Abstract
AIM: To compare the hemostatic efficacy and safety of two mechanical endoscopic methods: endoscopic band ligation (EBL) and endoscopic hemoclip placement (EHP) in patients with actively bleeding Mallory-Weiss syndrome (MWS).
METHODS: A prospective randomized study to compare the efficacy and safety of EHP with EBL was performed from January 2002 to August 2005. Forty-one patients with active bleeding from MWS were treated with EHP (n = 21) or EBL (n = 20).
RESULTS: There were no significant differences between groups with respect to clinical and endoscopic characteristics. The mean number of hemoclips applied was 3.2 ± 1.5 and the mean number of bands applied was 1.2 ± 0.4. Primary hemostasis was achieved in all patients. Recurrent bleeding was observed in one patient from the EHP group and two from the EBL group. Patients with recurrent bleeding were treated by the same modality as at randomization and secondary hemostasis was achieved in all. There were no significant differences between the two groups in total transfusion amount or duration of hospital stay. No complications or bleeding-related death resulted.
CONCLUSION: EHP and EBL are equally effective and safe for the management of active bleeding in patients with Mallory-Weiss syndrome, even in those with shock or comorbid diseases.
Keywords: Mallory-Weiss syndrome, Hemostasis, Endoscopic band ligation, Endoscopic clipping
INTRODUCTION
Mallory-Weiss syndrome (MWS), vomiting-induced mucosal lacerations in the region of the gastroesophageal junction, is one cause of nonvariceal upper gastrointestinal (UGI) bleeding and its incidence is considered to be 5% to 15%[1]. In most cases, MWS-related bleeding requires no intervention other than hemodynamic support[2]. However, some patients may require intensive care[3], especially those with risk factors such as evidence of active bleeding (for example, fresh blood hematemesis and hemodynamic instability), presence of stigmata of recurrent bleeding (such as visible vessel and adherent clots), and comorbid diseases or bleeding diathesis. Surgery or other therapeutic approaches such as balloon tamponade of the esophagus, transcatheter arterial embolization, and systemic or selective arterial infusion of vasopressin have been used to control active bleeding in patients with MWS[4–7]. In recent decades, endoscopic treatment has been the treatment of choice[8]. Various endoscopic techniques, mainly consisting of endoscopic coagulation or injection, have been used in the management of patients with MWS at high risk for recurrent bleeding[9–12]. However, injection hemostasis may be incomplete for patients with a large and/or long plexuses of vessels and coagulation has the risk of producing transmural injury and perforation due to relatively thin esophageal wall[13]. Mechanical endoscopic methods have recently become one of the therapeutic options for treating patients with actively bleeding MWS[13–20]. Among the mechanical methods, endoscopic band ligation (EBL) and endoscopic hemoclip placement (EHP) both has merits and problems related to the hemostatic mechanism and technical procedure itself. However, there have been few studies comparing the hemostatic efficacy of different mechanical endoscopic methods in the treatment of actively bleeding MWS. Therefore, this prospective randomized study was carried out to compare the hemostatic efficacy and safety of EBL with EHP in the treatment of actively bleeding MWS.
MATERIALS AND METHODS
Subjects
Among patients undergoing upper endoscopy at the gastrointestinal endoscopy center of Uijeongbu St Mary’s Hospital from January 2002 to August 2005 because of acute UGI bleeding, all consecutive patients with endoscopically verified MWS (defined as a mucosal tear or laceration near the esophagogastric junction with active bleeding, either spurting or oozing) were considered for inclusion in the study. Written informed consent for endoscopy and participation in the study was obtained from patients or near relatives before the procedure. This research was carried out in accordance with the Helsinki declaration.
After receiving basic life support, all patients underwent endoscopy within 12 h of the onset of UGI bleeding. Patients were excluded if they were unable or unwilling to give informed consent for endoscopic therapy, if active bleeding was not present at endoscopy, or if more than one source of bleeding was identified. Patients with old adherent clots and clean-based longitudinal mucosal tears near the esophagogastric junction as the only possible origin of bleeding were treated conservatively. All patients’ clinical characteristics, including age, gender, presenting symptoms, alcohol use, blood pressure, hemoglobin level, coagulopathy, and comorbid diseases, were recorded. Shock was defined as a systolic blood pressure of less than 90 mmHg and a pulse rate greater than 100 beats/min, accompanied by pallor or cold sweating.
