Abstract
Background
In the United States, blacks and Hispanics have lower cancer screening rates than whites have. Studies on the screening behaviors of minorities are increasing, but few focus on the factors that contribute to this discrepancy. This study presents the self-reported willingness by blacks, Puerto Rican Hispanics, and non-Hispanic whites to participate in cancer screenings in differing cancer screening situations.
Methods
The Cancer Screening Questionnaire (CSQ), a 60-item questionnaire, was administered via random-digit-dial telephone interviews to adults in three cities: Baltimore, Maryland; New York, New York; and, San Juan, Puerto Rico.
Results
The 1,148 participants in the CSQ study sample consisted of 355 blacks, 311 Puerto Rican Hispanics, and 482 non-Hispanic whites. Response rates ranged from 45% to 58% by city. Multivariable logistic regression analyses revealed that blacks and Puerto Ricans were often more likely (OR 2.0-3.0) and never less likely than whites to self-report willingness to participate in cancer screenings regardless of who conducted the cancer screening, what one was asked to do in the cancer screening, or what type of cancer was involved (with the exception of skin cancer where blacks, compared with whites, had an OR of 0.5).
Conclusions
The findings from this study provide evidence that blacks and Hispanics self-report that they are either as willing or more willing than whites to participate in cancer screening programs.
Introduction
Cancer is the second-leading cause of death in the United States and affects people of all racial and ethnic groups. However, the rates of cancer occurrence and cancer death vary significantly between ethnic groups. For example, overall cancer incidence and mortality rates are higher for blacks compared with other groups. According to the National Cancer Institute in 2005,1 the cancer incidence rate of blacks in the United States was 512.3 per 100,000, while for whites and Hispanics, it was 479.7 and 352.4 per 100,000, respectively. A similar pattern was observed regarding cancer death rates (African Americans = 248.1, whites = 195.3, and Hispanics = 135.2 per 100,000).
Differences by gender have also been observed. Black females, for example, have the highest incidence rates for colorectal cancer (56.0) and lung and bronchus cancer (55.2) and the highest mortality rate for breast cancer (37.5). White females have the highest incidence for breast cancer (119.4) and the highest cancer death rate for lung and bronchus,1 and Hispanic women have the highest incidence for cervical cancer (15.8 per 100,000).1,2 Black men have the highest incidence and mortality rates for prostate, colorectal, and lung and bronchus cancers. Puerto Rican Hispanic males, living in either Puerto Rico or the United States, also have high incidence and mortality rates for prostate, colorectal, and lung and bronchus cancers.1,3,4
While the burden of cancer in minority populations is high, attempts to provide cancer screening examinations to minority populations have met with varied success at best.5-9 The evidence is clear that early detection of cancer is one of the most effective means of lowering cancer mortality rates,10,11 but it is also clear that blacks and Hispanics have lower cancer screening rates than whites in the United States.5,6 Given that disadvantaged minority populations have less access to health care, cancer screening programs often provide the only means of early detection for a substantial proportion of minority populations.12 The body of literature on reported past cancer screening behaviors of minorities has been expanding,5-9,12-15 but fewer reports focus on the underlying factors of the willingness of minorities to participate in cancer screenings, especially compared with whites.16 Most studies on factors related to minority participation in cancer screenings have been qualitative studies, usually utilizing focus group methodology that targets defining the concepts, language, and parameters of the issue.17-28 Far fewer quantitative studies have investigated these factors in minority populations,29,30 and only one study focused directly on the comparative question of whether minority populations are as willing as whites to participate in cancer screenings.16
A recent article focusing on the comparative willingness to participate in cancer screenings between Puerto Ricans living in San Juan, Puerto Rico, and Puerto Rican Americans living in New York, NY, reported that (1) those living in San Juan had a slightly but consistently higher self-reported willingness to participate in cancer screenings than those living in New York, and (2) the odds of San Juan Puerto Ricans participating in skin cancer screening, compared with New York Puerto Ricans were 3-fold higher in regard to participation in skin cancer screenings.16
The overall aim of the 3-City Cancer Screening Study was to address and understand a range of issues related to factors that determine whether blacks and Puerto Rican Hispanics, compared with non-Hispanics whites, would be willing to take part in cancer screening examinations. This understanding is critical to achieving early cancer detection goals in order to reduce the higher cancer mortality currently observed in minority populations. Specifically, this report focused on the self-reported willingness of blacks, Puerto Rican Hispanics, and non-Hispanic whites to participate in cancer screenings under differing cancer screening situations: (1) for differing site-specific types of cancer screening examinations, (2) for differing health care providers/institutions conducting the cancer screenings, and (3) for differing circumstances as to “what one is asked to do”as a part of that cancer screening examination.
Methods
The 3-City Cancer Screening Study was designed to administer the 60-item Cancer Screening Questionnaire (CSQ) via random-digit-dial telephone interviews to 900 adults aged 18 years and older in three cities: Baltimore, Maryland; New York, New York; and San Juan, Puerto Rico. The within-city recruitment goals were to recruit 300 blacks (150 in New York and 150 in Baltimore), 300 whites (150 in New York and 150 in Baltimore), and 300 Puerto Rican Hispanics (150 in New York and 150 in San Juan). The CSQ was developed in 2001 by a multidisciplinary, multi-university research team within the New York University Oral Cancer Research on Adolescent and Adult Health Promotion (RAAHP) Center, an Oral Health Disparities Center, funded from 2001-2009 by the National Institute of Dental and Craniofacial Research (NIDCR) at the National Institutes of Health (NIH). The CSQ addresses a range of issues related to the willingness of minorities to participate in cancer screening examinations, with a focus on whether minorities are more reluctant to participate in cancer screening examinations and, if so, the reasons for their reluctance.
