Abstract
Thymosin beta 4 (Tβ4) is a low molecular weight protein present in all cells except erythrocytes. Although Tβ4 is the major monomeric actin-sequestering peptide in cells and can depolymerize F-actin, evidence is mounting to support the idea that it has multiple, seemingly diverse, cellular functions. In cornea, as in other tissues, Tβ4 promotes cell migration and wound healing, has anti-inflammatory properties, and suppresses apoptosis. In this review we discuss the current state of knowledge regarding the effects of Tβ4 in maintaining the healthy, functional cornea. The clinical implications of the use of Tβ4 as a wound healing and anti-inflammatory agent are discussed.
Keywords: apoptosis, cell migration, cornea, inflammation, thymosin beta 4, wound healing
Corneal epithelial wounds: overview
The cornea consists of three types of cells, epithelial, stromal, and endothelial. It is avascular, transparent, and the most sensitive tissue in the body. The cornea functions as an optical lens that refracts light, but it also contributes to the rigid shell of the eyeball. In order to optimally refract light and ensure clear vision, the cornea must maintain optical transparency. This is accomplished in the stroma by a well-organized arrangement of collagen fibers into lamellae (Meek et al 2003). The endothelium functions to preserve corneal transparency by regulating the level of hydration in the stroma. The corneal epithelium also contributes to the maintenance of corneal transparency (Verkman 2003). Damage to the corneal epithelium caused by chemical, physical or microbial insults can lead to swelling of the stroma, the activation of stromal fibroblasts, and the infiltration of inflammatory cells, leading to the loss of corneal transparency and integrity. Timely resurfacing of the epithelium after injury is thus essential in preventing the loss of normal corneal function and loss of vision.
Following wounding, corneal epithelial healing occurs in several stages by a combination of three separate mechanisms, migration, mitosis, and differentiation (Gipson and Inatomi 1995). Through a highly organized chain of events, cells must migrate to cover the denuded stroma, and then proliferate and differentiate to restore the normal multi-layered epithelial cytoarchitecture (Zhao et al 2003). In most instances, corneal epithelial defects caused by a simple injury, such as a surface scrape or abrasion, are healed promptly. However, in individuals with certain clinical disorders, such as diabetic keratopathy, basement membrane dystrophies, neuropathies, and infections, corneal epithelial defects persist and do not respond to conventional treatment regimens (Sanchez-Thorin 1998). Not only is the rate of corneal re-epithelialization important after injury, the re-normalization of the epithelial cytoarchitecture and re-establishment of the epithelial barrier are paramount (Huang et al 1990).
In order to re-establish the epithelial barrier, cells migrate over the denuded surface of the cornea in a manner that is dependent both on the interaction of the cells with the underlying substrate via cell-extracellular matrix adhesions called hemidesmosomes, and on cell–cell adhesions called desmosomes (Suzuki et al 2003). Regeneration of cell adhesions to reconstitute the epithelial barrier protects the cornea from infectious agents and also is important to prevent the persistence of corneal epithelial fragility that can lead to recurrent erosions (McCartney and Cantu-Crouch 1992).
The wound repair process is intricately linked to a complex inflammatory response that must be precisely regulated to ensure proper healing and optimal visual outcome. Infiltration of inflammatory cells into injured corneal tissue is a hallmark of wound repair (Kenyon 1985). Retardation of epithelial recovery by persistent inflammation, release of enzymatic products from resident corneal cells and infiltrating inflammatory cells, and stimulation by cytokines and chemokines, all contribute to poor re-epithelialization. With regard to the cornea, detailed information on cytokine expression and activity is emerging, and great interest centers around identifying which cytokines and chemokines are induced in the cornea by a particular stimulant or insult (Wakefield and Lloyd 1992; Cubitt et al 1993, 1995).
Although much progress has been made in understanding how the cornea heals, current pharmacological therapies that accelerate and/or promote epithelial healing are severely limited. Clinicians still mainly aim to provide the patient with an environment conducive to healing and rely on the eye’s innate ability to repair itself. Emerging evidence from our laboratory and others shows that thymosin beta 4 (Tβ4) is a novel wound healing agent that promotes corneal repair and decreases inflammation after injury. In this review, we focus on the studies that provide evidence for the potential clinical usage of Tβ4 as a corneal wound healing agent.
Properties of Tβ4
Tβ4 is a 43-amino acid, 4.9 kDa protein originally isolated from bovine thymus (Low et al 1981; Goodall et al 1983; Yu et al 1994). Tβ4 is the major monomeric actin-sequestering peptide in cells and can depolymerize F-actin. For example, it has been found to depolymerize cystic fibrosis-derived sputum actin in both a dose-dependent and a time-dependent manner (Rubin et al 2006). Tβ4 influences T cell differentiation (Hu et al 1981; Low and Goldstein 1984). It has no signal sequence (Gondo et al 1987) but is found in serum (Naylor et al 1984; Weller et al 1988). Tβ4 does not appear to bind to either heparin or other extracellular matrix molecules, suggesting it can rapidly diffuse throughout tissue compartments.
