Abstract
Acute pancreatitis is an acute inflammatory disease of the pancreas which can lead to a systemic inflammatory response syndrome with significant morbidity and mortality in 20% of patients. Gallstones and alcohol consumption are the most frequent causes of pancreatitis in adults. The treatment of mild acute pancreatitis is conservative and supportive; however severe episodes characterized by necrosis of the pancreatic tissue may require surgical intervention. Advanced understanding of the pathology, and increased interest in assessment of disease severity are the cornerstones of future management strategies of this complex and heterogeneous disease in the 21st century.
Keywords: Acute necrotizing pancreatitis, Systemic inflammatory response syndrome, Surgery, Pancreatectomy, Minimal surgical procedures
INTRODUCTION
The death of Alexander the Great (356-323 BC) at the age of 33 has been ascribed to acute necrotizing pancreatitis secondary to rich food and heavy alcohol consumption[1].
In 1856, the great French physiologist Claude Bernard (1813-1878) demonstrated the capacity of pancreatic secretions to digest proteins, carbohydrate and fat[2]. However, the first review on acute pancreatitis (AP) was published by Reginald Huber Fitz (1843-1913) in 1889[3]. In his observation of 53 patients with clinical signs of AP, he believed that the disease was a complication of gastroduodenitis causing inflammation of the biliary duct.
Nevertheless, only in late 19th century did Chiari propose pancreatic autodigestion as the main pathological mechanism of the disease[4]. This theory facilitated the understanding of the late 19th and early 20th century clinicians in the pathophysiology of AP. In 1901, Eugen Opie proposed the “common channel hypothesis”, which was based on the assumption that a gallstone lodged in the ampulla could occlude both the common bile duct (CBD) and the pancreatic duct. The obstruction caused the formation of a common channel that would allow reflux of bile into the pancreatic duct with activation of pancreatic enzymes and pancreatitis[5,6].
The pathophysiology and treatment of AP has been intensely studied during the last century and our aim is to review recent evidence and achievements in the diagnosis and treatment of this serious condition at the beginning of the 21st century.
EPIDEMIOLOGY
AP is a growing problem in Europe, posing significant medical, surgical and financial sequelae[7]. A recent systematic review presented trends in incidence of the first attack of AP using data from 12 longitudinal studies[8]. The mean age of the first attack was in the 6th decade. This outcome can be explained by an increasing incidence of gallstone pancreatitis among white women over the age of 60 years[9,10]. The most common causes were gallstones (11%-56%), idiopathic (8%-44%) and alcohol (3%-66%). However, occult microlithiasis is probably responsible for most cases of idiopathic AP[11].
Gallstone AP was found to be more common in female subjects, alcohol pancreatitis more common amongst men and idiopathic pancreatitis similar in both sexes.
The incidence of AP has been reported to be markedly increasing[8,12,13]. The explanation of this increased incidence could be explained by the routine testing of pancreatic enzymes in patients presenting with abdominal pain at emergency departments, and in over-diagnosis in cases of non-specific increases in enzymes due to other causes. Another explanation is an increase in the incidence of gallstone disease and obesity in the population.
Although fatalities associated with AP have decreased over time from 15%-20% to below 5%, the population mortality rate has remained unchanged with increasing age associated with higher mortality[14–16]. A correlation with duration of disease was also shown with 65% of the deaths occurring in the first 14 d and 80% within 30 d[17].
Overall, severe AP (SAP) occurs in 10%-20% of patients and despite improvements in critical care between 10% and 25% of patients with SAP die[18,19].
PATHOPHYSIOLOGY
The pathogenesis of AP is caused by an inappropriate activation of trypsinogen to trypsin. Once activated these enzymes are responsible of autodigestion of pancreatic tissues resulting in necrosis of the acini and pancreatic islets with interstitial fat necrosis and necrotizing vasculitis[20].
These pathological changes in the pancreatic gland are responsible for releasing active pancreatic enzymes into the bloodstream and stimulating the production of inflammatory cytokines such as interleukin-1, interleukin-6 and interleukin-8 from neutrophils, macrophages and lymphocytes. The release of those interleukins and tumor necrosis factor-α (TNF-α) from macrophages triggers an inflammatory cascade which leads to the systemic inflammatory response syndrome (SIRS)[21]. SIRS may develop into acute respiratory distress syndrome or multiorgan dysfunction syndrome. This systemic inflammatory response to pancreatic injury marks the “first or early phase” of the natural course of SAP, which normally characterizes the first 14 d of the disease[21,22]. In this phase, organ failure is common and often is not associated with infection[23]. The “second or late phase” which starts 14 d after the onset of the disease, is marked by infection of the gland, necrosis and septic systemic complications causing a significant increase in mortality[24]. Infection of the necrotic pancreas occurs in the 8% to 12% of the patients with AP and in 30% to 40% of patients with necrotizing pancreatitis, and it is considered the most important risk factor of necrotic pancreatitis[25,26].
DIAGNOSIS
Abdominal pain together with elevation of plasma levels of pancreatic enzymes is the cornerstone of diagnosis. The pain normally is generalized in the upper abdomen and occurs suddenly without a prodrome. The pain, which tends to last a few days, is often radiated in a bandlike manner to the lower thoracic region of the back. Nausea and vomiting normally appear in about 90% of patients and can be severe. Physical signs of severe disease such as ecchymoses in the flank (Gray-Turner’s sign) or in the periumbilical region (Cullen sign) occurs in less than 3% of patients, and have been associated with a mortality of 37%[27]. Pancreatic enzymes are released into the circulation during an acute attack. Levels peak early, and decline over 3-4 d. As a consequence, the diagnosis should not rely on arbitrary levels 3 or 4 times greater than normal, but levels should be interpreted in light of the time since the onset of abdominal pain.
Enzymes released by acinar cells during an attack of AP are amylase and lipase, and their concentration in the serum is used to confirm the diagnosis[28]. The half-life of elevated amylase is shorter than that of lipase: the diagnosis using plasma lipase has slightly superior sensitivity and specificity and greater overall accuracy than amylase.
There are more specific tests in detection of AP, such as urinary trypsinogen activation peptide (TAP), serum and urinary trypsinogen[29–32], but these are less widely available.
Other laboratory tests can exclude metabolic causes such as hypercalcemia and lipid disorders.
AETIOLOGY
In order to optimize the instant management and prevent recurrence of AP it is essential identify the aetiology.
In the Western world, biliary tract disease (38%) and alcoholism (36%) are accountable for the majority of cases of AP[33]. However, in up to 10% of cases, the cause of AP remains unknown (idiopathic AP).
Gallstones
In patients with no history of alcohol consumption, an increased level of serum alanine aminotransferase up to 3 times its normal value is indicative of gallstone pancreatitis.
Gallstone pancreatitis, in most cases, is caused by gallstones passing into the bile duct and temporarily lodging at the sphincter of Oddi. However, duct obstruction can also be localized in the pancreatic duct. Although not completely proven, it is thought that duct obstruction leads to increased pancreatic duct pressure with subsequence injury to acinar cells and activation of digestive enzymes. It is supposed that only gallstones with a diameter up to 5 mm can migrate distally into the biliary duct whilst gallstones with a diameter of 8 mm or more remain in the gallbladder[34].
However, a biliary aetiology should not be excluded when liver function tests are normal since 15%-20% of patients with biliary AP can have normal concentrations of hepatic enzymes[35].
In cases where a biliary aetiology is suspected, the first line of investigation should be a trans-abdominal ultrasound (T-A US). The value of US lies in its ability to demonstrate gallbladder stones and dilatation of the CBD as well as other pathology unrelated to the pancreas. In the case of high clinical suspicion of a biliary cause of AP with normal T-A US, magnetic resonance cholangiopancreatography or endoscopic US should be performed in order to visualize the presence of microlithiasis or other causes of duct obstruction.
Alcohol
Alcohol consumption is the second cause of AP. Although the acinar cell is considered the main target of damage by ethanol, there is not an accepted explanation for why some patients are more predisposed to developing AP than others who consume similar quantities of alcohol. The pathogenesis of alcohol pancreatitis can be explained by a combination of environmental and genetic factors. Genetic studies have suggested that, in hereditary pancreatitis, mutation of the cationic trypsinogen gene and serine peptidase inhibitor, Kazal type 1 (SPINK1) genes can promote AP in the presence of alcohol[36].
Post-ERCP acute pancreatitis
The risk of developing AP after endoscopic retrograde cholangiopancreatography (ERCP) is around 5%[37]. The main risk factors for post-ERCP AP include female gender, presence of periampullary diverticulum, and procedure-related factors such as a cannulation time of more than 10 min and major papilla sphincterotomy. However, the risk of developing asymptomatic hyper-amylasemia, which appears in 35%-70% of patients, seems to be linked with procedure-related factors[38].
Trauma
Abdominal trauma causes an elevation of amylase and lipase levels in 17% of cases and clinical AP in 5% of cases. Pancreatic injury occurs more often in penetrating injuries (e.g. from knives, bullets) than in blunt abdominal trauma (e.g. from steering wheels, horses, bicycles). Blunt injury may crush the gland across the spine, leading to a ductal injury in that location[39].
Drug-induced pancreatitis
Drug-induced pancreatitis is considered a rare event (0.1%-2%) and is normally mild and self-limiting. In the literature, the true incidence of drug-induced AP is not known since the evidence is derived mainly from case reports and the diagnosis is always challenging because of the difficulty in distinguishing the effects of drugs from other causes of AP[40].
Drugs strongly associated with AP include azathioprine, sulfonamides, sulindac, tetracycline, valproic acid, didanosine, methyldopa, estrogens, furosemide, 6-mercaptopurine, pentamidine, 5-aminosalicylic acid compounds, corticosteroids, and octreotide.
Infections
Infections are accountable for less than 1% of all AP and tend to be milder than biliary and alcohol-induced AP[41]. Viral infections such as Epstein-Barr, coxsackie virus, echovirus, varicella-zoster and measles are the most common causes of infectious AP especially in children.
Bacterial causes include Mycoplasma pneumoniae, Salmonella typhosa, Leptospira, Campylobacter and Mycobacterium tuberculosis.
Worldwide, ascariasis can cause AP by migration of worms in and out of the duodenal papillae.
Hereditary pancreatitis
Hereditary pancreatitis is an autosomal dominant gain-of-function disorder related to mutations of the cationic trypsinogen gene (PRSS1), which has an 80% penetrance. Mutations in this gene cause premature conversion of trypsinogen to active trypsin causing pancreatic autodigestion. This genetic syndrome is associated with a high risk of developing chronic pancreatitis at a young age and of developing pancreatic cancer[42].
Mutations in the SPINK1 gene, which blocks the active binding site of trypsin, rendering it inactive, are associated with acute and chronic pancreatitis. Patients who have severe SPINK1 mutations normally develop chronic pancreatitis in childhood[43].
In patients with mild CFTR gene mutations, an increased risk of developing acute and chronic pancreatitis has been observed in comparison with the general population.
Hypercalcemia
Hypercalcemia and primary hyperparathyroidism can lead to AP. Hypercalcemia, which causes less than 1% of all cases of pancreatitis, normally appears with excessive doses of vitamin D, familial hypocalciuric hypercalcemia and total parenteral nutrition.
Hypertriglyceridemia
AP usually does not occur until serum triglyceride levels reach 1000 mg/dL. Hypertriglyceridemia causes about 2% of AP and it is normally associated with type I, Type II and Type V hyperlipidemia. The triglyceride level should be measured as soon as clinical presentation of AP appears since this level tends to decline during hospitalization because of fasting and IV fluid resuscitation.
Acquired hypertriglyceridemia can appear in adults because of alcoholism, obesity and poorly controlled diabetes mellitus.
In order to prevent recurrent attacks of AP, the patient should be placed on a low-fat diet, a regular exercise regimen, and tight control of diabetes, with use of lipid-lowering drugs such as statins.
Developmental abnormalities of the pancreas
The pancreas develops from two buds stemming from the alimentary tract of the developing embryo.
Pancreas divisum is a failure of the dorsal and ventral pancreatic ducts to fuse during embryogenesis and it occurs in about 5%-7% of the healthy population. Pancreatitis appears only in 5% of patients with pancreas divisum and it is thought to be the result of ductal hypertension caused by a narrow duct at its papillary origin.
