Abstract
Low adherence to antihypertensive medication remains a public health challenge. Understanding barriers to, and determinants of, adherence to antihypertensive medication adherence may help identify interventions to increase adherence and improve outcomes. The Cohort Study of Medication Adherence in Older Adults (CoSMO) is designed to assess risk factors for low antihypertensive medication adherence, explore differences across age, gender, and race subgroups, and determine the relationship of adherence with blood pressure (BP) control and cardiovascular outcomes over time. Between August 2006 and September 2007, 2194 participants, age 65 years and older, taking antihypertensive medication were recruited and enrolled in CoSMO and completed a baseline telephone survey. Antihypertensive medication adherence was assessed with the Morisky Medication Adherence Scale (MMAS) and the medication possession ratio (MPR). Low adherence was defined as a MMAS score < 6; non-persistent MPR was defined as <0.80. BP data were abstracted from outpatient electronic medical records; uncontrolled BP was defined as systolic or diastolic BP ≥140 or 90 mmHg, respectively.
The mean age of participants was 75.0 ± 5.6 years, 58.8% were women, 30.7% were black, and 83.6% were taking 2 or more classes of antihypertensive medication. Overall, 14.1% of participants had low adherence, 27.0% had a non-persistent MPR, and 33.7% had uncontrolled BP. Participants with low MMAS were 2.71 (95% confidence interval (CI) 2.31-3.18) times more likely to have non-persistent MPR and 1.20 (95% CI 1.00-1.43) times more likely to have uncontrolled BP than participants with high MMAS. Low antihypertensive medication adherence and uncontrolled blood pressure are common in older, insured patients. Research identifying barriers to achieving antihypertensive medication adherence may assist in developing tailored interventions to increase medication adherence and improve outcomes.
Keywords: medication adherence, hypertension, Morisky Scale, cohort, older adults, blood pressure control
Introduction
Although there has been recent progress in the prevention, detection and treatment of hypertension, it persists as a major public health challenge affecting approximately one billion persons worldwide and about 70 million people in the United States(1-3). Hypertension is a significant and often asymptomatic chronic disease, which requires persistent adherence to prescribed medication to reduce the risks of stroke, cardiovascular disease and renal disease (4). Effective medical therapy and evidence-based treatment guidelines for hypertension are readily available; yet, hypertension management at the population level is not optimal (5). For example, over 36% of US adults treated for hypertension have uncontrolled blood pressure (3). Low patient adherence to antihypertensive medication is the most significant modifiable patient-related barrier to achieving controlled blood pressure (6).
Barriers to medication adherence are multi-factorial and include complex medication regimens, convenience factors (e.g. dosing frequency), behavioral factors and issues with treatment of asymptomatic diseases (e.g. treatment side effects) (7). There is a lack of understanding of which patient groups are at greatest risk of low adherence, how barriers to medication-taking behavior influence low adherence, and what interventions are most effective in overcoming barriers and improving adherence rates in different patient populations.
The Cohort Study of Medication Adherence in Older Adults (CoSMO), a prospective study among older adults with essential hypertension who are enrolled in a single managed care organization, is designed to investigate barriers to, and determinants of, antihypertensive medication adherence and lay the groundwork for interventions to improve adherence and clinical outcomes. The specific aims of CosMO are (a) to assess the effect of psychosocial, behavioral, quality of life, and clinical factors on changes in medication adherence over two years of follow-up; (b) to assess health care system barriers, uses of prescribed and over-the-counter medications, complementary/alternative therapies and lifestyle modification on medication adherence and change in adherence; and (c) to determine the relationship of medication adherence with future medical and psychosocial outcomes including blood pressure control, cardiovascular disease incidence, all-cause mortality, quality of life, and healthcare utilization.
The purpose of this paper is to describe the design and methods of CoSMO and to present baseline demographic characteristics as well as levels of medication adherence and blood pressure control for the overall study population and for demographic subgroups. The associations of self-reported medication adherence to pharmacy fill adherence and blood pressure control in older insured adults, which have not been well documented previously, are presented. A framework for understanding the barriers for adherence to antihypertensive medications is reviewed.
Collection of data to understand barriers to antihypertensive medication adherence
A sample size of 2000 participants was selected to provide adequate statistical power to detect clinically important and meaningful differences between persons with and without low adherence to their antihypertensive medication. CoSMO has 80% power to detect prevalence ratios of low medication adherence as low as 1.2 for cross-sectional analyses and as low as 1.4 for longitudinal analyses of reductions in medication adherence depending on the prevalence of low medication adherence, the percent of the population reducing adherence, and the prevalence of the exposure or barrier being studied.
The catchment area for CoSMO reflects a demographically diverse group of individuals in urban and suburban areas. Recruitment was conducted from August 21, 2006 to September 30, 2007. Participants, 65 years and older with essential hypertension, were randomly selected from the roster of a large managed care organization in southeastern Louisiana. An introductory letter with a reply card including an opt-out option was mailed to potentially eligible participants based on the review of administrative criteria from the managed care organization (MCO) database (N=7020). Administrative criteria from the MCO's database used to initially assess eligibility included:
Men and women aged 65 years of age or older enrolled in the Medicare Risk product
At least one encounter in calendar year 2005 with a primary or secondary diagnosis of essential hypertension (ICD-9 code 401) in the outpatient administrative database
At least one antihypertensive medication prescription filled in calendar year 2005
Continuously enrolled in the MCO for at least 2 years at the time of the baseline survey
No ICD-9 diagnosis (ICD-9 codes 290, 291-294,317-319, 331) of cognitive impairment
No ICD-9 diagnosis of malignancy or human immunodeficiency virus (ICD-9 codes 140-172.9, 174-195.8, 200-208.99, 042-044.9)
For those not opting out and with valid contact information, eligibility was confirmed using a brief telephone questionnaire. Eligibility criteria confirmed with each participant included:
English speaking
Community dwelling
Current diagnosis of and prescribed medication for hypertension
Current enrollment in the MCO
No cognitive impairment via a cognitive function screener (8)
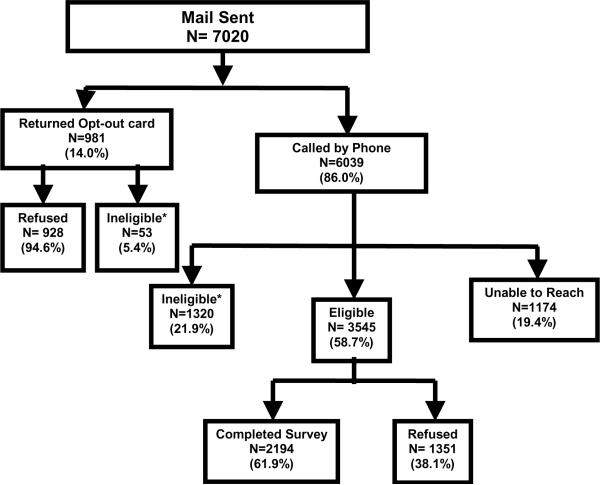
There were 1373 individuals deemed ineligible for the study and 2279 individuals refused to participate (Figure 1). We were unable to reach 1174 individuals due to invalid contact information likely resulting from displacement following Hurricane Katrina. A total of 2194 participants enrolled in the study. Those who refused compared to those who participated in the survey were more likely to be male (50.4% versus 41.5%, respectively; p<0.001), white (84.5% versus 68.8%, respectively; p<0.001), and older (76.3 years versus 74.5 years, respectively; p<0.001). Those who we were unable to reach compared to their counterparts who participated in the study were more likely to be male (45.1% versus 41.5%, respectively; p=0.043), white (77.5% versus 68.8%, respectively; p<0.001), and older (75.2 years versus 74.5 years, respectively; p=0.001).