Tβ4 is an ubiquitous polypeptide, highly conserved across species, and is found at concentrations of 1 × 10−5 to 5.6 × 10−1 M in a variety of tissues and cell types, yet, no receptors for the protein have been identified (Hannappel et al 1982; Hannappel and Leibold 1985; Hannappel and van Kampen 1987). A recent study suggests that internalization of exogenous Tβ4 is essential for its subsequent cellular functions (Ho et al 2007).
Previous work identified Tβ4 as an induced gene in endothelial cells undergoing differentiation in vitro (Grant et al 1995). Tβ4 is active for endothelial cell and keratinocyte migration in vitro and for angiogenesis in vivo (Malinda et al 1997; Malinda et al 1999). Tβ4 levels are highest in platelets and polymorphonuclear neutrophilic leukocytes (PMN), which are among the first formed elements and cells, respectively, to enter a wound and release their factors, some of which recruit additional cells to the wound site (Cassimeris et al 1992). Although the mechanism(s) of action of exogenous Tβ4 on wound repair remains unclear, the high levels of Tβ4 present in human wound fluid (13 μg/ml) suggest its importance in wound healing (Frohm et al 1996). Tβ4 promotes cardiomyocyte migration, survival, and repair after experimental myocardial infarction, suggesting its potential as a new therapeutic target in the setting of acute myocardial damage (Bock-Marquette et al 2004). It is interesting to note that Tβ4 does not have any effect on cell proliferation (Leeanansaksiri et al 2004; Huang et al 2006; Sosne et al 2006).
In addition to its effects on wound healing, the anti-inflammatory properties of Tβ4 are beginning to be elucidated. Young et al (1999) reported that Tβ4 inhibited PMN chemotaxis to the bacterial chemoattractant, N-for-myl-methionyl-leucyl-phenylalanine (fMLP). Whether Tβ4 exerts its effects on PMN directly or indirectly is an intriguing question. Other studies showed that the activation-responsive expression of the lymph-specific form of Tβ4 may be one mechanism by which dendritic epidermal T cells, and possibly other intraepithelial lymphocytes, down-regulate local inflammation (Girardi et al 2003). In a separate study, Tβ4 lowered circulating levels of inflammatory cytokines and intermediates following LPS administration in vivo (Badamchian et al 2003). Additionally, Tβ4 levels rapidly disappeared in the blood following LPS administration or during septic shock, suggesting that it may be involved in early events leading to activation of the inflammatory cascade and ultimately the clinical sequelae of sepsis.
Tβ4 stimulates corneal epithelial cell migration and wound healing
Two major epithelial cell responses to wounding are cell migration to cover the wound bed, and cell proliferation to re-epithelialize the wound. We and others have shown that while not affecting cell proliferation, Tβ4 significantly enhances the migration of endothelial cells, keratinocytes, tumor cells, and corneal epithelial cells (Sosne et al 2001, 2007; Moon et al 2006; Philp et al 2006). It has been proposed that Tβ4 may promote migration via its upregulation of zyxin expression, a protein that regulates the actin cytoskeleton (Moon et al 2006). Tβ4 promoted full thickness dermal wound repair in normal, steroid-treated and diabetic animal models (Malinda et al 1999; Philp et al 2003). These findings suggest that Tβ4 may be useful in promoting corneal wound healing in healthy individuals as well as in people with healing-impaired pathologies like diabetes.
Because diabetic retinopathy (DR) corneas have delayed wound healing (Kabosova et al 2003), we investigated the expression of Tβ4, a potent epithelial cell migration stimulator, in DR corneas. Human DR corneas were analyzed by gene microarray and quantitative RT-PCR and were found to express significantly less Tβ4 compared to normal corneas (Saghizadeh et al 2006). We hypothesize that reduced expression of Tβ4 may contribute to delayed wound healing in DR corneas. These findings may have important clinical relevance in the treatment of complications stemming from diabetic keratopathy.
In addition to systemic diseases that manifest in the cornea such as diabetic keratopathy, other commonly seen corneal wounds can range from simple epithelial scrape wounds, recurrent erosions, persistent epitheliopathies post-refractive surgery, to severe inflammatory reactions such as seen in alkali injury. Tβ4 accelerated the re-epithelialization of corneal wounds in both heptanol debridement and alkali-burn animal models (Sosne et al 2001, 2002). Corneal alkali injury is marked by a massive PMN infiltration and inflammatory response characterized by over-expression of pro-inflammatory cytokines/chemokines and matrix-metalloproteinases (MMPs), much more extreme than that seen in the setting of scrape injury (Wagoner, 1997; Kenyon et al 1979; Foster et al 1982). The mouse alkali burn model mimics many aspects of the injury seen in humans by clinical slit-lamp and histopathological criteria. Slit-lamp observations of mouse eyes with alkali injury showed that 70% had readily apparent hyphema and total corneal opacification. In contrast 20% of alkali-injured eyes treated with Tβ4 exhibited the same characteristics. The overall anatomical integrity of the anterior segment in the Tβ4-treated eyes was markedly more normal in appearance, providing evidence that Tβ4 treatment improves corneal healing and clarity following alkali injury (Sosne et al 2005).