Sphincter of Oddi dysfunction (SOD) is suspected clinically by recurrent episodes of epigastric or right upper quadrant pain that last 30 min or longer and that are not relieved by bowel movements or by antiacids[44]. SOD can lead to AP by causing increased pancreatic ductal pressure. However, SOD is a controversial cause of AP especially in patients without elevated sphincter pressures on manometry.
Tumor
Obstruction of the pancreatic ductal system by a tumor can increase the intraduct pressure and causing AP in proximately 14% of patients suffering from pancreatic tumors.
Pancreatic ductal carcinoma, ampullary carcinoma, islet cell tumor, solid pseudotumor of the pancreas, sarcoma, lymphoma, cholangiocarcinoma, or metastatic tumor can cause AP.
In addition, a pancreatic cystic neoplasm, such as intraductal papillary-mucinous neoplasm (IPMN), mucinous cystadenoma, or serous cystadenoma, can also cause AP[45].
Postoperative
AP may occur in the postoperative period of various surgical procedures. The mechanism of this pancreatitis includes transient intraoperative hypotension or pancreatic trauma by intraoperative manipulation. Postoperative AP is often a difficult diagnosis to confirm, and it has a higher complication rate than pancreatitis associated with other etiologies.
Autoimmune pancreatitis
This relatively newly described entity is an extremely rare cause of AP. The diagnosis of autoimmune pancreatitis has to be confirmed by specific radiological and histological findings. Radiologically, there is a focal mass in the pancreatic head on computed tomography (CT) scan and irregular narrowing of the proximal pancreatic duct on ERCP.
Patients normally have an elevated Ig G4 level in the serum and infiltration of IgG4-containing plasma cells in the pancreas. It normally occurs in young people who also suffer from inflammatory bowel disease, primary sclerosing cholangitis, primary biliary cirrhosis and Sjogren’s syndrome. The therapy of choice is based on steroids.
PREDICTION OF SEVERITY
Although, the majority of patients have a mild episode of AP, it is difficult to identify the patients who are at risk of developing severe disease on admission to the hospital.
There is agreement that there is still a need for an early objective measure of severity. Clinical examination in the first 24 h of admission although specific, lacks sensitivity and hence is unreliable and should be supported by objective measures[46].
Although there is no ideal single serum marker for predicting severity, C-reactive protein (cut-off of 150 mg/L) is a useful indicator of necrosis with a sensitivity and specificity of 80% but is required to be measured more than 48 h after the onset of symptoms[47–49].
Different markers of severity shown to be useful on admission are serum procalcitonin and urinary TAP and trypsinogen-2[50], serum interleukins-6 and -8 and polymorphonuclear elastase at 24 h after admission[51].
The severity of the inflammatory response to pancreatic injury and the presence of organ failure are normally assessed by scoring systems. Multi-factorial scoring systems based on clinical and laboratory findings such as the Ranson’s score, Glasgow Score and the Acute Physiology and Chronic Health Evaluation II (APACHE II) are considered accurate predictors of the severity of AP[52,53].
In 1974, John Ranson selected 11 prognostic signs based on statistical analysis of 43 parameters gathered retrospectively from 450 AP patients. Five of these criteria are measured on admission and the remaining 11 are measured 48 h post admission (Table 1).
Table 1.
Ranson’s criteria for prediction of severity of acute pancreatitis
| On admission | During initial 48 h |
| Age > 55 yr | Hemoglobin falls below 10 mg/dL |
| White cell count < 16 × 109/L | Blood urea nitrogen increases by > 5 mg/dL |
| Lactate dehydrogenase > 350 U/L | Calcium < 8 mg/dL |
| Aspartate aminotransferase > 250 U/L | PaO2 < 60 mmHg (8 kPa) |
| Glucose > 200 mg/dL | Base deficit > 4 mEq/L |
| Fluid sequestration > 6 L |
PaO2: Arterial partial pressure of oxygen.
The Glasgow severity scoring system considered 9 variables and can be applied from admission although it is not complete for 48 h[54] (Table 2).
Table 2.
Glasgow (Imrie) severity scoring system for acute pancreatitis
| Age > 55 yr |
| White cell count > 15 × 109/L |
| PaO2 < 60 mmHg (8 kPa) |
| Serum lactate dehydrogenase > 600 U/L |
| Serum aspartate aminotransferase > 200 U/L |
| Serum albumin < 32 g/L |
| Serum calcium < 2 mmol/L |
| Serum glucose > 10 mmol/L |
| Serum urea > 16 mmol/L |
Developed in 1985, the APACHE II score has been used to predict severity in AP patients[55]. APACHE II measures 12 physiological variables and additional points are added based on patient age and on severe baseline chronic diseases. Measuring APACHE II score daily can allow an assessment of progression of the disease[56].
Other markers should also be considered such as body mass index (BMI) since obesity has been shown to increase the risk of systemic complications and mortality[57]. This has led to a modification of the APACHE II scoring system which includes up to 2 points for obesity[58]. This system is called APACHE-O and although Johnson and colleagues have reported its superiority in predicting outcomes, other authors have not confirmed these results[59].
Although these scoring systems can help the physician in a first assessment of the patient, the most important distinction in terms of prediction of severity is the presence of severe manifestations of the disease such as evidence of SIRS and presence of organ failure.
Mofidi, in a recent retrospective study of 259 patients admitted with AP, showed that the mortality rate was significantly higher in patients who developed or had persistent SIRS at 48 h after admission (25.4%) than in patients who had transient SIRS (8%) or no SIRS in the first 48 h (0.7%)[60].
Therefore, immediate assessment should include clinical evaluation particularly of any cardiovascular, respiratory and renal compromise, BMI, chest X-ray and different acute diseases scores. The presence of any single and/or multiple organ failure has been increasingly recognized as an important variable for predicting mortality from AP. The most common organ dysfunction scores used for critically ill patients are the Multiple Organ Dysfunction Score (MODS) and the Sequential Organ Failure Assessment (SOFA)[61,62] (Tables 3 and 4).
Table 3.
Modified multiple organ dysfunction score
| Organ system involved |
Score |
||||
| 1 | 2 | 3 | 4 | 5 | |
| Cardiovascular PAHR (beats/min) | ≤ 10 | 10-15 | 30-15 | 20-30 | > 30 |
| Respiratory PaO2/FiO2 (mmHg) | > 300 | 300-225 | 150-225 | 75-150 | < 75 |
| Renal creatinine (μmol/L) | < 100 | 100-200 | 200-350 | 350-500 | > 500 |
| Neurological glasgow coma score | 15 | 14-13 | 12-10 | 9-7 | ≤ 6 |
| Hematological platelet count (× 109/L) | > 120 | 80-120 | 50-80 | 20-50 | ≤ 20 |
| Hepatic bilirubin (μmol/L) | < 20 | 20-60 | 60-120 | 120-240 | > 240 |
PAHR: Pressure-adjusted heart rate [heart rate × (right atrial pressure/mean arterial pressure]; FiO2: Fraction of inspired oxygen.
Table 4.
Sequential organ failure assessment score (SOFA)
| Organ system involved |
Score |
||||
| 1 | 2 | 3 | 4 | 5 | |
| Cardiovascular | No hypotension | MAP < 70 mmHg | Dopamine or dobutamine (any dose) | Dopamine > 5 μg/kg per min or adrenaline (epinephrine) < 0.1 μg/kg per min or noradrenaline (norepinephrine) < 0.1 μg/kg per min | Dopamine < 0.1 μg/kg per min or > 15 μg/kg per min or adrenaline > 0.1 μg/kg per min or noradrenaline > 0.1 μg/kg per min |
| Respiratory PaO2/FiO2 (mmHg) | > 400 | 400-300 | 300-200 | 200-1001 | ≤ 1001 |
| Renal creatinine (μmol/L) | < 100 | 100-200 | 200-350 | 350-500 | > 500 |
| Neurological glasgow coma score | 15 | 14-13 | 12-10 | 9-7 | ≤ 6 |
| Haematological platelet count (× 109/L) | > 150 | 150-100 | 100-50 | 20-50 | ≤ 20 |
| Hepatic bilirubin (μmol/L) | < 20 | 20-60 | 60-120 | 120-240 | > 240 |
These values are calculated with ventilatory support. MAP: Mean arterial pressure; SOFA: Sequential organ failure assessment, and is calculated as the sum of the scores for the individual organs.
Since the SOFA score uses the mean arterial pressure and therapeutic interventions with vasopressors, its outcome prediction for cardiovascular dysfunction is considered better than the MODS[63].
Since the mortality in the presence of pancreatic necrosis increases from 1% to 10%-23%, the importance of early detection of pancreatic necrosis is not to be overlooked[64]. Contrast-enhanced CT has been considered the “gold standard” for the diagnosis of pancreatic necrosis[65,66].
However, it is not clear how soon the full extent of the necrotic process occurs, but it is at least 4 d after onset of the symptoms, and early CT may therefore underestimate the final severity of the disease. Finally, unless some management decision is required based on the extent of necrosis (for example use of prophylactic antibiotics), CT for staging is unlikely to materially affect the management of patients with AP during the first week of the illness. If CT staging of AP is required, the CT severity index (CTSI) as proposed by Balthazar should be used (Table 5). Recent studies demonstrated that AP patients with a CTSI higher than 5 had 8 times higher mortality. Moreover, they were 17 times more likely to have a prolonged hospital course and were 10 times more likely to require necrosectomy than their counterparts with CT scores < 5[67]. There is also evidence that the site of pancreatic necrosis is an important prognostic factor with a worse outcome observed in patients with necrosis affecting the head of the pancreas[68]. The finding of free intraperitoneal fluid and extensive peri-pancreatic fat stranding have also been demonstrated to be associated with worse outcomes.
Table 5.
Acute pancreatitis graded with CT and CT severity index table
| Grade | CT finding | Points |
Necrosis |
Severity index | |
| Percentage | Additional points | ||||
| A | Normal pancreas | 0 | 0 | 0 | 0 |
| B | Pancreatic enlargement | 1 | 0 | 0 | 1 |
| C | Pancreatic inflammation and/or peripancreatic fat | 2 | < 30 | 2 | 4 |
| D | Single peripancreatic fluid collection | 3 | 30-50 | 4 | 7 |
| E | Two or more fluid collections and/or retroperitoneal air | 4 | > 50 | 6 | 10 |
Although CT is useful in detecting pancreatic necrosis, it is not able to detect a super-infection of necrosis in the later stage of the disease unless gas bubbles are seen within the necrotic area[69].
Patients with persisting organ failure, or in whom new organ failure develops, and in those with persisting pain and signs of sepsis, will require evaluation by dynamic contrast enhanced CT. CT evidence of necrosis correlates well with the risk of other local and systemic complications.
Since pancreatic necrosis commonly remains stable in appearance, a follow-up CT scan at 3 to 4 wk is not normally considered[70].
MANAGEMENT OF MILD AP
In most cases AP is mild and its initial management is directed towards maintenance of adequate organ perfusion in order to reduce the systemic complications caused by the pancreatic injury. This consists of fluid resuscitation, analgesia, oxygen administration, antiemetics and repeated evaluation of the patient’s vital signs with the intention of identifying early manifestations of organ dysfunction.
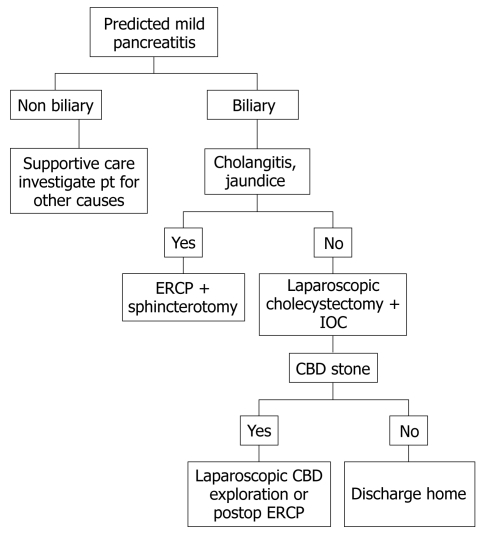
Since fluid loss in mild pancreatitis can be significant, appropriate fluid resuscitation is a crucial part of the management in order to improve the microcirculation of the pancreas (Figure 1).
Figure 1.