Figure 1. Recruitment Flowchart for the Cohort Study of Medication Adherence among Older Adults (CoSMO).
*Reason for ineligibility were as follows: no confirmed diagnosis of hypertension (22.9%), hard of hearing (16.4%), too ill to complete survey (12.6%), deceased (11.5%), cognitive screen failure (11.1%), not currently prescribed antihypertensive medication (8.4%), no longer using Humana insurance (6.9%), non-English speaker (5.8%), confined to a nursing home (1.9%), moved out of state (1.1%), current treatment for cancer (1%), or miscellaneous reason (<1%).
All participants provided verbal informed consent, and CoSMO was approved by the Ochsner Clinic Foundation Institutional Review Board and the privacy committee of the MCO. Participants completed a survey at baseline and will be followed longitudinally and re-surveyed both one year and two years following their baseline interview to assess changes in adherence, barriers, risk factors and outcomes.
Study measures were collected through participant surveys, clinic and hospital electronic medical records (EMR), and the MCO's administrative databases. The baseline survey was administered by telephone using trained interviewers and lasted 30-45 minutes. A complete outline of the study measurements is provided in Table 1. Of relevance to the current analyses, the participant survey included assessment of socio-demographic factors, medication adherence, and clinical variables. In addition, information regarding co-morbid conditions and medication complexity was downloaded from the administrative databases of the MCO. Blood pressure data were abstracted from the outpatient EMR. These domains are described in detail below.
Table 1.
Study Measurements for the Cohort Study of Medication Adherence among Older Adults (CoSMO)
| Variable Domain | Study Measurements | Source |
|---|---|---|
| Risk Factors | ||
| Socio-demographics | • Age, gender, race, education, marital status, dependents, social support (56), knowledge of hypertension (57) | • Survey |
| Clinical | • Duration of hypertension, body mass index | • Survey |
| • Severity of hypertension-JNC 7(1), cholesterol | • Medical record | |
| • Co-morbidities (16;17) | • Administrative data | |
| Behavioral | • Smoking status, alcohol use, sexual function (58), depression -CES-D (59-62), coping (63), stress (64) | • Survey |
| Medication complexity, source and self-efficacy | • Antihypertensive medication, dose, frequency, and drug class; hypertensive medication change over prior year | • Survey |
| • Medication source, pill-splitting practices, medication-taking self efficacy (20) | • Pharmacy utilization data | |
| Self-management | • Provider blood pressure checks, lifestyle modifications -NHANES (65), complementary/alternative therapy use (66), home blood pressure monitoring | • Survey |
| Health care system issues | • Perception of primary care provider, satisfaction with access to care and communication (67-70) | • Survey |
| • Number of visits to healthcare provider in past year, co-payment, pharmacy benefit package | • Survey and administrative data | |
| Life events | • Life experiences in the last 12 months-Holmes-Rahe scale (71) | • Survey |
| Hurricane Katrina | • Damage to residence (72), hurricane coping self-efficacy (73), post-traumatic stress disorder (74;75), primary cause of stress before and after the disaster, distance from and visits with family and friends (76) | • Survey |
| Adherence | ||
| Medication adherence | • Self-report adherence -Morisky Medication Adherence Scale (10) | • Survey |
| • Pharmacy fill (11) | • Pharmacy utilization data | |
| Outcomes | ||
| Blood pressure control | • Systolic blood pressure (mmHg); diastolic blood pressure (mmHg) | • Medical record |
| Quality of life | • MOS-36- 8 scales (56;77-80) | • Survey |
| Cardiovascular events | • Heart failure, myocardial infarction, end-stage renal disease, stroke, transient ischemic attack, atrial fibrillation, peripheral vascular disease | • Administrative data, medical record, and survey |
| Mortality | • All-cause and disease-specific mortality | • National Death Index37 |
| Healthcare utilization | • Emergency department, in-patient, out-patient, home health, rehabilitation, pharmacy and laboratory encounters | • Administrative data |
MOS-Medical Outcomes Study, MOS-36 - Medical Outcomes Study Short form -36, CES-D- Center for Epidemiologic Studies-Depression Scale,, JNC 7-Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure-7th report, NHANES - National Health and Nutrition Examination Survey,
Socio-demographics
Participant age, gender, race, level of education, marital status and number of dependents were obtained through the telephone survey. If self-reported race was missing (n=37), it was determined using data in the participants' medical records (9). The socio-demographic factors were categorized as follows: age: < 75 years of age and ≥ 75 years of age; race: white and black; education: high school graduate and not a high school graduate; marital status: married and not married; and dependents: one or more and none.