Therapy
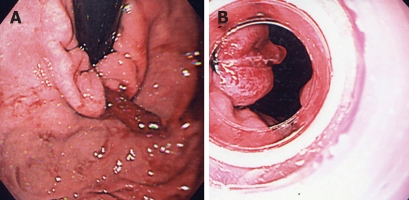
Forty-one patients were randomized to undergo EBL (n = 20) or EHP (n = 21) by concealed allocation determined according to a table of random numbers. All diagnostic and therapeutic endoscopic procedures were performed by members of the research team of four staff gastroenterologists. They did not participate in the postprocedure care of the patients, which was conducted by other physicians. Endoscopic procedures were performed with videoendoscopes (GIF-Q230, GIF-XQ230, Olympus Optical Co. Ltd, Tokyo, Japan). In the EBL group, an endoscopic ligating device (Pneumoactive EVL device; Sumitomo Bakelite Company, Tokyo, Japan) was used with no overtube. After endoscopic identification of the lesion, the endoscope was withdrawn and was reinserted after attachment of the band ligator. After the hood had been placed over the bleeding site, endoscopic suction was activated to draw the bleeding site into the banding cylinder. After suction and band release, a polypoid mass of mucosa 1 cm in diameter was formed and active bleeding stopped immediately (Figure 1). In the EHP group, hemoclips (MDS50, Olympus) were placed with a clip application device (HX-3L, HX-5 LR-1; Olympus). In terms of technique, hemoclips were applied directly on spurting or oozing vessels along with surrounding tissues (Figure 2).
Figure 1.
Endoscopic view of a Mallory-Weiss tear at the cardia of the stomach. A: An actively bleeding vessel ; B: After band placement.
Figure 2.
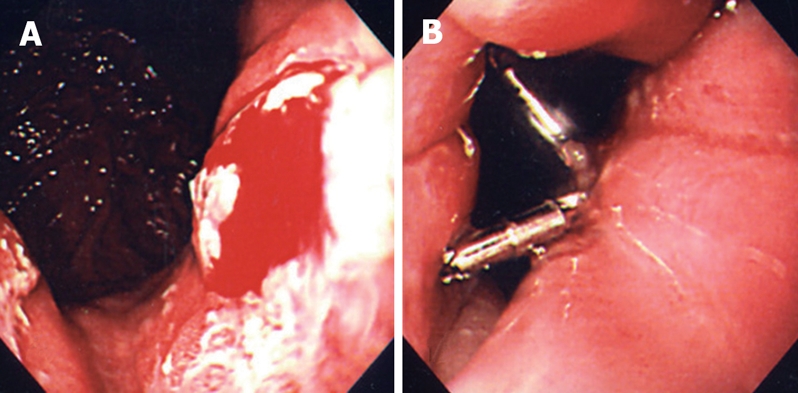
Endoscopic view of a Mallory-Weiss tear at the esophagogastric junction. A: Oozing vessel; B: After hemoclip application to the bleeding vessel.