Algorithm for management of mild acute pancreatitis. IOC: Intraoperative cholangiography; CBD: Common bile duct.
As a marker of third-space losses, hemoconcentration has been associated with a higher probability of developing pancreatic necrosis and organ failure[71]. Moreover, patients who experienced a worsening or a lack of improvement of their hemoconcentration after 24 h of fluid resuscitation have a higher chance of developing necrotizing pancreatitis[72]. Therefore, all patients with AP should receive very close clinical monitoring with emphasis on vigorous fluid resuscitation. Rehydratation has to be monitored with the help of invasive monitoring such as a Foley catheter and a central line to measure the urine output and central venous pressure, respectively. Patients who have borderline cardiac dysfunction or respiratory failure may require a Swann-Ganz catheter. Crystalloids are preferred to colloids in most instances. However, electrolyte disturbances and fluid overload can be serious complications of fluid resuscitation especially in patients who have developed cardiovascular dysfunction or acute respiratory distress syndrome.
Adequate pain control is essential. Parenteral analgesia is usually needed with an advantage in using patient-controlled analgesia. Opiates are normally used including morphine and meperidine. Since there are no studies directly comparing the effects of meperidine or morphine on sphincter of Oddi manometry, morphine seems to provide more benefit by offering a longer duration of action and fewer side effects[73].
Supplemental oxygen is required in all patients. The oxygen saturation should be maintained at 95% or higher with supplemental oxygen administered by nasal cannula or by a face mask in order to prevent pancreatic necrosis.
The role of activated protease in producing organ failure is not clear. Although antiprotease treatment has been successful in experimental pancreatitis, it has not been shown to offer a survival benefit, but only a reduction of the incidence of complications in human disease[74,75].
Since cytokines could play an important role in AP, many agents have been used in experimental animals to ameliorate or prevent the inappropriate activation of the immune systems.
Anti-TNF-α antibody has been shown to reduce the induction of further cytokines by inflammatory cells but the peak TNF-α production appears to be within 1 or 2 h of the onset of disease. This action can compromise the use of TNF-α blockers in the clinical setting since the presentation and diagnosis of disease occurs after the peak of TNF-α production[76–78].
The role of calcium channel signaling in cytokine release and systemic organ injury in AP has been reported in one animal study. In this study, Hughes demonstrated that calcium channel blockers were associated with a dramatic reduction of TNF-α release with an improvement in overall survival from 40% to 80% between untreated rats and animals pre-treated with diltiazem, respectively[79].
An interleukin-1 receptor antagonist has been shown to be associated with decreased severity of pancreatitis in animal models, however these results have not been translated into clinical practice so far[80,81].
Since acute lung injury in AP results in an up-regulation of vascular adhesion molecule-1 (VCAM-1) cell surface receptor expression on pulmonary vascular endothelium, and neutrophil sequestration, experimental studies showed that blocking VCAM-1 decreased lung injury in AP[82,83]. It is believed that a VCAM-1 antagonist can offer a therapeutic option to improve the systemic manifestation and therefore the prognosis of AP.
Administration of monoclonal antibodies directed against the adhesion molecule, junctional adhesion molecule C expressed by endothelial cells showed a significant reduction in secretion of inflammatory cytokines, and in acinar cell necrosis[84].
Recently, there have been reports considering 5-fluorouracil treatment more effective compared to single inflammatory cytokine blockers in modulation of inflammatory mediators in experimental AP[85]. However, although the last decade has seen an increase in experimental studies on cytokines, the clinical treatment of the disease remains unchanged.
MANAGEMENT OF SAP: “EARLY PHASE”
SAP is defined by the Atlanta classification as an AP with local and/or systemic complications[86]. Some patients develop pancreatitis-associated organ failure during the early phase of the SAP[87].
The initial management of SAP is supportive based on fluid resuscitation, analgesia and enteral nutrition.
All patients should have thrombo-prophylaxis with low molecular weight heparin; however the decision to begin stress ulcer prophylaxis is still debatable.
SAP induces a catabolic state. Hence, early nutritional support is essential in order to avoid malnutrition.
An important issue in the early treatment of SAP is the optimal delivery of nutrition. After initial enthusiasm towards parenteral nutrition (PN), recent guidelines advise early enteral nutrition (EN) through a nasojejunal tube[88]. Patients with AP are characterized by loss of the gut barrier function which is involved in both local and systemic infectious complications[89]. In a meta-analysis analyzing 5 randomized control trials since 1997, Petrov et al[90] showed that EN, compared to PN, had a statistically significant lower risk of infection and mortality. Although there are studies supporting a lower infection rate when the tube is positioned in the jejunum, Eatock et al[91] demonstrated that nasogastric feeding is as good as nasojejunal feeding.
Although the role of probiotics in AP has been investigated in different clinical trials and meta-analyses, in a recent randomized controlled trial Besselink et al[92] showed that, in patients with predicted SAP, probiotic prophylaxis did not reduce the risk of infectious complications and was even associated with an increased risk of death.
Although the main management in the early phase of SAP is advocated to be mainly conservative and supportive in order to avoid organ dysfunction, there are conditions such as gallstone pancreatitis for which early endoscopic or surgical intervention has to be sought.
The benefits of ERCP with sphincterotomy (ES) has been studied in 3 randomized trials[93–95] and 2 meta-analyses[96,97]. Patients with predicted mild acute biliary pancreatitis (ABP) in the absence of cholangitis have not shown benefits from an early ERCP.
The decision on management of patients with predicted severe ABP is still debatable. The most recent United Kingdom guidelines recommend that urgent therapeutic ERCP should be performed within 72 h of admission in all patients with predicted severe ABP, whether or not cholangitis is present[98].
However, a recent meta-analysis by Petrov et al[97] demonstrated that early ERCP with or without ES had no beneficial effect in patients with predicted mild or severe ABP without cholangitis. The conclusion of this study was partially supported by the 2007 guidelines of the American Gastroenterology Association which stated that early ERCP in patient with severe ABP without signs of acute cholangitis is still not uniformly accepted in the literature[99].
However, optimal timing of laparoscopic cholecystectomy (LC) in patients with ABP is still contentious. In mild ABP, LC with operative cholangiography has been considered the definitive treatment[100].
Early laparoscopic cholecystectomy (ELC) can be performed as soon as the serum amylase decreases and symptoms improve[101].
Heinrich et al recently analyzed 4 prospective trials evaluating the optimal timing for surgery and concluded that ELC should be preferred in patients with mild to moderate ABP while in patients with severe ABP who did not have surgery for necrotizing pancreatitis, cholecystectomy appears to be favorable after full recovery[101–105].
MANGEMENT OF SAP: “LATE PHASE”
The main life-threatening event which characterizes the late phase of SAP is infection of the necrotic pancreatic parenchyma. Infection tends to occur in 10% to 50% of patients with necrotizing pancreatitis and develops 2-3 wk after the onset of symptoms[26,106–108]. The mortality increases from 5%-25% in patients with sterile necrosis to 15%-28% when infection occurs[24,107,109–112].
The infection is thought to be caused by translocation of enteric flora from the small and large bowel, since gram-negative bacteria such as Esherichia coli has been the most common species isolated. The use of antibiotic prophylaxis has changed the microbiology in favor of gram-positive and fungal organisms such as Staphylococcus species and Candida[113–116].
The debate on prophylactic antibiotics in sterile necrotic pancreatitis is still open. Since 1991, when Bradley introduced the concept of conservative treatment of sterile necrotic pancreatitis with the use of antibiotics, different randomized, controlled trials were conducted in order to investigate the beneficial effects of antibiotic therapy[117]. Initial studies were conducted with imipenem, ciprofloxacin and metronidazole[118–121].
These studies showed that antibiotic prophylaxis in SAP is capable of reducing the incidence of bacterial infection of pancreatic necrosis but it was unable to improve hospital mortality.
Two placebo-controlled, double-blind trials by Isenmann and Dellinger demonstrated a lack of significant benefit of prophylactic antibiotics on infection and surgical intervention rates[122,123]. However, a recent Cochrane meta-analysis, which included the Isenmann study, showed a reduction in mortality with the use of β-lactams, although there was no evidence of a reduction in the pancreatic necrosis infection rate[124].
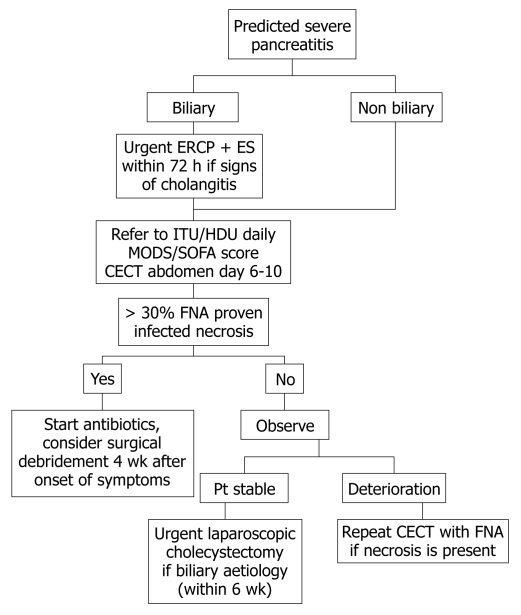
Despite the requirement for further multicenter double-blind studies, the use of prophylactic antibiotics in patients with proven necrotic pancreatitis on CT has been advocated. β-lactam agents are preferred to quinolones and the length of the therapy has to be at least 2 wk (Figure 2).
Figure 2.
Algorithm for management of severe acute pancreatitis. ERCP: Endoscopic retrograde cholangiopancreatography; ES: ERCP with sphincterotomy; Pt: Patient; MODS: Multiple organ dysfunction score; SOFA: Sequential organ failure assessment; CECT: Contrast-enhanced computed tomography; FNA: Fine needle aspiration.
SURGICAL INTERVENTION
Surgery is considered the gold standard treatment for proven infected pancreatic necrosis[125].
Since Bradley has introduced the concept of conservative treatment in non-infected pancreatic necrosis, the timing of surgical intervention has changed substantially[117]. In the past, early surgical intervention was advocated and had a mortality rate up to 65%[126,127]. Recent studies demonstrated the benefit of postponing surgical intervention in reducing the mortality rate to 27%, allowing the immune system to demarcate the pancreatic necrosis[128,129].
The IAP (International Association of Pancreatology) Guidelines recommend that a patient with infected necrotic pancreatitis has to undergo surgery in the 3rd or 4th wk after the onset of symptoms[88]. However, postponing surgical intervention in necrotic pancreatitis can lead to prolonged use of antibiotics and an increased antibiotic resistance and higher incidence of Candida infection[130,131].
In a recent retrospective study, Besselink strongly advised avoidance of surgical intervention in the first 14 d even in the presence of multiple organ failure, and withholding of necrosectomy until day 30[132].
The aim of surgical management is to remove all the pancreatic tissue with necrosis in order to reduce the release of inflammatory mediators. Necrosectomy and drainage of infected acute necrotizing pancreatitis can be performed with different approaches such as radiological, endoscopical and surgical intervention.
Radiologic necrosectomy
Since Freeny presented the first series of patients with infected necrotic pancreatitis treated with only CT-guided percutaneous catheter drainage in 1998, this approach has not been considered very successful in debriding thick necrotic pancreatic tissue[133–135]. However, a combination of percutaneous catheter drainage and intensive care support can offer an alternative to surgery[136]. In unstable patients, percutaneous catheter drainage can be successful in draining pus and reducing the systemic manifestations of sepsis and in doing so, prepare the patient for surgery[133].
The placement of the catheter can be obtained through an anterior or retroperitoneal approach. To achieve an adequate drainage of the thick pancreatic necrotic collection, catheters with multiple side holes with a minimum diameter of 12-14 Fr are required[137]. Percutaneous drainage can lead to suprainfection of the pancreatic collection due to colonization of the indwelling catheter. However, clinical infection has been shown to be unlikely if all material is drained within 2-3 d.
Endoscopic necrosectomy
The endoscopic approach with the help of endoscopic US (EUS) has been reported to be effective in recent retrospective studies[138–141]. This technique can be considered as a natural orifice transluminal endoscopic surgery (NOTES) procedure since it employs a transenteric access route.
The most common access is through the posterior wall of the stomach under EUS and under Doppler imaging in order to avoid vascularized areas. The procedure is normally performed under sedation and requires good endoscopic skills.