Corneal epithelial wounds cannot heal properly without the re-establishment of cell attachment to the underlying connective tissue ie, basement membrane. Hemidesmosomes, specialized adhesion junctions present along the basal cell membrane of the basal cells of stratified squamous epithelia, are involved in the adherence of the basal cells to the basement membrane (Susi et al 1967; Jones et al 1994). Heptanol or alkali-burned corneal epithelial cells treated with Tβ4 showed more hemidesmosomal adhesions to the basement membrane, and less widening of the space between epithelium and basement membrane. Laminin-5 is a major glycoprotein of the basement membrane underlying corneal epithelial cells. It plays a central role in both epithelial cell migration and in adhesion, and is associated with hemidesmosomes (Larjava et al 1993). In cultured corneal epithelial cells and in mouse cornea wounded by scraping, topical Tβ4 treatment resulted in increased laminin-5 expression (Sosne et al 2002). This property of Tβ4 has important clinical implications, since it could be utilized in the treatment of recurrent erosions or other situations in which corneal epithelial cell adhesion to the basement membrane is impaired.
As an essential step in the cascade of cellular events culminating in wound healing, epithelial cells participate in extracellular matrix synthesis and remodeling (Lu et al 2001; Santoro and Gaudino 2005). Human MMPs are a family of more than 20 zinc-dependent endopeptidases that upon activation degrade both matrix and non-matrix proteins as part of key rate-limiting steps in tissue repair and remodeling (Nagase et al 2006). Tβ4 treatment modulates MMP expression in several epithelial models (Sosne et al 2005Sosne et al 2007; Philp et al 2006). The majority of MMPs is secreted from the cell as non-catalytic zymogens (pro-MMPs) and is activated via removal of the inhibitory propeptides by proteinases such as thrombin, plasmin, trypsin, and other activated MMPs. Studies suggest that part of the wound healing activity of Tβ4 may be related to its ability to transiently increase MMP activity (MMP-1, -2, and -9) via its central actin-binding domain (Philp et al 2006).
Using an in vitro model of corneal epithelial cell scrape wound healing we showed that blocking MMP activity with specific or broad-spectrum inhibitors decreased Tβ4-mediated epithelial cell migration. This suggests that MMP catalytic activity is necessary for Tβ4 promotion of epithelial cell migration (Sosne et al 2007). Alterations in MMP expression are linked to improper corneal wound healing and the formation of persistent epithelial defects and chronic corneal ulcers (Fini et al 1996). Tβ4 differentially regulates the expression of MMPs in many tissues, and also regulates the MMP/TIMP balance in the cornea. Thus, it is plausible to hypothesize that Tβ4 may promote corneal repair and matrix remodeling following wounding by modulating MMP expression and activity.
Tβ4 modulates corneal inflammation
Many studies have contributed information regarding the roles of cytokine and chemokine expression and activity in the post-wound corneal inflammatory response in a wide array of clinical pathologies (Gillitzer and Goebeler 2001; Wilson et al 2003; Agrawal and Tsai 2003; Stramer et al 2004). For example, in chemically injured corneal epithelial cells, the levels of pro-inflammatory cytokines and chemokines are upregulated (Planck et al 1997; Sotozono et al 1997; Sosne et al 2002), and dry eye stimulates the expression of tumour necrosis factor-alpha (TNF-α) in mice (Luo et al 2004). Corneal epithelial monolayers infected with Pseudomonas aeruginosa demonstrated increased expression and secretion of IL-6, IL-8, and TNF-α (Zhang et al 2005). IL-6 has been associated with enhanced corneal epithelial cell migration (Wang et al 1994; Nakamura and Nishida 1999).
In the first ocular studies to provide evidence that Tβ4-treatment accelerates in vivo wound healing and modulates corneal cytokine production, we showed in the rat corneal epithelial debridement model that mRNA transcripts for IL-1β and IL-6 were increased in Tβ4-treated corneas after injury. Additionally, topical Tβ4 treatment after alkali injury down-regulated the expression of the potent PMN chemoattractants, MIP-2 and KC, in the murine cornea. We suggested that these cytokines may be involved in corneal inflammation and wound healing, and that the decreased corneal chemokine expression may be responsible for the observed decreased PMN infiltration.