Once hemostasis was achieved, the bleeding site was observed for at least 1 min. Primary hemostasis was defined as no endoscopic evidence of bleeding during this time after band ligation or after hemoclipping, during the first endoscopic session. Patients who continued to bleed, despite receiving EBL or EHP, were given endoscopic injections of epinephrine. If patients continued to bleed despite endoscopic treatment, we planned to undergo transcatheter arterial embolization or emergency surgery, depending on the status of the patient and/or the volume of blood transfused. After endoscopic treatment, all patients were observed closely. During admission, treatment included partial parenteral nutrition and intravenous administration of histamine H2 receptor antagonists at standard doses. Evidence of recurrent bleeding included the following signs of ongoing bleeding: (1) new hematemesis; (2) fresh blood aspirated via a nasogastric tube; (3) continuous melena with instability of vital signs (systolic blood pressure ≤ 90 mm Hg, heart rate ≥ 100 beats/min, or orthostatic changes in systolic blood pressure of ≥ 20 mmHg or heart rate of ≥ 20 beats/min), or a decrease in hemoglobin level of more than 20 g/L within 24 h of obtaining primary hemostasis. When recurrent bleeding was suspected, endoscopy was performed immediately and the same initial therapeutic modality used at randomization was used. After patients were discharged, the clinical outcome was evaluated by physicians who were blinded to the type of endoscopic treatment and who followed the patients for 30 d including initial hospitalization. Permanent hemostasis was defined as the absence of recurrent bleeding during this period.
To evaluate the efficacy of the two hemostatic procedures, data for each patient were collected during hospitalization and included information on demographics, medical history, presenting symptoms, initial hemodynamic status, laboratory values, rate of primary hemostasis, permanent primary hemostasis rate, number of therapeutic endoscopic sessions, need for emergency operation or transcatheter arterial embolization, bleeding-related deaths, transfusion requirements, and duration of hospitalization.
Statistical analysis
Quantitative data are summarized as the mean ± SD. The Mann-Whitney nonparametric U test was used to compare the mean values of continuous variables and Fisher’s exact test was used for the comparison of discrete variables. P < 0.05 was accepted as indicating statistical significance. The analyses were performed using SPSS version 11.0 for Windows (SPSS Inc., Chicago, IL, USA).
RESULTS
During the study period, 137 patients with MWS tears underwent emergency endoscopy, but only 41 patients (30%) met the entry criteria and were randomized. Clinical and endoscopic characteristics for the patients at entry are outlined in Table 1. No differences were noted between the two groups with respect to age, gender, presenting symptoms, alcohol use, shock, hemoglobin level, coagulopathy, comorbid diseases, number of bleeding points, length of tear, stigmata of bleeding, or locations of the lacerations. Comorbid diseases in the EBL group included liver cirrhosis, coronary artery disease, stroke, and chronic renal failure; in the EHP group, comorbid diseases included liver cirrhosis, pancreatitis, valvular heart disease, and rheumatoid arthritis. However, no differences were noted between the two groups with respect to frequency of having a spurting vessel or oozing. The most common location of the tear was the esophagogastric junction in all patients (23/41, 56%; Table 1).
Table 1.
Clinical characteristics and outcome of patients in endoscopic band ligation (EBL) and endoscopic hemoclip placement (EHP) groups
| EHP | EBL | P value | |
| (n = 21) | (n = 20) | ||
| Age (yr) | 49.5 ± 13.2 | 47.1 ± 11.9 | 0.58 |
| Gender (male/female) | 21/0 | 17/3 | 0.10 |
| Alcohol use | 13 (62%) | 13 (65%) | 1.00 |
| Hematemesis/melena | 21/1 | 20/2 | 0.61 |
| Shock | 3 (14%) | 4 (20%) | 0.70 |
| Hemoglobin level (g/L) | 125 ± 33 | 112 ± 25 | 0.14 |
| Comorbid disease | 9 (43%) | 9 (45%) | 1.00 |
| Number of tears | 1.7 ± 0.9 | 1.4 ± 0.6 | 0.29 |
| Bleeding stigmata | 0.45 | ||
| Spurting vessel | 3 (14%) | 5 (25%) | |
| Oozing vessel | 18 (86%) | 15 (75%) | |