An international opinion research corporation (Macro International, Inc, Burlington,Vermont) conducted the random-digit-dial survey using a computer-assisted telephone interviewing (CATI) system. The survey sample was drawn from the total noninstitutionalized adult populations (ages 18 years and over) residing in telephone-equipped dwelling units in the three target cities. The telephone survey followed a 10-attempt dialing protocol, in which up to 10 attempts were made unless a final disposition was obtained. A final disposition was attained when (1) the respondent completed the interview,(2) the telephone number was found to be invalid, (3) the record reached 10 attempts distributed among three different day parts, or (4) the respondent gave a final refusal. Experienced, supervised personnel conducted the interviews using CATI software (Computers for Marketing Corp, San Francisco, California) The CSQ study provided for a disproportionally allocated, stratified, random digit sample of telephone-equipped residential households in the targeted sites. Each of the three sites, New York, Baltimore, and San Juan, was sampled independently. Both English and Spanish versions of the CSQ were available and used at the preference of the interviewee.
Table 1 shows the key questions from the CSQ that constituted the primary dependent variables, ie, willingness to participate in cancer screenings. Question 7 is the single best gestalt item in the CSQ to assess overall willingness to participate without regard to specific type of cancer, while the subsections of Question 16 ask about willingness to participate in 10 site-specific types of cancer screenings. The influence of “who conducts” the cancer screening is the focus of Question 17 as its subquestions present the respondent with a choice of 10 different providers. Finally, Question 18 focuses on the influence of “what one is asked to do” in the cancer screening on willingness to participate as it describes 11 different activities. The primary independent variable of race/ethnicity was obtained using the standard two-part question, first asking about Hispanic status (Yes/No), then asking about race using the standard US categories of white, black/African-American, Asian/Pacific Islander, American Indian/Native American, and Other. Respondents who indicated that they are Hispanic further specified whether they are Puerto Rican or Mexican-American, or Other Hispanic. The variable of age was calculated from a “date of birth” variable on the CSQ. The level of education and level of income variables were collected via an ordinal listing of nine ascending categories of educational level and of 10 ascending categories of income level, each of which was then collapsed into three ascending categories for the demographic table and five ascending categories for the multivariable analyses. To acknowledge and account for cultural differences between the cities (above and beyond simple demographic differences), the variable of “city” was included as a separate covariate in all multivariable analyses.
Table 1.
Four Questions From the CSQ on the Likelihood of Participation in Cancer Screening Examinations
| Response choices for all four questions are: | |
| • very likely | |
| • somewhat likely | |
| • not quite sure | |
| • somewhat unlikely | |
| • very unlikely | |
| Question 7. How likely are you to agree to have a cancer screening exam at the present time? Are you … (read response choices above)? | |
| Question 16. How likely are you to have each of the following specific types of cancer screening exams? If the screening exams were for … (give specific exam from list below), would you be … (read responses choices above)? | |
| • breast cancer | • prostate cancer |
| • colon cancer | • blood cancer |
| • lung cancer | • skin cancer |
| • stomach cancer | • rectal cancer |
| • liver cancer | • oral cancer |
| Question 17. Some people would feel differently depending on who was providing the cancer screening. I'm going to read you a list of people who might do a cancer screening. For each one, tell me how likely you would be to participate in a cancer screening exam. If the screening exam were provided by …(give specific “who” from list below), would you be …(read response choices above)? | |
| • own doctor | • own dentist |
| • university medical school | • nonprofit foundation |
| • university dental school | • university nursing school |
| • insurance company | • government |
| • drug company | • tobacco company |
| Question 18. There are different types of cancer screening exams that involve different things. How likely are you to participate in a cancer screening exam if you had to do the following? How about if you had to …(give specific activity from list below), would you be (read response choices above): | |
| • give blood sample | • x-rays taken |
| • exam by doctor | • diet interview |
| • spit out saliva | • exam by dentist |
| • scrape cells from mouth/skin | • smoking habit interview |
| • exam by nurse | • alcohol habit interview |
| • surgical skin biopsy | |
Unadjusted bivariable analysis was used as a pathway leading to adjusted multivariable analyses. For the unadjusted bivariable analyses, the proportion of those willing to participate in cancer screenings were dichotomized into Likely (Very Likely + Somewhat Likely) and Unlikely (Not Quite Sure + Somewhat Unlikely + Very Unlikely) and statistical significance was evaluated by means of chi-square tests with the significance level set at P ≤ .05. Multivariable logistic regression analysis, which accounted for the multistage sampling techniques used in the random-digit-dial telephone survey and which adjusted for age, sex, education, income, and city, produced odds ratios (ORs) with 95% confidence intervals (CIs). Specifically, the PROC SURVEYFREQ and PROC SURVEYLOGISTIC procedures (SAS Institute Inc, Cary, North Carolina) were used for all data analyses to account for the complex sampling frame used in this random-digit-dial survey. Finally, the fit of the logistic regression was assessed by the omnibus test, the Hosmer-Lemeshow Test, as well as the classification table and the residual scores.
Results
The CSQ response rates (ie,number of completed interviews/number of contacted households) ranged from 45% to 58% by city, with an overall completion rate (ie, number of completed interviews/number of initiated interviews) of 82.6%. The original targeted within-city enrollment goals for each ethnic/racial group were met or exceeded, and the overall final CSQ study sample (N = 1,148) consisted of 355 blacks, 311 Puerto Rican Hispanics, and 482 non-Hispanic whites. The mean age of respondents was 46.8 years (SD = 16.0), with a range of 19 to 96 years, and 65.1% of the respondent sample were female. Table 2 shows the age, sex, education, and income distribution of the 1,148 subjects within the three racial/ethnic groups.
Table 2.