TNF-alpha is a potent pro-inflammatory mediator that influences wound healing and apoptotic cell death (Zhang et al 2004). TNF-α stimulation activates transcription factors including nuclear factor kappa B (NFκB) (Baud and Karin 2001; Hanada and Yoshimura 2002; Ritchie et al 2004). NFκB dimers are maintained in an inactivated state in the cytoplasm by a family of inhibitory proteins, the IκBs. IκB can be phosphorylated following cellular stimulation, resulting in its degradation and release from the NFκB dimer. Activatied NFκB translocates to the nucleus where it binds to κB enhancer elements of a wide panel of target genes (Karin and Ben-Neriah 2000). Because of its ability to regulate the expression of inflammatory genes, NFκB is believed to play a major role in the inflammatory process (Hayden and Ghosh 2004).
In cultured human corneal epithelial cells stimulated with TNF-α, Tβ4 treatment significantly decreased nuclear NFκB protein levels, NFκB activity, and p65 subunit phosphorylation. The nuclear translocation of NFκB was also inhibited. Although there are many inflammatory signaling pathways, we hypothesize that Tβ4 mediates NFκB inflammatory signaling pathways in the cornea based on our findings. These observations have important clinical implications for the potential role of Tβ4 as a corneal anti-inflammatory agent.
Tβ4 inhibits corneal epithelial cell apoptosis
Evidence that Tβ4 functions as an anti-apoptotic agent is mounting. HeLa cells that overexpressed Tβ 4 showed a higher growth rate and a lower percentage of basal apoptosis compared to control HeLa cells. In addition, the overexpressing cells were more resistant to paclitaxel-induced cell death (Oh et al 2006). The death of human corneal epithelial cells (HCET) induced by FasL or by hydrogen peroxide was significantly inhibited by Tβ4 treatment. In this study it was observed that the internalization of exogenous Tβ4 was essential for its anti-apoptotic activity in human corneal epithelial cells (Ho et al 2007). Resistance to FasL-induced apoptosis was also achieved in SW480 colon carcinoma cells that overexpressed Tβ4 (Hsiao et al 2006). Using an in vitro culture model, we demonstrated that Tβ4 suppressed ethanol-induced corneal epithelial cell apoptosis via the inhibition of caspases and suppression of bcl-2 release from mitochondria (Sosne et al 2004). In cultured corneal and conjunctival epithelium, Tβ4 did not protect cells from benzalkonium chloride-induced inhibition of proliferation, but apoptosis was significantly inhibited (Sosne et al 2006).
Regarding the mechanism by which Tβ4 exerts its anti-apoptotic activity, it has been suggested that the reduction of early cell death initiation signals, such as the phosphorylation of c-Jun, may prevent apoptosis of neurons (Choi et al 2006). Additionally, it has been demonstrated that Tβ4 promotes survival of cardiomyocytes through the formation of a functional complex with PINCH and integrin-linked kinase, resulting in activation of the survival kinase Akt (Bock-Marquette et al 2004).
Future directions
The mounting evidence suggesting the use of Tβ4 as a novel corneal wound healing and anti-inflammatory agent presents an exciting new potential therapy for practicing ophthalmologists. The plethora of clinical entities related to retarded corneal wound healing present significant challenges for the practicing ophthalmologist. Tβ4, a ubiquitous, naturally occurring molecule, has been demonstrated to promote corneal re-epithelialization, reduce inflammation and inhibit apoptosis. From routine corneal injuries such as abrasions and recurrent erosions to more severe inflammatory-mediated pathologies, ophthalmologists need an agent that can quickly promote corneal healing and properly modulate the inflammatory response.
More basic science studies focused on the mechanisms of action of Tβ4 are needed to help guide future clinical applications. For example, it is interesting to speculate whether the anti-apoptotic properties of Tβ4 could help to preserve tissue after acute injury or for corneal transplantation. Additionally, Tβ4 may be useful as an adjuvant therapy to BAK-containing eye drops to prevent the adverse ocular surface side effects seen with many anti-glaucoma medications. Regarding the anti-inflammatory properties of Tβ4, a wide array of clinical entities such as inflammatory keratopathies, corneal graft rejection, infections, uveitis, and dry eye syndromes may be just a few examples of potential therapeutic treatments. In addition to the basic science studies, we believe that the published animal studies showing Tβ4’s efficacy in a variety of models of injury provide a solid basis for testing the efficacy and safety of Tβ4 in well controlled clinical trials and this is presently being planned (http://www.regenerx.com).
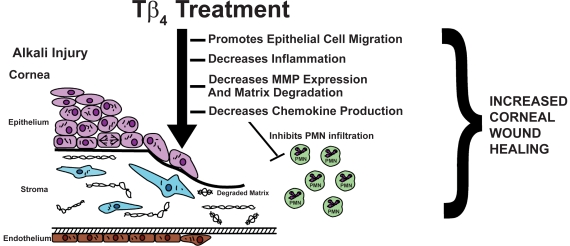
Figure 1.
Tβ4 promotes corneal wound healing. By modulating the corneal inflammatory response and promoting re-epithelialization in response to injury, Tβ4 may be a new a therapeutic option for ophthalmologists treating corneal inflammatory and wound healing disorders.