Initially, a trans-gastric puncture under EUS guidance is performed using a 19-gauge needle through which a guidewire is passed into the cavity and coiled multiple times under fluoroscopic vision. The tract is dilated by a dilator which is passed over the guide and further dilatations can be done using 10-15 mm balloons. This dilation will allow an optimal insertion of the upper endoscope into the pancreatic cavity. The necrosectomy is performed using different devices such as polypectomy snare, transparent cap baskets and different graspers.
The debridement of necrotic tissue is followed by copious irrigation with normal saline solution. A pig-tail drain inserted into the cavity and a nasocystic drain are used for continuous lavage. The lavage has to be repeated until all the necrotic material is removed[139,140]. The use of antibiotics is advised until the nasocystic drain has been removed.
Although optimal necrosectomy is normally achieved with multiple sessions, in a recent retrospective study which included 6 consecutive patients, Mathew et al[139] demonstrated that complete removal of necrotic tissue can be achieved with a single procedure. In this study none of the patients had procedure-related complications; however injury to visceral and vascular structures must be borne in mind as potential life-threatening complications.
Recent data from the literature indicated that the endoscopic approach could be a safe and effective modality for management of infected pancreatic necrosis with potentially lower morbidity than the traditional surgical approach. However, the data was from small prospective studies and multicenter prospective randomized trials are needed to clarify the role of the endoscopic approach in necrotic pancreatitis.
Surgical necrosectomy
The aim of surgery is to control the focus of infection through removal of necrotic tissue. This is based on preserving the endocrine and exocrine functions of the pancreas and allowing postoperative removal of retroperitoneal debris and exudates.
Until recently, necrosectomy was generally performed only by an open route. In order to achieve postoperative continuous drainage of debris, 4 different techniques have been advocated[142]: (1) open necrosectomy with open packing and planned re-laparotomy[143–149]; (2) open necrosectomy with planned re-laparotomy, staged and repeated lavage[150–153]; (3) open necrosectomy with continuous lavage of the lesser sac and retroperitoneum[153–161]; (4) open necrosectomy with closed packing[162].
Open necrosectomy with open packing and planned re-laparotomy: The abdominal cavity is filled with non-adherent packing. Successive laparotomies are performed every 48 h for further debridement which can be performed in intensive care under sedation. The abdomen is closed with drains when granulation tissue appears.
Open necrosectomy with planned re-laparotomy, staged and repeated lavage: After a primary necrosectomy repeated debridement is performed on alternate days until all necrotic tissue has been replaced by granulation tissue. To improve the surgical access some surgeons use an abdominal wall zip.
Open necrosectomy with continuous lavage of the lesser sac and retroperitoneum: Primary necrosectomy is followed by continuous closed lavage of the retroperitoneum. The procedure is based on insertion of 2 or more double 20-24 French drains and a single lumen 28-38 French silicone rubber on each side of the abdomen and placed with the tip at the tail of the pancreas. The smaller lumen of the drains is used for the inflow of the lavage and the larger lumen for the outflow. At least 35-50 L lavage are requested in the first days. Drains can be removed after 2-3 wk.
Open necrosectomy with closed packing: After the removal of the necrotic tissue, the residual cavity is filled with gauze-packed Penrose drains and suction drains. Drains are removed after 7 d.
Of these techniques open necrosectomy with closed continuous lavage of the lesser sac and the retroperitoneum seems to have the lowest mortality and it is the most common approach used by surgeons.
In specialized centers, open surgical management of infected necrosis can reduced the mortality from 80% to 10%-20%. This high mortality has induced surgeons to find a new, less invasive approach in order to reduce the activation of an inflammatory response in patients who are already seriously ill.
MINIMAL INVASIVE SURGICAL APPROACH
Over the last 2 decades, the role of minimal invasive surgical approaches to necrotic pancreatitis has increased. Minimal invasive techniques can be classified under 2 groups: (1) video-assisted retroperitoneal debridement (VARD) and (2) laparoscopic transperitoneal debridement (LTPD).
VARD
This approach was first described by Carter et al[163] in 2000 using an operative nephroscope inserted over an 8 Fr pigtail catheter, positioned under CT guidance. Since this initial experience, different studies have performed necrosectomy through a retroperitoneal approach using a rigid nephroscope or zero degree laparoscope.
This technique is performed by placing the patient in a supine position with his left flank elevated. A subcostal or intercostal incision is made to follow the retroperitoneal drains up to the necrotic area which is opened bluntly through digital examination. Necrotic tissue is debrided by a ring forceps and a suction device. A 10 mm laparoscope and a long 10 mm trocar are inserted through the retroperitoneal wound. Under laparoscopic vision, the remaining necrotic tissue is removed by laparoscopic graspers. Two surgical drains are inserted into the necrotic cavity via the incision[164–170].
Recently, Bucher et al[170] described a new technique based on a single laparoscopic port in order to avoid repeated necrosectomies. Using a 5 mm laparoscope with a 30 degree optic, a 12 mm trocar was placed in the drain tract. Through this big trocar, 5 mm instruments were used simultaneously with the 5 mm laparoscope. The necrotic cavity was dilated by insufflation with CO2 at a pressure of 8 mmHg in order to avoid potential bacterial translocation. At the end the procedure, the cavity was inspected with a 30 degree 10 mm laparoscope. Among 8 patients who underwent this new procedure only one did not have a successful debridement and had repeated necrosectomy.
The VARD approach has the great advantage of avoiding peritoneal contamination but is limited in necrosis extraction, and the need for repeated sessions is quite common. Other limitations of VARD are its low ability in detecting colonic ischemia, and in performing cholecystectomy or insertion of a feeding jejunal tube at the time of debridement[141].
LTPD
Cuschieri described for the first time the technique of laparoscopic infracolic necrosectomy with irrigation of the lesser sac as a valid alternative to open necrosectomy[171].
Although this laparoscopic technique has been described in the literature through case reports since 2002[172–175], only recently Parehk reported a retrospective study on hand-assisted laparoscopic surgery for pancreatic necrosectomy[174]. This study described 18 patients with necrotizing pancreatitis who underwent laparoscopic necrosectomy using an infracolic approach to access the lesser sac with a hand access port in order to enlarge the window in the transverse mesocolon and to bluntly remove the necrotic tissue. The outcomes were encouraging with mean length of stay of 16.3 d after the procedure and a reduction in the incidence of major wound complications.
This technique gives a better exposure of the lesser sac, left paracolic gutter and head of the pancreas, apparently overcoming the main limitation of the retroperitoneal approach in not debriding necrotic tissue completely. On the other hand the transperitoneal approach carries the risk of peritoneal contamination with infected necrosis.
Despite the use of less invasive techniques, complications following debridement of necrotic pancreatic tissue are still common. Pancreatic or enterocutaneous fistulae occur in 30% of patients and it seems related to the severity and extent of the underline necrosis[176]. Fistulae should be managed conservatively initially, deferring surgical closure of fistulae until pancreatitis is completely resolved. Other early complications are wound infection and wound dehiscence which seems less common with the minimal invasive approach. Postoperative bleeding is normally treated through an endovascular procedure with the help of an interventional radiologist.
Late complications such as pancreatic insufficiency and development of organized sterile necrosis are also common[177].
CONCLUSION
Although most patients with AP will have a benign outcome, it is crucial to assess the patient using multi-factorial scoring systems and inflammatory markers in order to evaluate the severity of the condition.
Early management should be conservative, based on fluid resuscitation with a focus on maintaining optimal organ perfusion. Managing the patient in the ICU should be contemplated when patients show signs of clinical deterioration.
A CT scan should be performed at least 48 h after the onset of symptoms and is considered the gold standard for diagnosis of necrotic pancreatitis. As part of the conservative intensive treatment, nasojejunal feeding is recommended in order to reduce bacterial translocation.
In ABP, early ERCP in patients without signs of acute cholangitis is not recommended. Infected necrotizing pancreatitis is the main indication for surgical debridement. The best time of surgery is 3-4 wk after the onset of the condition.
The last 2 decades have seen the emergence of new minimal invasive approaches in performing surgical debridement. However, no randomized controlled studies have been published in comparing different techniques.
Nevertheless, the results of the PANTER trial, a prospective multi-institutional randomized study comparing VARD versus open laparotomy, are still awaited[178].
Peer reviewers: Jens Werner, MD, Associate Professor, Department of General and Visceral Surgery, University of Heidelberg, INF 110, Heidelberg 69120, Germany; Rakesh Kumar Tandon, Professor, Pushpawati Singhania Research Institute for Liver, Renal and Digestive Diseases, Sheikh Sarai-Phase II, New Delhi 110017, India
S- Editor Li LF L- Editor Cant MR E- Editor Lin YP
References
- 1.Sbarounis CN. Did Alexander the Great die of acute pancreatitis? J Clin Gastroenterol. 1997;24:294–296. doi: 10.1097/00004836-199706000-00031. [DOI] [PubMed] [Google Scholar]
- 2.Bernard C. Lecons de physiologie experimentale appliquee a la medecine. 2 vols. Paris: Bailliere, 1855-1856. [Google Scholar]
