Abstract
Objective
The objective of these two studies was to assess the efficacy of FL-41 tinted lenses in the treatment of benign essential blepharospasm (BEB).
Design
A randomized crossover study and a randomized crossover case-control study.
Participants
The first study included 30 subjects with BEB. The second study included 26 subjects with BEB and 26 controls.
Methods
For the first study, subjects were randomized to wear either FL-41 or gray tinted lenses for 2 weeks. After a two-week washout period, the other lens was worn for 2 weeks. Questionnaires were completed at baseline, after the first lens, and after the second lens. In the second study, surface electromyography (EMG) was used to measure blink frequency, duration, and force while subjects read and wore FL-41, rose, or gray tinted lenses.
Main Outcome Measures
Questionnaires were used to assess perceptions of light sensitivity and the effect of light sensitivity on activities of daily living. EMG was used to measure blink frequency, duration, and force.
Results
Most participants observed improvement while wearing both FL-41 and gray tinted lenses. FL-41 tinted lenses provided superior improvement in the areas of reading, fluorescent light sensitivity, overall light sensitivity, blepharospasm frequency, and blepharospasm severity. FL-41 lenses reduced mean blink rate compared to both rose and gray tinted lenses, and reduced eyelid contraction force compared to rose tinted lenses.
Conclusions
FL-41 lenses provided both subjective and objective benefit to subjects with BEB. Physicians should consider recommending this noninvasive and inexpensive lens tint to patients with BEB.
Benign essential blepharospasm (BEB) is a movement disorder characterized by involuntary spasmodic contractions of the orbicularis oculi. More than 50,000 people, most over age 50 and female, are estimated to have BEB in the United States, with 1,500-2,000 new diagnoses annually.(1) This physically and socially debilitating condition interferes significantly with visual performance, quality of life, and activities of daily living (ADL) such as driving, reading and shopping. In severe cases patients can be rendered functionally blind.(2-6)
Most BEB patients report photophobia, an aversive response and abnormal intolerance to light. The pain and discomfort of photophobia cause patients to avoid both ambient and bright light.(7-9) Previous research has indicated that BEB-associated light sensitivity may be a form of sympathetically maintained pain, supporting the hypothesis that BEB is a neurologic disease.(8)
Because of the limited understanding of the pathophysiology of both BEB and photophobia, treatment options have focused primarily on symptom control. One such option is the wearing of tinted lenses. BEB patients have reported a preference for FL-41, a rose-colored tint that blocks visible light at the green-to-blue end of the spectrum, over a variety of other tints.(10) We conducted two studies of FL-41 tinted lenses to assess the effects of photophobia in patients with BEB. First, we performed a randomized crossover study to compare the perceived improvement in light sensitivity and ADL provided by FL-41 lenses in subjects with BEB. We then used surface electromyography (EMG) to evaluate the effects of FL-41 on blink frequency, duration, and force in subjects with BEB and in controls.
Methods
Study Population
University of Utah Institutional Review Board (IRB)/Ethics Committee approval was obtained. All study procedures were performed in compliance with prevailing HIPAA regulations. All study subjects provided informed consent before participation.
BEB subjects were recruited from previous University of Utah BEB studies, Moran Eye Center outpatient clinics, and the Annual Meeting of the Benign Essential Blepharospasm Research Foundation. Some subjects participated in both studies. Because discussing the anticipated outcomes of the study could bias the results, the authors refrained from discussing the hypothesis and anticipated outcomes of the study with subjects.
BEB subjects were included if they had a history of involuntary contraction of the orbicularis oculi muscles for one year or more. One of the authors (MKB, RDL, KBD, GS, JW, BJK) interviewed and examined all participants to ensure that their symptoms were consistent with only BEB and not with other similar or related conditions (e.g. hemifacial spasm, oromandibular dystonia, facial tic, orbicularis myokymia, migraine headaches, iritis).
Subjects with prior use of tinted lenses prescribed for BEB were excluded from the subjective study because we were concerned that they would be biased toward favoring their chosen lenses. Because the objective (EMG) study should not be confounded by personal bias, subjects with prior lens use were not excluded.