Table 1.
Properties of thymosin beta 4 in the eye
|
Table 2.
Thymosin β4: Some potential clinical ocular applications
|
References
- Agrawal VB, Tsai RJ. Corneal epithelial wound healing. Indian J Ophthalmol. 2003;51:5–15. [PubMed] [Google Scholar]
- Badamchian M, Fagarasan MO, Danner RL, et al. Thymosin beta(4) reduces lethality and down-regulates inflammatory mediators in endotoxin-induced septic shock. Int Immunopharmacol. 2003;3:1225–33. doi: 10.1016/S1567-5769(03)00024-9. [DOI] [PubMed] [Google Scholar]
- Bock-Marquette A, Saxena M, White MD, et al. Thymosin beta 4 activates integrin-linked kinase and promotes cardiac cell migration, survival and cardiac repair. Nature. 2004;432:466–72. doi: 10.1038/nature03000. [DOI] [PubMed] [Google Scholar]
- Cassimeris L, Safer D, Nachmias VT, et al. Thymosin beta 4 sequesters the majority of G-actin in resting human polymorphonuclear leukocytes. J Cell Biol. 1992;119:1261–70. doi: 10.1083/jcb.119.5.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi SY, Kim DK, Eun B, et al. Anti-apoptotic function of thymosin-beta in developing chick spinal motoneurons. Biochem Biophys Res Commun. 2006;346:872–8. doi: 10.1016/j.bbrc.2006.05.207. [DOI] [PubMed] [Google Scholar]
- Cubitt CL, Tang Q, Monteiro CA, et al. IL-8 gene expression in cultures of human corneal epithelial cells and keratocytes. Invest Ophthalmol Vis Sci. 1993;34:3199–206. [PubMed] [Google Scholar]
- Cubitt CL, Lausch RN, Oakes JE. Differences in interleukin-6 gene expression between cultured human corneal epithelial cells and keratocytes. Invest Ophthalmol Vis Sci. 1995;36:330–6. [PubMed] [Google Scholar]
- Fini ME, Parks WC, Rinehart WB, et al. Role of matrix metalloproteinases in failure to re-epithelialize after corneal injury. Am J Pathol. 1996;149:1287–302. [PMC free article] [PubMed] [Google Scholar]
- Frohm M, Gunne H, Bergman AC, et al. Biochemical and antibacterial analysis of human wound and blister fluid. Eur J Biochem. 1996;237:86–92. doi: 10.1111/j.1432-1033.1996.0086n.x. [DOI] [PubMed] [Google Scholar]
- Gillitzer R, Goebeler M. Chemokines in cutaneous wound healing. J Leukoc Biol. 2001;69:513–21. [PubMed] [Google Scholar]
- Gipson IK, Inatomi T. Extracellular matrix and growth factors in corneal wound healing. Curr Opin Ophthalmol. 1995;6:3–10. doi: 10.1097/00055735-199508000-00002. [DOI] [PubMed] [Google Scholar]
- Girardi M, Sherling MA, Filler RB, et al. Anti-inflammatory effects in the skin of thymosin-beta 4 splice-variants. Immunology. 2003;109:1–7. doi: 10.1046/j.1365-2567.2003.01616.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gondo H, Kudo J, White JW, et al. Differential expression of the human thymosin-beta 4 gene in lymphocytes, macrophages, and granulocytes. J Immunol. 1987;139:3840–8. [PubMed] [Google Scholar]
- Goodall GJ, Hempstead JL, Morgan JI. Production and characterization of antibodies to thymosin beta 4. J Immunol. 1983;131:821–5. [PubMed] [Google Scholar]
- Grant DS, Rose W, Yaen C, et al. Thymosin beta 4 enhances endothelial cell differentiation and angiogenesis. Angiogenesis. 1999;3:125–35. doi: 10.1023/a:1009041911493. [DOI] [PubMed] [Google Scholar]
- Hanada T, Yoshimura A. Regulation of cytokine signaling and inflammation. Cytokine Growth Factor Rev. 2002;13:413–21. doi: 10.1016/s1359-6101(02)00026-6. [DOI] [PubMed] [Google Scholar]
- Hannappel E, Xu GJ, Morgan J, et al. Thymosin beta 4: a ubiquitous peptide in rat and mouse tissues. Proc Natl Acad Sci USA. 1982;79:2172–5. doi: 10.1073/pnas.79.7.2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannappel E, Leibold W. Biosynthesis rates and content of thymosin beta 4 in cell lines. Arch Biochem Biophys. 1985;240:236–41. doi: 10.1016/0003-9861(85)90028-1. [DOI] [PubMed] [Google Scholar]
- Hannappel E, van Kampen M. Determination of thymosin beta 4 in human blood cells and serum. J Chromatogr. 1987;397:279–85. doi: 10.1016/s0021-9673(01)85010-x. [DOI] [PubMed] [Google Scholar]