- 3.Fitz RH. Acute Pancreatitis: a consideration of pancreatic hemorrhage, hemorrhagic, suppurative and gangrenous pancreatitis of disseminated fat necrosis. Boston Med Surg J. 1889;120:181–235. [Google Scholar]
- 4.Chiari H. Über selbstverdauung des menschlichen Pancreas. Z Heilk. 1896;17:69–96. [Google Scholar]
- 5.Opie EL. The etiology of acute hemorrhagic pancreatitis. Johns Hopks Hosp Bull. 1901;12:182–188. [Google Scholar]
- 6.O'Reilly DA, Kingsnorth AN. A brief history of pancreatitis. J R Soc Med. 2001;94:130–132. doi: 10.1177/014107680109400308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Neoptolemos JP, Raraty M, Finch M, Sutton R. Acute pancreatitis: the substantial human and financial costs. Gut. 1998;42:886–891. doi: 10.1136/gut.42.6.886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yadav D, Lowenfels AB. Trends in the epidemiology of the first attack of acute pancreatitis: a systematic review. Pancreas. 2006;33:323–330. doi: 10.1097/01.mpa.0000236733.31617.52. [DOI] [PubMed] [Google Scholar]
- 9.Chwistek M, Roberts I, Amoateng-Adjepong Y. Gallstone pancreatitis: a community teaching hospital experience. J Clin Gastroenterol. 2001;33:41–44. doi: 10.1097/00004836-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Lévy P, Boruchowicz A, Hastier P, Pariente A, Thévenot T, Frossard JL, Buscail L, Mauvais F, Duchmann JC, Courrier A, et al. Diagnostic criteria in predicting a biliary origin of acute pancreatitis in the era of endoscopic ultrasound: multicentre prospective evaluation of 213 patients. Pancreatology. 2005;5:450–456. doi: 10.1159/000086547. [DOI] [PubMed] [Google Scholar]
- 11.Cavallini G, Frulloni L, Bassi C, Gabbrielli A, Castoldi L, Costamagna G, De Rai P, Di Carlo V, Falconi M, Pezzilli R, et al. Prospective multicentre survey on acute pancreatitis in Italy (ProInf-AISP): results on 1005 patients. Dig Liver Dis. 2004;36:205–211. doi: 10.1016/j.dld.2003.11.027. [DOI] [PubMed] [Google Scholar]
- 12.Frey CF, Zhou H, Harvey DJ, White RH. The incidence and case-fatality rates of acute biliary, alcoholic, and idiopathic pancreatitis in California, 1994-2001. Pancreas. 2006;33:336–344. doi: 10.1097/01.mpa.0000236727.16370.99. [DOI] [PubMed] [Google Scholar]
- 13.Lindkvist B, Appelros S, Manjer J, Borgström A. Trends in incidence of acute pancreatitis in a Swedish population: is there really an increase? Clin Gastroenterol Hepatol. 2004;2:831–837. doi: 10.1016/s1542-3565(04)00355-6. [DOI] [PubMed] [Google Scholar]
- 14.Corfield AP, Cooper MJ, Williamson RC. Acute pancreatitis: a lethal disease of increasing incidence. Gut. 1985;26:724–729. doi: 10.1136/gut.26.7.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trapnell JE, Duncan EH. Patterns of incidence in acute pancreatitis. Br Med J. 1975;2:179–183. doi: 10.1136/bmj.2.5964.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eland IA, Sturkenboom MC, van der Lei J, Wilson JH, Stricker BH. Incidence of acute pancreatitis. Scand J Gastroenterol. 2002;37:124. doi: 10.1080/003655202753387473. [DOI] [PubMed] [Google Scholar]
- 17.Floyd A, Pedersen L, Nielsen GL, Thorladcius-Ussing O, Sorensen HT. Secular trends in incidence and 30-day case fatality of acute pancreatitis in North Jutland County, Denmark: a register-based study from 1981-2000. Scand J Gastroenterol. 2002;37:1461–1465. doi: 10.1080/003655202762671369. [DOI] [PubMed] [Google Scholar]
- 18.McKay CJ, Imrie CW. The continuing challenge of early mortality in acute pancreatitis. Br J Surg. 2004;91:1243–1244. doi: 10.1002/bjs.4750. [DOI] [PubMed] [Google Scholar]
- 19.Gloor B, Müller CA, Worni M, Martignoni ME, Uhl W, Büchler MW. Late mortality in patients with severe acute pancreatitis. Br J Surg. 2001;88:975–979. doi: 10.1046/j.0007-1323.2001.01813.x. [DOI] [PubMed] [Google Scholar]
- 20.Hirano T, Manabe T. A possible mechanism for gallstone pancreatitis: repeated short-term pancreaticobiliary duct obstruction with exocrine stimulation in rats. Proc Soc Exp Biol Med. 1993;202:246–252. doi: 10.3181/00379727-202-43534. [DOI] [PubMed] [Google Scholar]
- 21.Norman J. The role of cytokines in the pathogenesis of acute pancreatitis. Am J Surg. 1998;175:76–83. doi: 10.1016/s0002-9610(97)00240-7. [DOI] [PubMed] [Google Scholar]
- 22.Gloor B, Reber HA. Effects of cytokines and other inflammatory mediators on human acute pancreatitis. J Int Care Med. 1998;13:305–312. [Google Scholar]
- 23.Tenner S, Sica G, Hughes M, Noordhoek E, Feng S, Zinner M, Banks PA. Relationship of necrosis to organ failure in severe acute pancreatitis. Gastroenterology. 1997;113:899–903. doi: 10.1016/s0016-5085(97)70185-9. [DOI] [PubMed] [Google Scholar]
- 24.Beger HG, Bittner R, Block S, Büchler M. Bacterial contamination of pancreatic necrosis. A prospective clinical study. Gastroenterology. 1986;91:433–438. doi: 10.1016/0016-5085(86)90579-2. [DOI] [PubMed] [Google Scholar]
- 25.Beger HG, Rau B, Mayer J, Pralle U. Natural course of acute pancreatitis. World J Surg. 1997;21:130–135. doi: 10.1007/s002689900204. [DOI] [PubMed] [Google Scholar]
- 26.Bassi C, Falconi M, Girelli R, Nifosi F, Elio A, Martini N, Pederzoli P. Microbiological find-ings in severe pancreatitis. Surg Res Commun. 1989;5:1–4. [Google Scholar]
- 27.Meyers MA, Feldberg MA, Oliphant M. Grey Turner's sign and Cullen's sign in acute pancreatitis. Gastrointest Radiol. 1989;14:31–37. doi: 10.1007/BF01889150. [DOI] [PubMed] [Google Scholar]
- 28.Matull WR, Pereira SP, O'Donohue JW. Biochemical markers of acute pancreatitis. J Clin Pathol. 2006;59:340–344. doi: 10.1136/jcp.2002.002923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Neoptolemos JP, Kemppainen EA, Mayer JM, Fitzpatrick JM, Raraty MG, Slavin J, Beger HG, Hietaranta AJ, Puolakkainen PA. Early prediction of severity in acute pancreatitis by urinary trypsinogen activation peptide: a multicentre study. Lancet. 2000;355:1955–1960. doi: 10.1016/s0140-6736(00)02327-8. [DOI] [PubMed] [Google Scholar]
- 30.Lempinen M, Stenman UH, Halttunen J, Puolakkainen P, Haapiainen R, Kemppainen E. Early sequential changes in serum markers of acute pancreatitis induced by endoscopic retrograde cholangiopancreatography. Pancreatology. 2005;5:157–164. doi: 10.1159/000085267. [DOI] [PubMed] [Google Scholar]
- 31.Kylänpää-Bäck ML, Kemppainen E, Puolakkainen P, Hedström J, Haapiainen R, Korvuo A, Stenman UH. Comparison of urine trypsinogen-2 test strip with serum lipase in the diagnosis of acute pancreatitis. Hepatogastroenterology. 2002;49:1130–1134. [PubMed] [Google Scholar]
- 32.Lempinen M, Stenman UH, Finne P, Puolakkainen P, Haapiainen R, Kemppainen E. Trypsinogen-2 and trypsinogen activation peptide (TAP) in urine of patients with acute pancreatitis. J Surg Res. 2003;111:267–273. doi: 10.1016/s0022-4804(03)00044-1. [DOI] [PubMed] [Google Scholar]
- 33.Whitcomb DC. Clinical practice. Acute pancreatitis. N Engl J Med. 2006;354:2142–2150. doi: 10.1056/NEJMcp054958. [DOI] [PubMed] [Google Scholar]
- 34.Diehl AK, Holleman DR Jr, Chapman JB, Schwesinger WH, Kurtin WE. Gallstone size and risk of pancreatitis. Arch Intern Med. 1997;157:1674–1678. [PubMed] [Google Scholar]
- 35.Dholakia K, Pitchumoni CS, Agarwal N. How often are liver function tests normal in acute biliary pancreatitis? J Clin Gastroenterol. 2004;38:81–83. doi: 10.1097/00004836-200401000-00017. [DOI] [PubMed] [Google Scholar]
- 36.Lucrezio L, Bassi M, Migliori M, Bastagli L, Gullo L. Alcoholic pancreatitis: new pathogenetic insights. Minerva Med. 2008;99:391–398. [PubMed] [Google Scholar]
- 37.Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909–918. doi: 10.1056/NEJM199609263351301. [DOI] [PubMed] [Google Scholar]
- 38.Wang P, Li ZS, Liu F, Ren X, Lu NH, Fan ZN, Huang Q, Zhang X, He LP, Sun WS, et al. Risk factors for ERCP-related complications: a prospective multicenter study. Am J Gastroenterol. 2009;104:31–40. doi: 10.1038/ajg.2008.5. [DOI] [PubMed] [Google Scholar]
- 39.Cappell MS. Acute pancreatitis: etiology, clinical presentation, diagnosis, and therapy. Med Clin North Am. 2008;92:889–923, ix-x. doi: 10.1016/j.mcna.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 40.Balani AR, Grendell JH. Drug-induced pancreatitis : incidence, management and prevention. Drug Saf. 2008;31:823–837. doi: 10.2165/00002018-200831100-00002. [DOI] [PubMed] [Google Scholar]
- 41.Parenti DM, Steinberg W, Kang P. Infectious causes of acute pancreatitis. Pancreas. 1996;13:356–371. doi: 10.1097/00006676-199611000-00005. [DOI] [PubMed] [Google Scholar]
- 42.Teich N, Mössner J. Hereditary chronic pancreatitis. Best Pract Res Clin Gastroenterol. 2008;22:115–130. doi: 10.1016/j.bpg.2007.10.019. [DOI] [PubMed] [Google Scholar]
- 43.Schneider A, Barmada MM, Slivka A, Martin JA, Whitcomb DC. Clinical characterization of patients with idiopathic chronic pancreatitis and SPINK1 Mutations. Scand J Gastroenterol. 2004;39:903–904. doi: 10.1080/00365520410006710. [DOI] [PubMed] [Google Scholar]
- 44.Talley NJ. Functional gastrointestinal disorders in 2007 and Rome III: something new, something borrowed, something objective. Rev Gastroenterol Disord. 2007;7:97–105. [PubMed] [Google Scholar]
- 45.Brugge WR, Lauwers GY, Sahani D, Fernandez-del Castillo C, Warshaw AL. Cystic neoplasms of the pancreas. N Engl J Med. 2004;351:1218–1226. doi: 10.1056/NEJMra031623. [DOI] [PubMed] [Google Scholar]
- 46.Larvin M, McMahon MJ. APACHE-II score for assessment and monitoring of acute pancreatitis. Lancet. 1989;2:201–205. doi: 10.1016/s0140-6736(89)90381-4. [DOI] [PubMed] [Google Scholar]
- 47.Dervenis C, Johnson CD, Bassi C, Bradley E, Imrie CW, McMahon MJ, Modlin I. Diagnosis, objective assessment of severity, and management of acute pancreatitis. Santorini consensus conference. Int J Pancreatol. 1999;25:195–210. doi: 10.1007/BF02925968. [DOI] [PubMed] [Google Scholar]
- 48.Uhl W, Büchler M, Malfertheiner P, Martini M, Beger HG. PMN-elastase in comparison with CRP, antiproteases, and LDH as indicators of necrosis in human acute pancreatitis. Pancreas. 1991;6:253–259. doi: 10.1097/00006676-199105000-00001. [DOI] [PubMed] [Google Scholar]
- 49.Al-Bahrani AZ, Ammori BJ. Clinical laboratory assessment of acute pancreatitis. Clin Chim Acta. 2005;362:26–48. doi: 10.1016/j.cccn.2005.06.008. [DOI] [PubMed] [Google Scholar]
- 50.Rau BM, Kemppainen EA, Gumbs AA, Büchler MW, Wegscheider K, Bassi C, Puolakkainen PA, Beger HG. Early assessment of pancreatic infections and overall prognosis in severe acute pancreatitis by procalcitonin (PCT): a prospective international multicenter study. Ann Surg. 2007;245:745–754. doi: 10.1097/01.sla.0000252443.22360.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rau BM. Predicting severity of acute pancreatitis. Curr Gastroenterol Rep. 2007;9:107–115. doi: 10.1007/s11894-007-0004-5. [DOI] [PubMed] [Google Scholar]
