Abstract
Mesenchymal stem cells (MSCs) can inhibit T cell proliferation; however, the underlying mechanisms are not clear. In this study, we investigated the mechanisms of the immunoregulatory activity of MSCs on T cells. Irradiated MSCs co-cultured with either naïve or pre-activated T cells in a mixed lymphocyte reaction (MLR) significantly suppressed T cell proliferation in a dose-dependent manner, irrespective of allogeneic disparity between responders and MSCs. Transwell assays revealed that the suppressive effect was primarily mediated by soluble factors that induced apoptosis. Splenocytes stimulated with alloantigen in the presence of the MSC culture supernatant (CS) produced a significant amount of IL-10, which was attributed to an increase in the number of IL-10 secreting cells, confirmed by an ELISPOT assay. The blockade of IL-10 and IL-10 receptor interaction by anti-IL-10 or anti-IL-10-receptor antibodies abrogated the suppressive capacity of MSC CS, indicating that IL-10 plays a major role in the suppression of T cell proliferation. The addition of 1-methyl-DL-tryptophan (1-MT), an indoleamine 2,3-dioxygenase (IDO) inhibitor, also restored the proliferative capacity of T cells. In conclusion, we demonstrated that soluble mediators from culture supernatant of MSCs could suppress the proliferation of both naïve and pre-activated T cells in which IL-10 and IDO play important roles.
Keywords: apoptosis; immunosuppression; indoleamine-pyrrole 2,3-dioxygenase; interleukin-10; mesenchymal stem cells; T-lymphocytes
Introduction
Mesenchymal stem cells (MSCs) are multipotential non-hematopoietic cells (Wakitani et al., 1995; Pittenger et al., 1999) that can not only expand ex vivo without any particular changes in phenotype and function (Reyes et al., 2001) but also differentiate in vitro into several mesenchymal cell lineages such as adipocytes, chondrocytes, osteocytes, myocytes, astrocytes and neurons (Krampera et al., 2003; Kato et al., 2004; Glennie et al., 2005; Zappia et al., 2005; Nauta et al., 2006; Stagg et al., 2006). Another important characteristic of MSCs is their immunosuppressive effect on several immune cells, including dendritic cells (DCs) (Jiang et al., 2005), B lymphocytes (Corcione et al., 2006) and T lymphocytes (Di Nicola et al., 2002; Krampera et al., 2003; Tse et al., 2003; Groh et al., 2005; Rasmusson et al., 2005). This makes MSCs attractive candidates for applications in regenerative medicine. Several recent studies have suggested that allotransplantation of MSCs may be feasible in clinical application such as metachromatic leukodystrophy and graft-versus- host disease (Frumento et al., 2002). Aggarwal and Pittenger (2005) showed that MSCs altered the phenotype of specific immune cells, providing evidence that transplantation of allogeneic MSCs could be clinically applicable. Despite all of this evidence for the therapeutic potential of MSCs, in order for MSCs to be accepted broadly as a therapeutic modality, the exact molecular mechanisms underlying their suppressive ability should be more fully understood. At present, these mechanisms remain unclear. Therefore, it is critical to identify the precise mechanisms by which MSCs exert their suppressive capabilities. Evidence from in vitro stimulation tests has demonstrated that both cell-cell contact and soluble factors contribute to the immunomodulatory function of MSCs. There are confounding data, however, with regard to the mechanisms involved. As for the soluble factors, indoleamine 2,3-dioxygenase (IDO) (Meisel et al., 2004), prostaglandin E2 (PGE2) (Aggarwal and Pittenger, 2005), TGF-β and nitric oxide (Sato et al., 2007; Ren et al., 2008) have all been reported to be involved. Furthermore, MSCs induce cell division arrest and apoptosis of activated T cells (Glennie et al., 2005; Plumas et al., 2005; Zappia et al., 2005), but the mechanisms behind the cell division arrest and apoptosis are not clearly defined.
To understand the precise mechanisms by which the MSCs exert their immunomodulatory activity, we investigated the effect of MSCs on T cell activation, including proliferation, expansion and cytokine secretion, and tried to define the extent of the contribution of each factor involved by using blocking studies. We observed that MSCs effectively suppressed the proliferation of alloreactive T cells in mixed lymphocyte reaction (MLR). Transwell experiments revealed that the suppressive capacity of MSCs could be attributed to soluble mediators, which was confirmed by showing that MSC culture supernatant (CS) had the same suppressive activity as the MSCs themselves. Splenocytes activated in the presence of MSC CS produced a significantly higher amount of IL-10; additionally, a blockade of IL-10/IL-10R interaction by antibodies or of IDO activity by 1-MT abrogated the suppressive capacity of MSC CS.
Results
MSCs effectively suppressed not only naïve but also pre-activated T cell proliferation irrespective of the allogeneic disparity between T cells and MSCs
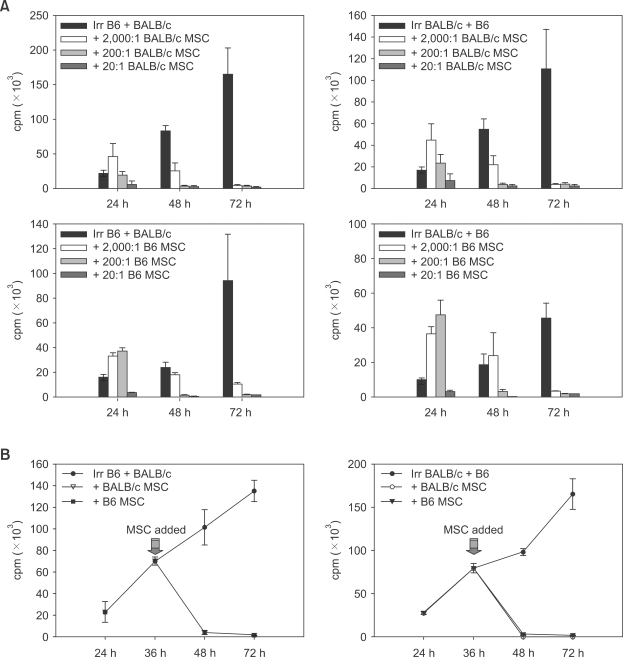
To investigate the ability of MSCs to suppress T cell proliferation, different doses of MSCs were added to MLR with a ratio of splenocyte to MSCs of 2,000:1, 200:1 or 20:1. Both BALB/c and C57BL/6 MSCs effectively inhibited the proliferation of both allogeneic and syngeneic T cells to a similar degree at 72 h after stimulation. Maximum inhibition was achieved with the 20:1 ratio; at 24 h after stimulation, however, the suppressive effect was not evident for the 200:1 and 2,000:1 ratios (Figure 1A). MSCs could suppress pre-activated T cells since the addition of MSCs at 36 h after the initiation of the MLR showed a comparable inhibitory effect to the addition of MSCs at the start of the MLR (Figure 1B). This indicated that MSCs exerted their inhibitory effects not only on naïve T cells but also on pre-activated T cells.