Medication Adherence
Self-reported medication adherence was measured with the eight-item Morisky Medication Adherence Scale (MMAS) (10). This adherence measure was designed to facilitate the identification of barriers to and behaviors associated with adequate adherence to chronic medications. In a previous study, the scale has been determined to be reliable (α= 0.83) and significantly associated with blood pressure control (p<0.05) in low income, mostly minority and underserved individuals with hypertension (i.e. low adherence levels were associated with lower rates of blood pressure control) (10). Also, the MMAS has been shown to have high concordance with antihypertensive medication pharmacy fill rates in a managed care population similar to the current study population (11). MMAS scores can range from zero to eight with low adherence defined as MMAS scores <6; medium adherence as scores of 6 to <8, and high adherence scores as a score of 8 (10).
Pharmacy fill data were extracted for the year prior to completion of the baseline survey and included a listing of all antihypertensive prescriptions filled, date filled, drug class, and number of pills dispensed. Medication possession ratio (MPR) is the sum of the days' supply obtained between the first pharmacy fill and the last fill, with the supply obtained in the last fill excluded, divided by the total number of days in this time period (11). Provided each participant had at least 3 pharmacy fills in a drug class in the time period, MPR was calculated for each antihypertensive medication class and averaged across all classes to assign a single MPR to each participant. Pharmacy fill non-persistency was defined as an MPR <0.8 (11-15). There were 2087 participants who had at least 3 pharmacy fills used to calculate MPR.
Other Risk Factors
Duration of hypertension was assessed through self-report. Cholesterol tests and values were obtained from the EMR. Using ICD-9 codes recorded in the MCO's administrative database in the year prior to each survey, a weighted co-morbidity score was generated using the Charlson co-morbidity index (16;17). Body mass index (BMI) was calculated from self-reported height and weight. The number and classes of antihypertensive medications were downloaded from the managed care pharmacy database.
Blood Pressure
Using standard data collection forms and trained record abstractors, blood pressure levels (including systolic and diastolic values, patient position, and date of blood pressure measurement) were abstracted from the primary care clinics' EMR for the year preceding the survey. The mean blood pressure was calculated for the seated measurements on 2 different dates closest to the survey date. Using established guidelines (1), uncontrolled blood pressure was defined as systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg. Blood pressure data were available for 1908 participants.
All study staff successfully completed a training program in human subjects' protection, data collection strategies, and on the study protocol. Additional training sessions for the telephone surveyors provided instructions on computer-assisted administration and data entry of the study questionnaire. Baseline surveys were recorded using Versadial technology (VS Logger, version 3.0 release, 2008, Irvine, CA), and data were entered into a Microsoft Access database. A ten percent random sample of recorded surveys was selected for audit and quality check; any discrepancies or illogical values identified were reviewed by the investigative team.
Characteristics of the study population were calculated, overall and by age group (<75 and ≥ 75 years of age), gender and race. Data analyses were limited to black and white participants; 14 participants reporting another race were excluded from the current analyses. Significance in the differences in demographics, clinical factors, uncontrolled blood pressure, and low adherence across age group, gender, and race were determined using t-tests and chi-square tests. Log binomial regression models that included adjustment for age, gender, and race were used to determine the prevalence ratio of antihypertensive medication nonpersistency by MPR and uncontrolled blood pressure associated with low and medium adherence by MMAS using those with high adherence as the reference group. Analyses were performed using SAS 9.1 (Cary, NC).
New findings regarding antihypertensive medication adherence in older adults
Baseline characteristics of the CoSMO participants are presented in Table 2. Those younger than 75 years, compared to those 75 years and older, were more likely to be black, a high school graduate, married, have at least one dependent, a lower comorbidity score, and a higher BMI. Women enrolled in the study, compared to men, were significantly older, less likely to be married, less likely to have hypertension for more than 10 years, and have higher cholesterol levels and a lower comorbidity score. Blacks, compared to whites, were significantly younger; less likely to be a high school graduate and married, more likely to have a hypertension diagnosis longer than 10 years and have filled two or more antihypertensive medications in the prior year, and have a higher comorbidity score, higher cholesterol levels, and a higher BMI.
Table 2.
Socio-demographics, other risk factors, medication adherence, and blood pressure levels for the Cohort Study of medication Adherence among Older Adults (CoSMO)
| Overall£ (N=2180) | Age | Gender | Race | ||||
|---|---|---|---|---|---|---|---|
| <75 yrs (N=1111) | ≥75 yrs (N=1069) | Men (N=905) | Women (N=1275) | White (N=1510) | Black (N=670) | ||
| Socio-demographics | |||||||
| Age, years; mean (SD) | 75.0 (5.6) | 70.6 (2.6) | 79.7 (3.7)** | 74.7 (5.4) | 75.3 (5.6)* | 75.4 (5.7) | 74.3 (5.2)** |
| Female gender, % | 58.8 | 57.0 | 60.1 | 0 | 100 | 53.0 | 70.9** |
| Black race, % | 30.7 | 34.4 | 26.9** | 21.6 | 37.3** | 0 | 100 |
| High school graduate, % | 79.3 | 82.7 | 75.7** | 81.0 | 78.0 | 86.6 | 62.8** |
| Married, % | 56.7 | 66.1 | 47.1** | 77.1 | 42.3** | 61.4 | 46.3** |
| At least one or more dependents, % | 40.5 | 45.8 | 34.9** | 53.0 | 31.5** | 42.0 | 36.9* |
| Other Risk Factors | |||||||
| Cigarette smoking, % | 5.6 | 7.0 | 4.0** | 6.2 | 5.1 | 5.4 | 5.8 |
| Hypertension duration > 10 years, % | 62.8 | 62.4 | 63.3 | 65.3 | 61.0* | 60.9 | 67.0** |
| Co-morbid index score ≥2, % | 49.6 | 45.8 | 53.6** | 56.3 | 44.8** | 48.1 | 52.9* |
| Body mass index, kg/m2; mean (SD) | 29.1 (5.9) | 30.3 (6.4) | 27.8 (5.0)** | 28.8 (5.7) | 29.2 (6.1) | 28.4 (5.8) | 30.4 (6.0)** |
| Total cholesterol, mg/dl; mean (SD) | 178 (36) | 178 (36) | 178 (36) | 164 (34) | 188 (35)** | 176 (37) | 183 (33)** |
| Two or more classes of anti-hypertensive medication used in the prior year, % | 83.6 | 82.4 | 84.8 | 82.2 | 84.5 | 82.5 | 86.0* |
| Adherence | |||||||
| Low medication adherence, % | 14.1 | 16.4 | 11.8** | 13.0 | 14.9 | 12.3 | 18.4** |
| Non-persistent MPR (<0.8), % | 27.0 | 27.1 | 27.0 | 26.4 | 27.5 | 21.9 | 38.5** |
| Blood Pressure¥ | |||||||
| Blood Pressure | |||||||