- 52.Ranson JH, Rifkind KM, Roses DF, Fink SD, Eng K, Spencer FC. Prognostic signs and the role of operative management in acute pancreatitis. Surg Gynecol Obstet. 1974;139:69–81. [PubMed] [Google Scholar]
- 53.Imrie CW, Benjamin IS, Ferguson JC, McKay AJ, Mackenzie I, O'Neill J, Blumgart LH. A single-centre double-blind trial of Trasylol therapy in primary acute pancreatitis. Br J Surg. 1978;65:337–341. doi: 10.1002/bjs.1800650514. [DOI] [PubMed] [Google Scholar]
- 54.Blamey SL, Imrie CW, O'Neill J, Gilmour WH, Carter DC. Prognostic factors in acute pancreatitis. Gut. 1984;25:1340–1346. doi: 10.1136/gut.25.12.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–829. [PubMed] [Google Scholar]
- 56.Wilson C, Heath DI, Imrie CW. Prediction of outcome in acute pancreatitis: a comparative study of APACHE II, clinical assessment and multiple factor scoring systems. Br J Surg. 1990;77:1260–1264. doi: 10.1002/bjs.1800771120. [DOI] [PubMed] [Google Scholar]
- 57.Martínez J, Johnson CD, Sánchez-Payá J, de Madaria E, Robles-Díaz G, Pérez-Mateo M. Obesity is a definitive risk factor of severity and mortality in acute pancreatitis: an updated meta-analysis. Pancreatology. 2006;6:206–209. doi: 10.1159/000092104. [DOI] [PubMed] [Google Scholar]
- 58.Johnson CD, Toh SK, Campbell MJ. Combination of APACHE-II score and an obesity score (APACHE-O) for the prediction of severe acute pancreatitis. Pancreatology. 2004;4:1–6. doi: 10.1159/000077021. [DOI] [PubMed] [Google Scholar]
- 59.Papachristou GI, Papachristou DJ, Avula H, Slivka A, Whitcomb DC. Obesity increases the severity of acute pancreatitis: performance of APACHE-O score and correlation with the inflammatory response. Pancreatology. 2006;6:279–285. doi: 10.1159/000092689. [DOI] [PubMed] [Google Scholar]
- 60.Mofidi R, Duff MD, Wigmore SJ, Madhavan KK, Garden OJ, Parks RW. Association between early systemic inflammatory response, severity of multiorgan dysfunction and death in acute pancreatitis. Br J Surg. 2006;93:738–744. doi: 10.1002/bjs.5290. [DOI] [PubMed] [Google Scholar]
- 61.Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter PM, Sprung CL, Colardyn F, Blecher S. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on "sepsis-related problems" of the European Society of Intensive Care Medicine. Crit Care Med. 1998;26:1793–800. doi: 10.1097/00003246-199811000-00016. [DOI] [PubMed] [Google Scholar]
- 62.Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ. Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med. 1995;23:1638–1652. doi: 10.1097/00003246-199510000-00007. [DOI] [PubMed] [Google Scholar]
- 63.Peres Bota D, Melot C, Lopes Ferreira F, Nguyen Ba V, Vincent JL. The Multiple Organ Dysfunction Score (MODS) versus the Sequential Organ Failure Assessment (SOFA) score in outcome prediction. Intensive Care Med. 2002;28:1619–1624. doi: 10.1007/s00134-002-1491-3. [DOI] [PubMed] [Google Scholar]
- 64.Balthazar EJ. Acute pancreatitis: assessment of severity with clinical and CT evaluation. Radiology. 2002;223:603–613. doi: 10.1148/radiol.2233010680. [DOI] [PubMed] [Google Scholar]
- 65.Ranson JH, Balthazar E, Caccavale R, Cooper M. Computed tomography and the prediction of pancreatic abscess in acute pancreatitis. Ann Surg. 1985;201:656–665. doi: 10.1097/00000658-198505000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Simchuk EJ, Traverso LW, Nukui Y, Kozarek RA. Computed tomography severity index is a predictor of outcomes for severe pancreatitis. Am J Surg. 2000;179:352–355. doi: 10.1016/s0002-9610(00)00375-5. [DOI] [PubMed] [Google Scholar]
- 67.Werner J, Uhl W, Hartwig W, Hackert T, Müller C, Strobel O, Büchler MW. Modern phase-specific management of acute pancreatitis. Dig Dis. 2003;21:38–45. doi: 10.1159/000071338. [DOI] [PubMed] [Google Scholar]
- 68.Kemppainen E, Sainio V, Haapiainen R, Kivisaari L, Kivilaakso E, Puolakkainen P. Early localization of necrosis by contrast-enhanced computed tomography can predict outcome in severe acute pancreatitis. Br J Surg. 1996;83:924–929. doi: 10.1002/bjs.1800830713. [DOI] [PubMed] [Google Scholar]
- 69.Uhl W, Roggo A, Kirschstein T, Anghelacopoulos SE, Gloor B, Müller CA, Malfertheiner P, Büchler MW. Influence of contrast-enhanced computed tomography on course and outcome in patients with acute pancreatitis. Pancreas. 2002;24:191–197. doi: 10.1097/00006676-200203000-00011. [DOI] [PubMed] [Google Scholar]
- 70.Vitellas KM, Paulson EK, Enns RA, Keogan MT, Pappas TN. Pancreatitis complicated by gland necrosis: evolution of findings on contrast-enhanced CT. J Comput Assist Tomogr. 1999;23:898–905. doi: 10.1097/00004728-199911000-00013. [DOI] [PubMed] [Google Scholar]
- 71.Brown A, Orav J, Banks PA. Hemoconcentration is an early marker for organ failure and necrotizing pancreatitis. Pancreas. 2000;20:367–372. doi: 10.1097/00006676-200005000-00005. [DOI] [PubMed] [Google Scholar]
- 72.Brown A, Baillargeon JD, Hughes MD, Banks PA. Can fluid resuscitation prevent pancreatic necrosis in severe acute pancreatitis? Pancreatology. 2002;2:104–107. doi: 10.1159/000055899. [DOI] [PubMed] [Google Scholar]
- 73.Thompson DR. Narcotic analgesic effects on the sphincter of Oddi: a review of the data and therapeutic implications in treating pancreatitis. Am J Gastroenterol. 2001;96:1266–1272. doi: 10.1111/j.1572-0241.2001.03536.x. [DOI] [PubMed] [Google Scholar]
- 74.Andriulli A, Leandro G, Clemente R, Festa V, Caruso N, Annese V, Lezzi G, Lichino E, Bruno F, Perri F. Meta-analysis of somatostatin, octreotide and gabexate mesilate in the therapy of acute pancreatitis. Aliment Pharmacol Ther. 1998;12:237–245. doi: 10.1046/j.1365-2036.1998.00295.x. [DOI] [PubMed] [Google Scholar]
- 75.Messori A, Rampazzo R, Scroccaro G, Olivato R, Bassi C, Falconi M, Pederzoli P, Martini N. Effectiveness of gabexate mesilate in acute pancreatitis. A metaanalysis. Dig Dis Sci. 1995;40:734–738. doi: 10.1007/BF02064970. [DOI] [PubMed] [Google Scholar]
- 76.Hughes CB, Grewal HP, Gaber LW, Kotb M, El-din AB, Mann L, Gaber AO. Anti-TNFalpha therapy improves survival and ameliorates the pathophysiologic sequelae in acute pancreatitis in the rat. Am J Surg. 1996;171:274–280. doi: 10.1016/s0002-9610(97)89568-2. [DOI] [PubMed] [Google Scholar]
- 77.Hughes CB, Gaber LW, Mohey el-Din AB, Grewal HP, Kotb M, Mann L, Gaber AO. Inhibition of TNF alpha improves survival in an experimental model of acute pancreatitis. Am Surg. 1996;62:8–13. [PubMed] [Google Scholar]
- 78.Malleo G, Mazzon E, Siriwardena AK, Cuzzocrea S. Role of tumor necrosis factor-alpha in acute pancreatitis: from biological basis to clinical evidence. Shock. 2007;28:130–140. doi: 10.1097/shk.0b013e3180487ba1. [DOI] [PubMed] [Google Scholar]
- 79.Hughes CB, el-Din AB, Kotb M, Gaber LW, Gaber AO. Calcium channel blockade inhibits release of TNF alpha and improves survival in a rat model of acute pancreatitis. Pancreas. 1996;13:22–28. doi: 10.1097/00006676-199607000-00003. [DOI] [PubMed] [Google Scholar]
- 80.Norman J, Franz M, Messina J, Riker A, Fabri PJ, Rosemurgy AS, Gower WR Jr. Interleukin-1 receptor antagonist decreases severity of experimental acute pancreatitis. Surgery. 1995;117:648–655. doi: 10.1016/s0039-6060(95)80008-5. [DOI] [PubMed] [Google Scholar]
- 81.Norman JG, Franz MG, Fink GS, Messina J, Fabri PJ, Gower WR, Carey LC. Decreased mortality of severe acute pancreatitis after proximal cytokine blockade. Ann Surg. 1995;221:625–631; discussion 631-634. doi: 10.1097/00000658-199506000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Callicutt CS, Sabek O, Fukatsu K, Lundberg AH, Gaber L, Wilcox H, Kotb M, Gaber AO. Diminished lung injury with vascular adhesion molecule-1 blockade in choline-deficient ethionine diet-induced pancreatitis. Surgery. 2003;133:186–196. doi: 10.1067/msy.2003.84. [DOI] [PubMed] [Google Scholar]
- 83.Lundberg AH, Fukatsu K, Gaber L, Callicutt S, Kotb M, Wilcox H, Kudsk K, Gaber AO. Blocking pulmonary ICAM-1 expression ameliorates lung injury in established diet-induced pancreatitis. Ann Surg. 2001;233:213–220. doi: 10.1097/00000658-200102000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Vonlaufen A, Aurrand-Lions M, Pastor CM, Lamagna C, Hadengue A, Imhof BA, Frossard JL. The role of junctional adhesion molecule C (JAM-C) in acute pancreatitis. J Pathol. 2006;209:540–548. doi: 10.1002/path.2007. [DOI] [PubMed] [Google Scholar]
- 85.Chen XL, Ciren SZ, Zhang H, Duan LG, Wesley AJ. Effect of 5-FU on modulation of disarrangement of immune-associated cytokines in experimental acute pancreatitis. World J Gastroenterol. 2009;15:2032–2037. doi: 10.3748/wjg.15.2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bradley EL 3rd. A clinically based classification system for acute pancreatitis. Summary of the International Symposium on Acute Pancreatitis, Atlanta, Ga, September 11 through 13, 1992. Arch Surg. 1993;128:586–590. doi: 10.1001/archsurg.1993.01420170122019. [DOI] [PubMed] [Google Scholar]
- 87.Stanten R, Frey CF. Comprehensive management of acute necrotizing pancreatitis and pancreatic abscess. Arch Surg. 1990;125:1269–1274; discussion 1274-1275. doi: 10.1001/archsurg.1990.01410220053008. [DOI] [PubMed] [Google Scholar]
- 88.Uhl W, Warshaw A, Imrie C, Bassi C, McKay CJ, Lankisch PG, Carter R, Di Magno E, Banks PA, Whitcomb DC, et al. IAP Guidelines for the Surgical Management of Acute Pancreatitis. Pancreatology. 2002;2:565–573. doi: 10.1159/000071269. [DOI] [PubMed] [Google Scholar]
- 89.Juvonen PO, Alhava EM, Takala JA. Gut permeability in patients with acute pancreatitis. Scand J Gastroenterol. 2000;35:1314–1318. doi: 10.1080/003655200453683. [DOI] [PubMed] [Google Scholar]
- 90.Petrov MS, van Santvoort HC, Besselink MG, van der Heijden GJ, Windsor JA, Gooszen HG. Enteral nutrition and the risk of mortality and infectious complications in patients with severe acute pancreatitis: a meta-analysis of randomized trials. Arch Surg. 2008;143:1111–1117. doi: 10.1001/archsurg.143.11.1111. [DOI] [PubMed] [Google Scholar]
- 91.Eatock FC, Chong P, Menezes N, Murray L, McKay CJ, Carter CR, Imrie CW. A randomized study of early nasogastric versus nasojejunal feeding in severe acute pancreatitis. Am J Gastroenterol. 2005;100:432–439. doi: 10.1111/j.1572-0241.2005.40587.x. [DOI] [PubMed] [Google Scholar]
- 92.Besselink MG, van Santvoort HC, Buskens E, Boermeester MA, van Goor H, Timmerman HM, Nieuwenhuijs VB, Bollen TL, van Ramshorst B, Witteman BJ, et al. Probiotic prophylaxis in predicted severe acute pancreatitis: a randomised, double-blind, placebo-controlled trial. Lancet. 2008;371:651–659. doi: 10.1016/S0140-6736(08)60207-X. [DOI] [PubMed] [Google Scholar]
