Abstract
This work assesses the temporal resolution of dual-source CT in a visually intuitive manner. Exploiting the principles of ring artifact creation, a phantom containing a highly attenuating delta function signal (a wire) was rotated at the same speed as the gantry, creating a partial ring artifact where the angular extent of the artifact provides a direct indication of the temporal resolution. A demonstration of the effect of the evaluated 165 and 83 ms nominal temporal resolutions on motion artifacts in cardiac CT is provided using patient data.
Introduction
This work describes the assessment of temporal resolution and motion artifact of a dual-source CT system (Somatom Definition, Siemens Medical Solutions, Forchheim, Germany) 1–3. This system has two x-ray sources and two detector arrays mounted orthogonally on the gantry. The primary tube (Tube A) and detector array images a 50-cm field of view (FOV), while the secondary system (Tube B) images a 26-cm FOV. Each tube/detector array pair has an 80-kW generator, a 32 × 0.6 mm detector array and uses double z sampling to acquire 64 overlapping projections along the z axis at every tube position 4.
When the system is operated using only a single x-ray tube and detector array and a gantry rotation time of 330 ms, the nominal temporal resolution near isocenter for partial scan reconstructions is 165 ms 5. This is because, at isocenter, 180° of fan beam data are sufficient to provide 180° of rebinned parallel data. If redundant data from the fan beam are ignored, the temporal resolution at isocenter can be as good as one half of the gantry rotation time. When both tube/detector systems are used, the nominal temporal resolution for partial scan reconstructions (180 deg) is 83 ms because each tube provides one half of the required data, or one quarter of the gantry rotation time 1, 3.
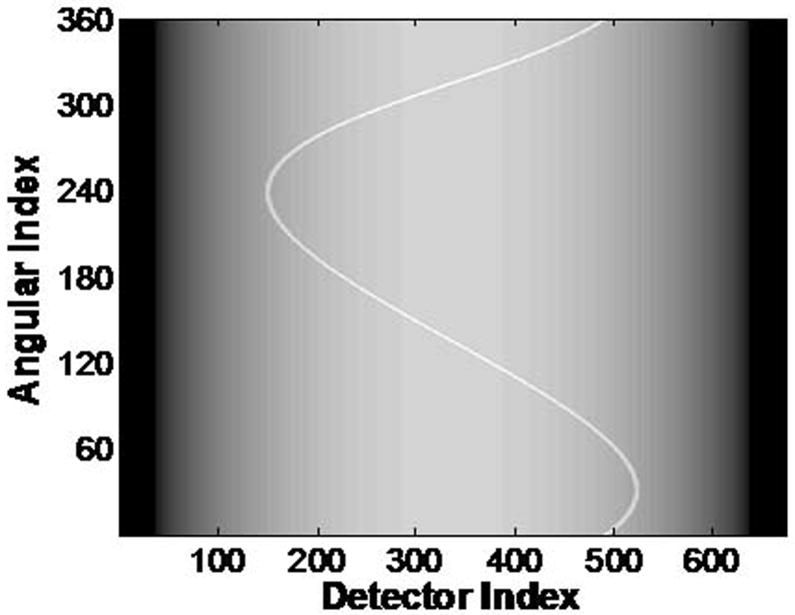
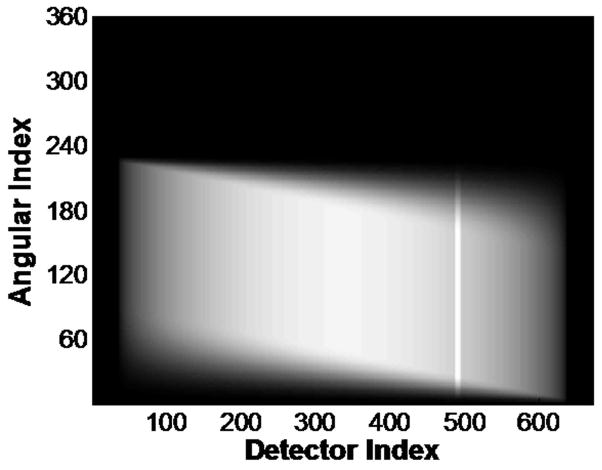
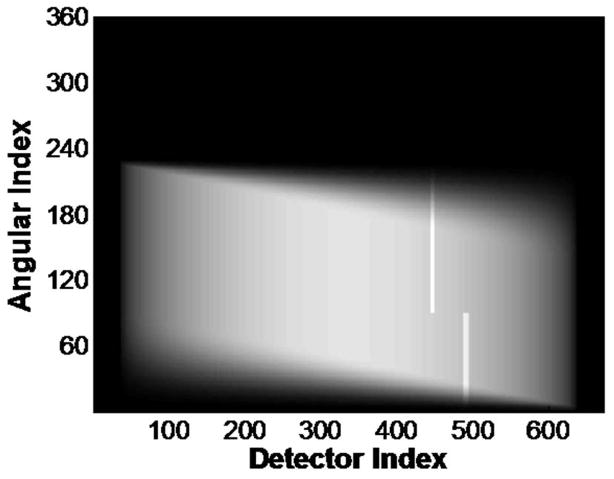
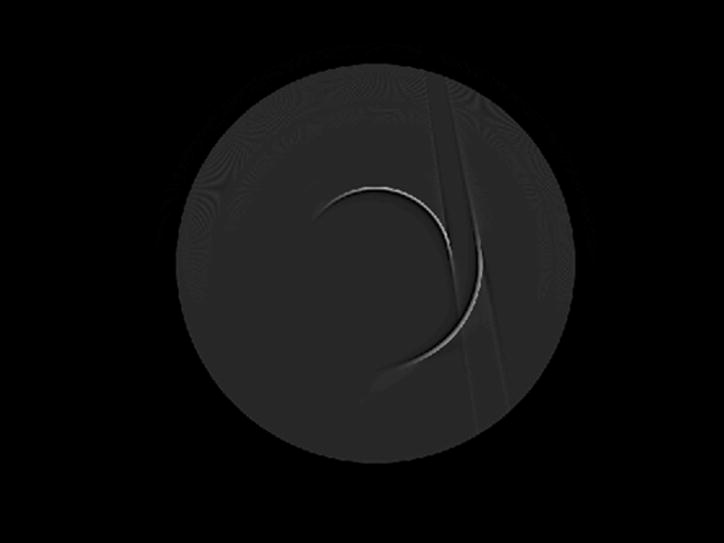
In this work, we describe a visually intuitive manner by which to measure temporal resolution. The method exploits the principles responsible for ring artifacts in 3rd generation CT geometry (where the x-ray tube and detector assembly rotate in synchrony) 5. This principle is demonstrated in Fig. 1. In Fig. 1a, the sinogram corresponding to a simulated uniform cylinder containing a highly