Lenses
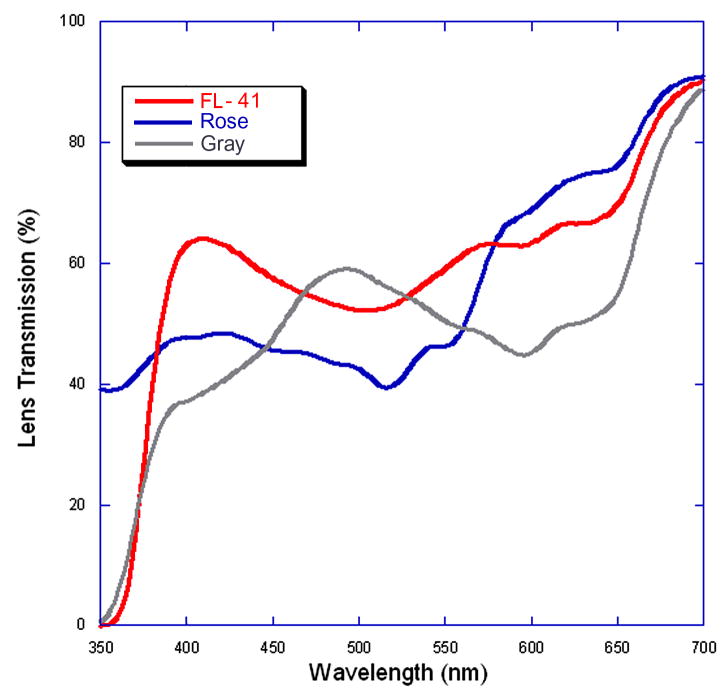
The lenses used in these two studies utilized three tints: FL-41, a standard gray tint, and a rose tint specifically designed to mimic FL-41. The gray tint was chosen to match that used in our previous investigations of BEB and to be representative of the standard tint used in sunglasses that one might purchase over-the-counter. The rose lenses were tinted in such a way as to be indistinguishable from FL-41 to both the investigators and the subjects. All lenses were custom tinted and manufactured to have equal optical densities of 55%. All lenses were examined for spectral characteristics using a spectrophotometer [Lambda 9; PerkinElmer Optoelectronics, Fremont, Calif]. The absorption spectra were compared, and the average percent visible transmission from 400-700 nm was calculated for each lens. The visible light transmission (VLT) was also calculated, as this is a common value used to characterize overall lens “darkness”. VLT is the mean of the visible transmission curve, in percent visible light, multiplied (weighted) by the photopic response function. The three lens tints differ in their spectral characteristics in that they all transmit the same amount of light overall, but differ in their transmission of various colors within the visible spectrum (Figure 1).
Figure 1.
Lens transmission spectra for lenses used in the study. Average percent visible transmission from 400-700 nm: FL-41=63.8%, rose=58.8%; gray=51.2%. Visible light transmission (mean of the visible transmission curve weighted by the photopic response function): FL-41=22.3%, rose=20.4%. gray=18.9%.
Subjects who already wore prescription lenses received clip-on frames with plano tinted lenses to place over their current spectacle correction. Participants who did not have prescription lenses wore plano tinted lenses in a standard spectacle frame.
Procedures
Patient Perceptions of FL-41 and Gray Lenses
Thirty patients with BEB completed a baseline questionnaire, and then were randomly assigned by coin toss to wear either gray or FL-41 tinted lenses. Patients wore the lenses at all times for two weeks, after which they completed a second questionnaire. Following the initial trial, the participants went through a two-week washout period, during which they did not wear any study-related lenses. They then switched to lenses with the opposite tint, which they wore at all times for a second two-week period. Finally, they completed a third and final questionnaire.
The baseline and second questionnaires used a six-level Likert scale to rank the improvement subjects perceived from 0 (no help) to 5 (very significant improvement). The areas assessed included photophobia specifically associated with being under fluorescent lights, overall light sensitivity, BEB frequency and severity, and performance of ADLs. The final questionnaire assessed improvement participants experienced while wearing the second pair of tinted lenses, and asked participants to directly compare the two tints and to choose the tint that most improved their BEB-associated symptoms.