| Tear location | 0.63 | ||
| Distal esophagus | 6 (29%) | 4 (25%) | |
| Esophagogastric junction | 9 (43%) | 14 (75%) | |
| Cardia | 6 (27%) | 2 (10%) | |
| Length of tear (cm) | 2.2 ± 0.6 | 2.1 ± 0.5 | 0.34 |
| Primary outcomes | |||
| Primary hemostasis | 21 (100%) | 20 (100%) | 1.00 |
| First episode of recurrent bleeding | 1 (6%) | 2 (10%) | 0.61 |
| Permanent primary hemostasis | 20 (94%) | 18 (90%) | 0.61 |
| Secondary hemostasis | 1 (100%) | 2 (100%) | 1.00 |
| Other outcomes | |||
| Blood transfusion (mean units) | 2.0 ± 2.5 | 3.3 ± 2.9 | 0.14 |
| Total procedure time (mean min) | 16.7 ± 3.2 | 17.1 ± 2.6 | 0.68 |
| Additional epinephrine injection | 0 | 0 | 1.00 |
| Bleeding-related deaths | 0 | 0 | 1.00 |
| Hospital stay (mean days) | 6.7 ± 5.1 | 7.3 ± 3.3 | 0.20 |
Primary hemostasis was obtained in all patients in each group. In the EBL group, treatment was completed in a single session (mean number of bands 1.2 ± 0.4). A single elastic band was applied in 17 patients; two bands were placed in three patients (Table 1). In the EHP group, the mean number of hemoclips applied was 3.2 ± 1.5. Two patients (10%) in the EBL group and one patient (6%) in the EHP group had recurrent bleeding; this was controlled in all three with endoscopic treatment and no patient required surgery. No differences were noted in primary outcomes including rates of primary hemostasis, recurrent bleeding, and permanent primary hemostasis. No differences were noted in the other secondary outcomes, including the number of endoscopic sessions, total procedure time, the need for additional epinephrine injection, the need for emergency operation or transcatheter arterial embolization, bleeding-related deaths, transfusion requirements, or the duration of hospitalization. No significant complications or adverse events attributable to endoscopic treatment were noted in either group, and no recurrent bleeding was noted in either group during outpatient follow-up.
DISCUSSION
MWS is a relatively common cause of nonvariceal UGI bleeding, in which an abrupt rise in abdominal pressure caused by retching or vomiting induces mucosal tears near the esophagogastric junction[1,2]. Because most patients stop bleeding spontaneously, emergency treatment is reserved for those showing active bleeding[3]. The rate of recurrent bleeding in patients with MWS is also lower than that for other nonvariceal bleeding[8]. However, when bleeding is active and severe, patients require surgical treatment or nonsurgical therapeutic approaches[4,5].
Several endoscopic methods have been used to treat actively bleeding MWS, including injection of different agents, electrocoagulation, application of hemoclips, and band ligation[8,18]. Thermal coagulation or injection therapies have been used successfully to control active bleeding from MWS[10–12,21]. Laine[21] reported that multipolar electrocoagulation significantly improved hemostasis and reduced surgery in patients with active bleeding from MWS and has been associated with few complications. However, repeated coagulation has the risk of producing transmural injury and perforation because the esophagus lacks serosa and is very thin at the tear site[22]. Injection therapy with various agents is an effective, simple, and inexpensive first-line approach[11,12]. Llach et al[11]. Reported that endoscopic injection therapy using epinephrine and polidocanol improved outcomes (rate of recurrent bleeding, hospital stay, and transfusion requirement) compared with supportive measures alone in a prospective, randomized controlled trial. However, injection therapy can produce cardiovascular complications such as ventricular tachycardia and should be avoided in patients with a history of coronary artery disease because of the potential for systemic absorption[23].
EBL, commonly used in variceal bleeding, has also been used to treat nonvariceal bleeding[8]. EBL is technically easier to perform than other methods, with the lesions well viewed under direct pressure and suction from the transparent ligation cap[20]. The use of EBL for treatment of patients with bleeding MWS has been described in several studies[13–15,18,20,24]. Our study also demonstrated high successful rates of primary and permanent hemostasis in such cases.