attenuating ”delta function” is shown. When the simulated phantom is static, the sinusoidal curve in the sinogram represents the projection of the attenuating point onto different detector elements as the tube is rotated about the object. In Fig. 1b, we have simulated the condition when the same phantom is rotated at the same angular velocity of the x-ray tube. In this case, the projected attenuation from the small bright object is mapped to a vertical line in the sinogram. The vertical line in the simulated sinogram is similar to that which occurs when a specific ray sum is affected in the same way at every projection angle, such as would occur in the case of one bad detector element. After image reconstruction, the result is a circular or ring artifact. If, for some reason, less than 360° of data are used for the image reconstruction process, the ring would be an incomplete circle, covering only the angular range included in the image reconstruction (Fig. 2). In the case of DSCT, the use of two sources, each acquiring half of the required projections, creates two arcs, each one reflecting the temporal resolution associated with the image. The purpose of this work was to assess the temporal resolution of dual-source CT (DSCT) using the described visually intuitive method and to demonstrate the reduction in motion artifact between 83 and 165 ms images using patient data.
Figure 1.
Simulation of sinograms (a, c) and corresponding reconstructed images (b,d) of a highly-attenuating “delta function” object in a uniformly dark cylindrical background for a stationary phantom and full-scan (360°) reconstruction (a, b) and the same phantom rotated at the same speed and direction as the gantry (c, d), also with a full-scan reconstruction. A ring artifact is created in 3rd generation CT when a ray sum is corrupted, typically due to a bad detector or problem with the x-ray source. The same effect occurs if a ray sum is blocked for every projection angle, in this case due to synchronous rotation of the gantry and phantom. If less than 360° are used in the scan reconstruction, the ring will be incomplete, covering only the angular range included in the image reconstruction. The radius of the ring in the reconstructed image depends on the position of the wire in the field of view at the beginning of the scan, which determines the location of the wire’s signal at a specific detector in the sinogram.