- Hayden MS, Ghosh S. Signaling to NF-kappaB. Genes Dev. 2004;18:2195–224. doi: 10.1101/gad.1228704. [DOI] [PubMed] [Google Scholar]
- Ho JH, Chuang CH, Ho CY, et al. Internalization is essential for the antiapoptotic effects of exogenous thymosin beta-4 on human corneal epithelial cells. Invest Ophthalmol Vis Sci. 2007;48:27–33. doi: 10.1167/iovs.06-0826. [DOI] [PubMed] [Google Scholar]
- Hsiao HL, Wang WS, Chen PM, et al. Overexpression of thymosin beta-4 renders SW480 colon carcinoma cells more resistant to apoptosis triggered by FasL and two topoisomerase II inhibitors via down-regulating Fas and upregulating Survivin expression, respectively. Carcinogenesis. 2006;27:936–44. doi: 10.1093/carcin/bgi316. [DOI] [PubMed] [Google Scholar]
- Hu SK, Low TL, Goldstein AL. Modulation of terminal deoxynucleotidyl transferase activity by thymosin. Mol Cell Biochem. 1981;41:49–58. doi: 10.1007/BF00225296. [DOI] [PubMed] [Google Scholar]
- Huang AJ, Tseng SC, Kenyon KR. Alteration of epithelial paracellular permeability during corneal epithelial wound healing. Invest Ophthalmol Vis Sci. 1990;31:429–35. [PubMed] [Google Scholar]
- Huang WQ, Wang BH, Wang QR. Thymosin beta4 and AcSDKP inhibit the proliferation of HL-60 cells and induce their differentiation and apoptosis. Cell Biol Int. 2006;30:514–20. doi: 10.1016/j.cellbi.2006.01.009. [DOI] [PubMed] [Google Scholar]
- Jones JC, Asmuth J, Baker SE, et al. Hemidesmosomes: extra-cellular matrix/intermediate filament connectors. Exp Cell Res. 1994;213(1):1–11. doi: 10.1006/excr.1994.1166. [DOI] [PubMed] [Google Scholar]
- Kabosova A, Kramerov AA, Aoki AM, et al. Human diabetic corneas preserve wound healing, basement membrane, integrin and MMP-10 differences from normal corneas in organ culture. Exp Eye Res. 2003;77:211–7. doi: 10.1016/s0014-4835(03)00111-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karin M, Ben-Neriah Y. Phosphorylation meets ubiquitination: the control of NF-[kappa]B activity. Annu Rev Immunol. 2000;18:621–63. doi: 10.1146/annurev.immunol.18.1.621. [DOI] [PubMed] [Google Scholar]
- Kenyon KR. Inflammatory mechanisms in corneal ulceration. Trans Am Ophthalmol Soc. 1985;83:610–63. [PMC free article] [PubMed] [Google Scholar]
- Larjava H, Salo T, Haapasalmi K, et al. Expression of integrins and basement membrane components by wound keratinocytes. J Clin Invest. 1993;92:1425–35. doi: 10.1172/JCI116719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeanansaksiri W, DeSimone SK, Huff T, et al. Thymosin beta 4 and its N-terminal tetrapeptide, AcSDKP, inhibit proliferation, and induce dysplastic, non-apoptotic nuclei and degranulation of mast cells. Chem Biodivers. 2004;1:1091–100. doi: 10.1002/cbdv.200490081. [DOI] [PubMed] [Google Scholar]
- Lindsey ML. Novel strategies to delineate matrix metalloproteinase (MMP)-substrate relationships and identify targets to block MMP activity. Mini Rev Med Chem. 2006;6:1243–8. doi: 10.2174/138955706778742777. [DOI] [PubMed] [Google Scholar]
- Low TL, Hu SK, Goldstein AL. Complete amino acid sequence of bovine thymosin beta 4: a thymic hormone that induces terminal deoxynucleotidyl transferase activity in thymocyte populations. Proc Natl Acad Sci USA. 1981;78:1162–6. doi: 10.1073/pnas.78.2.1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Low TL, Goldstein AL. Thymosins: structure, function and therapeutic applications. Thymus. 1984;6:27–42. [PubMed] [Google Scholar]
- Lu L, Reinach PS, Kao WW. Corneal epithelial wound healing. Exp Biol Med (Maywood) 2001;226:653–64. doi: 10.1177/153537020222600711. [DOI] [PubMed] [Google Scholar]
- Luo L, Li DQ, Doshi A, et al. Experimental dry eye stimulates production of inflammatory cytokines and MMP-9 and activates MAPK signaling pathways on the ocular surface. Invest Ophthalmol Vis Sci. 2004;45:4293–301. doi: 10.1167/iovs.03-1145. [DOI] [PubMed] [Google Scholar]