EMG Measurement of Blink Frequency, Duration and Force
Thirteen participants with BEB and thirteen controls compared FL-41 with rose tinted lenses. Thirteen different BEB participants and thirteen different controls compared FL-41 with gray tinted lenses. Each participant with BEB first read under calibrated, ambient light (78 foot-candles, approximately 840 lux) for five minutes, wearing the tinted lenses to which he or she had been randomized. Next, each subject read for five minutes without spectacles, or wearing his or her usual, untinted reading spectacles. Finally, the subject read for five minutes using the other tint. Total testing time for each subject was approximately fifteen minutes. In order to standardize recording conditions, including ambient light, EMG was performed with the patient reading under calibrated ambient light. We did not have patients perform other tasks during recording such as watching television or viewing distant objects, as lighting conditions are difficult to control and could produce artifactual changes in blink parameters.
EMG was recorded from the left orbicularis oculi using 2 mm disc electrodes. A ground electrode was placed on the left earlobe. The EMG signal was collected with a Synergy EMG machine, using a low frequency filter of 20 Hz and a high frequency filter of 20 kHz (Viasys Health Care, Madison, WI). A five minute recording was obtained under each condition. Blink frequency was calculated over the entire five minute epoch. A customized, Windows-based software program measured the duration and root mean square (RMS) voltage of twenty randomly selected individual blinks.
EMG study subjects also filled out a baseline questionnaire to evaluate symptoms and their impact on quality of life and ability to perform ADLs. The questionnaire contained items similar to those assessed in previous studies conducted at this institution.(4, 11) Some questions were derived from a Mayo Clinic Survey on eyelid spasms.(12)
Statistical Methods
In a crossover study, each subject serves as his or her own control. Therefore, the Wilcoxon signed rank sum test, the non-parametric form of the paired t-test, was used to compare the improvement reported for the FL-41 versus the improvement reported for the gray lenses. The McNemar exact test was used to compare subjects who reported moderate or significant improvement (3, 4, or 5 on the Likert scale) to participants who reported no or minimal improvement (0, 1, or 2 on the Likert scale). A power analysis showed a sample size of 30 would achieve 80% power to find a difference in means of 0.5. Statistical analyses were performed by a biostatistician (WL) using STATA® version 8.2 for Windows (StataCorp LP, College Station, TX).
In the EMG study, the Wilcoxon signed-rank test was performed to compare the differences in blink frequency (blinks/minute), blink duration (milliseconds), and blink amplitude (microvolts) when subjects wore different lens tints. Results were considered statistically significant at a P value of < 0.05. Data analyses were performed by a biostatistician (RH).
Results
Patient Perceptions of FL-41 and Gray Lenses
Twenty subjects were female and 10 were male; mean age was 66 years. Average time since BEB diagnosis was 12 years. One-third of participants had undergone a myectomy, and two-thirds were currently receiving botulinum toxin injections. Because nearly all patients with BEB have dry eye syndrome, artificial tears had been recommended by the patients’ physicians as part of their treatment. The median overall photophobia score at the time of initial evaluation was 3.8 on a six-level Likert scale (0=none, 5=maximum severity). Utilizing the same Likert scale, baseline ADL impairment assessments ranged from 2.2 (shopping) to 3.3 (driving).
Patients perceived greater improvement while wearing FL-41 tinted lenses as compared to gray tinted lenses for all activities of daily living, light sensitivity, and blepharospasm frequency and severity (Table 1). This difference was statistically significant for all categories except driving and watching television.
Table 1.