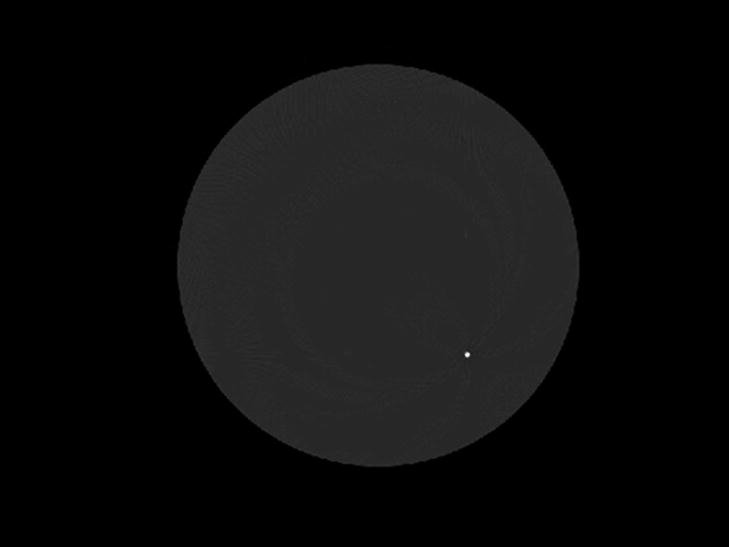
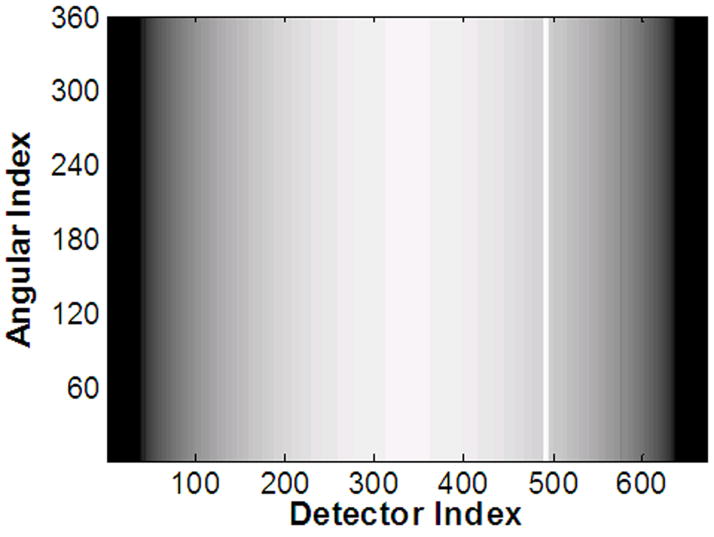
Figure 2.
Simulations of sinograms (a, c) and corresponding reconstructed images (b, d) of the same phantom shown in Figure 1. (a, b) The phantom was rotated at the same speed and direction as the gantry. The image was reconstructed from half-scan (180° + fan angle) data after smoothing of the sinogram using the Parker weighting. (c, d) The phantom was rotated at the same speed and direction as the gantry, while the image was reconstructed from the half-scan data formed from the combination of data acquired by two orthogonal x-ray sources. This sinogram was also smoothed by using the Parker weighting. Each x-ray source produces an arc that independently corresponds to the temporal resolution of the scan. Thus, two one-quarter rotation arcs are generated
Materials and Methods
Measurement of temporal resolution using a rotating phantom
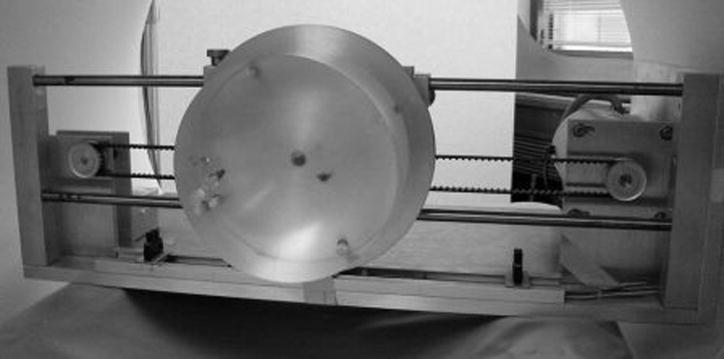
The phantom used to attenuate the ray sums corresponding to a small number of detectors was comprised of a narrow gauge needle inserted at a radius of 4 cm into a 15-cm diameter acrylic cylinder. The needle essentially creates a highly-attenuating “delta function” signal in the image FOV. The acrylic cylinder was mounted to a computer-controlled drive and imaged at rest and while spinning at 3 rotations/s (Fig. 3). Verification of the angular velocity of the rotating cylinder was performed by video recording the spinning phantom using the fast frame rate mode (60 fps) and playing back the data in slow motion to count the number of rotations per second of the needle (Handycam DCR-TRV460, Sony Electronics, Inc, San Diego, CA; iMovie 7.0, Apple Computers, Cupertino, CA). Because both the phantom and the gantry rotated with the same speed, a partial “ring” artifact was created. Thus, the angular extent of the ring artifact provided a direct visual indication of temporal resolution near isocenter.
