Abstract
Introduction
Modern investigation modalities allow markers of atherosclerosis to be detected at a subclinical stage. The aim of the study was to analyze the prevalence of these markers in relation to traditional risk factors.
Methods
The population based study included 4814 participants, aged 45 to 75 years, with a response rate of 55.8% of those contacted. The patients’ history, psychosocial and environmental risk factors were assessed.
Results
The prevalence of obesity was 26.2% in men and 28.1% in women, 26% of men and 21% of women were smokers. Hypertension was found in 46% of men and 31% of women, diabetes in 9.3% of men and 6.3% of women. Markers of subclinical peripheral arterial disease were found in 6.4% of men and 5.1% of women, of subclinical carotid artery disease in 43.2% and 30.7%, and of subclinical coronary artery calcification in 82.3% and 55.2%, respectively. The prevalence of coronary calcification measured using an Agatston Score >100 was in 40% in men and 15% in women, using a score >400, 16.8% and 4.5%, respectively.
Discussion
A high prevalence of subclinical atherosclerosis was found in the older population. The follow-up period will demonstrate whether the detection of markers of subclinical atherosclerosis will improve risk stratification beyond that offered by traditional risk factors.
Keywords: cardiovascular risk, atherosclerosis, peripheral arterial disease, carotid stenosis, ultrasound, CT, EBCT
Diabetes, hypertension, hypercholesterolemia, and smoking are the primary risk factors for cardiovascular events (1–5). Other contributory factors include lifestyle aspects such as physical activity, overweight, alcohol consumption (6), as well as inflammatory markers such as C-reactive protein, and psychosocial and environmental factors (7, 8, e1–e6).
These risk factors promote the development of arterial atherosclerosis, which begins as early as childhood or adolescence and manifests itself clinically decades later as acute myocardial infarction or stroke, or chronic coronary artery disease (CAD) or peripheral artery disease (PAD).
Today, imaging and other diagnostic techniques allow the markers of atherosclerosis to be identified at the subclinical stage (e7, e8). Subclinical PAD, for example, is diagnosed with the aid of the ankle-brachial index (ABI) (10, e9–e11), subclinical atherosclerosis of the carotid arteries by measuring intima-media thickness (IMT), plaque formation with the aid of ultrasound (11, e12–e15), and subclinical atherosclerosis of the coronary arteries by means of electron-beam computed tomography (EBCT) (12, e16–e21). EBCT can be used, without the need for contrast agents, to detect the arterial calcification that accompanies the development of atheromas and fibroatheromas, which become larger and thicker with advancing age. Detecting and quantifying calcification in this manner is reliable and precise, and radiation exposure is low (13, 14).
Concurrent to the Multi-Ethnic Study of Atherosclerosis (MESA) in the United States, the Heinz Nixdorf Recall Study is the first population-based study in Europe to use the above-mentioned diagnostic techniques to analyze the predictive value of subclinical markers of atherosclerosis compared to traditional risk factors (15, 16, e22, e23). The baseline examination of the cohort study has been completed. This paper will present the most important prevalence data on cardiovascular risk factors and subclinical atherosclerosis. The findings provide a picture of the distribution of risk factors in middle-aged and older individuals in the general urban population in Germany.
Methods
The Heinz Nixdorf Recall Study is a population-based, prospective cohort study of a random sample of 45- to 74-year-old subjects living the Ruhr-area cities of Bochum, Essen, or Mülheim/Ruhr (e23). Between the years 2000 and 2003, a total of 4814 out of 8400 eligible subjects took part in the study (participation rate: 55.8%) (e26) and were examined in a study center established by the medical school especially for the purposes of this investigation. Anamnestic data related, in particular, to cardiovascular risk factors were recorded by means of computer-aided personal interviews (CAPI) (22, e27, e28). In addition, anthropomet- ric data such as height and weight were collected, and blood pressure was measured using the oscillometric method and size-adjusted cuffs on the right arm (17). Hypertension was defined according to the JNC-7 guidelines as systolic blood pressure =140/90 mm Hg and/or use of blood pressure medication. Laboratory blood tests were performed to determine lipid metabolism parameters and other risk factors. Diabetes was defined as a fasting blood glucose level of =126 mg/dL, a postprandial blood glucose level of =200 mg/dL, or use of diabetes medication. The modified Framingham risk score was calculated based on these measurements (e8, e29). All subjects underwent resting ECG (MAC 5000, GE Health Care, Freiburg, Germany) (19).
To determine the presence of PAD, the ankle brachial index (ABI) was calculated; PAD was defined as a ratio <0.9 (10, 20, e9–e11, e30–e33). Duplex carotid ultrasound was used to measure IMT and detect plaque formation (Vivid FiVe, GE-Health Care, Freiburg) (11, e24).
EBCT (C-150, GE Imatron, San Francisco, USA) was performed in university radiology departments in Bochum and Mühlheim/Ruhr, and was the only diagnostic procedure to be conducted outside of the study center. To assess coronary artery calcification, 3-mm-thick slices were obtained with an image acquisition time of 100 ms; a calcified lesion was defined as a minimum of 4 adjacent pixels with a density of >130 Hounsfield units (13). Coronary artery calcification was quantified by means of Agatston score. The latter is calculated by multiplying the area of each lesion by a density factor and then summing the individual lesion scores (13, 15, 16, e22, e23). Based on a consensus recommendation, calcium scores were categorized as follows: 0 through 99, =100 through 399, and =400 (21, e34). The 75th percentile for age- and gender-adjusted Agatston score was also calculated. Alongside the absolute Agatston score, this cut-off is an established measure of increased myocardial infarction risk (18, e7, e8).
Psychosocial factors associated with cardiovascular disease were assessed by means of interviews and a questionnaire filled out by the participating subjects (22, e1, e2). These included, above all, aspects related to the social and economic backgrounds of the subjects, known stress factors (e.g. work stress), or psychological factors (e.g. depression). To measure potential environmental risk factors, the distance between place of residence and major roads was calculated, and median concentrations of ultrafine particles at each residential address were derived using a dispersion model (EURAD) (23, e3–e6, e25, e35). A distinction was drawn between subjects with CAD (n = 327) and those without it (n = 4487). CAD was defined as myocardial infarction or interventional/operative revascularization.
After the German Federal Office for Radiation Protection in Munich authorized use of the EBCT, the medical school’s ethics committee gave approval for the study. In addition, the study was monitored by an external agency and certified on more than one occasion according to DIN EN ISO 9001:2000 by TÜV Med Rheinland. The study was financed by the Heinz Nixdorf Foundation (chairman: Dr. G. Schmidt), and scientific review and oversight were provided on behalf of the foundation by a scientific advisory committee from the German Aerospace Center (under the auspices of the German Federal Ministry of Education and Research).
Statistics
Demographic data and risk factors are expressed as mean ± standard deviation, median, or as percentages. Gender differences were evaluated using the Wilcoxon rank-sum or chi-square test. Age-specific trends in ECG findings were analyzed (e-table) using the Mantel-Haenszel chi-square test (alternative hypothesis: non-vanishing correlation). The association between ECG findings and Agatston score was analyzed using multiple linear regression analysis with calcium score (logarithmized: log [calcium score + 1]) as dependent variable adjusted for age, gender, smoking status, systolic blood pressure, BMI, and LDL cholesterol.