Figure 1.
MSCs suppressed both naïve and pre-activated T cell proliferation in a time and dose-dependent manner. 5 × 105 BALB/c splenocytes and 5 × 105 C57BL/6 splenocytes were used as either stimulators or responders in MLR. (A) BALB/c or C57BL/6 MSCs were added to MLR at the start of the reaction, and the ratios of splenocytes to MSCs were 2,000:1, 200:1 or 20:1. The culture periods were 24 h, 48 h and 72 h. (B) BALB/c or C57BL/6 MSCs were added to the MLR at 36 h after the start of the reaction. The ratio of splenocytes to MSCs was 20:1. The culture continued for 24 h, 36 h, 48 h or 72 h. The results are expressed as the mean counts per minute (cpm) ± SD for three independent experiments.
Soluble factors in culture supernatant of MSCs suppressed T cell proliferation in MLR
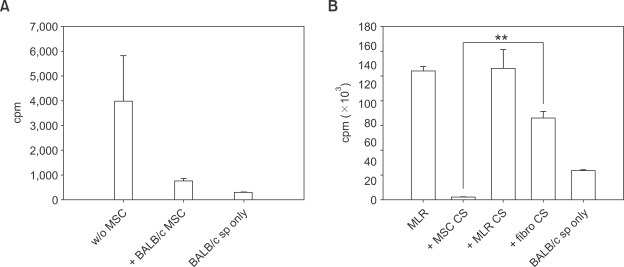
To determine whether the suppression of T cell proliferation required direct cellular contact by MSCs, splenocytes were separated from MSCs in a transwell chamber and activated by MLR. While MLR was occurring in the lower chamber, BALB/c MSCs were cultured in the upper chamber. In this system, soluble elements produced from MSCs in the upper chamber were free to pass the transmembrane while the cells were not allowed to contact each other. As shown in Figure 2A, BALB/c MSC suppressed T cell proliferation indicating that MSC suppression of T cell proliferation was not dependent on cell-to-cell contact but was caused by soluble factors. In order to confirm the ability of soluble factors from MSCs to suppress T cell proliferation, 72 h culture supernatant was added to the MLR at a 1:1 ratio. MLR CS and BALB/c fibroblast CS were used as controls. As shown in Figure 2B, significant suppression of T cell proliferation was observed only in the group with MSC CS, suggesting that soluble factors contained in the culture supernatant of MSCs could suppress T cell proliferation.
Figure 2.
Suppression of T cells by MSCs was not dependent on cell-cell contact but was evoked by soluble factors. 5 × 105 BALB/c splenocytes were stimulated with 5 × 105 γ-irradiated C57BL/6 splenocytes in MLR for 72 h. (A) The MLR took place on the bottom of a transwell, and MSCs were added to the indicated upper wells (splenocytes/MSCs ratio was 20:1). (B) Supernatant from day 3 cultures of BALB/c MSCs was added to the MLR at 0 h. MLR culture supernatant and BALB/c fibroblast culture supernatant were used as controls. MLR culture supernatant was obtained from 2 × 106 BALB/c splenocytes co-cultured with 2 × 106 γ-irradiated C57BL/6 splenocytes in 25 cm2 tissue culture flasks for 14 days. BALB/c fibroblast culture supernatant was collected from primary BALB/c fibroblast cells on a 100 mm plate fully cultured for 3 days. The volume of each culture supernatant added was 50% that of MLR. Results are expressed as mean values (± SD) of cpm obtained in triplicate cultures. **P < 0.001.
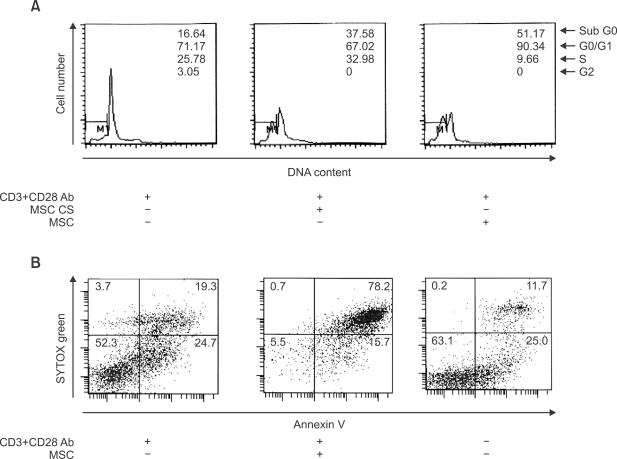
MSC culture supernatant caused apoptosis of proliferated splenocytes rather than cell cycle arrest
To determine whether the suppression of T cell proliferation by MSCs or MSC CS was due to the induction of cell death or cell cycle arrest, we examined whether MSC CS could delay the cell cycle or trigger apoptosis of splenocytes by estimating values of each cell-cycle phase. After 72 h incubation of MSC CS and T cells in splenocytes stimulated with anti-CD3 and anti-CD28 antibodies, the apoptotic population of splenocytes was increased more than twice, and MSC CS could not interrupt or delay the entry of them into the cell cycle. In contrast, MSC treatment instead of MSC CS caused almost all T cells to remain in the G0/G1 phase and also induced apoptosis of T cells (Figure 3A). In further experiments, MSCs were added to proliferating T cells among the splenocytes stimulated with anti-CD3 and anti-CD28 antibodies, and the level of apoptosis was analyzed by flow cytometry with annexin V and SYTOX green staining to confirm MSC-mediated apoptosis. Annexin V binds phosphatidylserine, which is released from the outer cell membrane early in the process of apoptosis (Koopman et al., 1994), and SYTOX green dye cannot permeate live cells but stains apoptotic cells with intense green fluorescence by binding to cellular nucleic acids. Annexin V single positive and SYTOX green and annexin V double positive cells indicated early and accumulated apoptosis, respectively. Almost 94 percent of the splenocytes (early apoptosis: 15.7%, accumulated apoptosis: 78.2%) underwent apoptosis when they were co-cultured with MSCs for 72 h. In contrast, cells cultured without MSCs (early apoptosis: 24.7%, accumulated apoptosis: 19.3%) showed a much lower percentage of cells undergoing apoptosis (activation- induced cell death was present even without any stimulation) (Figure 3B).