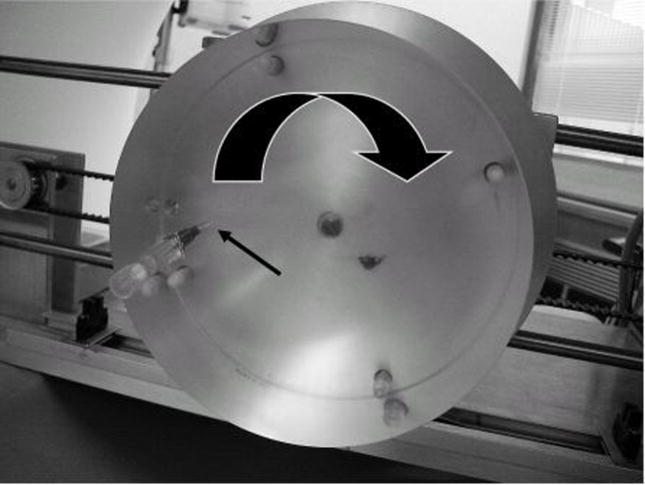
Figure 3.
(a) Photograph of the motion apparatus within the gantry of the CT system and a close-up of the phantom (b). The 22 gauge hypodermic needle inserted into the 15 cm acrylic cylinder is indicated by the narrow black arrow. The large arrow indicates the direction of rotation. The screws that mount the acrylic phantom to the metal plate of the motion apparatus are visible through the clear acrylic. Using a computer-controlled stepping motor, the phantom was rotated at 3 rotations per second to match the rotation time of the gantry. (c) A CT image of the static phantom demonstrates the appearance of the metal needle.
Five images of the rotating cylinder were acquired using each of the following modes: 1) axial single-source, 2) axial dual-source, and 3) helical dual-source. Partial (cardiac) reconstructions were performed on both axial data sets to produce 83 (dual-source) and 165 ms (single-source) images. Partial (cardiac) reconstructions were also performed on the dual-source helical data set to produce 83 and 165 ms images, using approximately 90 and 180° of projection data for each x-ray tube, respectively. This resulted in a total of 20 images.
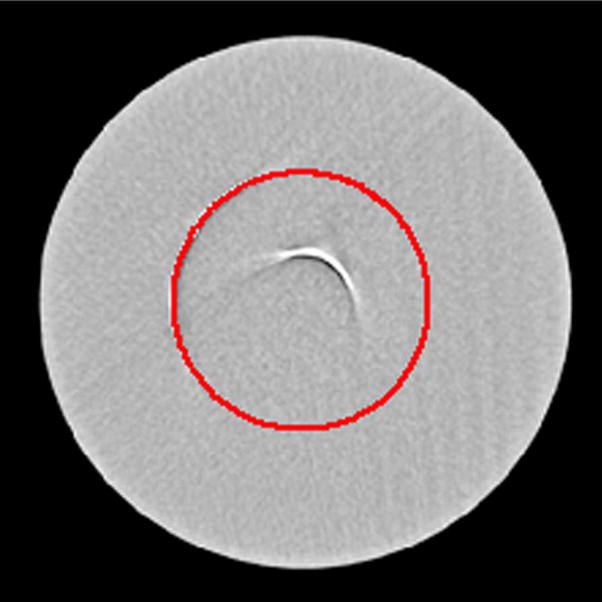
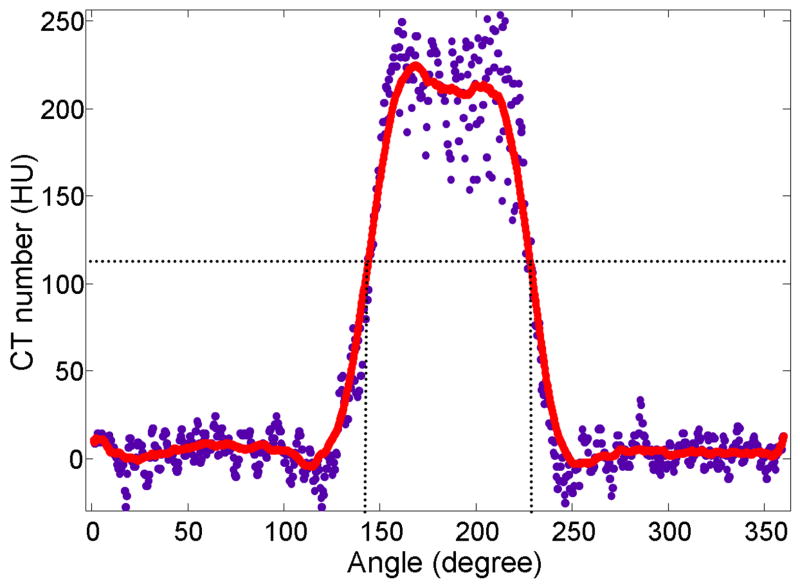
The angular extent of each partial ring artifact was measured by using a circle to fit the radius of curvature of each arc. The diameter and position of a circle were manually varied to achieve the best fit to the partial ring artifact, where the best