Distribution of Age, Sex, Education, and Income Within Racial/Ethnic Groups in the 3-City Cancer Screening Study (N = 1,148)
| Race/Ethnic Group | Mean Age (± SD) | Female | Education Level | Income Level |
|---|---|---|---|---|
| Blacks (n = 355)a,b | 45.1 ± 16.5 | 72.4% | Less than high school graduate = 19.9% | < $20,000 = 41.5% |
| High school graduate = 59.1% | $20,000-$74,999 = 49.5% | |||
| College graduate or greater = 21.0% | ≥ $75,000 = 9.0% | |||
| Whites (n = 482)a,c | 47.5 ± 17.0 | 56.8% | Less than high school graduate = 10.6% | < $20,000 = 19.6% |
| High school graduate = 44.0% | $20,000-$74,999 = 59.7% | |||
| College graduate or greater = 45.4% | ≥ $75,000 = 20.6% | |||
| Puerto Rican Hispanics (n = 311)b,c | 44.0 ± 15.9 | 69.5% | Less than high school graduate = 19.8% | < $20,000 = 39.2% |
| High school graduate = 43.3% | $20,000-$74,999 = 49.8% | |||
| College graduate or greater = 36.9% | ≥ $75,000 = 11.0% |
Statistically significant contrasts*:
For blacks vs whites contrast: differed on age, sex, education and income (P ≤ .05).
For blacks vs Puerto Rican Hispanics contrast: differed on education (P ≤ .05).
For Puerto Rican Hispanics vs whites contrast: differed on age, sex, education and income (P ≤ .05).
* = ANOVA test for age; Pearson chi-square tests for gender, education, and income.
In response to the question: “How likely are you to agree to have a cancer screening exam at the present time?” (Question 7), considered to be the overall single best gestalt question on willingness to participate in cancer screenings, the vast majority of each racial/ethnic group indicated that they were likely to participate in cancer screenings: 79.5% for Puerto Rican Hispanics, 73.7% for blacks, and 73.2% for whites (differences were not statistically significant, P = .11). Even after a multivariable logistic regression analysis adjusted for age, sex, education, income, and city, there were no statistically significant differences in willingness to participate in cancer screenings across the three racial/ethnic groups, as measured by Question 7.
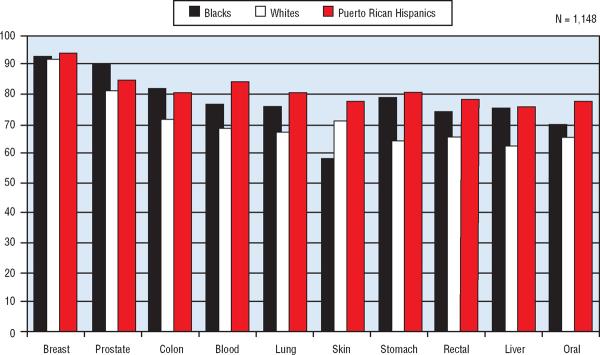
The differences by race/ethnicity in percent willing to participate in cancer screenings for different site-specific type-of-cancer examinations (Question 16a-j) are shown in Fig 1. The findings, for all subjects combined, ranged from a high in self-reported willingness to participate for the two sex-specific cancers (93% for breast cancer examinations and 85% for prostate cancer examinations) to a low for oral cancer examinations (70%). For the remaining seven site-specific type-of-cancer screening examinations, the findings revealed that the self-reported willingness to participate ranged from 71% to 77%. (The percent of “willingness to participate for skin cancer” in Fig 1 was calculated as 74% by using only the average “willingness to participate” percent of whites and Hispanics combined without including the percent for blacks, to acknowledge the reality of much lower skin cancer risk in blacks and thus to avoid biasing the “best” estimate for this specific cancer.)
Fig 1.
Percentage likely to participate in cancer screenings dependent on type of cancer being screened for in the 3-City Cancer Screening Study.
The observed racial/ethnic differences in willingness to participate in cancer screening examinations for the eight non-sex-specific cancer sites were all statistically significant (P < .002) with a clear pattern among the three racial ethnic groups. Whites were consistently the least likely to indicate willingness to participate, and Puerto Rican Hispanics were consistently the most willing. The only exceptions were colon cancer screenings (for which blacks were the most willing) and skin cancer screenings (with blacks appropriately seeing themselves at lowest risk and thus least willing). While there were no statistically significant differences between the racial/ethnic groups for the two sex-specific cancers (breast and prostate) regarding willingness to participate in cancer screenings, the observed difference for prostate cancer examinations was notable with blacks (91%) being more willing than whites (81%) (P =.096). This percent difference likely failed to achieve statistical significance due to the smaller sample size, ie, only male subjects or 35% of the total sample size for the non-sex-specific cancers.
As shown in Table 3, when a multivariable logistic regression analysis (adjusted for age, sex, education, income, and city) was performed for each of the 10 site-specific types of cancer, the ORs indicated that (1) Puerto Rican Hispanics, compared with whites, were more willing to participate in cancer for 4 of the 10 site-specific cancers: lung, stomach, liver, and blood (leukemia) cancers (OR = 2.07-2.60), (2) blacks, compared with whites, were more willing to participate in a cancer screening for stomach cancer (OR = 2.13, 95% CI 1.24-3.65), and (3) blacks, compared with whites, were less willing to participate in skin cancer screenings (OR = 0.53, 95% CI 0.31-0.89). Except for this finding on skin cancer in blacks, neither blacks nor Puerto Rican Hispanics self-reported a lower willingness than whites for any other of the site-specific types of cancer.
Table 3.