Figure 3.
MSC culture supernatant caused apoptosis of splenocytes rather than cell cycle arrest. 5 × 105 BALB/c splenocytes were stimulated with anti-CD3 (3 µg/ml) and CD28 (1 µg/ml) antibodies for 72 h. (A) 100 µl MSC culture supernatant or 2.5 × 104 MSCs were treated in the indicated groups. DNA content was assessed using PI staining. (B) 2.5 × 104 MSCs were added to the proper group. Apoptotic cells were stained with annexin V (PE) and SYTOX® green. These assays were analyzed using flow cytometry, and MSCs were excluded from the analysis by positive gating of CD45. One representative of three separate experiments is shown.
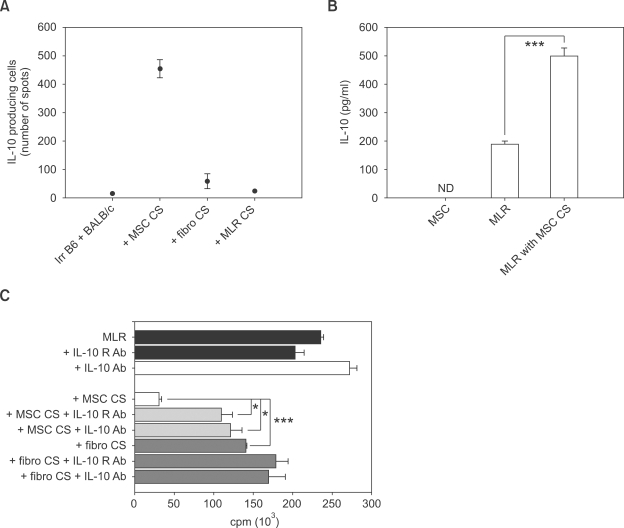
MSC culture supernatant stimulated splenocytes to secrete a significant amount of IL-10
To evaluate the effect of MSC CS on IL-10 secretion in splenocytes, the profile of IL-10 secretion in splenocytes stimulated in the presence of MSC CS was analyzed by an ELISPOT assay. BALB/c splenocytes stimulated with irradiated C57BL/6 splenocytes were cultivated on the ELISPOT plate with BALB/c MSC CS for 48 h (Figure 4A). For the controls, BALB/c fibroblast CS was used. The number of IL-10 secreting cells was only changed by the MSC CS treatment. In addition, no IL-10 was detected in MSC CS, whereas little IL-10 was present in MLR CS (Figure 4B). Because IL-10 is a well known inhibitor of T cell proliferation and activation, we next investigated whether T cell proliferation recovered when MSC CS was used in MLR with blocking antibodies for either IL-10 or IL-10 receptor. As shown in Figure 4C, T cell proliferation was significantly restored in MSC CS with each antibody, but this phenomenon was not observed in treatment with fibroblasts. These findings suggested that MSC CS drove splenocytes to produce IL-10. Moreover, MSC CS-mediated IL-10 production allowed the proliferation of T cells to be suppressed by a paracrine effect.
Figure 4.
Soluble factors from MSCs affected IL-10 secretion of splenocytes. (A) 5 × 105 BALB/c and 5 × 105 γ-irradiated C57BL/6 splenocytes were used as responder and stimulator cells, respectively, in MLR for 72 h. (A) ELISPOT assays were performed with or without culture supernatant from BALB/c MSCs. BALB/c fibroblast culture supernatant and MLR culture supernatant were used as controls. 100 µl of each supernatant was added per well. (B) The concentration of IL-10 in MLR culture supernatant, MSC culture supernatant or MLR with MSC CS was measured by ELISA. ***P < 0.0001. ('ND' means not detected) (C) Blocking of IL-10 and IL-10 receptor interaction was performed in the absence or presence of MSC culture supernatant, BALB/c fibroblast culture supernatant or MLR culture supernatant. A neutralizing IL-10 or IL-10 receptor Ab (5 µg/ml, respectively) was used in the indicated groups. The results shown are expressed as mean ± SD from three independent experiments. *P < 0.05, ***P < 0.0001.
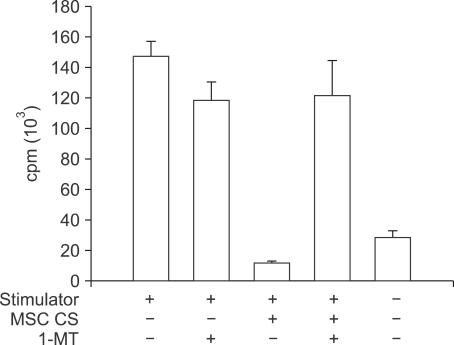
IDO relation to MSC culture supernatant to suppress T cell
IDO cleaves tryptophan, an essential amino acid for T cell growth, and converts it to kynurenine (Mellor and Munn, 1999). 1-methyl-tryptophan (1-MT) interferes with IDO activity as a competitive inhibitor (Bodaghi et al., 1999). To examine whether indoleamine-2,3-dioxygenase (IDO) was related to T cell suppression by MSC CS, 1-MT was added to MLR with MSC CS. The proliferation of T cells in the group treated with MSC CS and 1-MT was almost completely recovered (Figure 5). According to this result, we can state that IDO is sufficient to suppress T cell activity mediated by MSC CS.