E-Table. Definitions of ECG diagnoses based on the 12SL-Code (version MAC5K 12SL229).
| ECG diagnosis | Digital ECG code*1 |
| Normal ECG | #1684 (= normal ECG) |
| #1687 (= otherwise normal ECG)*2 | |
| Borderline ECG | #1687, #1693, #1694 |
| Abnormal ECG | #1699 |
| Normal SR (50<HR<100 bpm) | According to HR |
| Atrial fibrillation/flutter | #161, #162 |
| Frequent premature contractions | #181, #231, #232, #241, #243 [only when in combination with #212 (= with frequent)] |
| Left axis deviation (LAxD) | QRS axis more negative than -30° |
| AV block | #101 (= 1st°), #103 (= 2nd° Mobitz I), #104 (= 2nd° Mobitz II), #105 (= 2nd°), #106 (= 3rd°), #107 (= variable AV block), #480 (=bifascicular block) |
| BBB (complete) | #440, #460 (= complete right or left BBB) |
| BBB (incomplete)*3 | #450 (= rSr' or qR pattern in V1) |
| #445, #465 (= incomplete right or left BBB), | |
| #470, #471 (= left anterior and posterior fascicular block) | |
| LVH | #540 (= voltage criteria for LVH), #541 (LVH) |
| Borderline LVH | #542 (= minimal criteria for LVH; can be normal) |
| #548 (= moderate voltage criteria for LVH; can be normal) | |
| ST-segment depression | #1002 (junctional ST depression, presumably abnormal) |
| #1022*4 (ST depression, due to ischemia or digitalis) | |
| #1040-1081 (clear, ischemia-like ST abnormality in multiple leads) | |
| T-wave changes | #1140, #1141 (nonspecific T-wave or ST and T-wave abnormality) |
| #1142 (abnormal QRS-T angle, T-wave abnormality), #1182 (T-wave inversion), | |
| #1145-1181 (clear ischemia-like T-wave abnormality in multiple leads) | |
| Abnormal T axis | T axis: -180° to -15° or 105° to 180° |
| Long QT | QTc >440ms,*5 QTc (Bazett's formula) |
| Signs of ischemia*6 | #900, #904, #1021, #1023 (nonspecific ST changes)*7, #1140*7, #1141*7, #1145, #1181 |
| #1020*4, #1022*4 (ST changing/depression, possible digitalis effect) | |
| #1040-#1081 (see further above) | |
| #1142 (abnormal QRS-T angle, T-wave abnormality) | |
| Signs of infarction | #700-#829 (infarct in multiple leads) |
| #963-#968 (ST elevation, injury pattern or infarct) | |
| Major ECG findings | #161, #162, #1040-1081, #1145-#1182, #103-#106, #440, #460 (#181, #231, #232, #243 [only when in combination with #212 (= with frequent)] |
The "#" symbol signifies that the following number is a code number.
*1 The most important codes are listed; further statements provide additional details, e.g., anterior leads (#1451).
*2 Classified as normal only when the only other finding is bradycardia.
*3 Not including #482 and #487 (nonspecific intraventricular conduction block or delay)
*4 Persons who are digitalized were excluded.
*5 Persons with QRS interval >120 ms or with atrial fibrillation/flutter were excluded.
*6 Persons with pacemakers or QRS interval >120 ms were excluded.
*7 If it cannot be attributed to LVH, IV block (#482), (in)complete BBB, or digitalis effect
SR, sinus rhythm; HR, heart rate; AV, atrioventricular; BBB, bundle branch block; LVH, left ventricular hypertrophy. Major ECG findings: ST depression, T-wave inversion, complete or incomplete AV block, frequent premature ventricular contractions or atrial fibrillation/flutter.
Population-based Agatston-score percentiles were calculated separately for men and for women between 45 and 75 years of age and in 5-year increments. IMT percentiles were also calculated in this manner for male subjects. The association between chronic exposure to high traffic levels near a subject’s place of residence and an Agatston score >75th age- and gender-specific percentile was assessed using multiple logistic regression analysis. Odds ratios (OR) and their 95% confidence intervals (CI) based on Wald’s test were adjusted for age, gender, city, residential area, educational attainment, smoking status, exposure to passive smoke, physical activity, waist-hip ratio, diabetes, blood pressure, and lipid status. The bivariate association between IMT and Agatston score was assessed using Spearman’s rank correlation coefficient. Please see e-supplement for a more detailed description of the study methods and statistics.
E-Supplement. Methods and statistics.
Methods
Between the years 2000 and 2003, a total of 4814 persons from the cities of Bochum, Essen, and Mülheim were included in the study. A random sample of the general population aged 45 to 74 years was drawn from residents’ registration offices and invited to participate. A total of 55.8% of those who received an invitational letter ultimately took part in the investigation. The participation rate was thus well within the range of rates seen in comparable epidemiological studies conducted in Germany in recent years, including the EPIC study in 1999 (23%) and the KORA survey in 2004 (65%). Details on recruitment, characteristics of participants and non-participants, and potential determining factors have been published elsewhere (e26). Participants differed from non-participants only insofar as the latter were more likely to be current smokers and come from lower socioeconomic groups (e26).
Anthropometric data such as height, weight, waist and hip circumference were collected. Blood pressure was recorded three times for each participant, with a 3-minute interval in between measurements; the last two values were averaged for the analysis. Cuff size was chosen based on upper-arm circumference (17). In addition to a random-zero mercury device (Mark II Hawksley, Lancing, UK) like that used in previous epidemiological studies, the present study employed an automated oscillometric device (HEM-705CP, Omron, Hoofddrop, Netherlands). This was done to allow for comparison of both methods (17). Hypertension was defined as systolic blood pressure =140/90 mm Hg and/or use of blood pressure medication; patients were classified as having stage 1 or 2 hypertension according to the JNC-7 guidelines. Blood and urine samples were also collected. In addition to complete and differential blood counts, study physicians measured urea, electrolytes, and creatinine, as well as liver enzymes, thyroid hormones, and lipid metabolism parameters. Diabetes was defined as a fasting blood glucose level =126 mg/dL, a postprandial blood glucose level =200 mg/dL, or use of diabetes medication. Glycosylated hemoglobin was also measured. A total of 52 blood samples were frozen and stored at –80 °C.
Twelve-lead resting ECG was performed with a MAC 5000 (GE-Health Care, Freiburg, Germany) and evaluated using a computerized 12SL-Code (GE-Health Care, Freiburg, Germany) (19), as part of which each ECG diagnosis was assigned a numerical code. The different codes and the diagnoses upon which they are based (table 2) are listed in the e-table.
To determine the presence of PAD, medical history was taken and ankle-brachial index (ABI) calculated. Blood pressure was obtained in the posterior tibial artery or dorsal pedal artery of the right or left leg, and in the right arm. For each patient, the highest value was taken. A ratio of <0.9 was interpreted as PAD, and a ratio >1.3 as a sign of medial arterial calcification (20).
High-resolution ultrasound (7 to 10 MHz) was used to examine the carotid arteries and measure intima-media thickness (IMT) and plaque formation (Vivid FiVe, GE, Health Care, Freiburg, Germany).
Electron-beam computed tomography (EBCT; C-150, GE, Imatron, San Francisco, USA) was performed in two university radiology departments. The scanner was used in single-slice mode with an image acquisition time of 100 ms and a slice thickness of 3 mm. Prospective ECG triggering was used and set at 80% of the RR interval (16, e23), and contiguous slices from the apex to the base of the heart were obtained. A focus of coronary calcium was defined as a minimum of four adjacent pixels with a density of >130 Hounsfield units. Groups of pixels identified in this manner were assigned one of four density levels; this density factor was then multiplied by the area of the respective calcium focus. The resulting Agatston score (13) was calculated for the individual arterial segments, for the entire artery, and for all three coronary arteries (16, e23).
Another important aspect of the study is the role played by socioeconomic and psychological factors in the distribution of disease risk. As international research has shown, cardiovascular disease is strongly associated with socioeconomic status and psychosocial and physical environmental factors (e2). To identify these factors, the baseline examination employed standardized personal interviews conducted by a trained interviewer and, in the case of more sensitive information, questionnaires to be filled out by the participating subjects (CAPI, DAIMON, version 1.0).
Participants’ residential addresses (n = 4494) were coded using the geographic information system Mapinfo, and proximity to expressways and federal highways was calculated. High exposure was defined as living within 100 m of an expressway or federal highway. For each residential address, background concentrations of PM 2.5 were determined using the EURAD regional dispersion model (23). This model is based on the official emissions register of the German federal state of North Rhine-Westphalia, as well as on topographical and meteorological data, and was validated through comparison of measured and modeled values (23).
Following the examinations at the study center, all participants received copies of the laboratory results and resting ECG, as well as information about the findings of the carotid ultrasound.