EHP is acceptable for treating bleeding lesions in nonfibrotic tissues and has advantages over other hemostatic methods because it rarely causes perforation[25]. It is effective in the management of bleeding from a Mallory-Weiss tear[18,19,26]. Compared with cautery or sclerotherapy, it may be a safer option in the management of bleeding from MWS because of the lack of additional tissue damage with endoclips[8,19]. In the event of a deeper extension of the tear with an esophageal perforation, the placement of endoclips can fix both problems simultaneously[27]. EHP has been shown to be an effective alternative treatment in critically ill patients with severe gastrointestinal bleeding[28,29]. Park et al[30] reported that EHP and EBL showed similar efficacy and safety in the management of bleeding gastric Dieulafoy’s lesions. However, there have been no reports comparing the efficacy and safety of EHP with those of EBL for the treatment of active bleeding from MWS.
In our study, EBL and EHP both achieved low rates of recurrent bleeding and high rates of primary hemostasis. The recurrent bleeding was successfully treated using the same method as at randomization. Shock and comorbid diseases were present in four (20%) and nine (45%) patients in the EBL group, respectively; and three (14%) and nine (43%) patients in the EHP group. Despite these adverse factors, primary hemostasis was achieved in all patients. No patient in either group required additional epinephrine injection or advanced invasive therapy such as transcatheter arterial embolization or emergency surgery, and there was no procedure-related complication in either group. Therefore, the results of our study indicate that both EBL and EHP are effective and safe for treatment of patients with actively bleeding MWS, including those with shock, comorbid diseases, and/or coagulopathy.
In conclusion, EBL and EHP are equally safe and effective for the control of active bleeding in patients with hemodynamically unstable MWS and/or combined major diseases. Moreover, after treatment, the frequency of recurrent bleeding is low and the rate of permanent hemostasis is high.
COMMENTS
Background
Mallory-Weiss syndrome (MWS) is a relatively common cause of nonvariceal upper gastrointestinal bleeding. When bleeding is active and severe, patients require treatment. Several endoscopic methods have been used to treat actively bleeding MWS. We aimed to compare the hemostatic efficacy and safety of endoscopic band ligation (EBL) with endoscopic hemoclip placement (EHP) in the treatment of actively bleeding MWS.
Research frontiers
Endoscopic injection of epinephrine is effective treatment for MWS but has higher recurrent bleeding rate. Mechanical endoscopic methods is one of treatment options that are effective and safe for actively bleeding MWS.
Innovations and breakthroughs
EBL and EHP both have merits and problems related to the hemostatic mechanism and technical procedure itself. Although many investigators have reported the usefulness of mechanical endoscopic methods, there have been few studies comparing the hemostatic efficacy of different mechanical endoscopic methods in the treatment of actively bleeding MWS. We showed that both EHP and EBL are effective for MWS. These two methods are also used effectively in patients with hemodynamically unstable MWS or combined diseases.
Applications
This finding provides evidence that EBL or EHP in the management of actively bleeding MWS can be selected depending on physician’s expertise.
Peer review
This is a report designed to compare the efficacy of two different mechanical endoscopic methods in the management of actively bleeding MWS. It is concluded that EBL and EHP are equally safe and effective. After treatment with both, the frequency of recurrent bleeding is low and the rate of permanent hemostasis is high.