Figure 5.
IDO is related to the immunomodulatory effect of MSC culture supernatant on T cells. MLR was done with 5 × 105 splenocytes of BALB/c or C57BL/6 as responder or γ-irradiated stimulator, respectively, for 72 h. In the indicated groups, 1 mM 1-MT was used with or without 100 µl MSC CS in appropriate wells. T cell proliferation was measured by thymidine uptake by T cells. The results shown are expressed as mean ± SD from three independent experiments.
Discussion
Recently, MSCs have been actively studied with a view toward tissue regeneration and organ transplantation due to their ability to differentiate into several tissues and their potential to regulate many immune cells (Aggarwal and Pittenger, 2005; Glennie et al., 2005; Groh et al., 2005; Jiang et al., 2005; Plumas et al., 2005; Poggi et al., 2005; Rasmusson et al., 2005; Sordi et al., 2005; Zappia et al., 2005; Corcione et al., 2006; Nauta et al., 2006; Sotiropoulou et al., 2006; Spaggiari et al., 2006; Stagg et al., 2006; Taylor et al., 2006). It has been well known that MSCs inhibit T cell proliferation (Di Nicola et al., 2002; Krampera et al., 2003; Potian et al., 2003; Tse et al., 2003; Meisel et al., 2004; Aggarwal and Pittenger, 2005; Groh et al., 2005; Rasmusson et al., 2005), in addition to modulating DC functions, altering antigen-presenting cell maturation and interacting with NK cells (Beyth et al., 2005; Jiang et al., 2005; Poggi et al., 2005; Sotiropoulou et al., 2006; Spaggiari et al., 2006). Several studies have revealed that immunomodulatory effects of MSCs are mediated by cell-cell contact and soluble factors such as prostaglandin E2, IDO and TGF-β (Di Nicola et al., 2002; Krampera et al., 2003; Potian et al., 2003; Tse et al., 2003; Meisel et al., 2004; Aggarwal and Pittenger, 2005; Groh et al., 2005; Rasmusson et al., 2005). All of these mechanisms act directly on T cells, which we assume would not be enough to explain the bystander effect of MSCs. It is still unclear where these soluble factors come from and what causes them to be secreted.
In this report, we showed the following. (1) Murine MSCs inhibited the proliferation of either syngeneic or allogeneic T cells, irrespective of their activation status, i.e., unprimed and already activated effector T cells. (2) These effects were caused by not only MSCs but also MSC CS. (3) There was no requirement for direct MSC-T cell contact. (4) MSC CS induced apoptosis of splenocytes including T cells rather than cell-cycle arrest, and (5) it caused splenocytes to secrete cytokines, especially IL-10. (6) Neutralization of IL-10 and IL-10 receptor moderately restored the proliferation of T cells. (7) MSC culture supernatant also induced IDO in the MLR, which caused suppression of T cells. The IDO inhibitor 1-MT was able to almost completely reverse this suppression of T cells.
In Figure 1A, MSCs effectively suppressed T cell activation when different doses of MSCs (2000:1, 200:1 and 20:1) were used in the MLR at different times, and even when the T cells were allogeneic with the MSCs. The immunomodulatory effect of MSCs on T cells, however, was not evident except for the 20:1 ratio. It seems that few MSCs activated T cell proliferation rather than suppression. MSCs themselves were γ-irradiated with 60cGy to blunt MSC proliferation, and the cpm value of MSC culture alone was similar to that of non-stimulated responder cell culture. Moreover, the phenomenon of early activation of T cells by few MSCs did not occur when MSC CS was used in the MLR instead of MSCs at 24 h and 48 h (data not shown). Therefore, it appears that MSCs interacted with T cells at early time points, causing activation of the T cells. The results of experiments without direct cell contact, however, emphasize that T cell contact with MSCs is not necessary to inhibit T cell proliferation. It should be considered, though, whether contact between T cells and MSCs is fully dispensable.
Although MSCs have been known to induce apoptosis (Plumas et al., 2005), whether apoptosis is induced by MSC CS or not remains unclear. In this study, we showed that MSC CS induced cell cycle arrest independent of cellular apoptosis, while MSCs themselves induced splenocyte apoptosis, some of which was cell-cycle arrest dependent. Therefore, we can say that T cell cycle arrest requires cell-cell contact, while induction of cellular apoptosis demands not only cell contact but also soluble factors.
In an ELISPOT assay, IL-10 was secreted from splenocytes and not from MSCs, indicating that T cells might be influenced by paracrine effect. Moreover, downregulation of T cell proliferation by MSC CS was limited when IL-10 or IL-10 receptor was intercepted by neutralizing antibodies. It is well known that IL-10 is a suppressive cytokine for proliferation and cytokine production of T cells, and it plays a key role in inducing T cell anergy. Antigen-specific T cell suppression by IL-10 is essential in peripheral tolerance to allergens, autoantigens, transplantation antigens and tumor antigens (Taylor et al., 2006). Previous studies showed that IL-10 led to T cell apoptosis (Georgescu et al., 1997; Ayala et al., 2001; Oshima et al., 2002), and it appears that IL-10 from T cells influenced by MSC CS caused T cell apoptosis. It needs to be further investigated whether the increase of IL-10 is necessary and sufficient to suppress the T cell proliferation and induce apoptosis.