fit was determined by visual inspection. The CT numbers along the path of the circle were sampled using 1440 points to generate a one-dimensional profile of CT number vs. angular position. The data were background corrected by subtracting the mean CT number from a background region distant from the wire (120 HU) from each data point. The resultant profile was smoothed using a 101-point window width, and the full-width-at-half-maximum (FWHM) of the smoothed profile used to estimate the corresponding temporal resolution. The method used to quantify temporal resolution, as represented by the partial ring artifact, is demonstrated in Fig. 5. The mean and standard deviation were calculated for the 5 images from each of the 4 scan modes (axial and helical 83 ms and axial and helical 165 ms).
Figure 5.
Demonstration of the method used to measure the angular extent of the partial ring artifact. a) The image shown in Figure 4a with a circle manually fit to the radius of curvature of the outermost arc. b) Plot of the background-corrected CT number versus angular position of the values underneath the circle overlay (blue data points). A 101-voxel wide sliding average smoothing was performed (red line) to reduce the influence on noise. The FWHM of the smoothed profile was used to quantitate the temporal resolution of the associated scan mode.
Demonstration of the effect of temporal resolution on motion artifact for cardiac CT
Data from a patient having a mean heart rate of 90 bpm were reconstructed using either one or both x-ray tube(s). First, the data from both tubes were used for the commercially implemented dual source reconstruction (nominal 83 ms). Second, with assistance from the manufacturer, the reconstruction algorithm was modified to disregard data from tube B, and a single-source reconstruction was performed using only data from tube A (nominal 165 ms). This approach was required in order to reconstruct 165 ms images from the identical helical dataset (i.e. without rescanning the patient) and to ensure equivalent image noise between the 83 and 165 ms images.
Results and Discussion
The angular velocity of the rotating phantom was measured using video photography to be 2.994 rotations/sec, which is in excellent agreement with the programmed speed (3 rotations/sec).
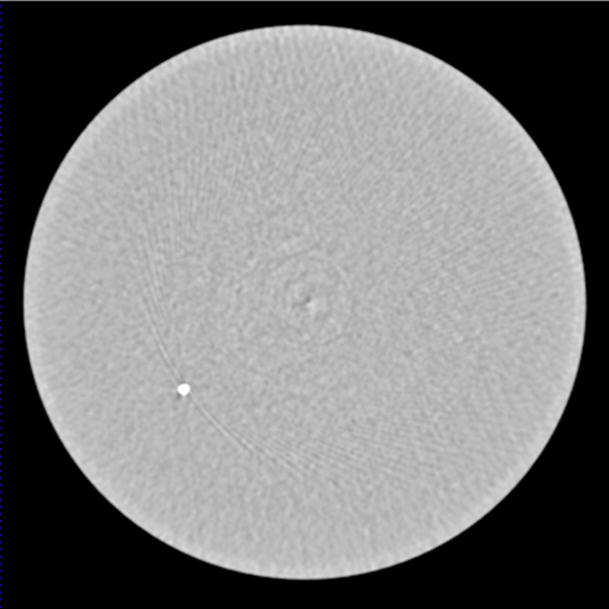
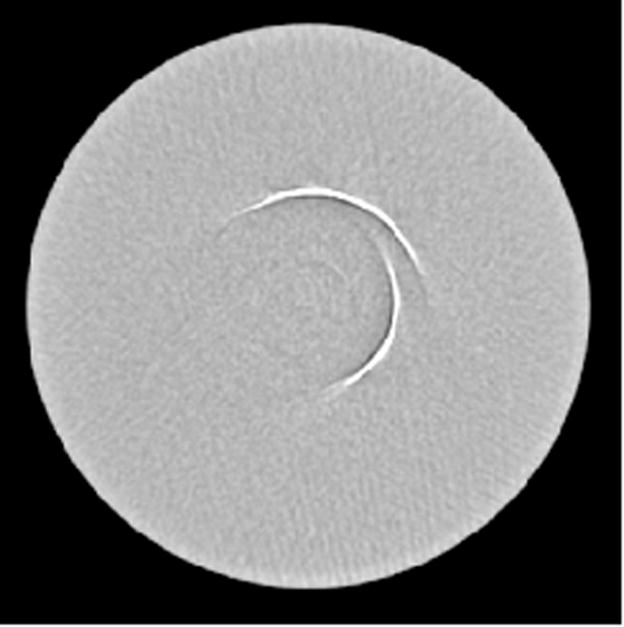
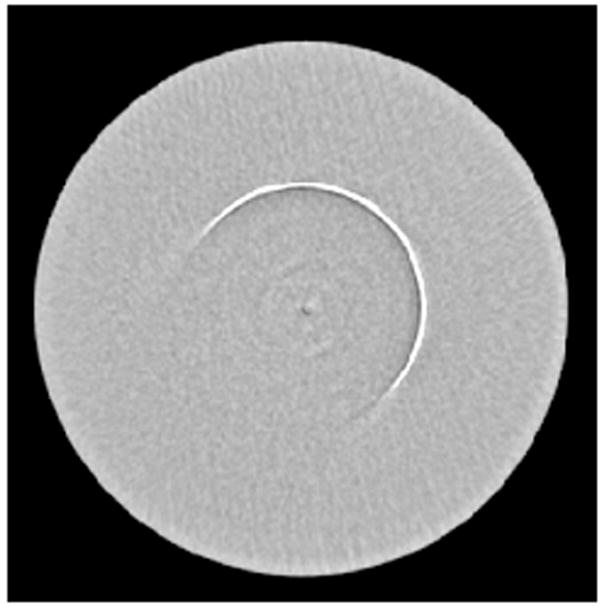
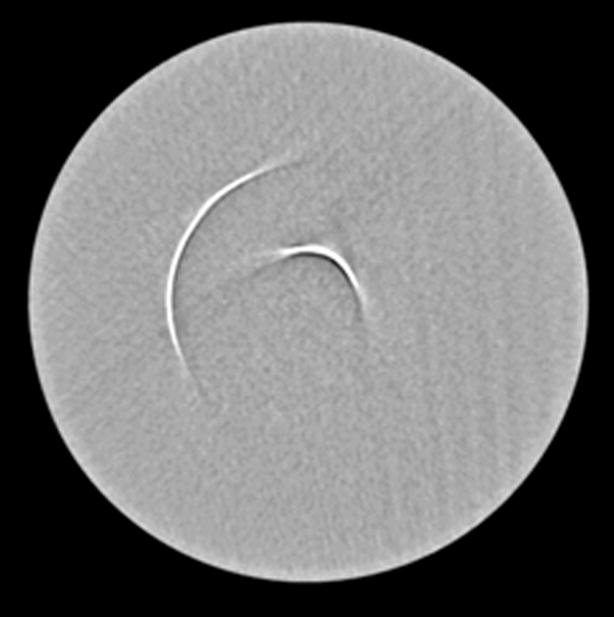
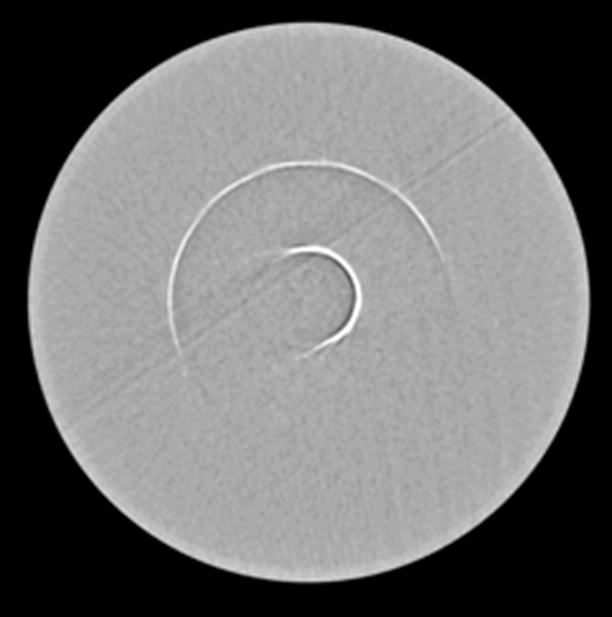
In Fig. 4a and 4c, the angular extent of the arcs appear to be approximately 90°, which is consistent with a temporal resolution of 83 ms for a gantry rotation time of 330 ms (90°/360° × 330 ms= 83 ms). In Fig 4b and 4d, the angular extent of the arcs appear to be approximately 180°, which is consistent with a temporal resolution of 165 ms for a gantry rotation time of 330 ms (180°/360° × 330 ms= 165 ms). Figs. 4a, 4c, and 4d each were reconstructed using data from both tubes, hence the presence of two arcs, each of which independently represents the temporal resolution of the image.