Logistic Regression Multivariable Analyses for Statistically Significant Findings From the Key Questions From the CSQ by Racial/Ethnicity Group in the 3-City CSQ Study (N = 1,148)*
| Question 16 | Specific Type of Cancer | Contrast | OR | 95% CI |
| Skin | Black vs white | 0.53 | 0.41-0.89 | |
| Lung | Puerto Rican Hispanic vs white | 2.16 | 1.20-3.87 | |
| Stomach | Black vs white | 2.13 | 1.24-3.65 | |
| Stomach | Puerto Rican Hispanic vs white | 2.60 | 1.43-4.70 | |
| Liver | Puerto Rican Hispanic vs white | 2.38 | 1.33-4.24 | |
| Blood | Puerto Rican Hispanic vs white | 2.07 | 1.06-4.05 | |
| Question 17 | “Who” Conducts Cancer Screening | Contrast | OR | 95% CI |
| Nonprofit foundation | Black vs white | 1.90 | 1.07-3.36 | |
| Nonprofit foundation | Puerto Rican Hispanic vs white | 1.96 | 1.07-2.58 | |
| Tobacco company | Black vs white | 1.78 | 1.08-2.92 | |
| Drug company | Black vs white | 2.06 | 1.28-3.31 | |
| Drug company | Puerto Rican Hispanic vs white | 2.64 | 1.54-4.52 | |
| Question 18 | “What Asked To Do” in Cancer Screening | Contrast | OR | 95% CI |
| Exam by nurse | Black vs white | 2.14 | 1.29-3.55 | |
| Diet interview | Black vs white | 2.97 | 1.44-6.11 | |
| Alcohol habit interview | Puerto Rican Hispanic vs white | 0.54 | 0.30-0.97 | |
| Skin biopsy | Black vs white | 0.45 | 0.28-0.72 |
Adjusted for race, age, sex, education, income, and city, and accounting for multistage sampling.
OR = odds ratio, CI = confidence interval.
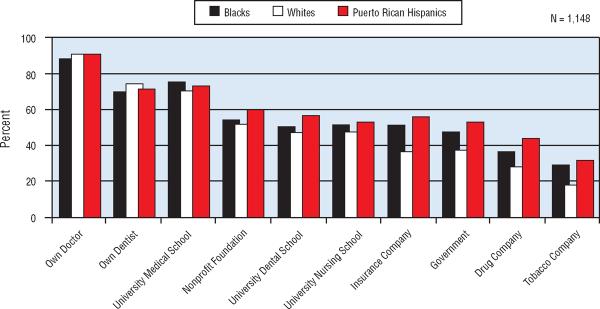
The unadjusted bivariable findings from Question 17a-j are shown in Fig 2. These findings reveal, for the study sample as a whole, a large range in percent likely to participate in cancer screenings depending on “who” was conducting the study, from a high of 91% “if conducted by your own MD” to a low of 25% “if run by a tobacco company” (a 3.6-fold difference). Statistically significant differences across racial/ethnic groups were detected for five specific “who” categories (university dental school, government, insurance company, drug company, and tobacco company) with a consistent pattern across the three racial/ethnic groups. Puerto Rican Hispanics were the most willing to indicate that they would participate; whites were the least willing. The three racial/ethnic groups showed slight to occasionally substantial differences in response to any one “who” probe, but on the whole they exhibited similar ratings across the “who” factor (Fig 2). The three racial/ethnic groups ranked “own doctor,”“own dentist,” and “university medical school” as the most trusted in “who” factors, while “drug company” and “tobacco company” ranked lowest. Among the other “who” factors that formed the middle responses (about 45% to 58% likelihood), “government” was the lowest of these middle-ranked factors (45%).
Fig 2.
Percentage likely to participate in cancer screenings dependent on “who” was conducting the screening in the 3-City Cancer Screening Study.
Table 3 also shows the multivariable logistic regression analysis (adjusted for age, sex, education, income, and city) performed for the 10 different health care providers or health agencies/institutions (ie,focused on the factor of “who” conducted the cancer screenings factor). The only statistically significant finding revealed ORs for blacks and Puerto Rican Hispanics that were higher than whites for willingness to participate when the “who” was either a nonprofit foundation, drug company, or tobacco company (the latter only for blacks). ORs ranged from 1.78 to 2.64. A check of the magnitude of the regression coefficients in these analyses revealed a good fit of the logistic regression model as used. Further in this exploratory first use of the CSQ in a survey, as none of the nonstatistically significant findings showed any noteworthy differences, they were not judged to be meaningful.
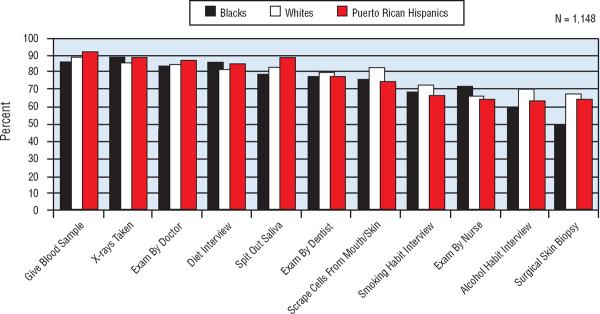
In parallel fashion, the unadjusted bivariable findings from Question 18a-k on “what one is asked to do in a study” are presented in Fig 3. Again, the range is considerable, depending on “what one is asked to do” in cancer screenings, and the three racial/ethnic groups generally demonstrated similar ratings across the 11 specific probes; they appeared to more or less travel together “up-and-down” the scale of willingness to participate, with no consistent pattern by race/ethnicity. The “what one is asked to do” categories that elicited the highest willingness to participate were “give blood sample” and “have x-rays taken” (89% and 88%, respectively) followed by “exam by doctor” (85%) and “diet interview” (84%). The middle group of categories were composed of “spit out saliva” (80%),“exam by dentist” (79%) and “scrape cells from mouth or skin” (79%). The lowest group included “smoking habit interview” (70%),“exam by nurse” (68%),“alcohol habit interview” (66%), with “surgical skin biopsy” having the lowest ranking (61%). Statistically significant differences between the racial/ethnic groups was found for only four of these “what one is asked to” categories: whites were highest and blacks lowest for “alcohol habit interviews” and “surgical skin biopsy,” whites were highest and Puerto Rican Hispanics lowest for “scraping cells from mouth or skin,” and Puerto Rican Hispanics were highest and blacks lowest for “give blood sample.”