- 93.Oría A, Cimmino D, Ocampo C, Silva W, Kohan G, Zandalazini H, Szelagowski C, Chiappetta L. Early endoscopic intervention versus early conservative management in patients with acute gallstone pancreatitis and biliopancreatic obstruction: a randomized clinical trial. Ann Surg. 2007;245:10–17. doi: 10.1097/01.sla.0000232539.88254.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Fölsch UR, Nitsche R, Lüdtke R, Hilgers RA, Creutzfeldt W. Early ERCP and papillotomy compared with conservative treatment for acute biliary pancreatitis. The German Study Group on Acute Biliary Pancreatitis. N Engl J Med. 1997;336:237–242. doi: 10.1056/NEJM199701233360401. [DOI] [PubMed] [Google Scholar]
- 95.Neoptolemos JP, Carr-Locke DL, London NJ, Bailey IA, James D, Fossard DP. Controlled trial of urgent endoscopic retrograde cholangiopancreatography and endoscopic sphincterotomy versus conservative treatment for acute pancreatitis due to gallstones. Lancet. 1988;2:979–983. doi: 10.1016/s0140-6736(88)90740-4. [DOI] [PubMed] [Google Scholar]
- 96.Sharma VK, Howden CW. Metaanalysis of randomized controlled trials of endoscopic retrograde cholangiography and endoscopic sphincterotomy for the treatment of acute biliary pancreatitis. Am J Gastroenterol. 1999;94:3211–3214. doi: 10.1111/j.1572-0241.1999.01520.x. [DOI] [PubMed] [Google Scholar]
- 97.Petrov MS, van Santvoort HC, Besselink MG, van der Heijden GJ, van Erpecum KJ, Gooszen HG. Early endoscopic retrograde cholangiopancreatography versus conservative management in acute biliary pancreatitis without cholangitis: a meta-analysis of randomized trials. Ann Surg. 2008;247:250–257. doi: 10.1097/SLA.0b013e31815edddd. [DOI] [PubMed] [Google Scholar]
- 98.UK guidelines for the management of acute pancreatitis. Gut. 2005;54 Suppl 3:iii1–iii9. doi: 10.1136/gut.2004.057026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Forsmark CE, Baillie J. AGA Institute technical review on acute pancreatitis. Gastroenterology. 2007;132:2022–2044. doi: 10.1053/j.gastro.2007.03.065. [DOI] [PubMed] [Google Scholar]
- 100.Taylor E, Wong C. The optimal timing of laparoscopic cholecystectomy in mild gallstone pancreatitis. Am Surg. 2004;70:971–975. [PubMed] [Google Scholar]
- 101.Heinrich S, Schäfer M, Rousson V, Clavien PA. Evidence-based treatment of acute pancreatitis: a look at established paradigms. Ann Surg. 2006;243:154–168. doi: 10.1097/01.sla.0000197334.58374.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Uhl W, Müller CA, Krähenbühl L, Schmid SW, Schölzel S, Büchler MW. Acute gallstone pancreatitis: timing of laparoscopic cholecystectomy in mild and severe disease. Surg Endosc. 1999;13:1070–1076. doi: 10.1007/s004649901175. [DOI] [PubMed] [Google Scholar]
- 103.Schachter P, Peleg T, Cohen O. Interval laparoscopic cholecystectomy in the management of acute biliary pancreatitis. HPB Surg. 2000;11:319–322; discussion 322-323. doi: 10.1155/2000/40290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Tate JJ, Lau WY, Li AK. Laparoscopic cholecystectomy for biliary pancreatitis. Br J Surg. 1994;81:720–722. doi: 10.1002/bjs.1800810533. [DOI] [PubMed] [Google Scholar]
- 105.Schietroma M, Carlei F, Lezoche E, Rossi M, Liakos CH, Mattucci S, Lygidakis NJ. Acute biliary pancreatitis: staging and management. Hepatogastroenterology. 2001;48:988–993. [PubMed] [Google Scholar]
- 106.Büchler MW, Gloor B, Müller CA, Friess H, Seiler CA, Uhl W. Acute necrotizing pancreatitis: treatment strategy according to the status of infection. Ann Surg. 2000;232:619–626. doi: 10.1097/00000658-200011000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Isenmann R, Rau B, Beger HG. Bacterial infection and extent of necrosis are determinants of organ failure in patients with acute necrotizing pancreatitis. Br J Surg. 1999;86:1020–1024. doi: 10.1046/j.1365-2168.1999.01176.x. [DOI] [PubMed] [Google Scholar]
- 108.Gerzof SG, Banks PA, Robbins AH, Johnson WC, Spechler SJ, Wetzner SM, Snider JM, Langevin RE, Jay ME. Early diagnosis of pancreatic infection by computed tomography-guided aspiration. Gastroenterology. 1987;93:1315–1320. doi: 10.1016/0016-5085(87)90261-7. [DOI] [PubMed] [Google Scholar]
- 109.Götzinger P, Wamser P, Barlan M, Sautner T, Jakesz R, Függer R. Candida infection of local necrosis in severe acute pancreatitis is associated with increased mortality. Shock. 2000;14:320–323; discussion 323-324. doi: 10.1097/00024382-200014030-00014. [DOI] [PubMed] [Google Scholar]
- 110.Rau B, Pralle U, Uhl W, Schoenberg MH, Beger HG. Management of sterile necrosis in instances of severe acute pancreatitis. J Am Coll Surg. 1995;181:279–288. [PubMed] [Google Scholar]
- 111.Wilson PG, Manji M, Neoptolemos JP. Acute pancreatitis as a model of sepsis. J Antimicrob Chemother. 1998;41 Suppl A:51–63. doi: 10.1093/jac/41.suppl_1.51. [DOI] [PubMed] [Google Scholar]
- 112.Beger HG, Rau B, Isenmann R, Schwarz M, Gansauge F, Poch B. Antibiotic prophylaxis in severe acute pancreatitis. Pancreatology. 2005;5:10–19. doi: 10.1159/000084485. [DOI] [PubMed] [Google Scholar]
- 113.Hoerauf A, Hammer S, Müller-Myhsok B, Rupprecht H. Intra-abdominal Candida infection during acute necrotizing pancreatitis has a high prevalence and is associated with increased mortality. Crit Care Med. 1998;26:2010–2015. doi: 10.1097/00003246-199812000-00031. [DOI] [PubMed] [Google Scholar]
- 114.Isenmann R, Schwarz M, Rau B, Trautmann M, Schober W, Beger HG. Characteristics of infection with Candida species in patients with necrotizing pancreatitis. World J Surg. 2002;26:372–376. doi: 10.1007/s00268-001-0146-9. [DOI] [PubMed] [Google Scholar]
- 115.Gloor B, Müller CA, Worni M, Stahel PF, Redaelli C, Uhl W, Büchler MW. Pancreatic infection in severe pancreatitis: the role of fungus and multiresistant organisms. Arch Surg. 2001;136:592–596. doi: 10.1001/archsurg.136.5.592. [DOI] [PubMed] [Google Scholar]
- 116.Grewe M, Tsiotos GG, Luque de-Leon E, Sarr MG. Fungal infection in acute necrotizing pancreatitis. J Am Coll Surg. 1999;188:408–414. doi: 10.1016/s1072-7515(98)00334-2. [DOI] [PubMed] [Google Scholar]
- 117.Bradley EL 3rd, Allen K. A prospective longitudinal study of observation versus surgical intervention in the management of necrotizing pancreatitis. Am J Surg. 1991;161:19–24; discussion 24-25. doi: 10.1016/0002-9610(91)90355-h. [DOI] [PubMed] [Google Scholar]
- 118.Pederzoli P, Bassi C, Vesentini S, Campedelli A. A randomized multicenter clinical trial of antibiotic prophylaxis of septic complications in acute necrotizing pancreatitis with imipenem. Surg Gynecol Obstet. 1993;176:480–483. [PubMed] [Google Scholar]
- 119.Sainio V, Kemppainen E, Puolakkainen P, Taavitsainen M, Kivisaari L, Valtonen V, Haapiainen R, Schröder T, Kivilaakso E. Early antibiotic treatment in acute necrotising pancreatitis. Lancet. 1995;346:663–667. doi: 10.1016/s0140-6736(95)92280-6. [DOI] [PubMed] [Google Scholar]
- 120.Nordback I, Sand J, Saaristo R, Paajanen H. Early treatment with antibiotics reduces the need for surgery in acute necrotizing pancreatitis--a single-center randomized study. J Gastrointest Surg. 2001;5:113–118; discussion 118-120. doi: 10.1016/s1091-255x(01)80021-4. [DOI] [PubMed] [Google Scholar]
- 121.Schwarz M, Isenmann R, Meyer H, Beger HG. [Antibiotic use in necrotizing pancreatitis. Results of a controlled study] Dtsch Med Wochenschr. 1997;122:356–361. doi: 10.1055/s-2008-1047621. [DOI] [PubMed] [Google Scholar]
- 122.Isenmann R, Rünzi M, Kron M, Kahl S, Kraus D, Jung N, Maier L, Malfertheiner P, Goebell H, Beger HG. Prophylactic antibiotic treatment in patients with predicted severe acute pancreatitis: a placebo-controlled, double-blind trial. Gastroenterology. 2004;126:997–1004. doi: 10.1053/j.gastro.2003.12.050. [DOI] [PubMed] [Google Scholar]
- 123.Dellinger EP, Tellado JM, Soto NE, Ashley SW, Barie PS, Dugernier T, Imrie CW, Johnson CD, Knaebel HP, Laterre PF, et al. Early antibiotic treatment for severe acute necrotizing pancreatitis: a randomized, double-blind, placebo-controlled study. Ann Surg. 2007;245:674–683. doi: 10.1097/01.sla.0000250414.09255.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Villatoro E, Bassi C, Larvin M. Antibiotic therapy for prophylaxis against infection of pancreatic necrosis in acute pancreatitis. Cochrane Database Syst Rev. 2006;245:CD002941. doi: 10.1002/14651858.CD002941.pub2. [DOI] [PubMed] [Google Scholar]
- 125.Gloor B, Uhl W, Büchler MW. Changing concepts in the surgical management of acute pancreatitis. Baillieres Best Pract Res Clin Gastroenterol. 1999;13:303–315. doi: 10.1053/bega.1999.0026. [DOI] [PubMed] [Google Scholar]
- 126.Kivilaakso E, Fräki O, Nikki P, Lempinen M. Resection of the pancreas for acute fulminant pancreatitis. Surg Gynecol Obstet. 1981;152:493–498. [PubMed] [Google Scholar]
- 127.Fernández-Cruz L, Navarro S, Valderrama R, Sáenz A, Guarner L, Aparisi L, Espi A, Jaurietta E, Marruecos L, Gener J. Acute necrotizing pancreatitis: a multicenter study. Hepatogastroenterology. 1994;41:185–189. [PubMed] [Google Scholar]
- 128.Mier J, León EL, Castillo A, Robledo F, Blanco R. Early versus late necrosectomy in severe necrotizing pancreatitis. Am J Surg. 1997;173:71–75. doi: 10.1016/S0002-9610(96)00425-4. [DOI] [PubMed] [Google Scholar]
- 129.Hartwig W, Werner J, Müller CA, Uhl W, Büchler MW. Surgical management of severe pancreatitis including sterile necrosis. J Hepatobiliary Pancreat Surg. 2002;9:429–435. doi: 10.1007/s005340200053. [DOI] [PubMed] [Google Scholar]
- 130.De Waele JJ, Blot SI, Vogelaers D, Colardyn F. High infection rates in patients with severe acute necrotizing pancreatitis. Intensive Care Med. 2004;30:1248. doi: 10.1007/s00134-004-2232-6. [DOI] [PubMed] [Google Scholar]
- 131.De Waele JJ, Vogelaers D, Blot S, Colardyn F. Fungal infections in patients with severe acute pancreatitis and the use of prophylactic therapy. Clin Infect Dis. 2003;37:208–213. doi: 10.1086/375603. [DOI] [PubMed] [Google Scholar]
- 132.Besselink MG, Verwer TJ, Schoenmaeckers EJ, Buskens E, Ridwan BU, Visser MR, Nieuwenhuijs VB, Gooszen HG. Timing of surgical intervention in necrotizing pancreatitis. Arch Surg. 2007;142:1194–1201. doi: 10.1001/archsurg.142.12.1194. [DOI] [PubMed] [Google Scholar]
- 133.Freeny PC, Hauptmann E, Althaus SJ, Traverso LW, Sinanan M. Percutaneous CT-guided catheter drainage of infected acute necrotizing pancreatitis: techniques and results. AJR Am J Roentgenol. 1998;170:969–975. doi: 10.2214/ajr.170.4.9530046. [DOI] [PubMed] [Google Scholar]
- 134.Gouzi JL, Bloom E, Julio C, Labbé F, Sans N, el Rassi Z, Carrère N, Pradère B. [Percutaneous drainage of infected pancreatic necrosis: an alternative to surgery] Chirurgie. 1999;124:31–37. doi: 10.1016/s0001-4001(99)80039-7. [DOI] [PubMed] [Google Scholar]