Patient perceived improvement during activities of daily living (ADL) and in blepharospasm symptoms while wearing FL-41 and gray lenses
| ADL and Blepharospasm Symptoms | FL-41* | Gray* | P Value |
|---|---|---|---|
| Driving | 2.92 | 2.20 | 0.071 |
| Reading | 2.19 | 1.32 | 0.032 |
| Watching television | 2.11 | 1.54 | 0.118 |
| Shopping | 2.64 | 1.61 | 0.046 |
| Fluorescent light sensitivity | 2.83 | 1.87 | 0.006 |
| Overall light sensitivity | 3.00 | 2.40 | 0.017 |
| Blepharospasm frequency | 2.10 | 1.10 | 0.002 |
| Blepharospasm severity | 2.13 | 0.97 | 0.002 |
Table values are mean scores reported from a six-level Likert scale (0 = no help at all, 5 = marked improvement).
P values were determined using Wilcoxon sign rank sum test.
In each category, the proportion of participants who perceived improvement only with the FL-41 lens ranged from 17% to 31%, whereas the proportion reporting improvement only with the gray lens was less than 5%. The proportion of subjects who perceived improvement with both FL-41 and gray lenses ranged from 13 to 46%. The proportion of subjects who perceived no improvement or minimal improvement with either lens ranged from 33 to 57% (Table 2).
Table 2.
Proportion of patients who perceived moderate or very significant improvement with FL-41 lenses only, gray lenses only, or with both lens types for activities of daily living (ADL) and blepharospasm symptoms
| ADL and Blepharospasm Symptoms | FL-41 only | Gray only | Both | P-Value |
|---|---|---|---|---|
| Driving | 17% | 4% | 46% | 0.375 |
| Reading | 31% | 4% | 27% | 0.039 |
| Watching television | 26% | 4% | 26% | 0.070 |
| Shopping | 29% | 4% | 33% | 0.070 |
| Fluorescent light sensitivity | 28% | 3% | 41% | 0.039 |
| Overall light sensitivity | 27% | 3% | 43% | 0.039 |
| Blepharospasm frequency | 27% | 3% | 20% | 0.039 |
| Blepharospasm severity | 27% | 3% | 13% | 0.039 |
Table values are the proportion of patients reporting moderate to very significant improvement (3-5 on a six-level Likert scale where 0 =no improvement and 5 = very significant improvement).
P values were determined using McNemar’s exact test, which tests the difference between the proportion of patients who only perceived improvement with the FL-41 lens versus the proportion who only perceived improvement with the gray lens.
EMG Measurement of Blink Frequency, Duration and Force
Results from the baseline questionnaire revealed that nearly all of the 22 female and 4 male BEB subjects (mean age 62, mean time since diagnosis 10 years) considered themselves to be at least moderately light sensitive and reported greater light sensitivity during spasms than at other times. Furthermore, light sensitivity and eyelid spasms affected many ADL. Almost all subjects reported that they wore tinted spectacles or sunglasses outdoors to decrease eyelid spasms; many subjects also reported wearing them indoors.
Table 3 summarizes blink frequency, duration, and amplitude data for the comparison of FL-41 and rose tinted lenses. In control subjects, no significant differences were observed in these three parameters when we compared the FL-41 to the rose-tinted lenses. However, in BEB subjects, FL-41 lenses reduced the mean blink rate by 7.0 blinks/min compared to rose tint (P = 0.004). There was also a significant, 6.7 μV reduction in blink force (P = 0.016). There was no significant effect on blink duration.
Table 3.
Effect on blink parameters in blepharospasm and control subjects for no lens tint, FL-41 tint, and rose tint as measured by electromyography (EMG)
| Blink Frequency (Blinks/Min) | Blink Duration (ms) | Blink Amplitude (μV, RMS) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group | None | Rose | FL-41 | P | None | Rose | FL-41 | P | None | Rose | FL-41 | P |
| BEB | 28.3 (17.4) | 28.9 (18.4) | 21.9 (17.3) | 0.004 | 135.0 (45.2) | 142.7 (46.9) | 136.9 (38.5) | 0.463 | 37.6 (15.6) | 38.5 (12.2) | 31.8 (11.4) | 0.016 |
| Control | 23.0 (13.1) | 21.6 (14.0) | 22.6 (12.0) | 0.442 | 172.3 (19.1) | 161.4 (26.1) | 167.7 (24.2) | 0.311 | 41.4 (28.1) | 42.0 (31.6) | 36.7 (26.6) | 0.064 |
Table values are mean (standard deviation).