| Systolic blood pressure; mean (SD) | 135 (14) | 134 (13) | 135 (14)* | 133 (13) | 136 (14)** | 134 (13) | 137 (14)** |
| Diastolic blood pressure; mean (SD) | 75 (9) | 76 (8) | 74 (9)* | 75 (9) | 75 (9) | 74 (9) | 77 (8)** |
| Uncontrolled Blood Pressure, % | 33.7 | 32.0 | 35.4 | 31.4 | 35.3 | 31.9 | 37.7* |
Excludes persons with race other than white or black (n=14)
Blood pressure (BP) included all participants with at least 2 blood pressure recordings on different days and used the 2 BP readings closest to the participant survey date to determine uncontrolled BP, N=1908; Uncontrolled BP was defined as mean SBP and DBP ≥140/90 mmHg
N= 1908 for blood pressure; N= 2087 for Medication Possession Ratio
p< 0.05;
p<0.01
SD -standard deviation; MPR-medication possession ratio
Overall, using MMAS, 14.1% of study participants had low adherence and 34.2% and 51.7% had medium and high adherence, respectively. Low medication adherence was more common among participants who were younger than 75 years of age, were black and had a higher BMI (BMI data not shown in table; p<0.01). Non-persistent MPR was more common among black participants. Those older than 75 years, women, and blacks had a higher mean systolic blood pressure; those younger than 75 years and blacks had a higher mean diastolic blood pressure. Overall, 33.7% of the participants had uncontrolled blood pressure. Blacks had a significantly higher prevalence of uncontrolled blood pressure (p<0.05). Marginally significant associations for gender (p=0.08) and duration of hypertension (data not shown in table; p=0.09) were also identified: women and participants with duration of hypertension > 10 years were more likely to have uncontrolled blood pressure.
Prevalence ratios (PR) of non-persistent MPR and uncontrolled blood pressure by category of medication adherence are presented in Table 3. After adjustment for age, race, and gender and compared to participants with high adherence by MMAS, participants with low adherence by MMAS were 2.71 (95% CI: 2.31 - 3.18) times more likely to have non-persistent MPR (p-trend<0.001). Also after age, race, and gender adjustment, participants with low medication adherence by MMAS were 1.20 (95% CI 1.00-1.43) times more likely to have uncontrolled blood pressure compared to those participants with high medication adherence by MMAS. Results were markedly similar after additional adjustment for duration of hypertension and BMI (data not presented). In addition, the association between adherence as measured by MPR and uncontrolled blood pressure was similar: participants with non-persistent MPR were 1.17 (95% CI 1.02-1.34) more likely to have uncontrolled blood pressure (data not presented in tables).
Table 3.
Associations of Morisky medication adherence scale scores with medication possession ratio and uncontrolled blood pressure in the Cohort Study of Medication Adherence among Older Adults (CoSMO)
| Morisky Medication Adherence Scale score category |
||||
|---|---|---|---|---|
| Low (<6) | Medium (6 to <8) | High (8) | p-value | |
| N | 291 | 709 | 1087 | N/A |
| Non-persistent MPRˇ (<0.8) | ||||
| Prevalence, % | 55% | 28% | 19% | <0.001 |
| Prevalence ratio* (95% CI) | 2.71 (2.31 - 3.18) | 1.42 (1.20 - 1.69) | 1.00 (ref) | <0.001 |
| N | 266 | 644 | 998 | N/A |
| Uncontrolled Blood Pressure^ | ||||
| Prevalence, % | 38 | 35 | 32 | 0.13 |
| PR (95% CI)* | 1.20 (1.00-1.43) | 1.07 (0.93-1.23) | 1.00 (ref) | <0.04 |
Included all participants with pharmacy fill data available for calculation of MPR, n=2087
Included all participants with at least 2 blood pressure recordings on different days and used the 2 BP readings closest to the participant survey date to determine uncontrolled BP, N=1908
Uncontrolled BP was defined as mean SBP and DBP ≥140/90 mmHg
PR-prevalence ratio, CI- confidence interval, MPR-medication possession ratio, BP-blood pressure
Adjusted for age, gender and race
Discussion
Relatively little is known about the relationship of demographics to medication adherence in older adults, and few studies have examined the validity of self-report adherence measures in the elderly (18). In the CoSMO study of older adults with hypertension, a substantial portion had low adherence to their antihypertensive medications and uncontrolled blood pressure. Black participants and individuals less than 75 years old had lower adherence levels compared to whites and individuals 75 years or older. Black participants had a significantly higher prevalence of uncontrolled blood pressure compared to their white counterparts. The current study of 2180 participants confirms a strong association between self-report adherence using the 8-item MMAS and pharmacy fill adherence using MPR, which was previously described in a small sample of hypertensive adults (11). Additionally, this study reports a significant association between self-reported low adherence by MMAS and uncontrolled blood pressure determined by clinic blood pressure readings, an association which has not been well-documented in an insured older population.
The baseline results of CoSMO support earlier findings that demographic and other risk factor differences in medication adherence and blood pressure control are present even in insured groups. Some work has been done to assess barriers to medication adherence in selected populations (19-21), yet, there is a paucity of information about which barriers affect different people. Understanding differences in barriers to medication adherence within demographic subgroups may help target interventions to overcome patient-specific barriers to adherence and to improve clinical outcomes (22-24). Several studies have found demographic disparities in medication adherence with lower adherence reported among younger individuals (25;26), men (25;27), and blacks (26;28;29). Numerous barriers to medication adherence have been identified including the asymptomatic nature of hypertension (21), depression (30), other non-cardiovascular comorbidities (31), lack of knowledge regarding hypertension and its treatment (32), beliefs about hypertension and its treatment (21), complexity and cost of medication regime (33-35), use of complementary and alternative medicine (34;36), health care system perceptions by the patient (37), sexual dysfunction (38), side effects of medication (39;40), forgetfulness (10;41), poor quality of life (2), inadequate social support (19;42), caring for dependents (28), and more recently disaster-related barriers (43;44). CoSMO will explore these barriers and their direct and indirect influence on medication adherence, blood pressure control and outcomes, overall, and in demographic subgroups. Barriers to medication adherence may be categorized into patient-specific (e.g. forgetfulness, beliefs), medication-specific (e.g. complexity of medication), logistic (e.g. frequency of clinic visits and pharmacy fills), and disease-specific (e.g. absence of symptoms for hypertension) barriers, which may provide a framework to facilitate communication with patients about medication adherence in clinical settings and may assist in developing multi-component behavioral interventions for further investigation (21).