Fig 3.
Percentage likely to participate in cancer screenings dependent on “what one is asked to do” in the screening in the 3-City Cancer Screening Study.
Multivariable logistic regression analysis (adjusted for age, sex, education, income, and city) performed for the 11 differing categories of “what one is asked to do” in the cancer screenings activities (Table 3) revealed statistically significant findings. The OR for blacks, compared with whites, to self-report willingness to participate in a cancer screening was higher when they were asked to be interviewed about diet habits (OR = 2.97, 95% CI 1.44-6.11) or asked about having an examination by a nurse (OR = 2.14, 95% CI 1.29-3.55). However, the OR for blacks, compared with whites, to self-report willingness to participate in a cancer screening when they were asked to have a surgical skin biopsy taken under local anesthetic was less than one-half that of whites (OR = 0.45, 95% CI 0.28-.072).
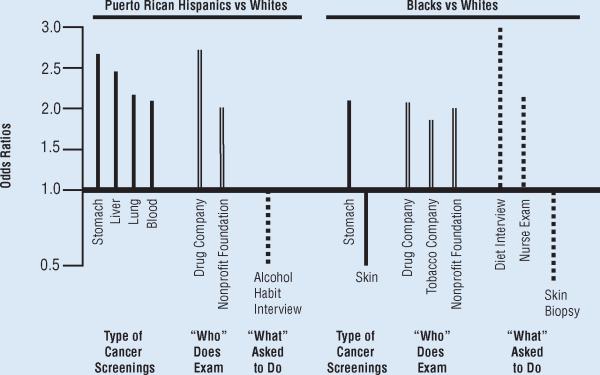
Fig 4 shows the statistically significant differences between blacks, Puerto Rican Hispanics, and whites presented in Table 3 on the willingness to participate in cancer screenings for site-specific type of cancer, for “who”does the examination, and for “what one is asked to do” in that cancer screening for the specific ethnic/racial group contrasts.
Fig 4.
Statistically significant odds ratios for likelihood of participating in cancer screenings: a comparison of blacks vs whites and of Puerto Rican Hispanics vs whites, type of cancer screenings, “who does exam,” and “what” one is asked to do in the screening in the 3-City Cancer Screening Study.
Discussion
Given that the overall aim of the 3-City Cancer Screening Study was to address a range of issues related to factors that determine whether blacks and Puerto Rican Hispanics, compared with non-Hispanics whites, would be willing to take part in cancer screening examinations, there is clear justification for presenting both the unadjusted bivariable analyses and the adjusted multivariable analyses since each has specific utility to different audiences. The unadjusted bivariable analyses has utility for those in the public health arena since the data provided have immediate “on the ground” reality; these data regarding a racial/ethnic group currently would be valid. Basically, the unadjusted bivariable analyses target the “what happens if I plan to do this in the community” type of question. On the other hand, adjusted multivariable analysis results possess a different utility, one more related to a long-term, more detached “controlled scientific understanding” of the factors that affect any observed differences across race/ethnicity. Specifically, multivariable analyses pursue the more analytical (albeit often hypothetical) “what if” type of question, seeking to search for the influence of a key factor of interest under the “artificial situation” where all other factors are kept equal across the racial/ethnic groups.
Thus, the answer to the question posed by public health workers — “Are minorities less likely to be willing to participate in cancer screenings than whites?”—is found in the unadjusted bivariable analyses, in the data that reflect all of the cultural and demographic imbalances in today's communities. The findings show that the overall answer is “no,” based on these self-reported data on willingness to participate in cancer screenings. Across 62 separate statistical contrasts between blacks and whites or Hispanics and whites for the 31 different specific circumstances of “type of cancer” screenings, “who” conducts the screening, and “what one is asked to do” in the screening, blacks and/or Hispanics were no less likely than whites to self-report willingness to participate in 93.5% of these specific contrasts.
Based on the adjusted multivariable analyses, the key scientific findings on influential factors show that race/ethnicity does have a measurable influence on many of the observed statistically significant differences in self-reported willingness to participate in cancer screenings when age, sex, education, income, and city are taken into account. For 12 of the 15 statistically significant multivariable adjusted contrasts between racial/ethnic groups (across the 62 contrasts for “type of cancer,”“who conducts the screening,”and “what one is asked to do”), the odds of being willing to participate were 2- to 3-fold higher for blacks and/or Hispanics than for whites. There were three exceptions in which a minority group was less likely to self-report willingness to participate than whites. Two involved blacks and skin cancer circumstances (for skin cancer screening, and having a skin biopsy) and one involved Puerto Rican Hispanics (having a alcohol habit interview).
A limitation of this study was that it was the first administration of the CSQ in a full survey, and therefore methodological questions remain to be answered about the CSQ as a research instrument. The CSQ was derived from the previously designed questionnaire, the Tuskegee Legacy Project (TLP) Questionnaire,which was designed to explore whether minorities are more reluctant than whites to participate in biomedical research, and if so, to explore the reasons (including the Tuskegee Syphilis Study) for any observed differences. The TLP Questionnaire was developed over a period of 3 years via focus group studies and a series of pilot studies and is described elsewhere.31,32 Subsequently, the same multidisciplinary team that developed the TLP Questionnaire on “willingness to participate in biomedical research studies” then developed a parallel questionnaire, the CSQ, to explore similar issues regarding “willingness to participate in cancer screenings.” As the CSQ was derived in format from the TLP Questionnaire, most questions were already refined via the focus group and pilot studies were done in developing the TLP Questionnaire over that 3-year period. Necessary changes in wording to address “cancer screening participation” were pretested on a small sample of pilot CSQ interviews. The current wording of questions related to cancer screening participation as used in the CSQ reflects how invitations to have screenings for a specific type of cancer are typically announced in a community or referred to by physicians, and thus they likely have face validity, as was demonstrated in our pilot study phase. Nevertheless, future methodological studies could probe for a clearer understanding of the beliefs of the respondents when they answered questions about willingness to participate in different types of cancer screenings. Was it a general concern about that type of cancer, or were they well enough informed to envision different specific cancer screening procedures as used by physicians (eg, FOBT vs colonoscopy for colon cancer)? These and other in-depth methodological probes would serve to improve both the CSQ as a research instrument (via modifications) and thereby improve our understanding of individuals' willingness to participate in cancer screenings as a result of either additional questions developed or modifications to existing questions currently used in the CSQ.