Figure 4.
(a) Partial scan reconstruction performed using data from both Tube A and Tube B (i.e. a cardiac dual-source reconstruction) for the axial scan acquisition. The mean angular extent of the partial ring artifacts (n=5) was 87.6°, which corresponds to 80.3 ms. (b) Partial scan reconstruction using only data from Tube A (i.e. a cardiac single-source reconstruction) for the axial scan reconstruction. The mean angular extent of the partial ring artifacts (n=5) was 177.2°, which corresponds to a temporal resolution of 162.4 ms. (c) Partial scan reconstruction performed using data from both tubes for the helical scan acquisition. The angular extent of the partial ring artifacts (n=5) was 87.4°, which corresponds to 80.1 ms. (d) Partial scan reconstruction performed using 180° of projection data from both tube A and tube B for the helical scan acquisition. Reconstruction of the longer temporal window (165 ms) from a dual-source helical scan is a reconstruction option on the CT system used. The mean angular extent of the partial ring artifacts (n=5) was 182.2°, which corresponds to a temporal resolution of 167.0 ms.
The FWHM (mean±standard deviation) of the angular ranges associated with the images in Fig. 4a-d were 87.6°±0.9°, 177.2°±2.8°, 87.4°±1.1° and 182.2°±3.3°, respectively. These correspond to temporal resolutions of 80.3±0.8, 162.4±2.5, 80.1±1.0, and 167±3.0 ms, respectively.
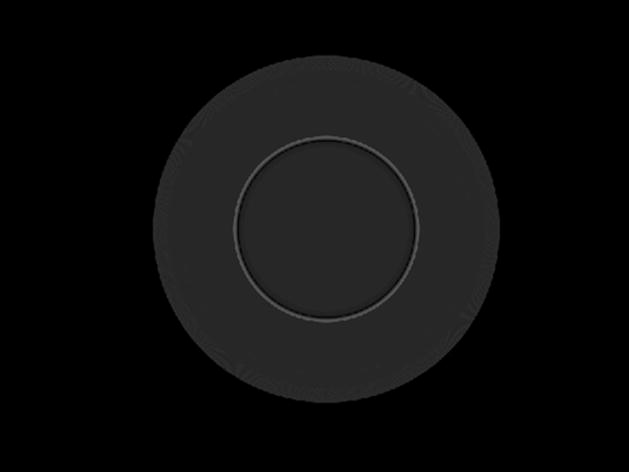
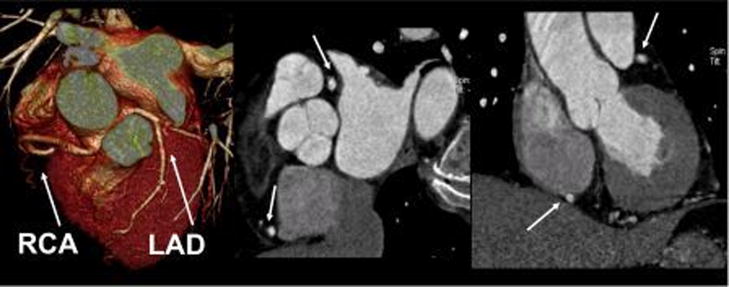
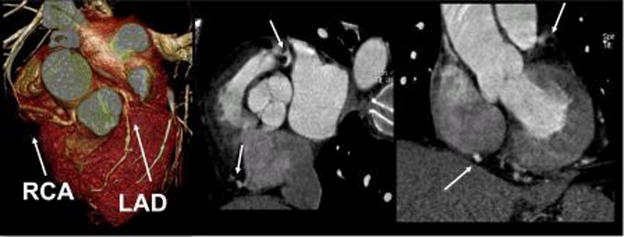
Fig. 6 demonstrates the differences in motion artifact between 83 and 165 ms nominal temporal resolutions for a patient having a mean heart rate of 90 bpm. The decrease in motion artifact with the dual-source reconstruction (83 ms temporal resolution) is evident.