Multiple strategies to improve medication adherence with the ultimate goal of improving rates of blood pressure control have been investigated; yet, no single intervention has emerged as superior (45-50). Interventions aimed at overcoming barriers to adherence have been classified into several broad groups: patient educational interventions (e.g. didactic teaching), patient behavioral interventions (e.g., patient motivation, support, reminders, drug packaging, simplification of dosing), provider interventions, and complex or combined patient interventions (e.g., educational coupled with behavioral interventions) (24). Although there is heterogeneity in the individual trials conducted to date, systematic reviews of the trials have revealed patient behavioral interventions (47;48;50), provider education interventions (46;47;51), and combination patient interventions (45;49) resulted in substantial improvements in adherence behaviors and in some studies blood pressure control; the benefits of patient educational interventions alone on medication adherence have been inconclusive (18;45;46;48). Given that several barriers may influence medication adherence and no single intervention has been identified as the gold standard for improving antihypertensive medication adherence, a patient-centered approach that tailors interventions to overcome patient-specific barriers to medication adherence is warranted (22-24;48;49).
It is important for physicians and other healthcare providers to consider low medication adherence as a factor contributing to poor blood pressure control, to communicate the importance of medication adherence in light of patient-specific barriers (i.e. tailored approach) with their patients, to consider strategies a priori that might lessen the effect of barriers on medication adherence, and to actively engage patients in the selection of strategies to improve adherence (24). However, clinicians often do not ask about medication adherence (52). Important limiting factors for providers considering adherence in their clinical decision-making are lack of time, doubt that low adherence is a cause of uncontrolled blood pressure, and uncertainty about how to accurately determine adherence and use this information in clinical practice (11;53). Determining patient adherence to antihypertensive medications in outpatient settings is an important first step for clinicians in understanding the effectiveness of the treatments they prescribe, identifying barriers to treatment, and improving blood pressure control. Validated and short self-report measures, such as MMAS, which provides information on factors affecting adherence such as forgetfulness and medication side effects may be useful in clinical settings (23). The baseline results of CoSMO reveal that the new 8-item self-report MMAS performed well with respect to its association with pharmacy fill adherence and blood pressure control in older insured adults, thus supporting its use in clinical settings to identify low adherers to antihypertensive medications.
The study results should be interpreted with the following limitations in mind. While, in the future, longitudinal data will be available from CoSMO, the analyses presented here were cross-sectional as data on change in medication adherence are not yet available. The current study was limited to English-speaking older adults with health insurance who were able to complete the baseline telephone survey. The association of MMAS with pharmacy fill was not perfect and may be due to short-comings of self-report measures (e.g. recall and social desirability bias) and inability of pharmacy fill data to capture nuances of medication-taking behavior (e.g. pill-splitting, taking medications on alternate days, stopping a medication because of side effects, and hospitalization) (11;53). The association of MMAS with uncontrolled blood pressure is conservative and the true association between low adherence and poor blood pressure control is likely larger than we report. Blood pressure measurements were abstracted from the EMR of primary care visits. Challenges of accurate blood pressure measurements in clinical settings have been documented, and missing data and misclassification are possible (54). The possible concern regarding missing data in the medical records is minimized due to the mandatory use of the EMR for all outpatient encounters at the primary institution providing care for the managed care participants (55). Nevertheless, our findings of associations between low adherence and poor blood pressure control are consistent with previous studies on middle-aged and disadvantaged patients which captured blood pressure as part of a standardized study protocol (10). Our study extends these findings to a population of older insured adults with diverse racial background.
The design of CoSMO has several strengths. The study population includes a large number of black and white patients and is diverse with respect to other socio-demographics and the presence of cardiovascular risk factors. The prospective cohort design, large sample size and breadth of the data being collected for this study provide the infrastructure for addressing many important questions. An added advantage of the current study is the ability to analyze these relationships across age, race and gender subgroups to distinguish whether groups of older patients are at greater risk of low adherence. The restriction of our sample to older adults in the managed care organization minimizes the confounding effects of health insurance, access to medical care, and employment status among older adults. Because hypertension is a prevalent disease, the results of this study may be useful in the evaluation and management of a substantial segment of the population.
Conclusions and Future Directions
Low adherence to antihypertensive medication is common and contributes to poor blood pressure control and adverse outcomes. There is lack of understanding of how patient-specific barriers influence low medication adherence and how effective interventions can be targeted to overcome barriers and improve adherence behavior in adults with hypertension. The CoSMO study is designed to provide data on the factors influencing medication adherence and lay the groundwork for interventions to improve antihypertensive medication adherence and clinical outcomes. Important next steps to move the field of antihypertensive medication adherence forward include understanding longitudinal changes in adherence, impact of low adherence on physiological measures, and development of tailored interventions that overcome patient-specific barriers.
Acknowledgement
Source of Support: The project described was supported by Grant Number R01 AG022536 from the National Institute on Aging. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health.
