathophysiologic mechanism. Can J Ophthalmol. 1992;27:10–15. [PubMed] [Google Scholar]
- Mojon D. Eye diseases in sleep apnea syndrome. Ther Umsch. 2001;58:57–60. doi: 10.1024/0040-5930.58.1.57. [DOI] [PubMed] [Google Scholar]
- Piest KL.1999Eyelid edema Decision making in ophthalmology; an algorithmic approach van Heuven WAJ, Zwaan Johan.(publishers) Mosby; 2nd edition112–13. [Google Scholar]
- Piffaretti JM, Haefliger IO. Etiology of eyelid edema. Ther Umsch. 2004;61:661–3. doi: 10.1024/0040-5930.61.11.661. [DOI] [PubMed] [Google Scholar]