Peer reviewer: Kyoichi Adachi, MD, Department of Gastroenterology and Hepatology, Shimane University, School of Medicine Shimane, 89-1 Enya-cho, Izumo-shi Shimane 693-8501, Japan
S- Editor Zhong XY L- Editor Zhong XY E- Editor Zhong XY
References
- 1.Katz PO, Salas L. Less frequent causes of upper gastrointestinal bleeding. Gastroenterol Clin North Am. 1993;22:875–889. [PubMed] [Google Scholar]
- 2.Harris JM, DiPalma JA. Clinical significance of Mallory-Weiss tears. Am J Gastroenterol. 1993;88:2056–2058. [PubMed] [Google Scholar]
- 3.Sugawa C, Benishek D, Walt AJ. Mallory-Weiss syndrome. A study of 224 patients. Am J Surg. 1983;145:30–33. doi: 10.1016/0002-9610(83)90162-9. [DOI] [PubMed] [Google Scholar]
- 4.Welch GH, McArdle CS, Anderson JR. Balloon tamponade for the control of Mallory-Weiss haemorrhage in patients with coagulation defects. Br J Surg. 1987;74:610–611. doi: 10.1002/bjs.1800740723. [DOI] [PubMed] [Google Scholar]
- 5.Fisher RG, Schwartz JT, Graham DY. Angiotherapy with Mallory-Weiss tear. AJR Am J Roentgenol. 1980;134:679–684. doi: 10.2214/ajr.134.4.679. [DOI] [PubMed] [Google Scholar]
- 6.Clark RA. Intraarterial vasopressin infusion for treatment of Mallory-Weiss tears of the esophagogastric junction. AJR Am J Roentgenol. 1979;133:449–451. doi: 10.2214/ajr.133.3.449. [DOI] [PubMed] [Google Scholar]
- 7.Thomas E, Reddy KR. Systemic vasopressin therapy for Mallory-Weiss bleeding. South Med J. 1982;75:691–693. doi: 10.1097/00007611-198206000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Church NI, Palmer KR. Ulcers and nonvariceal bleeding. Endoscopy. 2003;35:22–26. doi: 10.1055/s-2003-36411. [DOI] [PubMed] [Google Scholar]
- 9.Macedo G, Carvalho L, Ribeiro T. Endoscopic sclerotherapy for upper gastrointestinal bleeding due to Mallory-Weiss syndrome. Am J Gastroenterol. 1995;90:1364–1365. [PubMed] [Google Scholar]
- 10.Bharucha AE, Gostout CJ, Balm RK. Clinical and endoscopic risk factors in the Mallory-Weiss syndrome. Am J Gastroenterol. 1997;92:805–808. [PubMed] [Google Scholar]
- 11.Llach J, Elizalde JI, Guevara MC, Pellise M, Castellot A, Gines A, Soria MT, Bordas JM, Pique JM. Endoscopic injection therapy in bleeding Mallory-Weiss syndrome: a randomized controlled trial. Gastrointest Endosc. 2001;54:679–681. doi: 10.1067/mge.2001.119874. [DOI] [PubMed] [Google Scholar]
- 12.Peng YC, Tung CF, Chow WK, Chang CS, Chen GH, Hu WH, Yang DY. Efficacy of endoscopic isotonic saline-epinephrine injection for the management of active Mallory-Weiss tears. J Clin Gastroenterol. 2001;32:119–122. doi: 10.1097/00004836-200102000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Terada R, Ito S, Akama F, Kidogawa H, Kashima K, Yamayoshi T, Ooe H. Mallory-Weiss syndrome with severe bleeding: treatment by endoscopic ligation. Am J Emerg Med. 2000;18:812–815. doi: 10.1053/ajem.2000.18121. [DOI] [PubMed] [Google Scholar]
- 14.Myung SJ, Kim HR, Moon YS. Severe Mallory-Weiss tear after endoscopy treated by endoscopic band ligation. Gastrointest Endosc. 2000;52:99–101. doi: 10.1067/mge.2000.105071. [DOI] [PubMed] [Google Scholar]
- 15.Gunay K, Cabioglu N, Barbaros U, Taviloglu K, Ertekin C. Endoscopic ligation for patients with active bleeding Mallory-Weiss tears. Surg Endosc. 2001;15:1305–1307. doi: 10.1007/s004640000357. [DOI] [PubMed] [Google Scholar]
- 16.Lin LF, Siauw CP, Ho KS, Tung JC. Endoscopic hemoclip treatment of gastrointestinal bleeding. Chang Gung Med J. 2001;24:307–312. [PubMed] [Google Scholar]