The burden of cancer falls disproportionately on the poor and disadvantaged in society, but the reasons for these disproportionate cancer-related health disparities are still unclear. However, although there is consensus that early detection of cancer is one of the most effective means of assuring timely treatment and survival, too few people take advantage of the tests available to screen early for common cancers.10,11 This is especially true for Hispanics and blacks who have lower screening rates than whites have.5,6,33 Overall, blacks and Hispanics, as well as others with lower level of formal education, are less likely to have such examinations, possibly due to reduced access to medical care.7-9,12 Several other factors have been associated with low cancer screening utilization: low income level, low level of education, lack of insurance,6,7,34-36 older age,36-40 unemployment, poor housing, inadequate access to health care,1,36,41,42 limited knowledge about cancer, poor knowledge and attitude toward the screening process, lack of a regular physician, language barriers, and competing demands.7,12-14,40,43-45
Studies conducted with different minority groups have found that in addition to the barriers already mentioned, other important factors hinder cancer screening utilization for these populations. These factors include cultural differences, racial bias, emotions and beliefs,46,47 fear of cancer, embarrassment, acculturation,48,49 and fatalistic beliefs.37,50 Thus, it is not surprising that the burden of cancer deaths is particularly high among blacks and Hispanics compared with whites.
Several recent surveys have asked respondents about their past cancer screening activities and participation. Surveys on past cancer screening participation rates have reported a range of 46% to 80% for breast cancer in women,5,7-9 56% to 82% for cervical cancer,5,6,8,13 36% to 55% for colon cancer,12,14 and 41% for prostate cancer.5 While the range of these findings of reported past cancer screening participation (36% to 82%) is lower than those in this current study on rates of self-reported willingness to participate for 10 site-specific cancer screenings (70% to 94%), the fact that the two ranges do overlap is an indication that “cancer screening behavior” does approach cancer screening intentions. Clearly, the high end for both practices and intentions were found for those cancer screening programs that have received major attention in the media and have the biggest campaigns for participation, such as breast and cervical cancers in women.
Conclusions
The findings from this study show that blacks and Hispanics self-report a willingness to participate in cancer screenings that is at least equal to that of whites, and they are frequently more willing than whites, under several different circumstances. The only exception involved blacks and skin cancer, where the odds of willingness to participate in cancer screenings were,appropriately and understandably, half that of whites. Given these findings, efforts by researchers, medical personnel, and community health workers are needed to overcome the often-cited barriers faced by these minority populations. Encouraging the willingness of minorities to take part in screening programs would equalize participation rates in screening and thus improve outcomes as regards to cancer mortality.
Acknowledgments
Appreciation is expressed to Mr Piotr Brzoza, Ms Michelle M. Haghpanah, and Ms Anne X. Truong, three graduate students, for their assistance with preliminary analyses related to this manuscript.
Disclosures The 3-City Cancer Screening Study was supported by grant U54 DE 14257 from the National Institute of Dental and Craniofacial Research/National Institutes of Health (NIDCR/NIH), the New York University Oral Cancer Research on Adolescent and Adult Health Promotion Center (an Oral Health Disparities Research Center).
Abbreviations used in this paper
- CSQ
Cancer Screening Questionnaire
- TLP
Tuskegee Legacy Project
Footnotes
No significant relationship exists between the authors and the companies/organizations whose products or services may be referenced in this article.
References
- 1.National Cancer Institute Cancer Health Disparities: Questions and Answers. http://www.cancer.gov/cancertopics/factsheet/cancer-health-disparities. Accessed May 21, 2008.