Figure 6.
Patient data for a patient with a heart rate of 90 bpm were reconstructed using (a) tubes A and B or (b) tube A only. The 3D rendering and oblique reformatted images from patient with a mean heart rate of 90 bpm demonstrate the improved temporal resolution of the dual source technique.
Conclusions
We have demonstrated the utility of a rotating motion phantom for a visually intuitive assessment of temporal resolution in CT. For the dual-source CT system, the partial “ring artifact” covered approximately 87.5° of angular extent, corresponding to an 80.2 ms temporal resolution near isocenter. Using only one of the sources, the partial reconstruction demonstrated a partial “ring artifact” covering approximately 179.7°, corresponding to a temporal resolution of 164.7 ms near isocenter. These estimations of temporal resolution correspond well to the nominal values of 83 and 165 ms, respectively. The standard deviation of the measurements (n=5 for each scan mode) ranged from 0.8 to 3.0 ms.
Patient data reconstructed at the two temporal resolutions demonstrate improved sharpness and decreased motion artifact using dual-source CT for a heart rate of 90 bpm. Clinical experience with this technology has thus far supported the premise that the use of heart rate control is not required for a temporal resolution of 83 msec 1, 2, 6–8.
Acknowledgments
The authors would like to thank Mr. William Ollhoff for his assistance with phantom construction and Ms. Kristina Nunez for assistance with manuscript preparation.
Bibliography
- 1.Flohr TG, McCollough CH, Bruder H, Petersilka M, Gruber K, Suss C, Grasruck M, Stierstorfer K, Krauss B, Raupach R, Primak AN, Kuttner A, Achenbach S, Becker C, Kopp A, Ohnesorge BM. First performance evaluation of a dual-source CT (DSCT) system. Eur Radiol. 2006;16:256–68. doi: 10.1007/s00330-005-2919-2. [DOI] [PubMed] [Google Scholar]
- 2.Johnson TR, Nikolaou K, Wintersperger BJ, Leber AW, von Ziegler F, Rist C, Buhmann S, Knez A, Reiser MF, Becker CR. Dual-source CT cardiac imaging: initial experience. Eur Radiol. 2006;16:1409–15. doi: 10.1007/s00330-006-0298-y. [DOI] [PubMed] [Google Scholar]
- 3.McCollough CH, Primak AN, Saba O, Bruder H, Stierstorfer K, Raupach R, Suess C, Schmidt B, Ohnesorge BM, Flohr TG. Dose performance of a 64-channel dual-source CT scanner. Radiology. 2007;243:775–84. doi: 10.1148/radiol.2433061165. [DOI] [PubMed] [Google Scholar]
- 4.Flohr TG, Stierstorfer K, Ulzheimer S, Bruder H, Primak AN, McCollough CH. Image reconstruction and image quality evaluation for a 64-slice CT scanner with z-flying focal spot. Med Phys. 2005;32:2536–47. doi: 10.1118/1.1949787. [DOI] [PubMed] [Google Scholar]
- 5.Flohr T, Ohnesorge B. Heart rate adaptive optimization of spatial and temporal resolution for electrocardiogram-gated multislice spiral CT of the heart. J Comput Assist Tomogr. 2001;25:907–923. doi: 10.1097/00004728-200111000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Leber AW, Johnson T, Becker A, von Ziegler F, Tittus J, Nikolaou K, Reiser M, Steinbeck G, Becker CR, Knez A. Diagnostic accuracy of dual-source multi-slice CT-coronary angiography in patients with an intermediate pretest likelihood for coronary artery disease. Eur Heart J. 2007;28:2354–60. doi: 10.1093/eurheartj/ehm294. [DOI] [PubMed] [Google Scholar]
- 7.Lell MM, Panknin C, Saleh R, Sayre JW, Schmidt B, Dinh H, Ruehm SG. Evaluation of coronary stents and stenoses at different heart rates with dual source spiral CT (DSCT) Invest Radiol. 2007;42:536–41. doi: 10.1097/RLI.0b013e318041f674. [DOI] [PubMed] [Google Scholar]
- 8.Reimann AJ, Rinck D, Birinci-Aydogan A, Scheuering M, Burgstahler C, Schroeder S, Brodoefel H, Tsiflikas I, Herberts T, Flohr T, Claussen CD, Kopp AF, Heuschmid M. Dual-source computed tomography: advances of improved temporal resolution in coronary plaque imaging. Invest Radiol. 2007;42:196–203. doi: 10.1097/01.rli.0000254409.79193.96. [DOI] [PubMed] [Google Scholar]