- 135.Echenique AM, Sleeman D, Yrizarry J, Scagnelli T, Guerra JJ Jr, Casillas VJ, Huson H, Russell E. Percutaneous catheter-directed debridement of infected pancreatic necrosis: results in 20 patients. J Vasc Interv Radiol. 1998;9:565–571. doi: 10.1016/s1051-0443(98)70323-9. [DOI] [PubMed] [Google Scholar]
- 136.Segal D, Mortele KJ, Banks PA, Silverman SG. Acute necrotizing pancreatitis: role of CT-guided percutaneous catheter drainage. Abdom Imaging. 2007;32:351–361. doi: 10.1007/s00261-007-9221-5. [DOI] [PubMed] [Google Scholar]
- 137.Ferrucci JT 3rd, Mueller PR. Interventional approach to pancreatic fluid collections. Radiol Clin North Am. 2003;41:1217–1226, vii. doi: 10.1016/s0033-8389(03)00123-4. [DOI] [PubMed] [Google Scholar]
- 138.Charnley RM, Lochan R, Gray H, O'Sullivan CB, Scott J, Oppong KE. Endoscopic necrosectomy as primary therapy in the management of infected pancreatic necrosis. Endoscopy. 2006;38:925–928. doi: 10.1055/s-2006-944731. [DOI] [PubMed] [Google Scholar]
- 139.Mathew A, Biswas A, Meitz KP. Endoscopic necrosectomy as primary treatment for infected peripancreatic fluid collections (with video) Gastrointest Endosc. 2008;68:776–782. doi: 10.1016/j.gie.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 140.Schrover IM, Weusten BL, Besselink MG, Bollen TL, van Ramshorst B, Timmer R. EUS-guided endoscopic transgastric necrosectomy in patients with infected necrosis in acute pancreatitis. Pancreatology. 2008;8:271–276. doi: 10.1159/000134275. [DOI] [PubMed] [Google Scholar]
- 141.Bradley EL 3rd, Howard TJ, van Sonnenberg E, Fotoohi M. Intervention in necrotizing pancreatitis: an evidence-based review of surgical and percutaneous alternatives. J Gastrointest Surg. 2008;12:634–639. doi: 10.1007/s11605-007-0445-z. [DOI] [PubMed] [Google Scholar]
- 142.Werner J, Hartwig W, Hackert T, Büchler MW. Surgery in the treatment of acute pancreatitis--open pancreatic necrosectomy. Scand J Surg. 2005;94:130–134. doi: 10.1177/145749690509400209. [DOI] [PubMed] [Google Scholar]
- 143.Pemberton JH, Nagorney DM, Becker JM, Ilstrup D, Dozois RR, Remine WH. Controlled open lesser sac drainage for pancreatic abscess. Ann Surg. 1986;203:600–604. doi: 10.1097/00000658-198606000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Orlando R 3rd, Welch JP, Akbari CM, Bloom GP, Macaulay WP. Techniques and complications of open packing of infected pancreatic necrosis. Surg Gynecol Obstet. 1993;177:65–71. [PubMed] [Google Scholar]
- 145.Bradley EL 3rd. A fifteen year experience with open drainage for infected pancreatic necrosis. Surg Gynecol Obstet. 1993;177:215–222. [PubMed] [Google Scholar]
- 146.Branum G, Galloway J, Hirchowitz W, Fendley M, Hunter J. Pancreatic necrosis: results of necrosectomy, packing, and ultimate closure over drains. Ann Surg. 1998;227:870–877. doi: 10.1097/00000658-199806000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Bosscha K, Hulstaert PF, Hennipman A, Visser MR, Gooszen HG, van Vroonhoven TJ, v d Werken C. Fulminant acute pancreatitis and infected necrosis: results of open management of the abdomen and "planned" reoperations. J Am Coll Surg. 1998;187:255–262. doi: 10.1016/s1072-7515(98)00153-7. [DOI] [PubMed] [Google Scholar]
- 148.Nieuwenhuijs VB, Besselink MG, van Minnen LP, Gooszen HG. Surgical management of acute necrotizing pancreatitis: a 13-year experience and a systematic review. Scand J Gastroenterol Suppl. 2003;187:111–116. doi: 10.1080/00855920310002799. [DOI] [PubMed] [Google Scholar]
- 149.Nordback I, Paajanen H, Sand J. Prospective evaluation of a treatment protocol in patients with severe acute necrotising pancreatitis. Eur J Surg. 1997;163:357–364. [PubMed] [Google Scholar]
- 150.Garcia-Sabrido JL, Tallado JM, Christou NV, Polo JR, Valdecantos E. Treatment of severe intra-abdominal sepsis and/or necrotic foci by an 'open-abdomen' approach. Zipper and zipper-mesh techniques. Arch Surg. 1988;123:152–156. doi: 10.1001/archsurg.1988.01400260032002. [DOI] [PubMed] [Google Scholar]
- 151.van Goor H, Sluiter WJ, Bleichrodt RP. Early and long term results of necrosectomy and planned re-exploration for infected pancreatic necrosis. Eur J Surg. 1997;163:611–618. [PubMed] [Google Scholar]
- 152.Sarr MG, Nagorney DM, Mucha P Jr, Farnell MB, Johnson CD. Acute necrotizing pancreatitis: management by planned, staged pancreatic necrosectomy/debridement and delayed primary wound closure over drains. Br J Surg. 1991;78:576–581. doi: 10.1002/bjs.1800780518. [DOI] [PubMed] [Google Scholar]
- 153.Tsiotos GG, Luque-de León E, Sarr MG. Long-term outcome of necrotizing pancreatitis treated by necrosectomy. Br J Surg. 1998;85:1650–1653. doi: 10.1046/j.1365-2168.1998.00950.x. [DOI] [PubMed] [Google Scholar]
- 154.Nicholson ML, Mortensen NJ, Espiner HJ. Pancreatic abscess: results of prolonged irrigation of the pancreatic bed after surgery. Br J Surg. 1988;75:89–91. doi: 10.1002/bjs.1800750131. [DOI] [PubMed] [Google Scholar]
- 155.Larvin M, Chalmers AG, Robinson PJ, McMahon MJ. Debridement and closed cavity irrigation for the treatment of pancreatic necrosis. Br J Surg. 1989;76:465–471. doi: 10.1002/bjs.1800760513. [DOI] [PubMed] [Google Scholar]
- 156.Pederzoli P, Bassi C, Vesentini S, Girelli R, Cavallini G, Falconi M, Nifosi F, Riela A, Dagradi A. Retroperitoneal and peritoneal drainage and lavage in the treatment of severe necrotizing pancreatitis. Surg Gynecol Obstet. 1990;170:197–203. [PubMed] [Google Scholar]
- 157.Beger HG, Büchler M, Bittner R, Block S, Nevalainen T, Roscher R. Necrosectomy and postoperative local lavage in necrotizing pancreatitis. Br J Surg. 1988;75:207–212. doi: 10.1002/bjs.1800750306. [DOI] [PubMed] [Google Scholar]
- 158.Farkas G, Márton J, Mándi Y, Leindler L. Surgical management and complex treatment of infected pancreatic necrosis: 18-year experience at a single center. J Gastrointest Surg. 2006;10:278–285. doi: 10.1016/j.gassur.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 159.Rau B, Bothe A, Beger HG. Surgical treatment of necrotizing pancreatitis by necrosectomy and closed lavage: changing patient characteristics and outcome in a 19-year, single-center series. Surgery. 2005;138:28–39. doi: 10.1016/j.surg.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 160.Besselink MG, de Bruijn MT, Rutten JP, Boermeester MA, Hofker HS, Gooszen HG. Surgical intervention in patients with necrotizing pancreatitis. Br J Surg. 2006;93:593–599. doi: 10.1002/bjs.5287. [DOI] [PubMed] [Google Scholar]
- 161.Wig JD, Mettu SR, Jindal R, Gupta R, Yadav TD. Closed lesser sac lavage in the management of pancreatic necrosis. J Gastroenterol Hepatol. 2004;19:1010–1015. doi: 10.1111/j.1440-1746.2004.03434.x. [DOI] [PubMed] [Google Scholar]
- 162.Fernández-del Castillo C, Rattner DW, Makary MA, Mostafavi A, McGrath D, Warshaw AL. Débridement and closed packing for the treatment of necrotizing pancreatitis. Ann Surg. 1998;228:676–684. doi: 10.1097/00000658-199811000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Carter CR, McKay CJ, Imrie CW. Percutaneous necrosectomy and sinus tract endoscopy in the management of infected pancreatic necrosis: an initial experience. Ann Surg. 2000;232:175–180. doi: 10.1097/00000658-200008000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Alverdy J, Vargish T, Desai T, Frawley B, Rosen B. Laparoscopic intracavitary debridement of peripancreatic necrosis: preliminary report and description of the technique. Surgery. 2000;127:112–114. doi: 10.1067/msy.2000.102604. [DOI] [PubMed] [Google Scholar]
- 165.Horvath KD, Kao LS, Ali A, Wherry KL, Pellegrini CA, Sinanan MN. Laparoscopic assisted percutaneous drainage of infected pancreatic necrosis. Surg Endosc. 2001;15:677–682. doi: 10.1007/s004640080010. [DOI] [PubMed] [Google Scholar]
- 166.Connor S, Ghaneh P, Raraty M, Sutton R, Rosso E, Garvey CJ, Hughes ML, Evans JC, Rowlands P, Neoptolemos JP. Minimally invasive retroperitoneal pancreatic necrosectomy. Dig Surg. 2003;20:270–277. doi: 10.1159/000071184. [DOI] [PubMed] [Google Scholar]
- 167.Risse O, Auguste T, Delannoy P, Cardin N, Bricault I, Létoublon C. Percutaneous video-assisted necrosectomy for infected pancreatic necrosis. Gastroenterol Clin Biol. 2004;28:868–871. doi: 10.1016/s0399-8320(04)95150-0. [DOI] [PubMed] [Google Scholar]
- 168.Cheung MT, Ho CN, Siu KW, Kwok PC. Percutaneous drainage and necrosectomy in the management of pancreatic necrosis. ANZ J Surg. 2005;75:204–207. doi: 10.1111/j.1445-2197.2005.03366.x. [DOI] [PubMed] [Google Scholar]
- 169.Haan JM, Scalea TM. Laparoscopic debridement of recurrent pancreatic abscesses in the hostile abdomen. Am Surg. 2006;72:511–514. [PubMed] [Google Scholar]
- 170.Bucher P, Pugin F, Morel P. Minimally invasive necrosectomy for infected necrotizing pancreatitis. Pancreas. 2008;36:113–119. doi: 10.1097/MPA.0b013e3181514c9e. [DOI] [PubMed] [Google Scholar]
- 171.Cuschieri A. Pancreatic necrosis: pathogenesis and endoscopic management. Semin Laparosc Surg. 2002;9:54–63. [PubMed] [Google Scholar]
- 172.Ammori BJ. Laparoscopic transgastric pancreatic necrosectomy for infected pancreatic necrosis. Surg Endosc. 2002;16:1362. doi: 10.1007/s00464-002-4202-9. [DOI] [PubMed] [Google Scholar]
- 173.Zhou ZG, Zheng YC, Shu Y, Hu WM, Tian BL, Li QS, Zhang ZD. Laparoscopic management of severe acute pancreatitis. Pancreas. 2003;27:e46–e50. doi: 10.1097/00006676-200310000-00019. [DOI] [PubMed] [Google Scholar]
- 174.Parekh D. Laparoscopic-assisted pancreatic necrosectomy: A new surgical option for treatment of severe necrotizing pancreatitis. Arch Surg. 2006;141:895–902; discussion 902-903. doi: 10.1001/archsurg.141.9.895. [DOI] [PubMed] [Google Scholar]
- 175.Adamson GD, Cuschieri A. Multimedia article. Laparoscopic infracolic necrosectomy for infected pancreatic necrosis. Surg Endosc. 2003;17:1675. doi: 10.1007/s00464-003-0041-6. [DOI] [PubMed] [Google Scholar]
- 176.Lau ST, Simchuk EJ, Kozarek RA, Traverso LW. A pancreatic ductal leak should be sought to direct treatment in patients with acute pancreatitis. Am J Surg. 2001;181:411–415. doi: 10.1016/s0002-9610(01)00606-7. [DOI] [PubMed] [Google Scholar]
- 177.Haney JC, Pappas TN. Necrotizing pancreatitis: diagnosis and management. Surg Clin North Am. 2007;87:1431–1446, ix. doi: 10.1016/j.suc.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 178.Besselink MG, van Santvoort HC, Nieuwenhuijs VB, Boermeester MA, Bollen TL, Buskens E, Dejong CH, van Eijck CH, van Goor H, Hofker SS, et al. Minimally invasive 'step-up approach' versus maximal necrosectomy in patients with acute necrotising pancreatitis (PANTER trial): design and rationale of a randomised controlled multicenter trial [ISRCTN13975868] BMC Surg. 2006;6:6. doi: 10.1186/1471-2482-6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]