- Malinda KM, Goldstein AL, Kleinman HK. Thymosin beta 4 stimulates directional migration of human umbilical vein endothelial cells. FASEB J. 1997;11:474–81. doi: 10.1096/fasebj.11.6.9194528. [DOI] [PubMed] [Google Scholar]
- Malinda KM, Sidhu GS, Mani H, et al. Thymosin beta 4 accelerates wound healing. J Invest Dermatol. 1999;113:364–68. doi: 10.1046/j.1523-1747.1999.00708.x. [DOI] [PubMed] [Google Scholar]
- McCartney MD, Cantu-Crouch D. Rabbit corneal epithelial wound repair: tight junction reformation. Curr Eye Res. 1992;11:15–24. doi: 10.3109/02713689209069163. [DOI] [PubMed] [Google Scholar]
- Meek KM, Leonard DW, Connon CJ, et al. Transparency, swelling and scarring in the corneal stroma. Eye. 2003;17:927–36. doi: 10.1038/sj.eye.6700574. [DOI] [PubMed] [Google Scholar]
- Moon HS, Even-Ram S, Kleinman HK, et al. Zyxin is upregulated in the nucleus by thymosin β4 in SiHa cells. Exp Cell Res. 2006;17:3425–31. doi: 10.1016/j.yexcr.2006.07.021. [DOI] [PubMed] [Google Scholar]
- Nakamura M, Nishida T. Differential effects of epidermal growth factor and interleukin 6 on corneal epithelial cells and vascular endothelial cells. Cornea. 1999;18:452–8. doi: 10.1097/00003226-199907000-00011. [DOI] [PubMed] [Google Scholar]
- Naylor PH, McClure JE, Spangelo BL, et al. Immunochemical studies on thymosin: radioimmunoassay of thymosin beta 4. Immunopharmacology. 1984;7:9–16. doi: 10.1016/0162-3109(84)90003-1. [DOI] [PubMed] [Google Scholar]
- Oh SY, Song JH, Gil JE, et al. ERK activation by thymosin-beta-4 (TB4) overexpression induces paclitaxel-resistance. Exp Cell Res. 2006;312:1651–7. doi: 10.1016/j.yexcr.2006.01.030. [DOI] [PubMed] [Google Scholar]
- Philp D, Badamchian M, Scheremeta B, et al. Thymosin beta 4 and a synthetic peptide containing its actin-binding domain promote dermal wound repair in db/db diabetic mice and in aged mice. Wound Repair Regen. 2003;11:19–24. doi: 10.1046/j.1524-475x.2003.11105.x. [DOI] [PubMed] [Google Scholar]
- Philp D, Nguyen M, Scheremeta B, et al. Thymosin β4 increases hair growth by activation of hair follicle stem cells. FASEB J. 2004;18:385–7. doi: 10.1096/fj.03-0244fje. [DOI] [PubMed] [Google Scholar]
- Philp D, Scheremeta B, Sibliss K, et al. Thymosin beta4 promotes matrix metalloproteinase expression during wound repair. J Cell Physiol. 2006;208:195–200. doi: 10.1002/jcp.20650. [DOI] [PubMed] [Google Scholar]
- Planck SR, Rich LF, Ansel JC, et al. Trauma and alkali burns induce distinct patterns of cytokine gene expression in the rat cornea. Ocul Immunol Inflamm. 1997;5:95–100. doi: 10.3109/09273949709085057. [DOI] [PubMed] [Google Scholar]
- Ritchie MH, Fillmore RA, Lausch RN, et al. A role for NF-kappa B binding motifs in the differential induction of chemokine gene expression in human corneal epithelial cells. Invest Ophthalmol Vis Sci. 2004;45:2299–305. doi: 10.1167/iovs.03-0367. [DOI] [PubMed] [Google Scholar]
- Rubin BK, Kater AP, Goldstein AL. Thymosin beta 4 sequesters actin in cystic fibrosis sputum and decreases sputum cohesivity in vitro. Chest. 2006;130:1433–40. doi: 10.1378/chest.130.5.1433. [DOI] [PubMed] [Google Scholar]
- Saghizadeh M, Kramerov AA, Tajbakhsh J, et al. Proteinase and growth factor alterations revealed by gene microarray analysis of human diabetic corneas. Invest Ophthalmol Vis Sci. 2006;46:3604–15. doi: 10.1167/iovs.04-1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez-Thorin JC. The cornea in diabetes mellitus. Int Ophthalmol Clin. 1998;38:19–36. [PubMed] [Google Scholar]
- Santoro MM, Gaudino G. Cellular and molecular facets of keratinocyte reepithelization during wound healing. Exp Cell Res. 2005;304:274–86. doi: 10.1016/j.yexcr.2004.10.033. [DOI] [PubMed] [Google Scholar]
- Sosne G, Chan CC, Thai K, et al. Thymosin beta 4 promotes corneal wound healing and modulates inflammatory mediators in vivo. Exp Eye Res. 2001;72:605–8. doi: 10.1006/exer.2000.0985. [DOI] [PubMed] [Google Scholar]