P values were determined from a Wilcoxon sign rank sum test and test the difference between values for the rose and FL-41 lenses.
ms, milliseconds; μV, microvolts; RMS, root mean square; BEB, benign essential blepharospasm
Table 4 summarizes results for the comparison of FL-41 and gray tinted lenses. In controls, we observed no significant differences in the three blink parameters when we compared the two tints. In BEB subjects, the FL-41 lenses reduced the mean blink rate by 6.4 blinks/min compared to the gray tint (P = 0.006). There was no significant effect on blink force or duration.
Table 4.
Effect on blink parameters in blepharospasm and control subjects for no lens tint, FL-41 tint, and gray tint as measured by electromyography (EMG)
| Blink Frequency (Blinks/Min) | Blink Duration (ms) | Blink Amplitude (μV, RMS) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group | None | Gray | FL-41 | P | None | Gray | FL-41 | P | None | Gray | FL-41 | P |
| BEB | 33.2 (17.0) | 32.1 (14.4) | 25.7 (14.7) | 0.006 | 160.6 (29.3) | 167.7 (40.4) | 163.5 (27.4) | 0.116 | 65.4 (38.3) | 65.7 (37.8) | 62.4 (42.6) | 0.116 |
| Control | 25.2 (14.6) | 23.1 (13.0) | 21.6 (12.3) | 0.221 | 192.8 (34.3) | 189.5 (35.5) | 208.4 (43.8) | 0.087 | 29.1 (19.7) | 27.4 (12.9) | 40.2 (43.1) | 0.173 |
Table values are mean (standard deviation).
P values were determined from a Wilcoxon sign rank sum test and test the difference between values for the gray and FL-41 lenses.
ms, milliseconds; μV, microvolts; RMS, root mean square; BEB, benign essential blepharospasm
Discussion
All BEB subjects in these studies have characteristics that are similar to those observed in our and others’ previous studies of light sensitivity and BEB. Specifically, our study participants report photophobia severe enough to require use of sunglasses and to cause detrimental effects on ADLs.(4, 11, 15-19)
Both studies demonstrate that our BEB participants derived a significant benefit from wearing FL-41 rather than lenses with another tint. The study of subjective perceptions documented participant-reported decreases in limitations experienced while performing ADL, as well as decreases in photophobia and spasms, while wearing FL-41 tinted lenses. In the study that utilized EMG recordings, we found that FL-41 lenses reduced blink frequency compared to both rose and gray tinted lenses. The reduction in RMS force of individual blink responses when comparing FL-41 to rose tinted lenses suggests a reduction in the amplitude of the abnormal contractions, given that RMS voltage is proportional to contraction force.
The reason for the effectiveness of FL-41 lenses in reducing BEB symptoms remains speculative. Patients with BEB appear to have a particular sensitivity to that part of the visible spectrum attenuated by FL-41. Thus, it appears that a physiologic difference exists between BEB and control subjects, who did not display this sensitivity in our investigation. This physiologic difference might involve one or more ocular mechanisms that transduce certain wavelengths of light into photophobia in patients with BEB. Our findings suggest that FL-41 lenses are better than other tints at blocking frequencies of light that aggravate BEB symptoms.
In another study we showed that although both FL-41 and gray lenses reduced photophobia, there was no significant difference between the two tints in the amount of light sensitivity reduction. This previous study took place in a somewhat artificial situation, in which subjects were seated in front of a bright, full-spectrum halogen lamp.(11) In the present studies, the participants wore the tinted lenses while performing “real life” tasks. Furthermore, rather than making a simple measurement of overall light sensitivity, we have measured blink frequency, duration, and force.