- 2.Centers for Disease Control and Prevention (CDC) Invasive cervical cancer among Hispanic and non-Hispanic women: United States, 1992-1999. MMWR Morb Mortal Wkly Rep. 2002;51(47):1067–1070. [PubMed] [Google Scholar]
- 3.Puerto Rico Central Cancer Registry . Preliminary data on death rates-2003. Puerto Rico Dept of Health; Nov, 2006. [Google Scholar]
- 4.Puerto Rico Central Cancer Registry . Preliminary data on incidence rates-2003. Puerto Rico Dept of Health; Nov, 2006. [Google Scholar]
- 5.Swan J, Breen N, Coates RJ, et al. Progress in cancer screening practices in the United States: results from the 2000 National Health Interview Survey. Cancer. 2003;97(6):1528–1540. doi: 10.1002/cncr.11208. [DOI] [PubMed] [Google Scholar]
- 6.Zambrana RE, Breen N, Fox SA, et al. Use of cancer screening practices by Hispanic women: analyses by subgroup. Prev Med. 1999;29(6 pt 1):466–477. doi: 10.1006/pmed.1999.0566. [DOI] [PubMed] [Google Scholar]
- 7.Garza MA, Luan J, Blinka M, et al. A culturally targeted intervention to promote breast cancer screening among low-income women in East Baltimore, Maryland. Cancer Control. 2005;12(suppl 2):34–41. doi: 10.1177/1073274805012004S06. [DOI] [PubMed] [Google Scholar]
- 8.Coughlin SS, Uhler RJ. Breast and cervical cancer screening practices among Hispanic women in the United States and Puerto Rico, 1998-1999. Prev Med. 2002;34(2):242–251. doi: 10.1006/pmed.2001.0984. [DOI] [PubMed] [Google Scholar]
- 9.Coughlin SS, Uhler RJ, Bobo JK, et al. Breast cancer screening practices among women in the United States, 2000. Cancer Causes Control. 2004;15(2):159–170. doi: 10.1023/B:CACO.0000019496.30145.62. [DOI] [PubMed] [Google Scholar]
- 10.Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2006. CA Cancer J Clin. 2006;56(2):106–130. doi: 10.3322/canjclin.56.2.106. [DOI] [PubMed] [Google Scholar]
- 11.Smith RA, Cokkinides V, Eyre HJ. American Cancer Society guidelines for the early detection of cancer, 2006. CA Cancer J Clin. 2006;56(1):11–25. doi: 10.3322/canjclin.56.1.11. quiz 49-50. [DOI] [PubMed] [Google Scholar]
- 12.Wee CC, McCarthy EP, Phillips RS. Factors associated with colon cancer screening: the role of patient factors and physician counseling. Prev Med. 2005;41(1):23–29. doi: 10.1016/j.ypmed.2004.11.004. Epub 2004 Dec 29. [DOI] [PubMed] [Google Scholar]
- 13.Abraído-Lanza AF, Chao MT, Gammon MD. Breast and cervical cancer screening among Latinas and non-Latina whites. Am J Public Health. 2004;94(8):1393–1398. doi: 10.2105/ajph.94.8.1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.James AS, Campbell MK, Hudson MA. Perceived barriers and benefits to colon cancer screening among African Americans in North Carolina: how does perception relate to screening behavior? Cancer Epidemiol Biomarkers Prev. 2002;11(6):529–534. [PubMed] [Google Scholar]
- 15.Horowitz AM, Nourjah PA. Factors associated with having oral cancer examinations among US adults 40 years of age or older. J Public Health Dent. 1996;56(6):331–335. doi: 10.1111/j.1752-7325.1996.tb02460.x. [DOI] [PubMed] [Google Scholar]
- 16.Claudio C, Katz RV, Green BL, et al. Cancer screening participation: comparative willingness of San Juan Puerto Ricans versus New York City Puerto Ricans. J Natl Med Assoc. 2007;99(5):542–549. [PMC free article] [PubMed] [Google Scholar]
- 17.Blocker DE, Romocki LS, Thomas KB, et al. Knowledge, beliefs and barriers associated with prostate cancer prevention and screening behaviors among African-American men. J Natl Med Assoc. 2006;98(8):1286–1295. [PMC free article] [PubMed] [Google Scholar]
- 18.Forrester-Anderson IT. Prostate cancer screening perceptions, knowledge and behaviors among African American men: focus group findings. J Health Care Poor Underserved. 2005;16(4 suppl A):22–30. doi: 10.1353/hpu.2005.0122. [DOI] [PubMed] [Google Scholar]
- 19.McFall SL, Hamm RM, Volk RJ. Exploring beliefs about prostate cancer and early detection in men and women of three ethnic groups. Patient Educ Couns. 2006;61(1):109–116. doi: 10.1016/j.pec.2005.02.016. Epub 2005 Oct 26. [DOI] [PubMed] [Google Scholar]
- 20.Yu MY, Wu TY. Factors influencing mammography screening of Chinese American women. J Obstet Gynecol Neonatal Nurs. 2005;34(3):386–394. doi: 10.1177/0884217505276256. [DOI] [PubMed] [Google Scholar]
- 21.Skokar NK, Vernon SW, Weller SC. Cancer and colorectal cancer: knowledge, beliefs, and screening performance of a diverse population. Fam Med. 2005;37(5):341–347. [PubMed] [Google Scholar]
- 22.Ogedegbe G, Cassells AN, Robinson CM, et al. Perceptions of barriers and facilitators of cancer early detection among low-income minority women in community health centers. J Natl Med Assoc. 2005;97(2):162–170. [PMC free article] [PubMed] [Google Scholar]
- 23.Woods VD, Montgomery SB, Herring RP. Recruiting Black/African American men for research on prostate cancer prevention. Cancer. 2004;100(5):1017–1025. doi: 10.1002/cncr.20029. [DOI] [PubMed] [Google Scholar]
- 24.Jones AR, Thompson CJ, Oster RA, et al. Breast cancer knowledge, beliefs, and screening behaviors among low-income, elderly black women. J Natl Med Assoc. 2003;95(9):791–797. 802–805. [PMC free article] [PubMed] [Google Scholar]
- 25.Gupta A, Kumar A, Stewart DE. Cervical cancer screening among South Asian women in Canada: the role of education and acculturation. Health Care Women Int. 2002;23(2):123–134. doi: 10.1080/073993302753429004. [DOI] [PubMed] [Google Scholar]
- 26.McCoy CB, Anwyl RS, Metsch IR, et al. Prostate cancer in Florida: knowledge, attitudes, practices, and beliefs. Cancer Pract. 1995;3(2):88–93. [PubMed] [Google Scholar]