To avoid any potential physician/hospital effect, a study center was established outside of the university medical school, specifically for the purposes of this investigation. A comprehensive training and qualification program was implemented to ensure data quality. The study design was reviewed by an international advisory committee selected by the German Aerospace Center under the auspices of the German Federal Ministry of Education and Research.
In addition to regular internal quality control, the study is monitored by participation in external quality control programs. These include regular on-site inspections by the Helmholtz Association’s National Research Center for Environment and Health (GSF) and certification according to DIN EN ISO 9001:2000. The Heinz Nixdorf Recall Study is the first study of its kind to be certified and regularly recertified according to the DIN EN ISO 9001:2000 standard.
The study was approved by the ethics committee of the University of Duisburg-Essen Medical School after the German Federal Office for Radiation Protection in Munich authorized use of the EBCT. All participants gave written, informed consent. The study is financed by the Heinz Nixdorf Foundation (chairman: Dr. G. Schmidt). The German Research Foundation has funded 2 projects (Project SI 236/8–1 & Project SI 236/9–1), and the socioeconomic analysis has been made possible by a grant from the German Federal Ministry of Education and Research (01EG 0401).
Statistics
The primary endpoints in this study were defined as cardiac death and nonfatal myocardial infarction (e23). Secondary endpoints were overall mortality, stroke, revascularization, and cardiovascular-related hospital stays within 5 years after being included in the study. Calculations to determine the number of hard cardiac events required to detect a relative risk of 2.5 for the highest compared to the lowest Agatston-score quartile were based on figures from the PROCAM and MONICA studies (2, 3). Assuming 300 to 500 events per 100 000 inhabitants, we determined that a total of n = 60 hard endpoints would be required for an alpha error of 5% and power of 90%. Target parameters in the cross-sectional analysis included clinically manifest coronary artery disease (CAD), defined as past myocardial infarction or coronary angioplasty procedure (stent, bypass, balloon dilatation) in the patient’s medical history, and coronary calcium levels, as quantified by means of Agatston score. Analyses of the markers of subclinical atherosclerosis were adjusted for age and gender, and 25th, 50th, 75th, and 90th percentiles were calculated. Percentiles were smoothed with linear interpolation, which was based on the raw data available for each age group. The Agatston-score percentile can be calculated for each age or gender (www.recall-studie.uni-essen.de). If a score does not fall exactly within a given percentile, it is rounded to the nearest percentile.
Data on environmental pollution were evaluated using logistic regression analysis adjusted for age, gender, smoking status (non-smoker/ex-smoker for more than 1 year/active smoker), passive smoke exposure (frequently spending time in rooms with smokers), educational attainment (low: 10 years of school, in-company vocational training or vocational school; medium: 10 years of school, vocational college; high: 10 years of school and College/University or University of Applied Sciences), physical activity, anthropometric data, diabetes, blood pressure, lipid status, city, and residential area.
APPENDIX
Scientific advisory committee: Meinertz T, Hamburg (chair); Bode C, Freiburg; de Feyter PJ, Rotterdam, Netherlands; Güntert B, Hall i. T., Austria; Gutzwiller F, Schweiz; Heinen H, Bonn; Hess O, Bern, Switzerland; Klein B, Essen; Löwel H, Neuherberg; Reiser M, Munich; Schmidt G, Essen; Schwaiger M, Munich; Steinmüller C, Bonn; Theorell T, Stockholm, Sweden; Willich SN, Berlin. Criteria and endpoint committee: Bode C, Freiburg (chair); Berger K, Münster; Figulla HR, Jena; Hamm C, Bad Nauheim; Hanrath, Aachen; Köpcke W, Münster; Weimar C, Essen; Zeiher A. Frankfurt. Laboratory committee: Hafner, Essen (chair); Jäger B, Essen; Volbracht L, Essen; Bröcker-Preuss M, Essen. Data and safety monitoring: Hense HW, Münster (chair); Böhm M, Homburg; Breithardt G, Münster; Moshage W, Traunstein; Silber S, München; Tillmanns H. Gießen. Data analysis committee: Hense HW, Münster (chair); Böhm M, Homburg; Breithardt G, Münster; Moshage W, Traunstein; Silber S, München; Tillmanns H, Gießen.
In addition to the authors, the following individuals have played a substantial role in the development of the study in the investigator group, committees, and working groups. Earlier scientific partners of the investigator group: Baumgart D, Essen, Rauwolf M, Essen; Hirche H, Essen; Peter R, Ulm; K Lauterbach, Cologne. Earlier study group members: Assert R, Beck EM, Benemann J, Berenbein S, Ebralidze T, Freitag N, Gutersohn A, Jaeger B, Karoussos I, Kriener P, Mankovski J, Münkel S, Öffner A, Pump H, Püttmann P, Ritzel A, Schuldt K, Snyder-Schendel E, Erbel S,Weyhers S, Winterhalder S.
Results
In the 4487 subjects (93.2%) without CAD, 46.3% of men and 30.8% of women had hypertension (stage 1 or 2), 26% of men and 21.3% of women were smokers, 9.3% of men and 6.3% of women had diabetes, and 50.5% of men and 49.5% of women had hypercholesterolemia. A high Framingham risk score (>20% over 10 years) was found in 26.2% of men and 1.4% of women (table 1).
Table 1. Demographic data for men and women.
| Men | Women | P value | ||
| All subjects (%) | 2395 (49.8%) | 2419 (50.2%) | ||
| Age (years) | 59.5±7.8 | 59.6±7.8 | ||
| Known CAD | 259 (10.8%) | 68 (2.8%) | ||
| Subjects without CAD | 2136 (89.2%) | 2351 (97.2%) | ||
| Stroke | 3.0% | 1.8% | 0.01 | |
| Glucose (mg/dL) | 114.7±30.3 | 107.1±23.2 | <0.0001 | |
| Glycosylated hemoglobin (%) | 5.6±0.9 | 5.4±0.8 | <0.0001 | |
| < 6.5% | 90.4% | 93.9% | < 0.0001 | |
| ≥ 6.5 - 7.5% | 5.6% | 3.6% | ||
| ≥ 7.5% | 4.0% | 2.5% | ||
| Known diabetes | 9.3% | 6.3% | 0.0002 | |
| Known hypertension | 42.9% | 40.2% | 0.07 | |
| RR systolic (mm Hg) | 138.1±19.3 | 128.3±21.0 | < 0.0001 | |
| RR diastolic (mm Hg) | 84.5±10.5 | 79.0±10.5 | < 0.0001 | |
| Normal/borderline hypertension | 53.6% | 69.2% | < 0.0001 | |
| Stage 1: 140-159 / 90-99 mm Hg | 31.1% | 22.3% | ||
| Stage 2: ≥160 / ≥ 100 mm Hg | 15.2% | 8.5% | ||
| Non-smokers | 29.3% | 56.0% | < 0.0001 | |
| Ex-smokers | 44.7% | 22.7% | ||
| Smokers | 26.0% | 21.3% | ||
| BMI (kg/m2) | 28.2±4.0 | 27.6±5.2 | < 0.0001 | |
| BMI ≥ 25 kg/m2 | 80.8% | 65.6% | < 0.0001 | |
| BMI ≥ 30 kg/m2 | 26.2% | 28.1% | 0.16 | |
| Known hypercholesterolemia | 50.5% | 49.5% | 0.50 | |
| Total cholesterol (TC) (mg/dL) | 227.7±37.7 | 234.2-39.4 | < 0.0001 | |
| TC | < 200 mg/dl | 22.4% | 18.5% | < 0.0001 |
| ≥ 200-239 mg/dL | 41.9% | 38.7% | ||
| ≥ 240 mg/dL | 35.7% | 42.8% | ||
| HDL (mg/dL) | 51.5±14.4 | 65.1±17.0 | < 0.0001 | |
| Non-HDL (mg/dL) | 176.2±38.4 | 169.0±40.5 | < 0.0001 | |
| LDL (mg/dL) | 147.3±35.2 | 146.5±36.8 | 0.40 | |
| LDL | < 130 mg/dl | 30.8% | 33.4% | 0.88 |
| ≥ 130-159 mg/dL | 34.9% | 31.6% | ||
| ≥ 160-189 mg/dL | 23.6% | 23.0% | ||
| ≥ 190 mg/dL | 10.7% | 12.0% | ||
| Triglycerides (TG) (mg/dL) | 165.5±120.2 | 132.5±77.3 | < 0.0001 | |
| TG | < 150 mg/dl | 55.9% | 70.8% | < 0.0001 |
| ≥ 150-199 mg/dL | 18.6% | 15.8% | ||
| ≥ 200-499 mg/dL | 23.9% | 13.0% | ||
| ≥ 500 mg/dL | 1.6% | 0.4% | ||
| FRS (% over 10 years) | 15.8±9.5 | 7.6±4.9 | < 0.0001 | |
| FRS | < 10% over 10 years | 30.8% | 74.1% | < 0.0001 |
| ≥ 10 - ≤ 20% over 10 years | 43.0% | 24.5% | ||
| > 20% over 10 years | 26.2% | 1.4% | ||
| hs CRP (Median, mg/L) | 1.3 | 1.4 | 0.20 | |
| hs CRP | ≤1 mg/L | 40.8% | 38.4% | 0.09 |
| > 1 - ≤ 3 mg/L | 37.3% | 38.1% | ||
| > 3 - ≤ 10 mg/L | 21.9% | 23.5% | ||
| Degree of calcification (Agatston score) Median | 55.2 | 1.5 | < 0.0001 | |
| 0-99 | 59.6% | 84.6% | < 0.0001 | |
| ≥ 100-399 | 23.6% | 10.9% | ||
| ≥ 400 | 16.8% | 4.5% | ||
| 0 | 17.7% | 44.8% | < 0.0001 | |
| > 0 and < 75th percentile | 57.4% | 30.3% | ||
| ≥ 75th percentile | 24.9% | 24.9% | ||
Mean ± standard deviation, or percent, for various risk factors associated with cardiovascular disease; table also includes Framingham risk scores (FRS) and degree of coronary calcification (Agatston score).