IDO is known to induce T cell suppression by MSCs (Meisel et al., 2004; Ryan et al., 2007). However, the involvement of IDO in MSC CS mediated T cells suppression has not been reported. Our results showed almost complete restoration of T cell proliferation by adding 1-MT; therefore, IDO seems to be one of the factors related to the immunomodulatory effects of MSC CS. T cell proliferation is thought to be suppressed by a reduced amount of tryptophan, while apoptosis is induced by an increased level of kynurenine, a metabolite formed from tryptophan (Frumento et al., 2002; Terness et al., 2002). Tryptophan is an essential factor for T cell proliferation, while kynurenine blocks Ag-driven specific T cell proliferation, possibly leading to T cell death (Meisel et al., 2004). It has been reported that IL-10 secreted by regulatory T cells induced IDO secretion from APCs in a T cell proliferation niche by MLR (Finger and Bluestone, 2002). In our study, we observed IL-10 and IDO in MSC CS play an important role in suppression of T cell proliferation independently as shown in Figure 4 and 5. However, the addition of both antiIL-10 Ab and 1-MT at the same time did not show the additive effect in restoration of suppressive effect by MSC CS (data not shown) suggesting that IL-10 secreted by stimulated splenocytes might induce the production of IDO from APCs contained in the splenocytes. This should be further confirmed by showing dose-effect response between IL-10 and IDO in splenocytes. The results described thus far show that soluble factors from MSCs induced IL-10 production by splenocytes, which in turn suppressed the proliferation of the T cells themselves. We postulate that this underlies the bystander immunomodulatory effect exerted by MSCs in vivo.
Methods
Isolation and characterization of murine MSCs
C57BL/6 (H2-Kb) mice were purchased from Charles River Laboratories. MSCs were collected from bone marrow. Femurs and tibias were flushed with PBS containing 150 µg/ml gentamycin. The cells obtained were cultured in 100 mm cell culture plates with high-glucose DMEM (Gibco Laboratories, Grand Island, NY), which was supplemented with heat-inactivated 10% FBS, 5% horse serum, 50 µg/ml gentamycin, 2 mM L-glutamine, 100 µM non-essential amino acids, 10 mM HEPES and 55 µM 2-mercaptoethanol. Cells were incubated at a concentration of 106/ml at 37℃ in a 5% CO2 atmosphere. After 72 h, non-adherent cells were removed. When the plate was ~80% confluent, adherent cells were trypsinized and split. The MSCs of BALB/c mouse origin were obtained from Dr. Elizabeth Simpson (Imperial College Faculty of Medicine, London, UK). The cells were cultivated in complete DMEM-10 (DMEM containing heat-inactivated 10% FBS, 50 µg/ml gentamycin, 2 mM L-glutamine, 100 µM non-essential amino acids, 10 mM HEPES and 55 µM 2-mercaptoethanol). Surface antigen expression of the MSCs was confirmed by flow cytometry. 1 × 106 MSCs were incubated at 4℃ for 1 h in the following monoclonal antibodies: FITC conjugated anti-CD106, CD11c, H2Kd, I-Ab (BD Pharmingen, San Diego, CA) and CD34 (eBioscience, San Diego, CA); phycoerythrin (PE) conjugated anti-H2Kb and I-Ad (BD Pharmingen, San Diego, CA); biotin conjugated anti-CD14, CD31, and CD45 (eBioscience, San Diego, CA). Cells were washed with PBS containing 1% BSA and 0.1% sodium azide. Biotinylated cells were incubated with PerCP-streptavidin (BD Pharmingen, San Diego, CA) at 4℃ for 30 min. The cell suspensions were washed with PBS containing 0.5% BSA and 0.1% sodium azide and then analyzed by FACScan (Becton Dickinson, Heidelberg, Germany) using Cell Quest software. MSCs from both mouse strains were positive for CD106 and negative for CD45, CD14, CD34, CD31, and CD11c. MSCs from the BALB/c strain expressed neither MHC class I nor class II molecules, whereas those from the C57BL/6 strain expressed a modest level of MHC class I molecules with no MHC class II molecules. Osteogenic differentiation was induced by 10 mM β-glycero-phosphate, 50 µg/ml ascorbic acid 2-phosphate and 10-9 M dexamethasone in complete DMEM-10. Cultures for osteogenesis were maintained for 3-4 weeks, and differentiation medium was re-supplied twice a week. Cell differentiation for osteogenesis was identified by culture staining with 2% Alizarin Red S for 20 min at room temperature after fixation with 10% formalin for 20 min. To induce adipogenic differentiation, MSCs were cultured with 10-9 M dexamethasone and 5 µg/ml insulin in complete DMEM-10 for 3-4 weeks, changing the media twice a week. Cultured cells were fixed with 10% formalin for 20 min and incubated with Oil Red O for 1 h. Photographs of the cells were taken with a digital camera (Nikon Infinity) attached to a light microscope (Nikon ECLIPSE TS 100). MSCs from both strains differentiated into adipocytes and osteoblasts.
Preparation of MSC culture supernatants
1 × 105 cells of BALB/c MSCs were plated in a 100 mm plate and cultured for 72 h in complete DMEM-10. When the plate was confluent with about 90% cells, culture supernatant was harvested and centrifuged at 1,200 × g at room temperature for 10 min. The upper aqueous solution was aliquoted in 1.5 ml microtubes and kept in a -70℃ deep freezer.