- Sosne G, Szliter EA, Barrett R, et al. Thymosin beta 4 promotes corneal wound healing and decreases inflammation in vivo following alkali injury. Exp Eye Res. 2002;74:293–9. doi: 10.1006/exer.2001.1125. [DOI] [PubMed] [Google Scholar]
- Sosne G, Siddiqi A, Kurpakus-Wheater M. Thymosin beta-4 inhibits corneal epithelial cell apoptosis after ethanol exposure in vitro. Invest Ophthalmol Vis Sci. 2004;45:1095–100. doi: 10.1167/iovs.03-1002. [DOI] [PubMed] [Google Scholar]
- Sosne G, Christopherson PL, Barrett RP, et al. Thymosin-beta 4 modulates corneal matrix metalloproteinase levels and polymorphonuclear cell infiltration after alkali injury. Invest Ophthalmol Vis Sci. 2005;46:2388–95. doi: 10.1167/iovs.04-1368. [DOI] [PubMed] [Google Scholar]
- Sosne G, Albeiruti AR, Hollis B, et al. Thymosin beta4 inhibits benzalkonium chloride-mediated apoptosis in corneal and conjunctival epithelial cells in vitro. Exp Eye Res. 2006;83:502–7. doi: 10.1016/j.exer.2006.02.001. [DOI] [PubMed] [Google Scholar]
- Qiu P, Kurpakus-Wheater M, Sosne G. Matrix metalloproteinase activity is necessary for thymosin beta 4 promotion of epithelial cell migration. J Cell Physiol. 2007;212:165–73. doi: 10.1002/jcp.21012. [DOI] [PubMed] [Google Scholar]
- Sotozono C, He J, Matsumoto Y, et al. Cytokine expression in the alkali-burned cornea. Curr Eye Res. 1997;16:670–6. doi: 10.1076/ceyr.16.7.670.5057. [DOI] [PubMed] [Google Scholar]
- Suzuki K, Saito J, Yanai R, et al. Cell-matrix and cell-cell interactions during corneal epithelial wound healing. Prog Retin Eye Res. 2003;22:113–33. doi: 10.1016/s1350-9462(02)00042-3. [DOI] [PubMed] [Google Scholar]
- Verkman AS. Role of aquaporin water channels in eye function. Exp Eye Res. 2003;76:137–43. doi: 10.1016/s0014-4835(02)00303-2. [DOI] [PubMed] [Google Scholar]
- Wagoner MD. Chemical injuries of the eye: current concepts in pathophysiology and therapy. Surv Ophthalmol. 1997;41:275–313. doi: 10.1016/s0039-6257(96)00007-0. [DOI] [PubMed] [Google Scholar]
- Wakefield D, Lloyd A. The role of cytokines in the pathogenesis of inflammatory eye disease. Cytokine. 1992;4:1–5. doi: 10.1016/1043-4666(92)90028-p. [DOI] [PubMed] [Google Scholar]
- Weller FE, Mutchnick MG, Goldstein AL, et al. Enzyme immunoassay measurement of thymosin beta 4 in human serum. J Biol Response Mod. 1988;7:91–6. [PubMed] [Google Scholar]
- Wilson SE, Netto M, Ambrosio R., Jr Corneal cells: chatty in development, homeostasis, wound healing, and disease. Am J Ophthalmol. 2003;136:530–6. doi: 10.1016/s0002-9394(03)00085-0. [DOI] [PubMed] [Google Scholar]
- Young JD, Lawrence AJ, MacLean AG, et al. Thymosin beta 4 sulfoxide is an anti-inflammatory agent generated by monocytes in the presence of glucocorticoids. Nat Med. 1999;5:1424–7. doi: 10.1038/71002. [DOI] [PubMed] [Google Scholar]
- Yu FX, Lin SC, Morrison-Bogorad M, et al. Effects of thymosin beta 4 and thymosin beta 10 on actin structures in living cells. Cell Motil Cytoskeleton. 1994;27:13–25. doi: 10.1002/cm.970270103. [DOI] [PubMed] [Google Scholar]
- Zhang S, Lin ZN, Yang CF, et al. Suppressed NF-kappaB and sustained JNK activation contribute to the sensitization effect of parthenolide to TNF-alpha-induced apoptosis in human cancer cells. Carcinogenesis. 2004;25:2191–9. doi: 10.1093/carcin/bgh234. [DOI] [PubMed] [Google Scholar]
- Zhang J, Wu XY, Yu FS. Inflammatory responses of corneal epithelial cells to Pseudomonas aeruginosa infection. Curr Eye Res. 2005;30:527–34. doi: 10.1080/02713680590968150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao M, Song B, Pu J, et al. Direct visualization of a stratified epithelium reveals that wounds heal by unified sliding of cell sheets. FASEB J. 2003;17:397–406. doi: 10.1096/fj.02-0610com. [DOI] [PMC free article] [PubMed] [Google Scholar]