CAD, coronary artery disease; RR, blood pressure (Riva Rocci method); BMI, body mass index; HDL, high-density lipoprotein; LDL, light-density lipoprotein; FRS, Framingham risk score calculated according to (18); hs CRP, high-sensitive C-reactive protein. P values for gender differences.
Like these risk factors, the prevalence of detectable arrhythmias and pathological ECG findings were age- and gender-specific (table 2). ECG abnormalities indicative of a past myocardial infarction were found in 13.3% of men and 8.3% of women >65 years of age. Adjusted for age, gender, and risk factors, a normal ECG was independently predictive of low coronary calcification in subjects without CAD and with no treated risk factors. In contrast, left-ventricular hypertrophy, prolonged QTc interval, and major ECG abnormalities were associated with pronounced coronary calcification.
Table 2. Prevalence of ECG abnormalities potentially relevant to prognosis in individuals without known CAD in different age groups.
| Age 45-54 | Age 55-64 | Age 65-75 | P value | ||||
| Men | Women | Men | Women | Men | Women | for age trend | |
| (n = 693) | (n = 727) | (n = 836) | (n = 901) | (n = 559) | (n = 661) | Men/Women | |
| Normal ECG | 65.1% | 69.1% | 53.2% | 61.3% | 36.7% | 47.4% | <0.0001 / <0.0001 |
| Normal SR | 67.8% | 74.6% | 65.2% | 75.0% | 53.5% | 70.4% | <0.001 / 0.09 |
| Atrial fibrillation/flutter | 0.4% | 0.4% | 1.9% | 0.2% | 4.5% | 2.3% | <0.0001 / <0.0001 |
| Left axis deviation | 2.7% | 2.1% | 6.6% | 3.3% | 11.6% | 4.2% | <0.0001 / 0.07 |
| AV block | 2.6% | 1.9% | 4.1% | 1.9% | 7.7% | 4.5% | <0.0001 / 0.002 |
| BBB (complete) | 1.3% | 1.1% | 2.2% | 1.7% | 6.3% | 2.6% | <0.0001 / 0.1 |
| BBB (incomplete) | 3.3% | 2.2% | 4.1% | 2.3% | 7.3% | 2.4% | <0.002 / 0.96 |
| LVH | 2.2% | 0.8% | 4.0% | 1.6% | 5.4% | 2.1% | 0.01 / 0.1 |
| Borderline LVH | 10.0% | 5.6% | 9.3% | 5.3% | 10.9% | 8.8% | 0.62 / 0.01 |
| T-wave changes | 5.6% | 5.1% | 8.7% | 6.7% | 9.3% | 10.9% | 0.03 / <0.0001 |
| Abnormal T axis | 1.6% | 1.0% | 2.2% | 1.0% | 2.5% | 2.1% | 0.51 / 0.1 |
| QTc > 440 ms | 2.2% | 7.7% | 4.9% | 10.5% | 9.7% | 9.1% | <0.0001 / 0.14 |
| Signs of ischemia | 5.9% | 6.7% | 10.4% | 10.5% | 13.0% | 15.4% | <0.0001 / 0.003 |
| Signs of infarction | 4.6% | 4.3% | 7.5% | 5.0% | 13.3% | 8.3% | <0.001 / <0.001 |
| Major ECG findings | 3.5% | 3.3% | 6.9% | 3.6% | 14.0% | 9.4% | <0.001 / <0.001 |
Data are based on the integrated 12SL-Code (GE Medical Systems, Freiburg), which is generated independently of individual investigators. In 110 persons without CAD, a digital ECG analysis was not available. Persons with CAD (n = 327) were excluded.
SR, sinus rhythm; AV, atrioventricular; BBB, bundle branch block; LVH, left ventricular hypertrophy. Major ECG findings: ST-segment depression, T-wave inversion, complete or incomplete AV block, frequent premature ventricular contractions or atrial fibrillation/flutter; further definitions in (19).
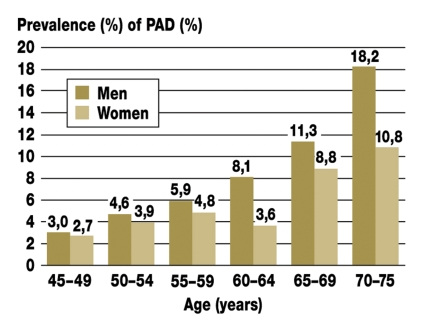
A total of 1.8% of men and 0.4% of women without CAD indicated that they had PAD; among men and women with CAD, however, these numbers rose to 24% and 18.2%, respectively. The age- and gender-specific prevalences of an ABI <0.9 are given in diagram 1. Medial arterial calcification, defined as an ABI >1.3, was observed in 1.7% of men and 0.7% of women.
Diagram 1.
Prevalence of peripheral artery disease (PAD), defined as an ankle-brachial index (ABI) <0.9 for men and women in different age groups (20)
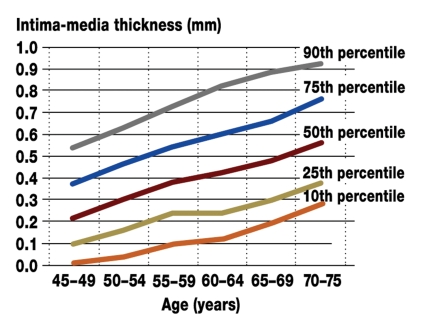
The prevalence of plaque formation in the carotid arteries was 43.2% in men and 30.7% in women. However, 23% of the 1526 men without any coronary calcification also showed plaque formation in the carotid arteries. IMT (diagram 2) was highly age-dependent, and the percentiles allow for an individual assessment of results.
Diagram 2.