Both of these studies had limitations in design and implementation. The subjective perceptions investigation was not masked, as rose tinted lenses were not a component of the study. One criticism of the subjective study, which was conducted prior to the objective (EMG) study, was that subjects with knowledge of FL-41 could be biased toward favoring this lens. Therefore, when we subsequently conducted the objective study, we added a comparison with a non-FL-41 rose-colored lens. The subjective perceptions investigation did not include objective measures of blink frequency or force. Since we only used EMG to record blinking parameters during a single task, reading, it is not possible for us to generalize this result to other ADL.
It might be argued that the wide variation in blink parameters observed in all groups, including controls, constitutes a limitation of the EMG study. Previous studies of spontaneous blinking have observed that although normal adults blink at widely variable rates, the blink rate is constant for an individual under similar conditions.(13, 14, 20) The differences and range of blink frequencies found in our subjects are similar to these previous reports.
Not every BEB subject experienced subjective or objective improvement when wearing FL-41 tinted lenses. Therefore, FL-41 tinted lenses should not be used as the sole treatment for BEB, but rather as an adjuvant to commonly accepted medical and surgical therapies such as cholinergic medications, botulinum toxin injections and myectomy. It is also reasonable to surmise that other tinted lenses could be as effective as or more effective than FL-41 lenses. Future studies could be directed at experimenting with other tints that more sharply attenuate the frequencies of light blocked by FL-41.
Prescribing tinted spectacles is a safe, non-invasive, and inexpensive means of improving BEB symptoms. Because a sufficient number of participants derived benefit from the FL-41 tint, we recommend that physicians offer their patients this option for BEB symptom control. These tints are commercially available through Brain Power, Inc. (www.callbpi.com; accessed September 8, 2008), Phantom Research Laboratories, Inc. (www.phantomresearch.com; accessed September 8, 2008), and the John A. Moran Eye Center Optical Shop (http://uuhsc.utah.edu/MoranEyeCenter/patientcare/optical_shop.html; accessed September 8, 2008).
Acknowledgments
The authors thank Charles Swallow (John A Moran Optical Shop, Salt Lake City, UT) for providing the lenses used in this study; and the Benign Essential Blepharospasm Research Foundation, Beaumont, TX, for referring study participants.
Financial support: This work was supported by NIH T35 HL07744 (MKL and RDL); a grant to Drs. Digre and Katz from the Benign Essential Blepharospasm Research Foundation, Houston, TX, by NIH K23 RR16427 (BJK), and the University of Utah Huntsman General Clinical Research Center (NIH M01 RR000064). This work was also supported in by an unrestricted grant from Research to Prevent Blindness, Inc., New York, NY, to the Department of Ophthalmology and Visual Sciences, University of Utah. The sponsor and funding organizations had no role in the design or conduct of this research.
Profits from the John A. Moran Eye Center Optical Shop help to support the Department of Ophthalmology and Visual Sciences.
Footnotes
Conflicts of interest: SD Nandedkar has a proprietary interest in the use of the electromyographic amplifier and customized, Windows-based software program used to analyze blink parameters. The other authors have reported no actual or potential conflicts of interest.