- 27.Morgan C, Park E, Cortes DE. Beliefs, knowledge, and behavior about cancer among urban Hispanic women. J Natl Cancer Inst Monogr. 1995;(18):57–63. [PubMed] [Google Scholar]
- 28.Tortolero-Luna G, Glober GA, Villarreal R, et al. Screening practices and knowledge, attitudes, and beliefs about cancer among Hispanic and non-Hispanic white women 35 years or older in Nueces County, Texas. J Natl Cancer Inst Monogr. 1995;(18):49–56. [PubMed] [Google Scholar]
- 29.Watts BG, Vernon SW, Myers RE, et al. Intention to be screened over time for colorectal cancer in male automotive workers. Cancer Epidemiol Biomarkers Prev. 2003;12(4):339–349. [PubMed] [Google Scholar]
- 30.Demark-Wahnefired W, Strigo T, Catoe K, et al. Knowledge, beliefs, and prior screening behavior among blacks and whites reporting for prostate cancer screening. Urology. 1995;46(3):346–351. doi: 10.1016/S0090-4295(99)80218-0. [DOI] [PubMed] [Google Scholar]
- 31.Katz RV, Kegeles SS, Green BL, et al. The Tuskegee Legacy Project: history, preliminary scientific findings and unanticipated societal benefits. Dent Clin North Am. 2003;47(1):1–19. doi: 10.1016/s0011-8532(02)00049-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Katz RV, Kegeles SS, Kressin NR, et al. The Tuskegee Legacy Project: willingness of minorities to participate in biomedical research. J Health Care Poor Underserved. 2006;17(4):698–715. doi: 10.1353/hpu.2006.0126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brown DR, Topcu M. Willingness to participate in clinical treatment research among older African Americans and Whites. Gerontologist. 2003;43(1):62–72. doi: 10.1093/geront/43.1.62. [DOI] [PubMed] [Google Scholar]
- 34.Palmer RC, Fernandez ME, Tortolero-Luna G, et al. Acculturation and mammography screening among Hispanic women living in a farmworker communities. Cancer Control. 2005;12(suppl 2):21–27. doi: 10.1177/1073274805012004S04. [DOI] [PubMed] [Google Scholar]
- 35.Cancer Trends Progress Report: 2005 Update. National Cancer Institute, National Institute of Health, Department of Health & Human Services; Bethesda, MD: 2005. http://progressreport.cancer.gov/faq.asp?did=2005&fid=2005&mid=vfq&pid=1. Accessed May 28, 2008. [Google Scholar]
- 36.Bowie JV, Curbow BA, Garza MA, et al. A review of breast, cervical, and colorectal cancer screening interventions in older women. Cancer Control. 2005;12(suppl 2):58–69. doi: 10.1177/1073274805012004S09. [DOI] [PubMed] [Google Scholar]
- 37.Mayo RM, Erwin DO, Spitler HD. Implications for breast and cervical cancer control for Latinas in the rural South: a review of the literature. Cancer Control. 2003;10(5):60–68. doi: 10.1177/107327480301005s09. [DOI] [PubMed] [Google Scholar]
- 38.Ramirez AG, Suarez L, Laufman S, et al. Hispanic women breast and cervical cancer knowledge, attitudes, and screening behaviors. Am J Health Promot. 2000;14(5):292–300. doi: 10.4278/0890-1171-14.5.292. [DOI] [PubMed] [Google Scholar]
- 39.Wu ZH, Black SA, Markides KS. Prevalence and associated factors of cancer screening: why are so many older Mexican-American women never screened? Prev Med. 2001;33(4):268–273. doi: 10.1006/pmed.2001.0880. [DOI] [PubMed] [Google Scholar]
- 40.Mandelblatt JS, Gold K, O'Malley AS, et al. Breast and cervix cancer screening among multiethnic women: role of age, health and sources of care. Prev Med. 1999;28(4):418–425. doi: 10.1006/pmed.1998.0446. [DOI] [PubMed] [Google Scholar]
- 41.Olsen S. Cancer prevention and screening for underserved populations. Adult Health. 1999;1(6) In HTML format accessed through Meniscus Educational Institute. http://www.meniscus.com/web/pages/homepage.asp. [Google Scholar]
- 42.Christian MC, Trimble EL. Increasing participation of physicians and patients from underrepresented racial and ethnic groups in National Cancer Institute-sponsored clinical trials. Cancer Epidemiol Biomarkers Prev. 2003;12(3):277s–283s. [PubMed] [Google Scholar]
- 43.McCoy CB, Preyra M, Metsch LR, et al. A community-based breast cancer-screening program for medically underserved women: its effect on disease stage at diagnosis and on hazard of death. Rev Panam Salud Publica. 2004;15(3):160–167. doi: 10.1590/s1020-49892004000300004. [DOI] [PubMed] [Google Scholar]
- 44.Luquis RR, Villanueva IJ. Knowledge, attitudes, and perceptions about breast cancer and breast cancer screening among Hispanic women residing in South Central Pennsylvania. J Community Health. 2006;31(1):25–42. doi: 10.1007/s10900-005-8187-x. [DOI] [PubMed] [Google Scholar]
- 45.Hannon P, Harris JR, Martin D, et al. Colorectal cancer screening in Washington State: predictors of current screening and explanations for no screening. Prev Chronic Dis. 2005;2 [Google Scholar]
- 46.Weissman JS, Schneider EC. Social disparities in cancer: lessons from a multidisciplinary workshop. Cancer Causes Control. 2005;16(1):71–74. doi: 10.1007/s10552-004-1255-1. [DOI] [PubMed] [Google Scholar]
- 47.Magai C, Consedine N, Conway F, et al. Diversity matters: unique populations of women and breast cancer screening. Cancer. 2004;100(11):2300–2307. doi: 10.1002/cncr.20278. [DOI] [PubMed] [Google Scholar]
- 48.Wong-Kim E, Sun A, DeMattos MC. Assessing cancer beliefs in a Chinese immigrant community. Cancer Control. 2003;10(5 suppl):22–28. doi: 10.1177/107327480301005s04. [DOI] [PubMed] [Google Scholar]
- 49.O'Malley AS, Kemer J, Johnson AE, et al. Acculturation and breast cancer screening among Hispanic women in New York City. Am J Public Health. 1999;89(2):219–227. doi: 10.2105/ajph.89.2.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chavez LR, Hubbell FA, Mishra SI, et al. The influence of fatalism on self-reported use of Papanicolaou smears. Am J Prev Med. 1997;13(2):418–424. [PubMed] [Google Scholar]