Different intima-media thickness (IMT) percentiles in men aged 45 to 75 years
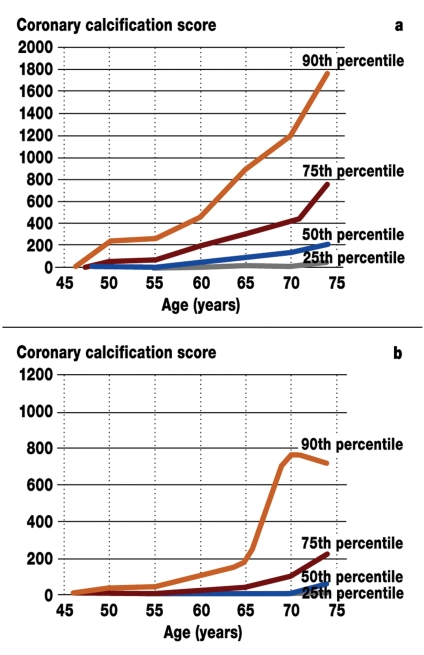
Coronary artery calcification, defined as a positive EBCT result (Agatston score >0), was found in 82.3% of men and 55.2% of women (table 1). Women had a considerably lower degree of calcification than men (diagram 3). All men and 92% of women with CAD had coronary artery calcification. If the Agatston score was =10, 65% of the participants had carotid plaque formation; 34%, if the Agatston score was =100. Twenty percent of male subjects had both a calcium score =100 and plaques in the carotid arteries. Only 3% of men had an ABI <0.9, plaques in the carotid arteries, and a coronary calcium score =100.
Diagram 3.
Extent of coronary calcification as quantified using the Agatston score a) in men and b) in women aged 45 to 75 years, shown for the 25th, 50th, 75th, and 90th percentiles (16). Please note the different ordinate scales for men and women (16).
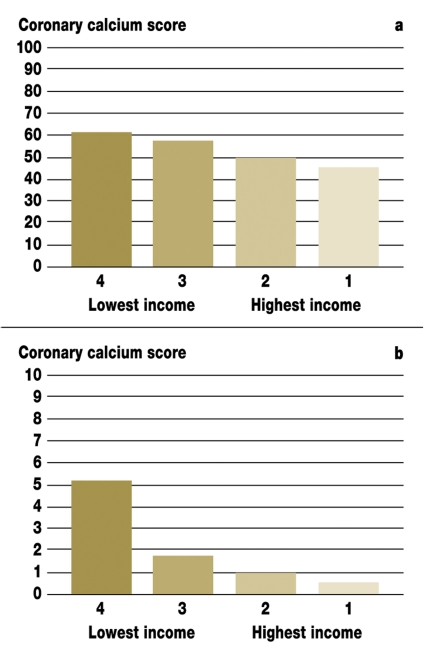
Various analyses demonstrated that the majority of established cardiovascular risk factors occurred more frequently in subjects from lower socioeconomic groups, as defined in terms of income, education, and occupation. Because the results cannot be presented here in detail, diagram 4 shows an example of this kind of social gradient – i.e., the median coronary calcium score according to income group. As can be seen in the diagram, the median calcification score increases as income decreases. This finding was statistically significant, even after adjusting for age in multivariate analysis (not shown).
Diagram 4.
Coronary calcium score according to income group a) in men and b) in women. The Agatston scores indicated are the median scores for each income group. The darkest bar shows the lowest income group, the lightest bar the highest. Groups were formed by dividing income into quartiles (22).
Population analyzed: 1932 men, 2036 women without CAD and with complete income data.
Men: Q1 = 1108 EUR, Q2 = 1108 to 1519 EUR,
Q3 = 1520 to 2173 EUR, Q4 = 2173 EUR
Women: Q1 = 938 EUR, Q2 = 938 to 1312 EUR,
Q3 = 1313 to 1875 EUR, Q4 =1875 EUR
Of the 4494 subjects for whom coded data on place of residence, coronary calcium score, and all documented risk factors were available, a total of 351 (7.8%) were living within 100 m of an expressway or federal highway with an average traffic flow of between 10 000 and 130 000 motor vehicles per day. A total of 8.0% (n = 28) of the subjects in this group had CAD compared to only 6.5% (n = 270) of the 4143 subjects who were not exposed to these levels of traffic. Among all subjects, the adjusted odds ratio for the association between living close (<100 m) to a major road or highway and having a coronary calcium score >75th percentile was 1.45 (95% CI: 1.15 to 1.82), with strong effects in men (OR: 1.65; 95% CI: 1.19 to 2.28) and in subjects with low educational attainment (OR: 1.64; 95% CI: 1.22 to 2.20). However, this association was weaker in women (OR: 1.26; 95% CI: 0.90 to 1.76), smokers (OR: 1.35; 95% CI: 0.86 to 2.14), and individuals with high levels of educational attainment (OR: 1.36; 95% CI: 0.69 to 2.68). As can be seen in diagram 5, there was a clear exposure-effect relationship between increasing proximity to a major road and having an Agatston score >75th percentile.
Diagram 5.
Odds ratios with 95% confidence intervals (CIs) for the association between proximity to a major road and an Agatston score >75th age- and gender-specific percentile. Adjusted for age, gender, city, residential area, educational attainment, smoking status, exposure to passive smoke, physical activity, waist-hip ratio, diabetes, blood pressure, and lipid status. Results shown are for 4196 subjects without CAD and for whom Agatston score and documentation of all risk factors were available.
Discussion
The Heinz Nixdorf Recall Study is the first study to determine the prevalence in Germany not only of known and new candidate cardiovascular risk factors, but also of subclinical atherosclerosis in the carotid arteries, the arteries of the lower limbs, and coronary vessels. The study sample is representative of the population of the Ruhr area, which is home to approximately 6 million people with a higher percentage of female smokers than elsewhere in Germany (4). Concurrent to the present study, the similarly designed MESA study in the United States examined, among other ethnic groups, 2619 white subjects aged 45 to 84 years (15, 24, e36). Gender distribution and BMI (at 28 ± 5 kg/m2) were comparable in both studies. However, participants in the Heinz Nixdorf Recall Study had cholesterol levels that were 35 mg/dL higher, LDL cholesterol levels that were 30 mg/dL higher, and triglyceride levels that were 15 mg/dL higher on average; they were also less likely to be taking cholesterol-lowering drugs (9.6% versus 18%). The prevalence of diabetes and hypertension in the present study were 7.7% and 35%, respectively, and were thus virtually identical to the prevalences observed among white subjects in the MESA study (7.8% and 36%, respectively). At 124 ± 20 and 70 ± 10 mm Hg, blood pressure in the cohorts of the present study was higher than in the MESA study. Moreover, in the German study there were twice as many smokers (24% versus 12%). The median Framingham score (risk of experiencing a cardiovascular event within the next 10 years) was 10.6 ± 7.6% in the present study versus 9.3 ± 7.1% in the MESA study. The follow-up data will show whether, as is to be expected (e37), the Framingham score overestimates the actual risk in Germany.
Peripheral artery disease
In the present study, PAD was present in almost 1 out of every 20 participants, a figure that rose to 1 out of every 5 men and 1 out of every 7 women among patients with CAD (20, e9). In the getABI study, which examined a German cohort of 6880 patients over 65 years of age, PAD was detected in 19.8% of men and 16.8% of women (25). The ABI is simple to perform and should be considered standard of care in the older population, because of therapeutic consequences (10, e9, e10), and because 20% to 50% of patients over 50 years of age have no symptoms and only 10% to 35% have classic claudication (10). Moreover, nonfatal myocardial infarction or stroke occurs in 20% to 40% of cases and is associated with a mortality of 10% to 30% over the following 5 years (10, e9). In the MESA study, the prevalence of PAD was considerably lower than in the present study (in men: 2.7%; in women: 3.4%) (20, e9).
Carotid artery disease
When evaluating IMT, age and gender need to be taken into account to ensure reliable risk stratification of individual patients. In general, an IMT of >0.9 mm to >1 mm is considered to be a cut-off value for identifying high-risk patients (5, 11, 18, e32, e33). Patients with evidence of plaque formation in the carotid artery are also to be considered at high risk (e24). However, according to the results of the present study, the current IMT cut-off values appear to be too high, thus leading to underestimates of cardiovascular risk. Analyses of data from the prospective study will demonstrate whether the cut-off values need to be modified.
Our data show that there was only a weak association between the degree of coronary calcification and IMT in male subjects (Spearman’s rank correlation coefficient of 0.26), which means that IMT measurements alone are insufficient to predict the presence of subclinical atherosclerosis of the coronary arteries.