Mixed lymphocyte reactions (MLRs)
BALB/c and C57BL/6 splenocytes were used as either stimulator or responder cells. Splenocytes were isolated by mechanical dissociation using fully frosted slides followed by red blood cell lysis with Red Blood Cell Lysing Buffer (Sigma-Aldrich, St-Louis, MO). Prior to the experiment, stimulator cells were irradiated with 20 Gy of γ-ray to prevent them from reacting against responder cells. Both BALB/c and C57BL/6 MSCs were irradiated with 60 cGy of γ-ray. A co-culture was then made by adding 5 × 105 stimulator and 5 × 105 responder cells per well (1:1) in 96-well round-bottom plates in 0.2 ml complete DMEM-10. 2.5 × 102, 2.5 × 103 or 2.5 × 104 MSCs were added to the co-culture at different time intervals, t = 0 or t = 36 h. Control cultures did not contain MSCs. In selected MLR experiments, MSCs were substituted with culture supernatant from MSCs. Along with the stimulator/responder population in the MLR, the prepared MSC supernatant mixed with 50% fresh media was added at different time points, t = 0 and t = 36 h of the reaction. Proliferation was assessed by 1 µCi of [3H]-thymidine (Amersham, Buckinghamshire, UK) incorporation. [3H]-thymidine was added to MLRs at 24 h, 36 h, 48 h or 72 h, and the cells were harvested onto glass fiber filters using a 96-well cell harvester (Inoteck, Bertold, Japan) after 18 h of extended culture. All of the T cell proliferation assays were done in triplicate. [3H]-thymidine incorporation was measured by a microbeta TriLux luminescence counter (Perkin Elmer, Wellesley, MA). The results were represented as counts per minute (cpm).
Transwell cultures
A transwell system (1.0 µm pore size membrane, Corning, Acton, MA) was used to prevent MSCs from contacting the splenocytes. BALB/c splenocytes were used as stimulators, and C57BL/6 splenocytes were used as responders. 5 × 105 stimulator and 5 × 105 responder cells were loaded into the lower chamber of the well, and 2.5 × 104 MSCs were added to the upper chamber at t = 0 and t = 36 h of the reaction. After 72 h, the reaction was pulsed with [3H]-thymidine for a further 18 h.
Analysis of cell-cycle arrest and apoptosis
In the cell-cycle arrest assay, the stimulated cells were harvested and stained with an allophycocyanin (APC) conjugated anti-CD45 Ab (BD Pharmingen, San Diego, CA), then fixed with a solution containing a ratio of PBS with 50% FBS to 70% ethanol of 3:7 at 4℃ overnight. The next day, the cells were centrifuged and stained with 300 µl propidium iodide stock solution (50 µg/ml) for 15 min. After staining, the DNA content of the cells was analyzed by FACSCanto II (Becton Dickinson, Heidelberg, Germany) using FACSDiva software. To assess apoptosis, the Vybranted apoptosis Assay Kit #8 (R-phycoerythrin annexin V/SYTOX green) (Invitrogen, Carlsbad, CA) was used. Briefly, cells were harvested and washed with annexin-binding buffer, then stained with R-phycoerythrin annexin V and SYTOX Green for 30 min on ice. After staining, the cells were analyzed by FACSCanto II using FACSDiva software.
ELISPOT and ELISA for the measurement of IL-10
96-well ELISPOT plates (Millipore, Bedford MA) were coated with anti-IL-10 capture mAb (diluted in sterile PBS) in a volume of 100 µl with 1:60 dilution and incubated overnight at 4℃. On the day of the experiment, the plates was washed five times with PBS-containing 0.05% Tween-20 (PBST) and blocked for 30 min with complete DMEM-10 at 37℃. Both 5 × 105 C57BL/6 splenocytes (γ-irradiated stimulator cells) and 5 × 105 BALB/c splenocytes (responder cells) in 100 µl of complete DMEM-10 were cultured with 100 µl of complete DMEM-10, BALB/c MSC CS or fibroblast CS for 48 h. After the incubation, cells were discarded and the plate was washed five times with PBST. A 1:60 dilution of detection antibody in PBS was added to the plate, which was then incubated for 1 h at 37℃. After washing five times with PBST, streptavidin-alkaline phosphatase (Promega, Madison, WI) was added to each well and incubated for 1 h at 37℃. The plate was then washed four times with PBST and two times with PBS. The developing solution composed of 20 µl/ml of NPT/BCIP stock solution (Roche, Indianapolis, IN) in alkaline phosphatase substrate buffer (100 mM Tris-Cl pH 9.5, 100 mM NaCl and 5 mM MgCl2 in distilled water) was added. The resulting spots were counted and analyzed on a computer-assisted AID EliSpot Reader System (AID, Straßberg, Germany). The amount of IL-10 in the MSC or MLR CS was quantified by ELISA (Duoset ELISA development system, R&D, MN) according to the manufacturer's instruction.
Blocking IL-10 and IL-10 receptor interaction and IDO inhibition
BALB/c splenocytes were co-cultured with irradiated C57BL/6 splenocytes in the absence or presence of MSC CS or fibroblast CS, with or without IL-10 or IL-10 receptor neutralizing antibodies (5 µg/ml) for 72 h. For IDO inhibition, 1 mM 1-methyl-DL-tryptophan (1-MT, Sigma-Aldrich, St-Louis, MO) was added instead of neutralizing antibodies. [3H]-thymidine was pulsed for 18 h.
Statistical analysis
Values for all measurements are presented as mean ± SD. Comparisons for all pairs were performed by Student's t-test. Significance levels were set at a P value of 0.05.
Acknowledgement
This study was supported by a grant of the Korea Health 21 R & D Project, Ministry of Health and Welfare, Republic of Korea (Project No. : A040004).