- 17.Will U, Seidel T, Bosseckert H. Endoscopic hemoclip treatment for bleeding artificially induced Mallory-Weiss tears. Endoscopy. 2002;34:748. doi: 10.1055/s-2002-33453. [DOI] [PubMed] [Google Scholar]
- 18.Chung IK, Kim EJ, Hwang KY, Kim IH, Kim HS, Park SH, Lee MH, Kim SJ. Evaluation of endoscopic hemostasis in upper gastrointestinal bleeding related to Mallory-Weiss syndrome. Endoscopy. 2002;34:474–479. doi: 10.1055/s-2002-32000. [DOI] [PubMed] [Google Scholar]
- 19.Huang SP, Wang HP, Lee YC, Lin CC, Yang CS, Wu MS, Lin JT. Endoscopic hemoclip placement and epinephrine injection for Mallory-Weiss syndrome with active bleeding. Gastrointest Endosc. 2002;55:842–846. doi: 10.1067/mge.2002.124560. [DOI] [PubMed] [Google Scholar]
- 20.Park CH, Min SW, Sohn YH, Lee WS, Joo YE, Kim HS, Choi SK, Rew JS, Kim SJ. A prospective, randomized trial of endoscopic band ligation vs. epinephrine injection for actively bleeding Mallory-Weiss syndrome. Gastrointest Endosc. 2004;60:22–27. doi: 10.1016/s0016-5107(04)01284-2. [DOI] [PubMed] [Google Scholar]
- 21.Laine L. Multipolar electrocoagulation in the treatment of active upper gastrointestinal tract hemorrhage. A prospective controlled trial. N Engl J Med. 1987;316:1613–1617. doi: 10.1056/NEJM198706253162601. [DOI] [PubMed] [Google Scholar]
- 22.Lum DF, McQuaid K, Lee JG. Endoscopic hemostasis of nonvariceal, non-peptic ulcer hemorrhage. Gastrointest Endosc Clin N Am. 1997;7:657–670. [PubMed] [Google Scholar]
- 23.Stevens PD, Lebwohl O. Hypertensive emergency and ventricular tachycardia after endoscopic epinephrine injection of a Mallory-Weiss tear. Gastrointest Endosc. 1994;40:77–78. doi: 10.1016/s0016-5107(94)70016-8. [DOI] [PubMed] [Google Scholar]
- 24.Higuchi N, Akahoshi K, Sumida Y, Kubokawa M, Motomura Y, Kimura M, Matsumoto M, Nakamura K, Nawata H. Endoscopic band ligation therapy for upper gastrointestinal bleeding related to Mallory-Weiss syndrome. Surg Endosc. 2006;20:1431–1434. doi: 10.1007/s00464-005-0608-5. [DOI] [PubMed] [Google Scholar]
- 25.Hachisu T. Evaluation of endoscopic hemostasis using an improved clipping apparatus. Surg Endosc. 1988;2:13–17. doi: 10.1007/BF00591392. [DOI] [PubMed] [Google Scholar]
- 26.Yamaguchi Y, Yamato T, Katsumi N, Morozumi K, Abe T, Ishida H, Takahashi S. Endoscopic hemoclipping for upper GI bleeding due to Mallory-Weiss syndrome. Gastrointest Endosc. 2001;53:427–430. doi: 10.1067/mge.2001.111774. [DOI] [PubMed] [Google Scholar]
- 27.Hurlstone DP. Successful endoscopic haemoclipping in Mallory-Weiss syndrome with concurrent closure of oesophageal perforation: further prospective evaluation of the technique is required. Scand J Gastroenterol. 2002;37:866. [PubMed] [Google Scholar]
- 28.Ohta S, Yukioka T, Ohta S, Miyagatani Y, Matsuda H, Shimazaki S. Hemostasis with endoscopic hemoclipping for severe gastrointestinal bleeding in critically ill patients. Am J Gastroenterol. 1996;91:701–704. [PubMed] [Google Scholar]
- 29.Ohta S, Goto H, Yukioka T, Mishima S, Shimazaki S. Efficacy of endoscopic hemoclipping for GI bleeding in relation to severity of shock. Hepatogastroenterology. 2003;50:721–724. [PubMed] [Google Scholar]
- 30.Park CH, Joo YE, Kim HS, Choi SK, Rew JS, Kim SJ. A prospective, randomized trial of endoscopic band ligation versus endoscopic hemoclip placement for bleeding gastric Dieulafoy's lesions. Endoscopy. 2004;36:677–681. doi: 10.1055/s-2004-825661. [DOI] [PubMed] [Google Scholar]