Coronary artery calcification
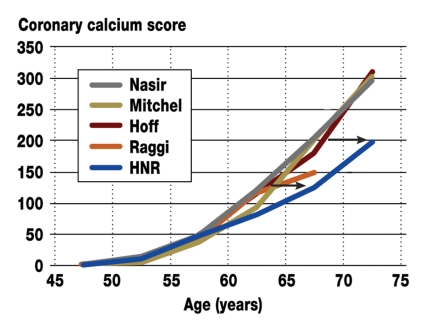
The prevalence of coronary artery calcification in men was 82.3%, which was significantly higher than the 55.2% detected in women. The age- and gender-adjusted percentiles allow for an individual assessment of results, which are available on the internet (www.recall-studie.uni-essen.de). Previous analyses of data from selected patient collectives have demonstrated that the actual risk has been considerably underestimated (diagram 6) (16, e16–e19).
Diagram 6.
Coronary calcification in relation to age. Agatston score in the 50th percentile in the Heinz Nixdorf Recall Study (HNR) and in earlier, exclusively patient-based studies: Raggi (e16), Hoff (e17), Mitchell (e18), and Nasir (e19). The two arrows indicate different Agatston scores (125 and 200), illustrating how the curve of the population-based studies is shifted by 6 to 8 years compared to studies of selected patient cohorts (16).
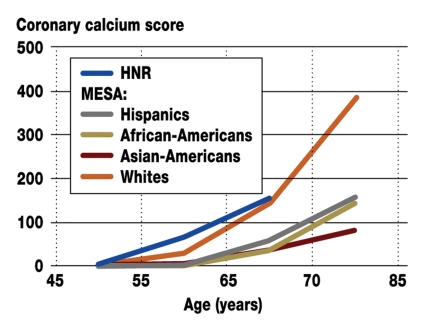
The analyses of the population-based studies thus confirmed the criticism directed at earlier publications in which selected patient collectives were investigated (e37). In comparison to the MESA study a very good agreement was found (24). In addition, the MESA study shows considerable differences between ethnicities (e-diagram).
E-Diagram.
Coronary calcification (Agatston score) in the 50th percentile among men in the Heinz Nixdorf Recall Study (HNR) and in different ethnic groups in the Multi-Ethnic Study of Atherosclerosis (MESA) (16, 24).
EBCT has recently given way to multislice computed tomography (MSCT), also known as multidetector computed tomography (MDCT); the results, however, are comparable (e38). By using correction factors, different CT systems can be compared to one another (e36).
Psychosocial risk factors
The cross-sectional data alone show a clear relationship between socioeconomic status and risk of disease (e39), as demonstrated by the association between income and degree of coronary calcification presented above (22). This example is confirmed by further analyses (not presented here), which reveal an association between educational attainment or occupation and coronary calcification, as well as between socioeconomic indicators and PAD. In addition, the cross-sectional data provide preliminary insight into the socioeconomic inequalities affecting disease risk. In lower socioeconomic groups, an unhealthy lifestyle (7, e27, e28) and increased exposure to illness-causing psychosocial and physical environmental factors appear to play a very important role. These initial findings suggest that socioeconomic characteristics should be taken more strongly into consideration when evaluating risk profiles, and that preventive measures are needed to help reduce socioeconomic inequalities.
Environmental risk factors
It is well-known that chronic exposure to high concentrations of ultrafine particles leads to increased cardiovascular morbidity and mortality (e3–e6, e40, e41) The present study shows that long-term exposure to high levels of traffic near an individual’s place of residence is associated with increased cardiovascular morbidity and subclinical atherosclerosis, independent of background concentrations of ultrafine particles (23, e35). The ultrafine particle fraction (<100 nm) or specific chemical components such as transition metals and traffic noise have been variously hypothesized to be responsible for the pathogenic effects of traffic emissions (e25).
The weaker association between traffic and coronary calcification in smokers is potentially due to the dominating effect of smoking, since the cardiovascular effects of smoking and those of ultrafine particles presumably involve the same pathophysiological mechanisms (e41).
Perspectives
Both the Heinz Nixdorf Recall Study and the MESA study aim to assess markers of subclinical atherosclerosis in relation to traditional and new candidate risk factors, as well as to the Framingham, PROCAM, and European Society of Cardiology (ESC) Score algorithms. A particularly important observation is that risk estimates based on established risk factors frequently underestimate the actual extent of subclinical atherosclerosis by considerable margins (e42). Data from the follow-up period will demonstrate whether this difference is also reflected in a different rate of cardiovascular events.
Acknowledgments
Translated from the original German by Matthew D. Gaskins.
Footnotes
Conflict of interest statement
Prof. Dr. Raimund Erbel declares that he received support from Siemens to organize a congress.
PD Möhlenkamp receives research support and fees from GE Medical Systems and Merck.
PD Schmermund received fees from GE Medical Systems and Siemens, as well as research support from Siemens.
Prof. Jöckel conducts a variety of externally funded projects at his institute, including some that are funded by the (pharmaceutical) industry.
Dr. Lehmann, Dr. Moebus, Prof. Stang, Dr. Dragano, Dr. Hoffmann, Prof. Grönemeyer, Prof. Seibel, Prof. Siegrist, Prof. Mann, PD Kröger, Dr. Broecker-Preuss, and Dr. Volbracht declare that no conflict of interest exists according to the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Kannel WB. CHD risk factors: a Framingham study update. Hosp Pract. 1990;25:119–127. doi: 10.1080/21548331.1990.11703974. [DOI] [PubMed] [Google Scholar]
- 2.Assmann G, Schulte H, Cullen P. New and classical risk factors - the Münster heart study (PROCAM) Eur J Med Res. 1997;2:237–242. [PubMed] [Google Scholar]
- 3.Keil U, Liese AD, Hense HW, Filipiakt B, Döring A, Stiebert J, Löwel H. Classical risk factors and their impact on incident non-fatal and fatal myocardial infarction and all-cause mortality in southern Germany. Results from the MONICA Augsburg cohort study 1984-1992. Eur Heart J. 1998;19:1197–1207. doi: 10.1053/euhj.1998.1089. [DOI] [PubMed] [Google Scholar]
- 4.Völzke H, Neuhauser H, Moebus S. Rauchen: Regionale Unterschiede in Deutschland. Dtsch Arztebl. 2006;103(42):B2784–B2790. [Google Scholar]
- 5.De Backer G, Ambrosioni E, Borch-Johnsen K. Executive summary. European guidelines on cardiovascular disease prevention in clinical practice. 3rd Joint Task Force of European and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J. 2003;24:1601–1610. doi: 10.1016/s0195-668x(03)00347-6. [DOI] [PubMed] [Google Scholar]
- 6.Yusuf S, Hawken S, Ounpuu S. INTERHEART Study Investigators: Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 7.Mackenbach JP, Bos V, Anderson O. Widening socioeconomic inequalities in mortality in six Western European countries. Int J Epidemiol. 2003;32:830–837. doi: 10.1093/ije/dyg209. [DOI] [PubMed] [Google Scholar]
- 8.Memmesheimer M, Friese E, Ebel A. Long-term simulations of particulate matter in Europe on different scales using sequentiel nesting of a regional model. Int J Environ Pollution. 2004;22:108–132. [Google Scholar]
- 9.Ridker P, Rifai N, Koenig W, Blumenthal RS. C-reactive protein and cardiovascular risk in the Framingham Study. Arch Intern Med. 2006;166:1327–1328. doi: 10.1001/archinte.166.12.1327-b. [DOI] [PubMed] [Google Scholar]
- 10.Hirsch AT, Haskal ZJ, Hertzer NR. ACC/AHA 2005 practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) Circulation. 2006;113:e463–e654. doi: 10.1161/CIRCULATIONAHA.106.174526. [DOI] [PubMed] [Google Scholar]