The authors gratefully acknowledge the contributions of the CoSMO Advisory Panel members including Edward Frohlich MD (Ochsner Clinic Foundation, New Orleans, LA), Jiang He MD, PhD (Tulane School of Public Health and Tropical Medicine, New Orleans, LA), Richard Re MD (Ochsner Clinic Foundation, New Orleans, LA), Paul K Whelton MD (Loyola University Medical Center, Chicago, IL)
The project described was supported by Grant Number R01 AG022536 from the National Institute on Aging. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- (1).Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- (2).Krousel-Wood M, Thomas S, Muntner P, et al. Medication adherence: A key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol. 2004;19:357–362. doi: 10.1097/01.hco.0000126978.03828.9e. [DOI] [PubMed] [Google Scholar]
- (3).Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999-2004. Hypertension. 2007;49:69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- (4).Hamilton GA. Measuring adherence in a hypertension clinic trial. Euro J Cardiovasc Nurs. 2003;2:219–228. doi: 10.1016/S1474-5151(03)00058-6. [DOI] [PubMed] [Google Scholar]
- (5).Dusing R. Overcoming barriers to effective blood pressure control in patients with hypertension. Curr Med Res Opin. 2006;22(8):1545–1553. doi: 10.1185/030079906X120995. [DOI] [PubMed] [Google Scholar]
- (6).Borzecki AM, Oliveria SA, Berlowitz DR. Barriers to hypertension control. Am Heart J. 2005;149:785–794. doi: 10.1016/j.ahj.2005.01.047. [DOI] [PubMed] [Google Scholar]
- (7).Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- (8).Callahan CM, et al. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40:771–781. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- (9).Stanley E, Wood RF, Kergosien L, Krousel-Wood MA. A comparison of self reported versus administrative race data (abstract) J Investig Med. 2008;56:485. [Google Scholar]
- (10).Morisky DE, Ang A, Krousel-Wood MA, Ward H. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10:348–354. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- (11).Krousel-Wood MA, Islam T, Webber LS, Morisky DE, Muntner P. New Medication adherence scale versus pharmacy fill rates in hypertensive seniors. Am J Managed Care. 2009 In press. [PMC free article] [PubMed] [Google Scholar]
- (12).Kopjar B, Sales AEB, Pineros SL, Sun H, Yu-Fang L, Hedeen AN. Adherence with statin therapy in secondary prevention of coronary heart disease in Veterans Administration male population. Am J Cardiol. 2003;92:1106–1108. doi: 10.1016/j.amjcard.2003.07.008. [DOI] [PubMed] [Google Scholar]
- (13).Rizzo JA, Simons WR. Variations in compliance among hypertensive patients by drug class: Implications for health care costs. Clin Ther. 1997;19:1446–1457. doi: 10.1016/s0149-2918(97)80018-5. [DOI] [PubMed] [Google Scholar]
- (14).Sikka R, Xia F, Aubert RE. Estimating medication persistency using administrative claims data. Am J Manag Care. 2005;11:449–457. [PubMed] [Google Scholar]
- (15).Simpson E, Beck C, Richard H, Eisenberg MJ, Pilote L. Drug prescriptions after acute myocardial infarction: dosage, compliance, and persistence. Am Heart J. 2003;145:438–444. doi: 10.1067/mhj.2003.143. [DOI] [PubMed] [Google Scholar]
- (16).Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidiity in Longitudinal studies: Development and validation. J Chron Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- (17).Deyo RA, Cherkin DC, MA Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM Administrative Databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- (18).Russell C, Conn V, Jantarakupt P. Older adult medication compliance: Integrated review of randomized controlled trials. Am J Health Behavior. 2006;30:636–650. doi: 10.5555/ajhb.2006.30.6.636. [DOI] [PubMed] [Google Scholar]
- (19).Fongwa MN, Evangelista LS, Hays RD, Martins DS, Elashoff D, Cowan MJ, et al. Adherence treatment factors in hypertensive African American women. Vasc Health Risk Manag. 2008;4(1):157–166. doi: 10.2147/vhrm.2008.04.01.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (20).Ogedegbe G, Mancuso CA, Allegrante JP, Charlson ME. Development and evaluation of a medication adherence self-efficacy scale in hypertensive African-American patients. J Clin Epidemiol. 2003;56:520–529. doi: 10.1016/s0895-4356(03)00053-2. [DOI] [PubMed] [Google Scholar]
- (21).Ogedegbe G, Harrison M, Robbins L, Mancuso CA, Allegrante JP. Barriers and facilitators of medication adherence in hypertensive African Americans: a qualitative study. Ethn Dis. 2004;14:3–12. [PubMed] [Google Scholar]
- (22).Harmon G, Lefante J, Krousel-Wood MA. The role of providers in improving patient adherence to antihypertensive medications. Curr Opin Cardiol. 2006;21:310–315. doi: 10.1097/01.hco.0000231400.10104.e2. [DOI] [PubMed] [Google Scholar]
- (23).Hawkshead J, Krousel-Wood MA. Techniques of measuring medication adherence in hypertensive patients in outpatient settings: advantages and limitations. Dis Manag Health Outcomes. 2007;15:109–118. [Google Scholar]
- (24).Krousel-Wood M, Hyre A, Muntner P, Morisky DE. Methods to improve medication adherence in hypertensive patients: Current status and future directions. Curr Opin Cardiol. 2005;20:296–300. doi: 10.1097/01.hco.0000166597.52335.23. [DOI] [PubMed] [Google Scholar]
- (25).Marentette MA, Gerth WC, Billings DK, Zarnke KB. Antihypertensive persistence and drug class. Can J Cardiol. 2002;18:649–656. [PubMed] [Google Scholar]
- (26).Monane M, Bohn RL, Gurwitz JH, Glynn RJ, Levin R, Avorn J. The effects of initial drug choice and comorbidity on antihypertensive therapy compliance: results from a population-based study in the elderly. Am J of Hypertens. 1997;10:697–704. doi: 10.1016/s0895-7061(97)00056-3. [DOI] [PubMed] [Google Scholar]
- (27).Caro JJ, Salas M, Speckman JL, Raggio G, Jackson JD. Persistence with treatment for hypertension in actual practice. CMAJ. 1999;160:31–37. [PMC free article] [PubMed] [Google Scholar]