Abbreviations
- B6
C57BL/6
- CS
culture supernatant
- DC
dendritic cellss
- IDO
indoleamine 2,3-dioxygenase
- MLR
mixed lymphocyte reaction
- MSC
mesenchymal stem cell
- 1-MT
1-methyl-DL-tryptophan
- sp
splenocyte
References
- 1.Aggarwal S, Pittenger MF. Human mesenchymal stem cells modulate allogeneic immune cell responses. Blood. 2005;105:1815–1822. doi: 10.1182/blood-2004-04-1559. [DOI] [PubMed] [Google Scholar]
- 2.Ayala A, Chung CS, Song GY, Chaudry IH. IL-10 mediation of activation-induced TH1 cell apoptosis and lymphoid dysfunction in polymicrobial sepsis. Cytokine. 2001;14:37–48. doi: 10.1006/cyto.2001.0848. [DOI] [PubMed] [Google Scholar]
- 3.Beyth S, Borovsky Z, Mevorach D, Liebergall M, Gazit Z, Aslan H, Galun E, Rachmilewitz J. Human mesenchymal stem cells alter antigen-presenting cell maturation and induce T-cell unresponsiveness. Blood. 2005;105:2214–2219. doi: 10.1182/blood-2004-07-2921. [DOI] [PubMed] [Google Scholar]
- 4.Bodaghi B, Goureau O, Zipeto D, Laurent L, Virelizier JL, Michelson S. Role of IFN-gamma-induced indoleamine 2,3 dioxygenase and inducible nitric oxide synthase in the replication of human cytomegalovirus in retinal pigment epithelial cells. J Immunol. 1999;162:957–964. [PubMed] [Google Scholar]
- 5.Corcione A, Benvenuto F, Ferretti E, Giunti D, Cappiello V, Cazzanti F, Risso M, Gualandi F, Mancardi GL, Pistoia V, Uccelli A. Human mesenchymal stem cells modulate B-cell functions. Blood. 2006;107:367–372. doi: 10.1182/blood-2005-07-2657. [DOI] [PubMed] [Google Scholar]
- 6.Di Nicola M, Carlo-Stella C, Magni M, Milanesi M, Longoni PD, Matteucci P, Grisanti S, Gianni AM. Human bone marrow stromal cells suppress T-lymphocyte proliferation induced by cellular or nonspecific mitogenic stimuli. Blood. 2002;99:3838–3843. doi: 10.1182/blood.v99.10.3838. [DOI] [PubMed] [Google Scholar]
- 7.Finger EB, Bluestone JA. When ligand becomes receptor--tolerance via B7 signaling on DCs. Nat Immunol. 2002;3:1056–1057. doi: 10.1038/ni1102-1056. [DOI] [PubMed] [Google Scholar]
- 8.Frumento G, Rotondo R, Tonetti M, Damonte G, Benatti U, Ferrara GB. Tryptophan-derived catabolites are responsible for inhibition of T and natural killer cell proliferation induced by indoleamine 2,3-dioxygenase. J Exp Med. 2002;196:459–468. doi: 10.1084/jem.20020121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Georgescu L, Vakkalanka RK, Elkon KB, Crow MK. Interleukin-10 promotes activation-induced cell death of SLE lymphocytes mediated by Fas ligand. J Clin Invest. 1997;100:2622–2633. doi: 10.1172/JCI119806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Glennie S, Soeiro I, Dyson PJ, Lam EW, Dazzi F. Bone marrow mesenchymal stem cells induce division arrest anergy of activated T cells. Blood. 2005;105:2821–2827. doi: 10.1182/blood-2004-09-3696. [DOI] [PubMed] [Google Scholar]
- 11.Groh ME, Maitra B, Szekely E, Koc ON. Human mesenchymal stem cells require monocyte-mediated activation to suppress alloreactive T cells. Exp Hematol. 2005;33:928–934. doi: 10.1016/j.exphem.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 12.Jiang XX, Zhang Y, Liu B, Zhang SX, Wu Y, Yu XD, Mao N. Human mesenchymal stem cells inhibit differentiation and function of monocyte-derived dendritic cells. Blood. 2005;105:4120–4126. doi: 10.1182/blood-2004-02-0586. [DOI] [PubMed] [Google Scholar]
- 13.Kato Y, Imabayashi H, Mori T, Tani T, Taniguchi M, Higashi M, Matsumoto M, Umezawa A, Tsunoda Y. Nuclear transfer of adult bone marrow mesenchymal stem cells: developmental totipotency of tissue-specific stem cells from an adult mammal. Biol Reprod. 2004;70:415–418. doi: 10.1095/biolreprod.103.020271. [DOI] [PubMed] [Google Scholar]
- 14.Koopman G, Reutelingsperger CP, Kuijten GA, Keehnen RM, Pals ST, van Oers MH. Annexin V for flow cytometric detection of phosphatidylserine expression on B cells undergoing apoptosis. Blood. 1994;84:1415–1420. [PubMed] [Google Scholar]
- 15.Krampera M, Glennie S, Dyson J, Scott D, Laylor R, Simpson E, Dazzi F. Bone marrow mesenchymal stem cells inhibit the response of naive and memory antigen-specific T cells to their cognate peptide. Blood. 2003;101:3722–3729. doi: 10.1182/blood-2002-07-2104. [DOI] [PubMed] [Google Scholar]
- 16.Meisel R, Zibert A, Laryea M, Gobel U, Daubener W, Dilloo D. Human bone marrow stromal cells inhibit allogeneic T-cell responses by indoleamine 2,3-dioxygenase-mediated tryptophan degradation. Blood. 2004;103:4619–4621. doi: 10.1182/blood-2003-11-3909. [DOI] [PubMed] [Google Scholar]
- 17.Mellor AL, Munn DH. Tryptophan catabolism and T-cell tolerance: immunosuppression by starvation? Immunol Today. 1999;20:469–473. doi: 10.1016/s0167-5699(99)01520-0. [DOI] [PubMed] [Google Scholar]
- 18.Nauta AJ, Westerhuis G, Kruisselbrink AB, Lurvink EG, Willemze R, Fibbe WE. Donor-derived mesenchymal stem cells are immunogenic in an allogeneic host and stimulate donor graft rejection in a nonmyeloablative setting. Blood. 2006;108:2114–2120. doi: 10.1182/blood-2005-11-011650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oshima K, Sen L, Cui G, Tung T, Sacks BM, Arellano-Kruse A, Laks H. Localized interleukin-10 gene transfer induces apoptosis of alloreactive T cells via FAS/FASL pathway, improves function, and prolongs survival of cardiac allograft. Transplantation. 2002;73:1019–1026. doi: 10.1097/00007890-200204150-00002. [DOI] [PubMed] [Google Scholar]