- 11.Bots ML, Hoes AW, Koudstaal PJ. Common carotis intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam study. Circulation. 1997;96:1432–1437. doi: 10.1161/01.cir.96.5.1432. [DOI] [PubMed] [Google Scholar]
- 12.Erbel R, Schmermund A, Möhlenkamp S, Sack S, Baumgart D. Electron-beam computed tomography for detection of early signs of coronary arteriosclerosis. Eur Heart J. 2000;21:720–732. doi: 10.1053/euhj.1999.1881. [DOI] [PubMed] [Google Scholar]
- 13.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 14.Hunold P, Vogt FM, Schmermund A, et al. Radiation exposure during cardiac CT: effective doses at multi-detector row CT and electron-beam CT. Radiology. 2003;226:145–152. doi: 10.1148/radiol.2261011365. [DOI] [PubMed] [Google Scholar]
- 15.Bild DE, Detrano R, Peterson D. Ethnic differences in coronary calcification: the Multhi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2005;111:1313–1320. doi: 10.1161/01.CIR.0000157730.94423.4B. [DOI] [PubMed] [Google Scholar]
- 16.Schmermund A, Möhlenkamp S, Berenbein S. Population-based assessment of subclinical coronary atherosclerosis using electron-beam computed tomography. Atherosclerosis. 2006;185:177–182. doi: 10.1016/j.atherosclerosis.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 17.Stang A, Moebus S, Möhlenkamp S. Algorithms for converting random-zero to automated oscillometric blood pressure values, and vice versa. Am J Epidemiol. 2006;164:85–94. doi: 10.1093/aje/kwj160. [DOI] [PubMed] [Google Scholar]
- 18.Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation and treatment of high blood cholesterol in adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 19.Möhlenkamp S, Schmermund A, Lehmann N, et al. for the Heinz Nixdorf Recall Study Investigators. Subclinical coronary atherosclerosis and resting ECG abnormalities in an unselected general population. Atherosclerosis. 2007 doi: 10.1016/j.atherosclerosis.2007.01.012. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 20.Kröger K, Stang A, Kondratieva J, et al. Prevalence of peripheral arterial disease - results of the Heinz Nixdorf Recall Study. Eur J Epidemiol. 2006;21:279–285. doi: 10.1007/s10654-006-0015-9. [DOI] [PubMed] [Google Scholar]
- 21.Greenland P, Bonow RO, Brundage BH, et al. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain. A Report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography). Developed in collaboration with the society of atherosclerosis imaging and prevention and the society of cardiovascular computed tomography. Circulation. 2007;115:402–426. doi: 10.1161/CIRCULATIONAHA..107.181425. [DOI] [PubMed] [Google Scholar]
- 22.Dragano N, Verde PE, Moebus S, et al. on behalf of the Heinz Nixdorf Recall Study Group. Subclinical coronary atherosclerosis is more pronounced in men and women with lower socioeconomic status. Associations in a population based study. Eur J Cardiovasc Prev Rehabil. 2007;14:568–574. doi: 10.1097/HJR.0b013e32804955c4. [DOI] [PubMed] [Google Scholar]
- 23.Hoffmann B, Moebus S, Möhlenkamp S, et al. for the Heinz Nixdorf Recall Study Investigative Group. Residential exposure to traffic is associated with coronary atherosclerosis. Circulation. 2007;116:489–496. doi: 10.1161/CIRCULATIONAHA.107.693622. [DOI] [PubMed] [Google Scholar]
- 24.McClelland RL, Chung H, Detrano R, Post W, Kronmal RA. Distribution of coronary artery calcium by race, gender and age: results from the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2006;113:30–37. doi: 10.1161/CIRCULATIONAHA.105.580696. [DOI] [PubMed] [Google Scholar]
- 25.Diehm C, Lange S, Darius H, et al. for the get ABI Study Group. Association of low ankle brachial index with high mortality in primary care. Eur Heart J. 2006;27:1743–1749. doi: 10.1093/eurheartj/ehl092. [DOI] [PubMed] [Google Scholar]
- e1.Marmot M, Elliott P, editors. Coronary heart disease epidemiology: From etiology to public health. 2. ed. Oxford: Oxford University Press; 2005. [Google Scholar]
- e2.Marmot M, Wilkinson RG, editors. Social determinants of health. 2.ed. Oxford: Oxford University Press; 2006.. [Google Scholar]
- e3.Brook RD, Franklin B, Cascio W, et al. Air pollution and cardiovascular disease: a statement for healthcare professionals from the Expert Panel on Population and Prevention Science of the American Heart Association. Circulation. 2004;109:2655–2671. doi: 10.1161/01.CIR.0000128587.30041.C8. [DOI] [PubMed] [Google Scholar]
- e4.Hoek G, Brunekreef B, Goldbohm S, Fischer P, van den Brandt PA. Association between mortality and indicators of traffic-related air pollution in the Netherlands: a cohort study. Lancet. 2002;360:1203–1209. doi: 10.1016/S0140-6736(02)11280-3. [DOI] [PubMed] [Google Scholar]
- e5.Miller KA, Siscovick DS, Sheppard L, et al. Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med. 2007;356:447–458. doi: 10.1056/NEJMoa054409. [DOI] [PubMed] [Google Scholar]
- e6.Zhu Y, Hinds WC, Kim S, Sioutas C. Concentration and size distribution of ultrafine particles near a major highway. J Air Waste Manag Assoc. 2002;52:1032–1042. doi: 10.1080/10473289.2002.10470842. [DOI] [PubMed] [Google Scholar]
- e7.Taylor AJ, Merz CN, Udelson JE. 34th Bethesda Conference: Executive summary „Can atherosclerosis imaging techniques improve the detection of patients at risk for ischemic heart disease?“. J Am Coll Cardiol. 2003;41:1860–1862. doi: 10.1016/s0735-1097(03)00363-2. [DOI] [PubMed] [Google Scholar]
- e8.Wilson PW, Smith SC, Jr, Blumenthal RS, Burke GL, Wong ND. Task Force 4 - How do we select patients for atherosclerosis imaging? J Am Coll Cardiol. 2003;41:1898–1906. doi: 10.1016/s0735-1097(03)00361-9. [DOI] [PubMed] [Google Scholar]
- e9.McDermott MM, Mandapat AL, Moates A, et al. Knowledge and attitudes regarding cardiovascular disease risk and prevention in patients with coronary or peripheral arterial disease. Arch Intern Med. 2003;163:2157–2162. doi: 10.1001/archinte.163.18.2157. [DOI] [PubMed] [Google Scholar]
- e10.Beckman JA, Jaff MR, Creager MA. The United States preventive services task force recommendation statement on screening for peripheral arterial disease: more harm than benefit? Circulation. 2006;114:861–866. doi: 10.1161/CIRCULATIONAHA.105.607846. [DOI] [PubMed] [Google Scholar]
- e11.McDermott MM, Liu K, Criqui MH, et al. Ankle-brachial index and subclinical cardiac and carotid disease: the multi-ethnic study of atherosclerosis. Am J Epidemiol. 2005;162:33–41. doi: 10.1093/aje/kwi167. [DOI] [PubMed] [Google Scholar]
- e12.Pignoli P, Tremoli E, Poli A, Oreste P, Paoletti R. Intimal plus medial thickness of arterial wall: a direct measurement with ultrasound imaging. Circulation. 1986;74:1399–1406. doi: 10.1161/01.cir.74.6.1399. [DOI] [PubMed] [Google Scholar]
- e13.O’Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK Cardiovascular Health Study Collaborative Research Group. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. N Engl J Med. 1999;340:14–22. doi: 10.1056/NEJM199901073400103. [DOI] [PubMed] [Google Scholar]
- e14.Lorenz MW, von Kegler S, Steinmetz H, Markus HS, Sitzer M. Carotid intima-media thickening indicates a higher vascular risk across a wide age range: prospective data from the Carotid Atherosclerosis Progression Study (CAPS) Stroke. 2006;37:87–92. doi: 10.1161/01.STR.0000196964.24024.ea. [DOI] [PubMed] [Google Scholar]