Meeting presentations: This work was presented in part at the 31st annual meeting of the North American Neuro-Ophthalmology Society, Copper Mountain, Colorado, February 15th, 2005; and at the 32nd Annual Meeting of the North American Neuro-Ophthalmology Society, Tucson, Arizona, February 27th, 2006.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Faucett D. Essential blepharospasm. In: Yanoff M, Duker JS, editors. Ophthalmology. 2. St. Louis, MO: Mosby; 2004. pp. 695–7. [Google Scholar]
- 2.Hallett M. Blepharospasm: recent advances. Neurology. 2002;59:1306–12. doi: 10.1212/01.wnl.0000027361.73814.0e. [DOI] [PubMed] [Google Scholar]
- 3.Jankovic J, Orman J. Blepharospasm: demographic and clinical survey of 250 patients. Ann Ophthalmol. 1984;16:371–6. [PubMed] [Google Scholar]
- 4.Judd RA, Digre KB, Warner JE, et al. Shedding light on blepharospasm: a patient-researcher partnership approach to assessment of photophobia and impact on activities of daily living. Neuroophthalmology. 2007;31:49–54. [Google Scholar]
- 5.Patrinely J, Anderson RL. Essential blepharospasm: a review. Geriatr Ophthalmol. 1986;2:27–33. [Google Scholar]
- 6.Lindeboom R, De Haan R, Aramideh M, Speelman JD. The Blepharospasm Disability Scale: an instrument for the assessment of functional health in blepharospasm. Mov Disord. 1995;10:444–9. doi: 10.1002/mds.870100407. [DOI] [PubMed] [Google Scholar]
- 7.Fine PG, Digre KB. A controlled trial of regional sympatholysis in the treatment of photo-oculodynia syndrome. J Neuroophthalmol. 1995;15:90–4. [PubMed] [Google Scholar]
- 8.McCann JD, Gauthier M, Morschbacher R, et al. A novel mechanism for benign essential blepharospasm. Ophthal Plast Reconstr Surg. 1999;15:384–9. doi: 10.1097/00002341-199911000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Anderson RL, Patel BC, Holds JB, Jordan DR. Blepharospasm: past, present, and future. Ophthal Plast Reconstr Surg. 1998;14:305–17. [PubMed] [Google Scholar]
- 10.Herz NL, Yen MT. Modulation of sensory photophobia in essential blepharospasm with chromatic lenses. Ophthalmology. 2005;112:2208–11. doi: 10.1016/j.ophtha.2005.06.030. [DOI] [PubMed] [Google Scholar]
- 11.Adams WH, Digre KB, Patel BC, et al. The evaluation of light sensitivity in benign essential blepharospasm. Am J Ophthalmol. 2006;142:82–7. doi: 10.1016/j.ajo.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 12.Chapman KL, Bartley GB, Waller RR, Hodge DO. Follow-up of patients with essential blepharospasm who underwent eyelid protractor myectomy at the Mayo Clinic from 1980 through 1995. Ophthal Plast Reconstr Surg. 1999;15:106–10. doi: 10.1097/00002341-199903000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Zametkin AJ, Stevens JR, Pittman R. Ontogeny of spontaneous blinking and of habituation of the blink reflex. Ann Neurol. 1979;5:453–7. doi: 10.1002/ana.410050509. [DOI] [PubMed] [Google Scholar]
- 14.Karson CN, Berman KF, Donnelly EF, et al. Speaking, thinking, and blinking. Psychiatry Res. 1981;5:243–6. doi: 10.1016/0165-1781(81)90070-6. [DOI] [PubMed] [Google Scholar]
- 15.Müller J, Kemmler G, Wissel J, et al. The impact of blepharospasm and cervical dystonia on health-related quality of life and depression. J Neurol. 2002;249:842–6. doi: 10.1007/s00415-002-0733-1. [DOI] [PubMed] [Google Scholar]
- 16.Müller J, Wissel J, Kemmler G, et al. Craniocervical Dystonia Questionnaire (CDQ-24): development and validation of a disease-specific quality of life instrument. J Neurol Neurosurg Psychiatry. 2004;75:749–53. doi: 10.1136/jnnp.2003.013441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reimer J, Gilg K, Karow A, et al. Health-related quality of life in blepharospasm or hemifacial spasm. Acta Neurol Scand. 2005;111:64–70. doi: 10.1111/j.1600-0404.2004.00357.x. [DOI] [PubMed] [Google Scholar]
- 18.Hall TA, Jr, McGwin G, Searcey K, et al. Health-related quality of life and psychosocial characteristics of patients with benign essential blepharospasm. Arch Ophthalmol. 2006;124:116–9. doi: 10.1001/archopht.124.1.116. [DOI] [PubMed] [Google Scholar]
- 19.Tucha O, Naumann M, Berg D, et al. Quality of life in patients with blepharospasm. Acta Neurol Scand. 2001;103:49–52. doi: 10.1034/j.1600-0404.2001.00109.x. [DOI] [PubMed] [Google Scholar]
- 20.Ponder E, Kennedy WP. On the act of blinking. Q J Exp Physiol. 1927;18:89–110. [Google Scholar]