- (28).Hyre A, Krousel-Wood MA, Muntner P, Kawasaki L, DeSalvo KB. Prevalence and predictors of poor antihypertensive medication adherence in an urban health clinic setting. J Clin Hypertension. 2007;9:179–186. doi: 10.1111/j.1524-6175.2007.06372.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (29).Sharkness CM, Snow DA. The patient's view of hypertension and compliance. Am J Prev Med. 1992;8:141–146. [PubMed] [Google Scholar]
- (30).Wang PS, Bohn RL, Knight E, Glynn RJ, Mogun H, Avorn J. Noncompliance with antihypertensive medications: the impact of depressive symptoms and psychosocial factors. J Gen Intern Med. 2002;17:504–511. doi: 10.1046/j.1525-1497.2002.00406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (31).Wang PS, Avorn J, Brookhart MA, et al. Effects of noncardiovascular comorbidites on antihypertensive use in elderly hypertensives. Hypertension. 2005;46:273–279. doi: 10.1161/01.HYP.0000172753.96583.e1. [DOI] [PubMed] [Google Scholar]
- (32).Egan BH, Lackland DT, Cutler NE. Awareness, knowledge and attitudes of older Americans about high blood pressure: implications for health care policy, education, and research. Arch Intern Med. 2003;163:681–687. doi: 10.1001/archinte.163.6.681. [DOI] [PubMed] [Google Scholar]
- (33).Iskedjian M, Einarson TR, MacKeigan LD, Shear N, Addis A, Mittmann N, et al. Relationship between daily dose frequency and adherence to antihypertensive pharmacotherapy: evidence from meta-analysis. Clin Ther. 2002;24:302–316. doi: 10.1016/s0149-2918(02)85026-3. [DOI] [PubMed] [Google Scholar]
- (34).Brown CM, Segal R. The effects of health and treatment perceptions on the use of prescribed medication and home remedies among African American and white American hypertensives. Soc Sci Med. 1996;43:903–917. doi: 10.1016/0277-9536(95)00434-3. [DOI] [PubMed] [Google Scholar]
- (35).Steinman MA, Sands LP, Covinsky KE. Self-retriction of medications due to cost in seniors without prescription coverage: a national survey. J Gen Intern Med. 2001;16:793–799. doi: 10.1111/j.1525-1497.2001.10412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (36).Gohar F, Greenfield SM, Beevers DG, Lip GYH, Jolly K. Self-care and adherence to medication: a survey in the hypertension outpatient clinic. BMC Complementary and Alternative Medicine. 2008;8:4. doi: 10.1186/1472-6882-8-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (37).World Health Organization . Hypertension in adherence to long-term therapies evidence for action. World Health Organization; 2003. pp. 107–114. [Google Scholar]
- (38).Grimm RH, Grandits GA, Prineas RJ, McDonald RH, Lewis CE, Flack JM, et al. Longterm effects on sexual function of five antihypertensive drugs and nutritional hygenic treatment in hypertensive men and women. Treatment of mild hypertension study. Hypertension. 1997;29:8–14. doi: 10.1161/01.hyp.29.1.8. [DOI] [PubMed] [Google Scholar]
- (39).Wassertheil-Smoller S, Blaufox MD, Oberman A, et al. Effects of antihypertensives on sexual function and quality of life: the TAIM study. Ann Intern Med. 1991;114:613–620. doi: 10.7326/0003-4819-114-8-613. [DOI] [PubMed] [Google Scholar]
- (40).Gregoire JP, Moisan J, Guibert R, et al. Tolerability of antihypertensive drugs in a community-based setting. Clin Ther. 2001;23:715–726. doi: 10.1016/s0149-2918(01)80021-7. [DOI] [PubMed] [Google Scholar]
- (41).Morisky DE, Green W, Levine DM, et al. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- (42).Schroeder K, Fahey T, Hollinghurst S, Peters TJ. Nurse-led adherence support in hypertension: A randomized controlled trial. Fam Pract. 2005;22:144–151. doi: 10.1093/fampra/cmh717. [DOI] [PubMed] [Google Scholar]
- (43).Islam T, Muntner P, Webber LS, Morisky DE, Krousel-Wood M. Cohort Study of Medication Adherence in Older Adults: Extended effects of Hurricane Katrina on medication adherence among older adults. Am J Med Sci. 2008;336(2):105–110. doi: 10.1097/MAJ.0b013e318180f175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (44).Krousel-Wood M, Islam T, Muntner P, et al. Medication adherence in older patients with hypertension after Hurricane Katrina: iimplications for clinical practice and disaster management. Am J Med Sci. 2008;336:99–104. doi: 10.1097/MAJ.0b013e318180f14f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (45).McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: scientific review. JAMA. 2002;288(22):2868–2879. doi: 10.1001/jama.288.22.2868. [DOI] [PubMed] [Google Scholar]
- (46).Morrison A, Wertheimer Al, Berger ML. Interventions to improve antihypertensive drug adherence: a quantitative review of trials. Formulary. 2000;35:234–255. [Google Scholar]
- (47).Roter DL, Hall JA, Merisca R, Nordstrom B, Cretin D, Svarstad B. Effectiveness of interventions to improve patient compliance: a meta-analysis. Med Care. 1998;36(8):1138–1161. doi: 10.1097/00005650-199808000-00004. [DOI] [PubMed] [Google Scholar]
- (48).Schroeder K, Fahey T, Ebrahim S. How can we improve adherence to blood pressurelowering medication in ambulatory care? Systematic review of randomized controlled trials. Arch Intern Med. 2004;164(7):722–732. doi: 10.1001/archinte.164.7.722. [DOI] [PubMed] [Google Scholar]
- (49).Takiya LN, Peterson AM, Finley RS. Meta-analysis of interventions for medication adherence to antihypertensives. Ann Pharmacother. 2004;38(10):1617–1624. doi: 10.1345/aph.1D268. [DOI] [PubMed] [Google Scholar]
- (50).Wetzels GE, Nelemans P, Schouten JS, Prins MH. Facts and fiction of poor compliance as a cause of inadequate blood pressure control: a systematic review. J Hypertens. 2004;22(10):1849–1855. doi: 10.1097/00004872-200410000-00002. [DOI] [PubMed] [Google Scholar]
- (51).Inui TS, Yourtee EL, Williamson JW. Improved outcomes in hypertension after physician tutorials: a controlled trial. Ann Intern Med. 1976;84:646–651. doi: 10.7326/0003-4819-84-6-646. [DOI] [PubMed] [Google Scholar]