- e15.Greenland P, Knoll MD, Stamler J, et al. Major risk factors as antecedents of fatal and nonfatal coronary heart disease events. JAMA. 2003;290:891–897. doi: 10.1001/jama.290.7.891. [DOI] [PubMed] [Google Scholar]
- e16.Raggi P, Callister TQ, Cooil B, et al. Identification of patients as increased risk of first unheralded acute myocardial infarction by electron-beam computed tomography. Circulation. 2000;101:850–855. doi: 10.1161/01.cir.101.8.850. [DOI] [PubMed] [Google Scholar]
- e17.Hoff JA, Chomka EV, Krainik AJ, Daviglus M, Rich S, Kondos GT. Age and gender distributions of coronary artery calcium detected by electron beam tomography in 35,246 adults. Am J Cardiol. 2001;87:1335–1339. doi: 10.1016/s0002-9149(01)01548-x. [DOI] [PubMed] [Google Scholar]
- e18.Mitchell TL, Pippin JJ, Devers SM, et al. Age- and sex-based nomograms from coronary artery calcium scores as determined by electron beam computed tomography. Am J Cardiol. 2001;87:453–456. doi: 10.1016/s0002-9149(00)01403-x. [DOI] [PubMed] [Google Scholar]
- e19.Nasir K, Raggi P, Rumberger JA, et al. Coronary artery calcium volume scores on electron beam tomography in 12,936 asymptomatic adults. Am J Cardiol. 2004;93:1146–1149. doi: 10.1016/j.amjcard.2004.01.043. [DOI] [PubMed] [Google Scholar]
- e20.Möhlenkamp S, Lehmann N, Schmermund A, et al. Prognostic value of extensive coronary calcium quantities in symptomatic males - a 5-year follow-up study. Eur Heart J. 2003;24:845–854. doi: 10.1016/s0195-668x(02)00826-6. [DOI] [PubMed] [Google Scholar]
- e21.Achenbach S, Schmermund A, Erbel R, et al. Detection of coronary calcifications by electron beam tomography and multislice spiral CT: clinical relevance. Z Kardiol. 2003;92:899–907. doi: 10.1007/s00392-003-0993-5. [DOI] [PubMed] [Google Scholar]
- e22.Bild DE, Bluemke DA, Burke GL, et al. Multi-ethnic study of atherosclerosis: objektives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- e23.Schmermund A, Möhlenkamp S, Stang A, et al. Assessment of clinically silent atherosclerotic disease and established and novel risk factors for predicting myocardial infarction and cardiac death in healthy middle-aged subjects: Rationale and design of the Heinz Nixdorf RECALL Study. Am Heart J. 2002;144:212–218. doi: 10.1067/mhj.2002.123579. [DOI] [PubMed] [Google Scholar]
- e24.Kitamura A, Iso H, Imano H, et al. Carotid intima-media thickness and plaque characteristics as a risk factor for stroke in Japanese elderly men. Stroke. 2004;35:2788–2794. doi: 10.1161/01.STR.0000147723.52033.9e. [DOI] [PubMed] [Google Scholar]
- e25.Babisch WF, Beule B, Schust M, Kersten N, Ising H. Traffic noise and risk of myocardial infarction. Epidemiology. 2005;16:33–40. doi: 10.1097/01.ede.0000147104.84424.24. [DOI] [PubMed] [Google Scholar]
- e26.Stang A, Moebus S, Dragano N, et al. Baseline recruitment and analyses of nonresponse of the Heinz Nixdorf Recall Study: Identifiability of phone numbers as the major determinant of response. Eur J Epidemiol. 2005;20:489–496. doi: 10.1007/s10654-005-5529-z. [DOI] [PubMed] [Google Scholar]
- e27.Dragano N, Bobak M, Wege N, et al. Neighbourhood socioeconomic status and cardiovascular risk factors: a multilevel analysis of nine cities in the Czech Republic and Germany. BMC Public Health. 2007;7:255. doi: 10.1186/1471-2458-7-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e28.Wege N, Dragano N, Moebus S, et al. When does work stress hurt? Testing the interaction with socioeconomic position in the Heinz Nixdorf Recall Study. J Epidemiol Commun Health. 2007 doi: 10.1136/jech.2007.062315. (im Druck/in press) [DOI] [PubMed] [Google Scholar]
- e29.Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using rist factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- e30.Criqui MH, Fronek A, Klauber MR, Barrett-Connor E, Gabriel S. The sensitivity, specifity, and predictive value of traditional clinical evaluation of peripheral arterial disease: results from non-invasive testing in a defined population. Circulation. 1985;71:516–522. doi: 10.1161/01.cir.71.3.516. [DOI] [PubMed] [Google Scholar]
- e31.Heald CL, Fowkes FG, Murray GD, Price JF. Risk of mortality and cardiovascular disease associated with the ankle-brachial index: Systematic review. Atherosclerosis. 2006;189:61–69. doi: 10.1016/j.atherosclerosis.2006.03.011. [DOI] [PubMed] [Google Scholar]
- e32.Taylor A, Shaw LJ, Fayad Z, et al. Tracking atherosclerosis regression: a clinical tool in preventive cardiology. Atherosclerosis. 2005;180:1–10. doi: 10.1016/j.atherosclerosis.2004.12.024. [DOI] [PubMed] [Google Scholar]
- e33.Meijer R, Grobee DE, Bots ML. Mannnheim consensus on carotid intima-media thickness: opposite and complementary points of view. Cerebrovasc Dis. 2006;21:415–416. doi: 10.1159/000092129. [DOI] [PubMed] [Google Scholar]
- e34.Budhoff MJ, Achenbach S, Blumenthal RS, et al. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on cardiovascular imaging and intervention, Council on Cardiovacular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation. 2006;114:1761–1791. doi: 10.1161/CIRCULATIONAHA.106.178458. [DOI] [PubMed] [Google Scholar]
- e35.Hoffmann B, Moebus S, Stang A, et al. on behalf of the Heinz Nixdorf Recall Study Investigation Group. Residence close to high traffic and prevalence of coronary heart disease. Eur Heart J. 2006;27:2696–2702. doi: 10.1093/eurheartj/ehl278. [DOI] [PubMed] [Google Scholar]
- e36.Carr JJ, Nelson JC, Wong ND, et al. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of multi-ethnic study of atherosclerosis (MESA) and coronary artery risk development in young adults (CARDIA) study. Radiology. 2005;234:35–43. doi: 10.1148/radiol.2341040439. [DOI] [PubMed] [Google Scholar]
- e37.Redberg RF. Coronary artery calcium: should we rely on this surrogate marker? Circulation. 2006;113:336–337. doi: 10.1161/CIRCULATIONAHA.105.600676. [DOI] [PubMed] [Google Scholar]
- e38.Schmermund A, Erbel R, Silber S. Age and gender distribution of coronary artery calcium measured by four-slice computed tomography in 2,030 persons with no symptoms of coronary artery disease. Am J Cardiol. 2002;90:168–173. doi: 10.1016/s0002-9149(02)02445-1. [DOI] [PubMed] [Google Scholar]
- e39.Lynch JW, Kaplan GA, Cohen RD, Tuomilehto J, Salonen JT. Do cardiovascular risk factors explain the relation between socioeconomic status, risk of all-cause mortality, cardiovascular mortality, and acute myocardial infarction? Am J Epidemiol. 1996;144:934–942. doi: 10.1093/oxfordjournals.aje.a008863. [DOI] [PubMed] [Google Scholar]
- e40.Oberdörster G. Pulmonary effects of inhaled ultrafine particles. Int Arch Occup Environ Health. 2001;74:1–8. doi: 10.1007/s004200000185. [DOI] [PubMed] [Google Scholar]
- e41.Kim JY, Chen JC, Boyce PD, Christiani DC. Exposure to welding fumes is associated with acute systemic inflammatory responses. Occup Environ Med. 2005;62:157–163. doi: 10.1136/oem.2004.014795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e42.Erbel R, Möhlenkamp S, Lehmann N, et al. on behalf of the Heinz Nixdorf Recall Study Investigative Group. Sex related cardiovascular risk stratification based on quantification of atherosclerosis and inflammation. Atherosclerosis. 2007 doi: 10.1016/j.atherosclerosis.2007.02.031. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]