- 20.Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143–147. doi: 10.1126/science.284.5411.143. [DOI] [PubMed] [Google Scholar]
- 21.Plumas J, Chaperot L, Richard MJ, Molens JP, Bensa JC, Favrot MC. Mesenchymal stem cells induce apoptosis of activated T cells. Leukemia. 2005;19:1597–1604. doi: 10.1038/sj.leu.2403871. [DOI] [PubMed] [Google Scholar]
- 22.Poggi A, Prevosto C, Massaro AM, Negrini S, Urbani S, Pierri I, Saccardi R, Gobbi M, Zocchi MR. Interaction between human NK cells and bone marrow stromal cells induces NK cell triggering: role of NKp30 and NKG2D receptors. J Immunol. 2005;175:6352–6360. doi: 10.4049/jimmunol.175.10.6352. [DOI] [PubMed] [Google Scholar]
- 23.Potian JA, Aviv H, Ponzio NM, Harrison JS, Rameshwar P. Veto-like activity of mesenchymal stem cells: functional discrimination between cellular responses to alloantigens and recall antigens. J Immunol. 2003;171:3426–3434. doi: 10.4049/jimmunol.171.7.3426. [DOI] [PubMed] [Google Scholar]
- 24.Rasmusson I, Ringden O, Sundberg B, Le Blanc K. Mesenchymal stem cells inhibit lymphocyte proliferation by mitogens and alloantigens by different mechanisms. Experimental cell research. 2005;305:33–41. doi: 10.1016/j.yexcr.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 25.Ren G, Zhang L, Zhao X, Xu G, Zhang Y, Roberts AI, Zhao RC, Shi Y. Mesenchymal stem cell-mediated immunosuppression occurs via concerted action of chemokines and nitric oxide. Cell Stem Cell. 2008;2:141–150. doi: 10.1016/j.stem.2007.11.014. [DOI] [PubMed] [Google Scholar]
- 26.Reyes M, Lund T, Lenvik T, Aguiar D, Koodie L, Verfaillie CM. Purification and ex vivo expansion of postnatal human marrow mesodermal progenitor cells. Blood. 2001;98:2615–2625. doi: 10.1182/blood.v98.9.2615. [DOI] [PubMed] [Google Scholar]
- 27.Ryan JM, Barry F, Murphy JM, Mahon BP. Interferon-gamma does not break, but promotes the immunosuppressive capacity of adult human mesenchymal stem cells. Clin Exp Immunol. 2007;149:353–363. doi: 10.1111/j.1365-2249.2007.03422.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sato K, Ozaki K, Oh I, Meguro A, Hatanaka K, Nagai T, Muroi K, Ozawa K. Nitric oxide plays a critical role in suppression of T-cell proliferation by mesenchymal stem cells. Blood. 2007;109:228–234. doi: 10.1182/blood-2006-02-002246. [DOI] [PubMed] [Google Scholar]
- 29.Sordi V, Malosio ML, Marchesi F, Mercalli A, Melzi R, Giordano T, Belmonte N, Ferrari G, Leone BE, Bertuzzi F, Zerbini G, Allavena P, Bonifacio E, Piemonti L. Bone marrow mesenchymal stem cells express a restricted set of functionally active chemokine receptors capable of promoting migration to pancreatic islets. Blood. 2005;106:419–427. doi: 10.1182/blood-2004-09-3507. [DOI] [PubMed] [Google Scholar]
- 30.Sotiropoulou PA, Perez SA, Gritzapis AD, Baxevanis CN, Papamichail M. Interactions between human mesenchymal stem cells and natural killer cells. Stem Cells. 2006;24:74–85. doi: 10.1634/stemcells.2004-0359. [DOI] [PubMed] [Google Scholar]
- 31.Spaggiari GM, Capobianco A, Becchetti S, Mingari MC, Moretta L. Mesenchymal stem cell-natural killer cell interactions: evidence that activated NK cells are capable of killing MSCs, whereas MSCs can inhibit IL-2-induced NK-cell proliferation. Blood. 2006;107:1484–1490. doi: 10.1182/blood-2005-07-2775. [DOI] [PubMed] [Google Scholar]
- 32.Stagg J, Pommey S, Eliopoulos N, Galipeau J. Interferon-gamma-stimulated marrow stromal cells: a new type of nonhematopoietic antigen-presenting cell. Blood. 2006;107:2570–2577. doi: 10.1182/blood-2005-07-2793. [DOI] [PubMed] [Google Scholar]
- 33.Taylor A, Verhagen J, Blaser K, Akdis M, Akdis CA. Mechanisms of immune suppression by interleukin-10 and transforming growth factor-beta: the role of T regulatory cells. Immunology. 2006;117:433–442. doi: 10.1111/j.1365-2567.2006.02321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Terness P, Bauer TM, Rose L, Dufter C, Watzlik A, Simon H, Opelz G. Inhibition of allogeneic T cell proliferation by indoleamine 2,3-dioxygenase-expressing dendritic cells: mediation of suppression by tryptophan metabolites. J Exp Med. 2002;196:447–457. doi: 10.1084/jem.20020052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tse WT, Pendleton JD, Beyer WM, Egalka MC, Guinan EC. Suppression of allogeneic T-cell proliferation by human marrow stromal cells: implications in transplantation. Transplantation. 2003;75:389–397. doi: 10.1097/01.TP.0000045055.63901.A9. [DOI] [PubMed] [Google Scholar]
- 36.Wakitani S, Saito T, Caplan AI. Myogenic cells derived from rat bone marrow mesenchymal stem cells exposed to 5-azacytidine. Muscle & Nerve. 1995;18:1417–1426. doi: 10.1002/mus.880181212. [DOI] [PubMed] [Google Scholar]
- 37.Zappia E, Casazza S, Pedemonte E, Benvenuto F, Bonanni I, Gerdoni E, Giunti D, Ceravolo A, Cazzanti F, Frassoni F, Mancardi G, Uccelli A. Mesenchymal stem cells ameliorate experimental autoimmune encephalomyelitis inducing T-cell anergy. Blood. 2005;106:1755–1761. doi: 10.1182/blood-2005-04-1496. [DOI] [PubMed] [Google Scholar]