- (52).Bokhour BG, Belowitz DR, Long JA, Kressin NR. How do providers assess antihypertensive medication adherence in medical encounters? J Gen Intern Med. 2006;21:577–583. doi: 10.1111/j.1525-1497.2006.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (53).Grymonpre R, Cheang M, Mmath, Fraser M, Metge C, Sitar DS. Validity of a prescription claims database to estimate medication adherence in older persons. Med Care. 2006;44:471–477. doi: 10.1097/01.mlr.0000207817.32496.cb. [DOI] [PubMed] [Google Scholar]
- (54).Jones DW, Appel LJ, Sheps SG, Roccella EJ, Lenfant C. Measuring Blood Pressure Accurately. New and Persistent Challenges. JAMA. 2003;289:1027–1030. doi: 10.1001/jama.289.8.1027. [DOI] [PubMed] [Google Scholar]
- (55).Elder NC, Hickner J. Missing Clinical Information. The System is Down. JAMA. 2005;293:617–619. doi: 10.1001/jama.293.5.617. [DOI] [PubMed] [Google Scholar]
- (56).Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- (57).Williams MV, et al. Relationship of functional health literacy to patients' knowledge of their chronic disease: a study of patients with hypertension and diabetes. Arch Internal med. 1998;158:166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- (58).Labbate LA, Lare SB. Sexual dysfunction in male psychiatric outpatients: validity of the Massachusetts General Hospital Sexual Functioning Questionnaire. Psychother Psychosom. 2001;70:221–225. doi: 10.1159/000056257. [DOI] [PubMed] [Google Scholar]
- (59).Kim MT, et al. Depression, substance use, adherence behaviors, and blood pressure in urban hypertensive black men. Ann Behav Med. 2003;26:24–31. doi: 10.1207/S15324796ABM2601_04. [DOI] [PubMed] [Google Scholar]
- (60).Knight RG, et al. Psychometric properties of the Center for Epidemiologic Studies Depression Scale (CES-D) in a sample of women in middle life. Behavior Research & Therapy. 1997;35:373–380. doi: 10.1016/s0005-7967(96)00107-6. [DOI] [PubMed] [Google Scholar]
- (61).Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- (62).Roberts R, et al. Effests of language and ethnic status on reliability and validity of the CES-D with psychiatric patients. J Nervous and Mental Disease. 1989;177:581–592. doi: 10.1097/00005053-198910000-00001. [DOI] [PubMed] [Google Scholar]
- (63).Fernander A, Duran R, Saab P, Liabre M, Schneiderman N. Assessing the reliability and validity of the John Henry Scale in an urban sample of African-Americans and white-Americans. Ethnicity and Health. 2003;8:147–161. doi: 10.1080/13557850303563. [DOI] [PubMed] [Google Scholar]
- (64).Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- (65).2003-04 Blood Pressure Questionnaire-BPQ_C. http://www.cdc.gov/nchs/data/nhanes/nhanes 03 04/sp bpq c.pdf. 2-15-2008.
- (66).Lengacher C, Bennett MP, Kipp KE, Berarducci A, Cox CE. Design and testing of the use of a complementary and alternative therapies survey in women with breast cancer. Oncol Nurs Forum. 2003;30:811–821. doi: 10.1188/03.ONF.811-821. [DOI] [PubMed] [Google Scholar]
- (67).Davies AR, Ware JE. In: GHAA's consumer satisfaction survey and user's manual. Group Health Association of America, editor. Washington, DC: 1991. [Google Scholar]
- (68).Jatulis DE, Bundek NI, Legorreta AP. Identifying predictors of satisfaction with access to medcial care and quality of care. Am J Med Qual. 1997;12:11–18. doi: 10.1177/0885713X9701200103. [DOI] [PubMed] [Google Scholar]
- (69).Krousel-Wood MA, Re R, Kleit A, Chambers R, Altobello C, Ginther B, Gomez N, et al. Patient and physician satisfaction in a clinical study of telemedicine in a hypertensive patient population. Journal of Telemedicine and Telecare. 2001;7:206–211. doi: 10.1258/1357633011936417. [DOI] [PubMed] [Google Scholar]
- (70).Meng YY, Jatulis DE, McDonald JP, Legoretta AP. Satisfaction with access to and quality of health care among medicare enrollees in a health maintenance organization. West J Med. 1997;166:242–247. [PMC free article] [PubMed] [Google Scholar]
- (71).Holmes TH, Rahe RH. The social readjustment rating scale. Jouranl of Psychosomatic Research. 1967;11:213–218. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- (72).Inui A, Kitaoaka H, Majima M, et al. Effects of the Kobe Earthquake on stress and glycemic control in patients with diabetes mellitus. Arch Intern Med. 1998;158:274–278. doi: 10.1001/archinte.158.3.274. [DOI] [PubMed] [Google Scholar]
- (73).Benight C, Ironson G, Durham R. Psychometric Properties of a hurricane coping self-efficacy measure. Journal of Traumatic Stress. 1999;12:379–386. doi: 10.1023/A:1024792913301. [DOI] [PubMed] [Google Scholar]
- (74).Ruggiero KJ, Del Ben K, Scotti JR, Rabalais AE. Psychometric properties of the PTSD Checklist-Civilian Version. J Trauma Stress. 2003;16:495–502. doi: 10.1023/A:1025714729117. [DOI] [PubMed] [Google Scholar]
- (75).Weathers FW, Huska JA, Keane TM. PCL-C for DSM-IV. Boston, MA: 1994. [Google Scholar]
- (76).Bland SH, Parinaro E, Krogh V, Jossa F, Scottoni A, Trevisan M. Long term relations between earthquake experiences and coronary heart disease risk factors. Am J Epidemiol. 2000;151:1086–1090. doi: 10.1093/oxfordjournals.aje.a010152. [DOI] [PubMed] [Google Scholar]
- (77).Krousel-Wood MA, Re RN. Health status assessment in a hypertension section of an internal medicine clinic. The American Journal of Medical Sciences. 1994;308:211–217. doi: 10.1097/00000441-199430840-00001. [DOI] [PubMed] [Google Scholar]
- (78).McHorney CA, Ware JE, Rogers W, Raczek AE, Rachel Lu JF. The validity and relative precision of MOS Short-and long-form health scales and Dartmouth COOP chart. Results from the Medical Outcomes Study. Medical Care. 1992;30:MS253–MS265. doi: 10.1097/00005650-199205001-00025. [DOI] [PubMed] [Google Scholar]
- (79).Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. conceptual framework and item selection. Medical Care. 1992;30:473–483. [PubMed] [Google Scholar]
- (80).Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey-Manual and Interpretation Guide. New England Medical Center; Boston, MA: 1993. [Google Scholar]